Category: Pediatrics
Keywords: pediatrics, fever, seizure (PubMed Search)
Posted: 1/9/2025 by Kathleen Stephanos, MD
(Updated: 3/14/2025)
Click here to contact Kathleen Stephanos, MD
Simple Febrile Seizures are a very common cause for presentation to the Emergency Department.
Up to 5% of children will have one in their lifetime, and a single febrile seizure increases risk of recurrence.
Definition:
While not part of the formal definition, the following details are critical to obtain on history, and high risk features that should not be missed on initial evaluation:
Evaluation and Management:
Consider a finger stick
Most patients can be discharged to home after a period of observation - most use a 2-4 hour minimum. More recent literature suggests considering a longer observation period in patients who have seizures at lower core body temperatures (<39°C) or those with a history of recurrent simple febrile seizures (2 simple febrile seizures within 24 hours with return to baseline in between)
Obtain a lumbar puncture in all patients with symptoms of meningitis
Consider a lumbar puncture, lab evaluation, and prolonged observation in patients who are under-vaccinated/unvaccinated/unknown vaccination status between 6 months and 12 months of age, or received antibiotics within the last 48 hours
Eilbert W, Chan C. Febrile seizures: A review. J Am Coll Emerg Physicians Open. 2022 Aug 23;3(4):e12769. doi: 10.1002/emp2.12769. PMID: 36016968; PMCID: PMC9396974.
Category: Pharmacology & Therapeutics
Keywords: tenecteplase, alteplase, stroke (PubMed Search)
Posted: 3/10/2025 by Ashley Martinelli
(Updated: 3/13/2025)
Click here to contact Ashley Martinelli
On March 3, 2025, the FDA approved tenecteplase to treat acute ischemic stroke. Historically, only alteplase was FDA-approved, but the stroke guidelines suggest tenecteplase as a reasonable alternative and many centers have made the change to use tenecteplase.
The EXTEND-IA TNK trial showed benefit of tenecteplase over alteplase in patients who were candidates for mechanical thrombectomy. The newer AcT trial found that tenecteplase was non-inferior to alteplase for patients eligible for thrombolysis, regardless of thrombectomy candidacy. There was no difference in safety outcomes, specifically ICH or angioedema in either trial.
Tenecteplase will soon be available in a new 25 mg vial with stroke-specific packaging (potentially as early as June 2025). Currently, there is only a 50 mg vial that is used for STEMI and PE which has higher maximum dosing compared to stroke.
The dosing is now recommended in weight-based groupings based on the supplemental appendix from the AcT trial. This is likely a change in practice for most centers that previously implemented tenecteplase for stroke before the FDA approval. Consult with your stroke and pharmacy team to discuss potential protocol changes at your institution.

Campbell BCV, et al. NEJM 2018;378:1573-1582.
Menon BK, et al. Lancet 2022;400:161-69.
TNKase [package insert]. South San Francisco, CA. Genetech, Inc. 2025.
Genetech Press Release: https://www.gene.com/media/press-releases/15053/2025-03-03/fda-approves-genentechs-tnkase-in-acute-#:~:text=South%20San%20Francisco%2C%20CA%20%2D%2D,stroke%20(AIS)%20in%20adults.
Category: Gastrointestional
Keywords: Droperidol, abdominal pain (PubMed Search)
Posted: 3/13/2025 by Neeraja Murali, DO, MPH
(Updated: 2/7/2026)
Click here to contact Neeraja Murali, DO, MPH
Many of us probably use droperidol for pain relief in the ED. If you don't, two recent studies highlight it's use in multimodal pain control:
-In the DRUGS study (2023), droperidol reduced opiod use (46% vs 60%), lowered pain scores (median of 9 vs 5), and decreased the need for antiemetics (60% vs 73%). Before you ask - mean pain score wasn't reported!
-This study evaluated gastroparesis patients, with most common dose of droperidol being 1.25 mg IV
-the DREAMER study (2024) showed that pateitns receiving droperidol required fewer opiods (median 10 Morphine Milligram Equivalents vs 19.4 MME). No significant different in need for antiemetics
-This study evaluated abdominal pain patients, with 2.5 mg IV being the most common dose
Neither study found statistically significant differences in length of stay. Additionally, neither study reported major adverse effects or healthcare costs. Note that these were both single center trials as well.
With droperidol shortages ongoing, suggestions were made to directly compare droperidol to haloperidol, with hopefully more research coming soon!
-Stirrup N, Jones G, Arthur J, Lewis Z. Droperidol undermining gastroparesis symptoms (DRUGS) in the emergency department. Am J Emerg Med. 2024 Jan;75:42-45. doi: 10.1016/j.ajem.2023.10.030. Epub 2023 Oct 21. PMID: 37897920.
-Townsend BR, Malka ST, Di Paola SG, Nisly AE, Gilbert BW. DRopEridol for Abdominal pain in the emergency department for Morphine Equivalent Reduction. The DREAMER study. Am J Emerg Med. 2025 Jan 4;90:31-34. doi: 10.1016/j.ajem.2024.12.082. Epub ahead of print. PMID: 39798184.
Category: Obstetrics & Gynecology
Posted: 2/25/2025 by Jennifer Wang, MD
(Updated: 3/10/2025)
Click here to contact Jennifer Wang, MD
So you have a patient who is pregnant and has abdominal pain. You, as the astute provider you are, decide to do an ultrasound to rule out an ectopic, and low and behold! You see a gestational sac and a yolk sac within the uterus! You show your patient, you both breathe a sigh of relief, and you discharge them…
But they return two weeks later, now hypotensive, excruciating pain, and extremely pale. On an emergent bedside ultrasound, you see copious amounts of free fluid, and OBGYN tells you, after they rush your patient to the OR, that it was an ectopic - but how? The pregnancy was in the uterus!
Welcome everyone to the world of interstitial and angular pregnancies, pregnancies that are much closer to the endometrium than normal ectopic pregnancies and therefore have a much higher chance of progressing further before they rupture, meaning that when they do, they are devastating!
To evaluate for these ectopics, make sure that you get a mantle distance on every pregnancy ultrasound you do looking for an ectopic. Mantle distance is measured from the end of the gestational sac to the outer edge of the thinnest side of endometrium. If your value is >0.8cm, you should be okay. If it's less than <0.5cm, you most likely have an ectopic. Between 0.5cm and 0.8cm, consult OB urgently or have extremely close follow up for your patient.

Doane B, Perera P. Emergency ultrasound identification of a cornual ectopic pregnancy. West J Emerg Med. 2012;13(4):315. doi:10.5811/westjem.2011.10.6912
https://radiopaedia.org/articles/interstitial-ectopic-pregnancy?lang=us
Category: Trauma
Keywords: Sarcopenia, trauma, ct scan (PubMed Search)
Posted: 3/9/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
Having a readily measurable variable to identify frailty on admission for critically injured patients would help prognosticate morbidity, mortality, and discharge destination. Sarcopenia has been used to prognosticate length of stay, discharge destination, and physical function recovery in oncology and general surgery patients. Sarcopenia is defined as “age-related progressive loss of muscle mass and strength. The main symptom of the condition is muscle weakness. Sarcopenia is a type of muscle atrophy primarily caused by the natural aging process. Scientists believe being physically inactive and eating an unhealthy diet can contribute to the disease.” 1. This study looked at admission CT scan psoas muscle sarcopenia in 197 critically injured patients. The authors concluded:
“For trauma critical care patients, sarcopenia on admission CT was associated with dependent discharge destination and therefore is unfavourable. Defining sarcopenia early in a trauma patient’s critical care admission may help to identify those at risk of poor outcomes.” 2
1. Sarcopenia (Muscle Loss): Symptoms & Causes
2. Badminton R, Christie R, Brohi K, Cole E. Pre-injury sarcopenia and the association with discharge destination in critical care trauma patients. Trauma. 2025;27(1):57-64. doi:10.1177/14604086231214878
Category: Orthopedics
Posted: 3/8/2025 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Lidocaine transdermal patches
Frequently used for lower back pain.
A single 5% patch contains 700mg of lidocaine.
There is low systemic absorption.
Data supporting efficacy for lower back pain are limited.
Best benefit in other neuropathic conditions such as post herpetic neuralgia.
Topical capsicum
Underused, safe, non-sedating.
Potential treatment option for acute and subacute back pain (<3 months duration).
Can be OTC or via prescription.
Available in cream, lotion and patches.
Best used 3-4 times per day for maximal effectiveness.
Grade A recommendation from North American Spine Society.
Category: Trauma
Keywords: Male. Female, outcome, trauma (PubMed Search)
Posted: 3/6/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
The Pan-Asia Trauma Outcomes Study database was reviewed for differences in in-hospital mortality and functional capacity at discharge between male and female trauma patients. There were 76,000 trauma patients from 12 Asian countries in this study. The authors concluded: “This study indicates no difference in the general trauma outcomes in the Asia Pacific between females and males. Although younger females with less severe injuries had better functional outcomes, this advantage disappeared in severe injuries and those over 50 years.” There were several differences in mechanism of injury and age of presentation. “With females more frequently represented in the ??50 age group (60.13%) compared to males (44.87%) (p?<?0.001). Trauma type also varied between sexes; 95.51% of females experienced blunt trauma compared to 93.65% of males (p?<?0.001). Anatomically, males predominantly sustained injuries to the head, face, thorax, abdomen, and upper extremities, whereas females more frequently suffered injuries to the lower extremities and spine (p?<?0.001).” This is similar toEuropean and North American data
Bin Kunji Mohamad, M., Jamaluddin, S.F., Ahmad, N. et al. Trauma outcomes differences in females: a prospective analysis of 76 000 trauma patients in the Asia-Pacific region and the contributing factors. Scand J Trauma Resusc Emerg Med 33, 34 (2025). https://doi.org/10.1186/s13049-025-01342-1
Category: Trauma
Keywords: EMS, AlS, trauma, Bls, outcome (PubMed Search)
Posted: 3/5/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
Large retrospective propensity matching study looking at mortality in trauma patients based on ALS vs. BLS transport crew found lower mortality in those attended by ALS crews. The matching was “based on patient age, sex, year, ICD-10-CM based injury severity score, mechanism of injury, AIS based body region of injury, EMS characteristics including time with patient and prehospital interventions performed, prehospital vital signs, and trauma center designation.”
This is different than other studies which showed limited difference. other studies have shown improved survival with police “scooping and running” with penetrating trauma patients.
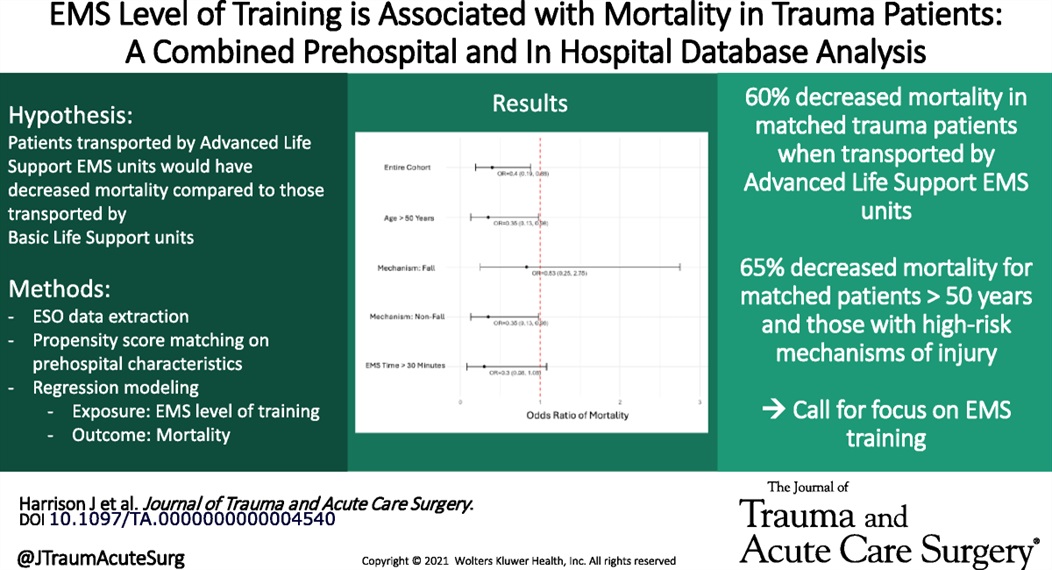
Harrison, Julia MD; Bhardwaj, Akshay MS; Houck, Olivia MPH; Sather, Kristiana MD; Sekiya, Ayako MPH; Knack, Sarah MD; Saarunya Clarke, Geetha PhD; Puskarich, Michael A. MD, MSCR; Tignanelli, Chris MD, MSc; Rogers, Lisa MPH; Marmor, Schelomo PhD; Beilman, Greg MD. Emergency medical services level of training is associated with mortality in trauma patients: A combined prehospital and in hospital database analysis. Journal of Trauma and Acute Care Surgery 98(3):p 402-409, March 2025. | DOI: 10.1097/TA.0000000000004540
Category: Critical Care
Keywords: Mechanical Ventilation, Brain Injury, ICH, Stroke, Hypercapnea, Hypoxia, Hyperoxia (PubMed Search)
Posted: 3/4/2025 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Intubation and mechanical ventilation of brain injured patients, which is extremely common in the Emergency Department, can be very challenging and subject to significant practice variation. It is often said that brain injured patients “can't take a joke”, meaning that they are less tolerant to hemodynamic and metabolic perturbations, and these perturbations tend to be associated with very large swings in their clinical outcomes. For example, hypo/hyperglycemia, hypo/hypernatremia, hypo/hypertension, hypo/hyperoxia, hypo/hypercapnea, etc are all extremely important to avoid. This is probably the one patient population where “euboxia” (the notion that we obsess too much about making all the numbers pretty in the EMR) is probably not as applicable. As such, there is at least good physiologic rationale, and now increasing empirical evidence, that ventilating these patients very thoughtfully is extremely important and likely to have meaningful impact on patient-oriented outcomes (mortality, neurologic outcome, etc).
The VENTIBRAIN study was a prospective observation trial of 2,095 intubated patients in 26 countries who had TBI, ICH (including SAH), or acute ischemic stroke. Interestingly, they found that patients with lower tidal volume (TV) per predicted body weight had higher mortality (although the majority of their TVs were well controlled and in a fairly tight range), which is contrary to conventional thinking in pulmonary pathologies like ARDS. They also found that higher driving pressure (DP) was associated with higher mortality, which agrees with data from other conditions. PEEP and FiO2 had U-shaped curves, but FiO2 in particular tended to favor lower FIO2, also similar to current thinking for ICU patients in general.
Take Home Points:
Learning Driving Pressure/PEEP Titration:
Category: Ultrasound
Keywords: POCUS, OB, retained products of conception (PubMed Search)
Posted: 3/3/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
A recent study evaluated the accuracy of POCUS in detecting retained products of conception (RPOC) in the emergency department.
In this study, a patient was considered positive for RPOC if they had heterogenous material in the endometrium measuring 10 mm or more. Color Doppler was not used for further evaluation, though it has been cited in obstetric literature as a helpful tool.
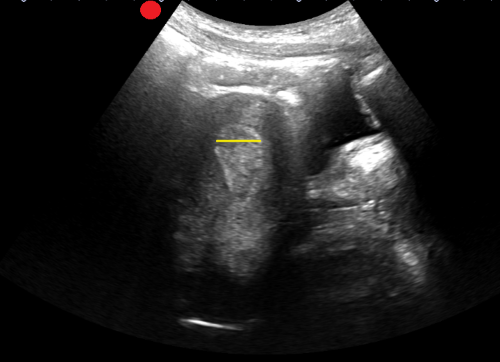
Among the 265 patients included, the prevalence of RPOC was 21.5%. POCUS had a sensitivity of 79.0 % and a specificity of 93.8 %.
The authors caution against the use of POCUS to diagnose RPOC in the setting of early pregnancy, as the endometrium can have a variable appearance, increasing the risk of a misdiagnosis. Of the 22 false positives identified, more than half were potentially viable pregnancies. Uterine fibroids can also lead to a heterogenous appearance of the uterus and can be another potential false positive.
Boivin Z, Barber D, Chimileski B, et al. Accuracy of point-of-care ultrasound in diagnosing retained products of conception. Am J Emerg Med. 2025;90:65-70. doi:10.1016/j.ajem.2025.01.032.
Category: Trauma
Keywords: Trauma, geriatric, fall, pain management, fracture, rib, pelvis (PubMed Search)
Posted: 3/1/2025 by Robert Flint, MD
(Updated: 3/2/2025)
Click here to contact Robert Flint, MD
Rib and pelvic fractures are common findings in geriatric trauma patients, even in low impact trauma such as falls from standing. Pain management is vital for improving morbidity and mortality. The IFEM White Paper suggests:
“Use multimodal pain management strategies, including regional anesthesia and non-opioid analgesics, to control pain without compromising recovery.
Monitor closely for complications such as pneumonia or hemodynamic instability, intervening promptly to mitigate risks.
Collaborate with physiotherapists to implement early mobility programs, reducing the risk of deconditioning and promoting recovery.”
A multidisciplinary team proficient in geriatric trauma care leads to better outcomes. This may require transfer to a trauma center.
Trauma in Older Adults: Evidence-Based Guidelines for Optimized Care White Paper
Trauma Special Interest Group and Geriatric Emergency Medicine Special Interest Group
https://assets.nationbuilder.com/ifem/pages/1768/attachments/original/1740084007/IFEM_Trauma_in_Older_Adults_Evidence-Based_Guidelines_for_Optimized_Care_White_Paper_December_2024.pdf?1740084007
Published: December 2024
Category: Trauma
Keywords: Trauma, geriatrics, frailty (PubMed Search)
Posted: 3/1/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This white paper reminds us that age is just a number; frailty is a better predictor of morbidity and mortality after trauma.
“Frailty, characterized by reduced physiological reserve and increased vulnerability to stressors, is a significant factor influencing recovery from trauma. Individuals with frailty may experience slower healing, higher rates of complications, and longer hospital stays. Tools such as the Clinical Frailty Scale (CFS) and the Trauma-Specific Frailty Index (TSFI) have been developed to assess frailty systematically, enabling clinicians to predict outcomes and guide treatment decisions.”
Trauma in Older Adults: Evidence-Based Guidelines for Optimized Care White Paper
Trauma Special Interest Group and Geriatric Emergency Medicine Special Interest Group
https://assets.nationbuilder.com/ifem/pages/1768/attachments/original/1740084007/IFEM_Trauma_in_Older_Adults_Evidence-Based_Guidelines_for_Optimized_Care_White_Paper_December_2024.pdf?1740084007
Published: December 2024
Category: Administration
Keywords: Nurse Practitioner, Physician Assistant, job satisfaction, burnout, longevity (PubMed Search)
Posted: 2/20/2025 by Steve Schenkel, MPP, MD
(Updated: 2/26/2025)
Click here to contact Steve Schenkel, MPP, MD
Nurse Practitioners and Physician Assistants practice alongside Physicians in Emergency Departments. In 2021, an estimated 17,679 NPs and PAs worked in EDs.
How long do NPs and PAs continue in Emergency Medicine practice?
An analysis of Medicare data reports that over the eight years of the study, the annual attrition rate averaged 13.8%, or almost 1 in 7 leaving Emergency Medicine practice every year. At the time of attrition, the median age for women was 40.2 years (IQR 33.8 to 49.9) and for men was 45.9 (IQR 37.8 to 56.3).
For additional breakdown and discussion of these numbers, see Gettel CJ, Chosh R, Rothenberg, et al. Workforce Attrition Among Emergency Medicine Non-Physician Practitioners. Ann Emerg Med, in press, https://www.annemergmed.com/article/S0196-0644(24)01294-0/fulltext.
Category: Critical Care
Keywords: Critically Ill, Intubated, Mechanical Ventilation, Ventilator-Associated Pneumonia (PubMed Search)
Posted: 2/25/2025 by Mike Winters, MBA, MD
(Updated: 2/7/2026)
Click here to contact Mike Winters, MBA, MD
Non-Pharmacologic Measures to Prevent VAP
Krone M, Seeber C, Nydahl P. What's New in Intensive Care: Preventing Ventilator-Associated Pneumonia Non-Pharmacologically. Intensive Care Med. 2024; 50:2185-2187.
Category: Ultrasound
Keywords: ONSD, POCUS, ocular exam, intracranial pressure (PubMed Search)
Posted: 2/24/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Point-of-care ultrasound (POCUS) measurement of the optic nerve sheath diameter (ONSD) has been shown to correlate with increases in intracranial pressure (ICP).
In adults, an ONSD measurement of less than 5 mm is considered normal, while a measurement greater than 6 mm suggests elevated ICP.
How to Measure the Optic Nerve Sheath Diameter:
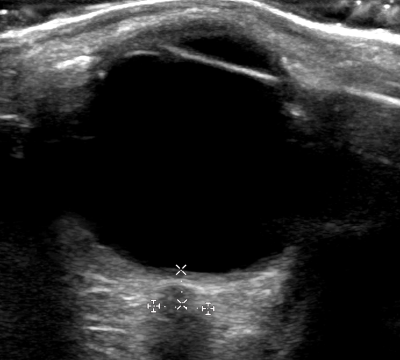
A small cross-sectional study examined whether ONSD measurements varied when taken at different depths. The findings indicated that ONSD increased by 0.32 mm at a depth of 4 mm and decreased by 0.54 mm at a depth of 2 mm.
These variations highlight the importance of maintaining a consistent measurement depth. To ensure accuracy and avoid misinterpretation, the ONSD should always be measured 3 mm posterior to the retina.
Gottlieb M, Kayarian F, Johnson J, Peksa GD. Differences in mean optic nerve sheath diameter measurements based on depth. Am J Emerg Med. 2024 Aug;82:197-198. doi: 10.1016/j.ajem.2024.06.013.
Category: Trauma
Keywords: Ems, trauma, arrest, resuscitation (PubMed Search)
Posted: 2/23/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
This position paper from American College of Surgeons, NAEMSP, and ACEP outlines a literature based approach to prehospital care of traumatic circulatory arrest. It logically could be applied to care in the hospital as well. Care of a traumatic arrest is different than a medical etiology arrest.
“Emphasize the identification of reversible causes of traumatic circulatory arrest and timely use of clinically indicated life-saving interventions (LSIs) within the EMS clinician’s scope of practice. These include:
Epinephrine should not be routinely used, and if used should not be administered before other LSIs.
External chest compressions may be considered but only secondary to other LSIs.
Chest decompression if there is clinical concern for a tension pneumothorax. Empiric bilateral decompression, however, is not indicated in the absence of suspected chest trauma.
Airway management using the least-invasive approach necessary to achieve and maintain airway patency, oxygenation, and adequate ventilation.
External hemorrhage control with direct pressure, wound packing, and tourniquets.”
Amelia M. Breyre, Nicholas George, Alexander R. Nelson, Charles J. Ingram, Thomas Lardaro, Wayne Vanderkolk, John W. Lyng,
Prehospital Management of Adults With Traumatic Out-of-Hospital Circulatory Arrest—A Joint Position Statement,
Annals of Emergency Medicine,
Volume 85, Issue 3,
2025,
Pages e25-e39,
ISSN 0196-0644,
https://doi.org/10.1016/j.annemergmed.2024.12.015.
Category: Orthopedics
Posted: 2/22/2025 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
A previous pearl discussed Spondylolysis. Once clinical concern is sufficient, the question of appropriate imaging arises.
Traditionally, the addition of oblique radiographs was recommended because they showed the pathognomonic “Scotty dog” sign. Recent studies have shown there is no significant increase in diagnosing spondylolysis with the addition of these oblique views. These additional views carry added cost and radiation exposure (approximately double).
AP and lateral radiographs offer similar diagnostic sensitivity to the old four view series.
If plain films are negative and symptoms persist despite 2-3 weeks of rest from offending activities, advanced imaging can be pursued on an outpatient basis. This is also strongly considered if the patient wishes to return to sport.
Despite being primarily osseous pathology, studies have shown that MRI can have similar diagnostic sensitivity to CT particularly in cases of acute injury. MRI may also show signs of stress reaction before complete fracture occurs.
Communicate with radiology and MRI technicians that you are looking for spondylolysis as this may affect the MRI sequences.
If a positive finding occurs on plain film, ordering CT imaging for the entire lumbar spine should be deferred due to added radiation concerns especially in cases where MRI would be available.
If MRI is not practical, consider limiting CT to one level above and one level below the region of concern. This would decrease the radiation exposure by approximately 50%
If advanced imaging is not practical or available and patient has a positive plain film, consider recommending repeat imaging in 4-6 weeks as an outpatient with rest from all offending activities.
Category: Pediatrics
Keywords: SI, hypotension, trauma, shock (PubMed Search)
Posted: 2/20/2025 by Jenny Guyther, MD
(Updated: 2/21/2025)
Click here to contact Jenny Guyther, MD
This was a retrospective cohort study of the national trauma data bank that included about 64000 pediatric trauma patients in the derivation group and the same amount in the validation group. The authors empirically created upper and lower cut off values for the shock index based on age. They compared the shock index based on age cut offs with major trauma as defined by the standardized triage assessment tool criteria.
The empirically derived age adjusted values had a sensitivity of 43.2% and a specificity of 79.4% for major trauma. The sensitivity of the pediatric shock index (PSI) in that same group was 33.9% with a specificity of 90.7%. The pediatric-adjusted shock index (SIPA) had a 37.4% sensitivity and 87.8% sensitivity for 4-16 year olds.
Shock index = (Heart Rate / Systolic BP)
Pediatric Shock Index (PSI)
For children age 1-12 years
SI > 1.55 - (0.5) x (age in years)
Patients with an elevated shock index had a 5.02 greater odds of major trauma in this study.
This study used age specific cut offs such as:
1 yr to < 3 years = lower limit of 0.73 and an upper limit of 1.40
(see article for a full table).
Patients with a shock index below the lower limit had a 1.55 greater offs of major trauma and patients with a shock index above the upper limit had a 3.97 greater risk of major trauma.
Bottom line: Shock index alone has a limited role in the identification of major trauma in children. Of these three methods for calculating/interpreting shock index, PSI seemed to do better.
Ramgopal S, Gorski JK, Chaudhari PP, Spurrier RG, Horvat CM, Macy ML, Cash RE, Stey AM, Martin-Gill C. Establishing thresholds for shock index in children to identify major trauma. Injury. 2024 Aug 23:111840. doi: 10.1016/j.injury.2024.111840. Epub ahead of print. PMID: 39198074.
Category: Neurology
Keywords: Stroke, ICH, Hypertension (PubMed Search)
Posted: 2/20/2025 by Nicholas Contillo, MD
Click here to contact Nicholas Contillo, MD
Multiple trials have aimed to assess the effect of blood pressure control in the prehospital setting for patients with suspected acute stroke. The INTERACT-4 trial was a multicenter, prospective, randomized, open-label, blind endpoint trial conducted in China, in which 2404 hypertensive patients with suspected acute stroke (based on FAST score >2, symptom onset <2h, SBP >150mmHg) were randomized to receive urapidil versus usual care in the prehospital setting. The primary outcome was modified Rankin score (mRs) distribution at 90 days. Overall, no significant difference in functional outcomes at 90 days were observed in the urapidil versus usual care groups (OR 1.00, 95% CI 0.87-1.15). However, when analyzed by stroke type, improved functional outcomes and lower rates of rebleeding were seen in patients with hemorrhagic stroke (46.5% of all enrolled patients), while worsened functional outcomes and mortality were seen in patients with ischemic stroke. These observations are consistent with standard practices of intensive blood pressure reduction in patients found to have ICH, versus the “permissive hypertension” approach to patients found to have cerebrovascular occlusion. The results of this trial are not practice-changing, but do highlight the importance of prompt stroke recognition, streamlined hospital workflows for expedited diagnostics (CT), and timely initiation of antihypertensive therapy in ICH patients.
Bottom line: Prehospital blood pressure reduction was not shown to improve clinical outcomes in hypertensive patients suspected to have acute undifferentiated stroke.
Li, G., Lin, Y., Yang, J., Anderson, C. S., Chen, C., Liu, F., Billot, L., Li, Q., Chen, X., Liu, X., Ren, X., Zhang, C., Xu, P., Wu, L., Wang, F., Qiu, D., Jiang, M., Peng, Y., Li, C., Huang, Y., … INTERACT4 Investigators (2024). Intensive Ambulance-Delivered Blood-Pressure Reduction in Hyperacute Stroke. The New England Journal of Medicine, 390(20), 1862–1872. https://doi.org/10.1056/NEJMoa2314741
Category: EMS
Keywords: cardiac arrest, epinephrine, ROSC (PubMed Search)
Posted: 2/19/2025 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
Previous studies have suggested that a single dose of epinephrine in out of hospital cardiac arrests compared to multiple dose protocols result in a similar survival to hospital discharge rate. This study aimed to see if single dose epinephrine compared to multiple doses improved survival in the subset of patients that were 1) in a shockable rhythm or 2) received bystander CPR.
This study looked at patients from 5 EMS systems in North Carolina before and after a protocol change from multiple dose epinephrine to single dose epinephrine in cardiac arrest. 1690 patients were included, 19.2% with a shockable rhythm and 38.9% who received bystander CPR.
The study found:
- Survival to hospital discharge was higher in the single dose epinephrine group who received bystander CPR
- Survival rates were similar in the single and multiple dose epinephrine groups for patients who were initially in shockable rhythms, in asystole/PEA and who did NOT receive bystander CPR.
Bottom Line: More studies are needed to support prehospital protocol changes.
George TS, Ashburn NP, Snavely AC, et al. Does Single Dose Epinephrine Improve Outcomes for Patients with Out-of-Hospital Cardiac Arrest and Bystander CPR or a Shockable Rhythm?. Prehosp Emerg Care. Published online May 21, 2024. doi:10.1080/10903127.2024.2348663
