Category: Pharmacology & Therapeutics
Keywords: Albuterol, Lactate (PubMed Search)
Posted: 4/10/2025 by Wesley Oliver
(Updated: 2/8/2026)
Click here to contact Wesley Oliver
Albuterol, a common bronchodilator used in the treatment of asthma and chronic obstructive pulmonary disease (COPD), can cause a surprising increase of lactate levels. The increase in lactate is usually mild to moderate (typically < 4 mmol/L) and transient. It does not necessarily indicate underlying sepsis, tissue hypoxia, or severe metabolic acidosis.
Mechanism:
Albuterol can cause a transient increase in lactate levels due to its beta-2 agonist effects, which promote glycogenolysis and increase anaerobic metabolism. This can result in elevated lactic acid production, even in the absence of tissue hypoxia or shock.
Timing:
This effect is typically seen within 30 minutes of albuterol administration and can persist for 1-2 hours after discontinuing treatment.
Monitoring:
If lactate levels are elevated in a patient receiving albuterol, consider the possibility of a pharmacologic cause rather than immediately assuming a more serious etiology like shock or severe metabolic disturbance.
Differentiating Causes of Elevated Lactate:
In a critically ill patient, elevated lactate can indicate hypoperfusion (e.g., septic shock, cardiogenic shock, or hypovolemic shock). However, when elevated lactate is associated with albuterol administration, the rise in lactate is often lower and resolves without intervention.
Management:
If albuterol-induced lactate elevation is suspected, continue with supportive care and monitor lactate trends. No specific treatment is necessary for the elevated lactate unless there are other concerning clinical findings that suggest a different underlying cause.
Conclusion:
In emergency settings, it's important to recognize that albuterol can cause a transient increase in lactate levels. Understanding this phenomenon can help avoid misdiagnosis and prevent unnecessary interventions in patients receiving albuterol therapy. Always correlate lactate levels with the broader clinical picture to guide management decisions.
Hockstein M, Diercks D. Significant Lactic Acidosis from Albuterol. Clin Pract Cases Emerg Med. 2018 Mar 14;2(2):128-131. doi: 10.5811/cpcem.2018.1.36024. PMID: 29849230.
Lewis LM, Ferguson I, House SL, Aubuchon K, Schneider J, Johnson K, Matsuda K. Albuterol administration is commonly associated with increases in serum lactate in patients with asthma treated for acute exacerbation of asthma. Chest. 2014 Jan;145(1):53-59. doi: 10.1378/chest.13-0930. PMID: 23949578.
Liedtke AG, Lava SAG, Milani GP, Agostoni C, Gilardi V, Bianchetti MG, Treglia G, Faré PB. Selective ß2-Adrenoceptor Agonists and Relevant Hyperlactatemia: Systematic Review and Meta-Analysis. J Clin Med. 2019 Dec 27;9(1):71. doi: 10.3390/jcm9010071. PMID: 31892109.
Maeda T, Paralkar J, Kuno T, Patrawalla P. Inhaled Albuterol Use and Impaired Lactate Clearance in Patients With Sepsis: A Retrospective Cohort Study. J Intensive Care Med. 2021 Mar;36(3):284-289. doi: 10.1177/0885066619901095. Epub 2020 Jan 22. PMID: 31964210.
Zitek T, Cleveland N, Rahbar A, Parker J, Lim C, Elsbecker S, Forred W, Slattery DE. Effect of Nebulized Albuterol on Serum Lactate and Potassium in Healthy Subjects. Acad Emerg Med. 2016 Jun;23(6):718-21. doi: 10.1111/acem.12937. Epub 2016 May 11. PMID: 26857949.
Category: Critical Care
Keywords: Catheter, flow rates, resuscitation (PubMed Search)
Posted: 4/9/2025 by Harry Flaster, MD
Click here to contact Harry Flaster, MD
Flow rates are, in theory, determined by Poiseuille’s Law, which states that the flow rate depends on fluid viscosity, pipe length, and the pressure difference between the ends of the pipe .
Of course we won’t be calculating this during a resuscitation! Nor would it be useful if we did: the equation assumes laminar flow, whereas turbulent flow is more likely. Nor is it practical to look up the viscosity of crystalloid/blood/plasma, which also dramatically impacts flow rates.
Instead, remember this equation: Larger + shorter = faster
And keep in mind the following:
In practice, our friends in Australia actually put common catheters to the test, and provided these helpful results:
Or, as a picture:
Note, these flow rates were achieved using crystalloid. Blood will be slower due to higher viscosity.
Category: Gastrointestional
Keywords: admission, abdominal pain (PubMed Search)
Posted: 4/9/2025 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
Do you ever tell your patients to “follow up with your primary care physician in 3-5 days”? How many of them actually do it? And does it make a difference?
Study Overview:
This study is a retrospective analysis of 28,085 adults (?20 years) presenting with acute abdominal pain (AAP) at 15 German emergency departments (EDs) in 2016.
Key Findings:
Hospitalization rate:
39.8% were admitted to the hospital from the ED.
Outpatient Care (OC) Before ED Visit:
33.9% had an OC visit within 3 days before their ED visit.
Of these, 48.6% were hospitalized.
Outpatient Care After ED Visit:
62.7% had OC follow-up within 30 days.
Factors Increasing Hospitalization Odds:
Age ?65 years: aOR 3.05
Prior OC: aOR 1.71
Male sex: aOR 1.44
In-Hospital Mortality:
3.1%
ED Re-visits Within 30 Days:
More likely in age ?65: aOR 1.32
Less likely with prior OC: aOR 0.37
Conclusion:
Acute abdominal pain in the ED is associated with high hospitalization and mortality rates, especially in older adults and those with prior outpatient visits. Prior outpatient contact is linked with both increased admission likelihood and reduced risk of ED re-visits, highlighting its complex role in care continuity. Improving outpatient care access and coordination may reduce ED burden and enhance outcomes for AAP patients.
While there are other factors to consider ie the health care system and its infrastructure, this does provide some interesting food for thought about what happens when we discharge patients.
Verleger K, Fischer-Rosinsky A, Möckel M, et al. Health care utilization of patients with acute abdominal pain before and after emergency department visits. Scand J Trauma Resusc Emerg Med. 2024;32(1):68. Published 2024 Aug 12. doi:10.1186/s13049-024-01237-7
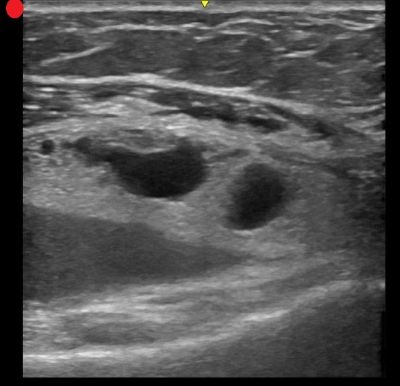
Category: Ultrasound
Keywords: POCUS; GI; Diverticulitis (PubMed Search)
Posted: 4/7/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
A recent systematic review and meta-analysis evaluated the diagnostic accuracy of ultrasound in detecting acute diverticulitis. The analysis included 12 studies with a total of 2,056 patients. Ultrasound demonstrated a sensitivity of 92.5% (95% CI: 86.9%–95.8%) and a specificity of 87.7% (95% CI: 75.7%–94.2%).
The most commonly used diagnostic criteria across the studies included:
Similar to prior research on POCUS for nephrolithiasis, these findings support a POCUS-first approach for patients at low risk for serious alternative diagnoses. Ultrasound is a great alternative for patients with contraindications to contrast-enhanced CT, such as those with contrast allergies.
As the authors state, while ultrasound may be effective in identifying acute diverticulitis and its complications, such as abscess, additional imaging with CT may still be required to assess the severity of complications.
Shokoohi H, Peksa GD, Hutchison A, Al Jalbout N, Montoya K, Westrick JC, Goldsmith A, Nazerian P, Gottlieb M. Ultrasound accuracy in acute diverticulitis: A systematic review and Meta-analysis. Am J Emerg Med. 2025 Mar 10;92:96-103. doi: 10.1016/j.ajem.2025.03.002.
Category: Gastrointestional
Keywords: Appendicitis, scoring, prediction, Alvarado Score (PubMed Search)
Posted: 4/6/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
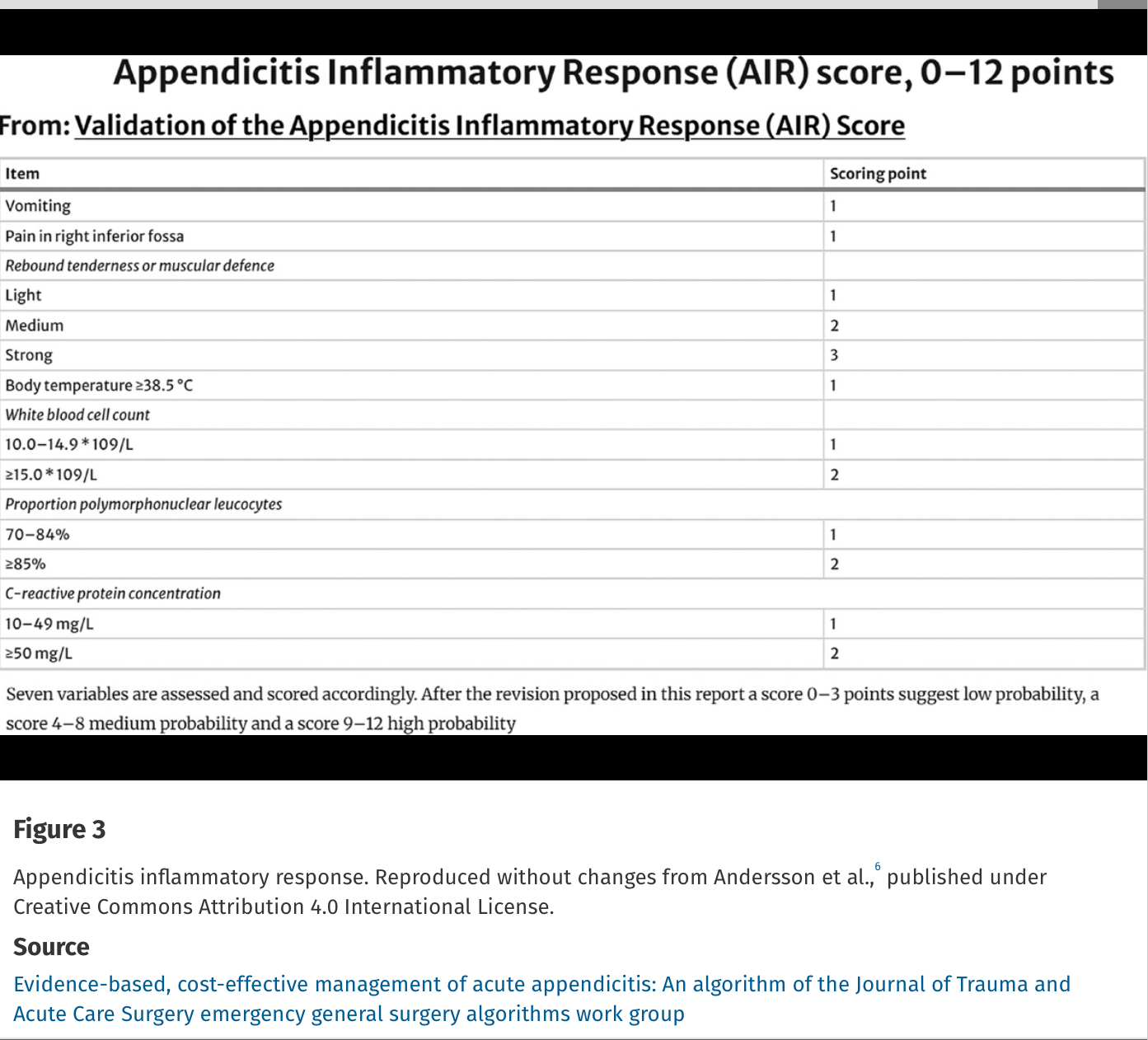
Missed appendicitis leading to rupture and peritonitis leads to morbidity, mortality, and malpractice claims. Part of a longer article looking at evaluation and management of appendicitis, these authors provide three scoring systems that can be used to identify appendicitis. Use of these scores can guide imaging and surgical consultation.
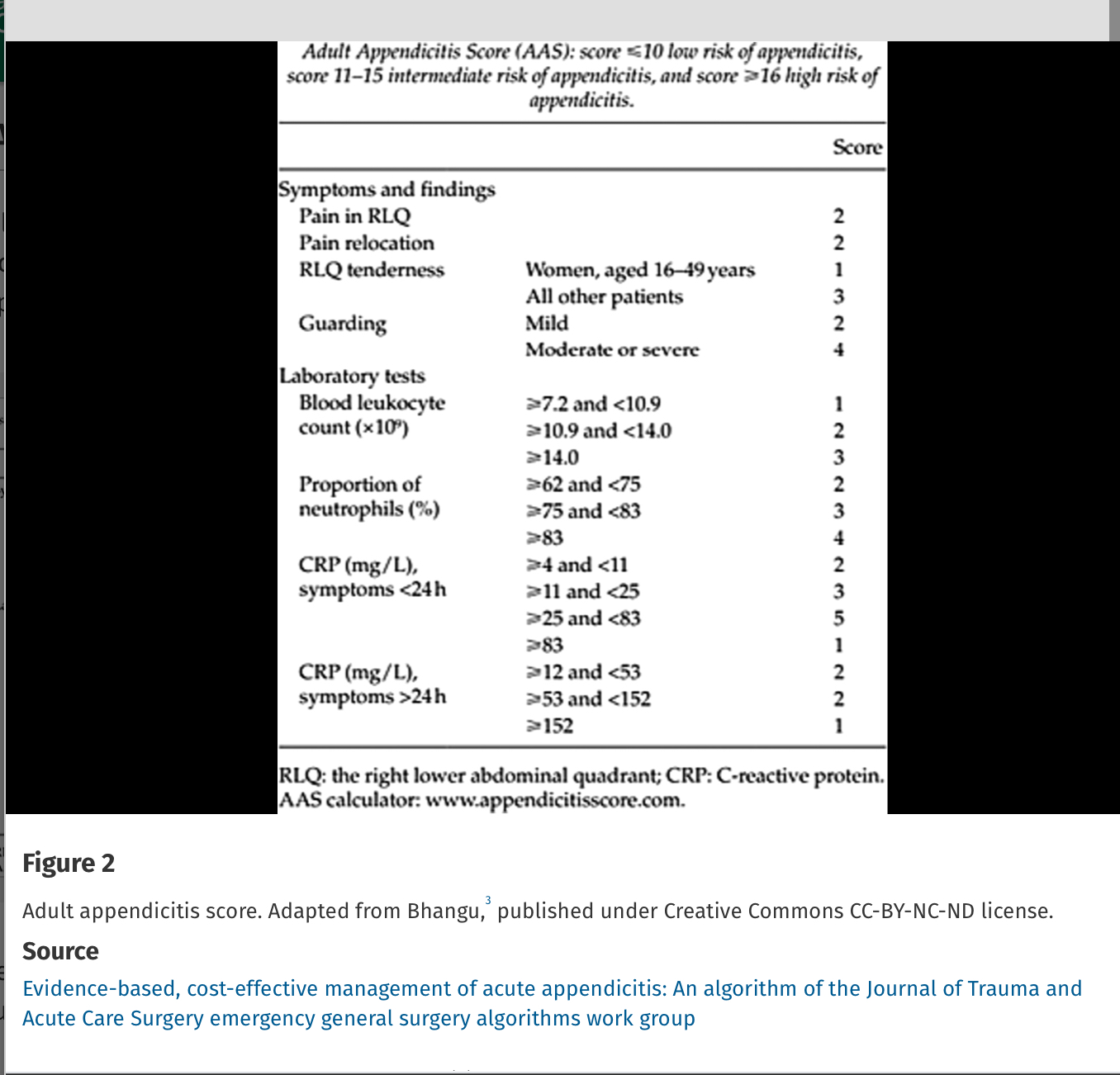
Alvarado Score: If a patient scores 1 to 4, the risk of appendicitis drops to 33%. If a patient scores >5, the risk of acute appendicitis is 66% or greater.
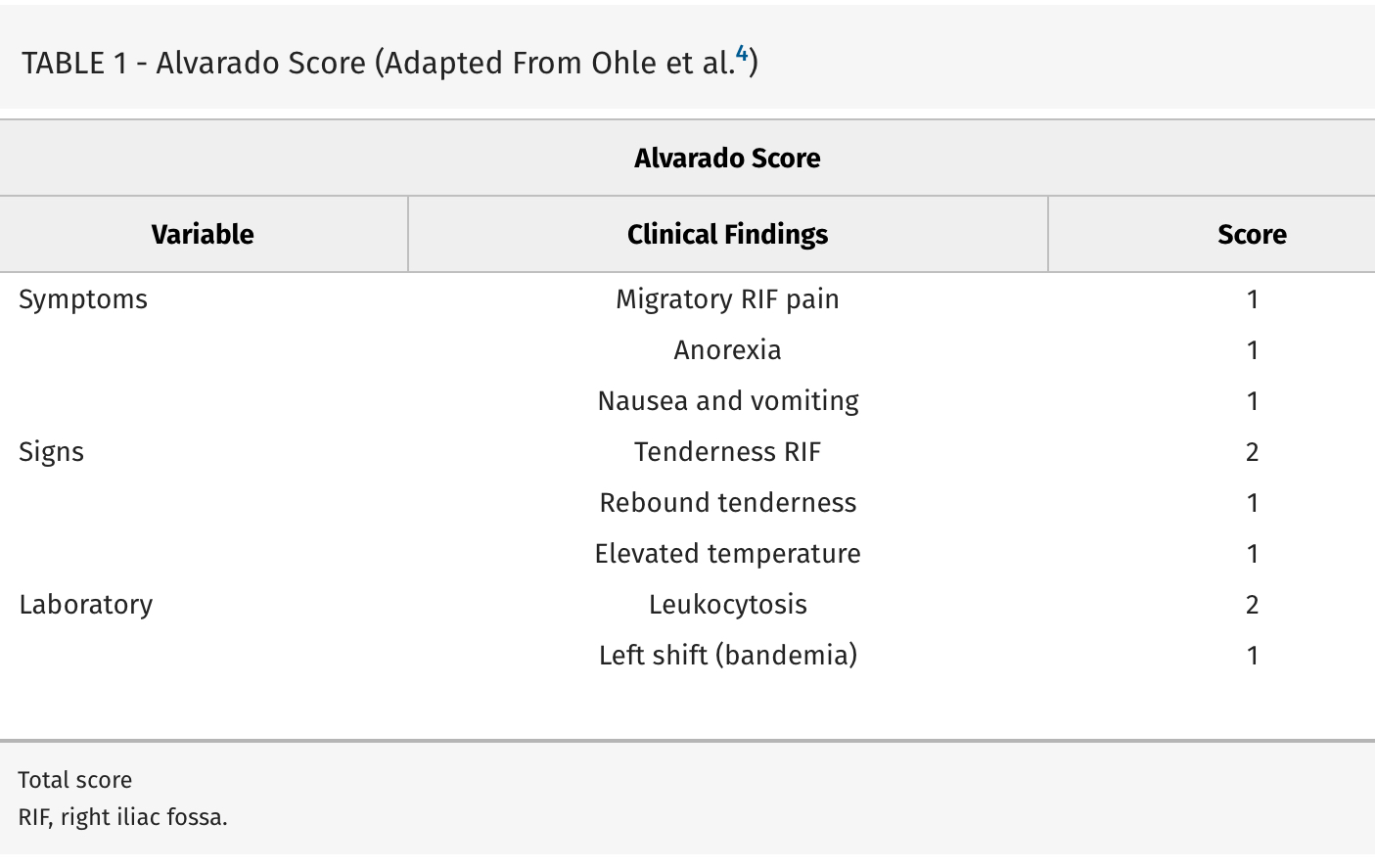
Evidence-based, cost-effective management of acute appendicitis: An algorithm of the Journal of Trauma and Acute Care Surgery emergency general surgery algorithms work group
Diaz, Jose J. MD, CPE, CNS, FACS, FCCM; Napolitano, Lena MD; Livingston, David H. MD; Costantini, Todd MD; Inaba, Kenji MD; Biffl, Walter L. MD; Winchell, Robert MD; Salim, Ali MD; Coimbra, Raul MD, PhD
Journal of Trauma and Acute Care Surgery 98(3):p 368-373, March 2025. | DOI: 10.1097/TA.0000000000004569
Category: Toxicology
Keywords: Toxicology, contaminate, opiate, stimulant (PubMed Search)
Posted: 4/5/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This study from Australia reminds us that what patients think they ingested isn’t always what they did ingest. A high percentage of “cocaine” and other stimulants was actually fentanyl or other opiates. The authors do a nice job referencing similar studies in the United States. Any overdose could be a mixed picture due to impure street drugs.
Emergency Medicine AustralasiaVolume 37, Issue 2 e70038
Original Research
Open Access
Peter Chisholm MBBS, B Med Sc, MPH, Jared Brown BPharm, MPH, Thanjira Jiranantakan MD, MPH, FAFPHM, FACOEM, Mary Ellen Harrod PhD, Catherine McDonald BSc, Una Cullinan BSc, Darren M Roberts MBBS, PhD, FRACP, FAChAM
First published: 03 April 2025
Category: Obstetrics & Gynecology
Keywords: HIV; perinatal transmission (PubMed Search)
Posted: 4/3/2025 by Michele Callahan, MD
(Updated: 2/8/2026)
Click here to contact Michele Callahan, MD
Perinatal HIV transmission in the U.S. can approach rates of <1% if appropriate interventions are offered to both pregnant individuals and their neonates.
However, a recently published case series evaluating hospitals in Maryland noted that there were 6 new cases of perinatal HIV transmission in 2022, compared with nationwide decreases and zero cases in the state of MD in 2021. Transmission was believed to be related to several issues: delayed entry to prenatal care, HIV diagnosis occurring in pregnancy (as opposed to pre-conception), adherence in the setting of hardships such as substance use, and delays in anti-retroviral therapy (ART) initiation during pregnancy.
How can we work to lower perinatal HIV transmission? Opportunities include the use of pre-exposure prophylaxis (PrEP), routine HIV testing in individuals of child-bearing age (especially if at high-risk of HIV acquisition), and rapid initiation of ART in pregnant individuals. As emergency physicians and providers, we are at the front line of assessing for these barriers and getting patients the resources they need to minimize perinatal transmission.
Griffith DC, Grant M, Koay WLA, Rakhmanina N, Powell AM, Agwu A. Increase in Cases of Perinatal HIV Transmission in Maryland in 2022. Pediatrics. 2024;154(5):e2023065371. doi:10.1542/peds.2023-065371
Category: Critical Care
Keywords: OHCA, cardiac arrest, refractory VT/VF, shockable, ventricular arrhythmia, amiodarone, lidocaine (PubMed Search)
Posted: 4/2/2025 by Kami Windsor, MD
(Updated: 2/8/2026)
Click here to contact Kami Windsor, MD
A 2023 retrospective cohort study comparing amiodarone to lidocaine for in-hospital cardiac arrests (IHCA) with refractory VT/VF found that use of lidocaine was associated with increased chance of ROSC, 24 hour survival, survival to discharge, and favorable neurologic outcome at hospital discharge.[1]
Now, a recent study comparing amiodarone to lidocaine in the pre-hospital setting for OHCA has found similar results. [2] Another retrospective cohort study using propensity score matching, they evaluated 23,263 adult patients with OHCA and defibrillation refractory VT/VF managed by 1700 EMS agencies.
Use of lidocaine was associated with greater odds of prehospital ROSC, fewer post-drug administration defibrillations, and greater odds of survival to discharge.
In comparison to earlier trials, these studies are some of the first demonstrating benefits to lidocaine use over amiodarone that reach statistical significance, but of course have all the limitations that come with retrospective studies and are not further analyzed in the context of etiologies for cardiac arrest or application of post-ROSC care.
Bottom Line: If you happen to be someone who reaches for amiodarone as your go-to, it may be time to start considering lidocaine.
Category: Infectious Disease
Keywords: JHR, syphillis, penicillin (PubMed Search)
Posted: 3/31/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
The Jarisch-Herxheimer reaction (JHR) is a non-specific set of symptoms (fever, malaise, worsened rash, hemodynamic instability, leukocytosis) seen after treating syphillis and other spirochete induced infections. In this study 1 in 4 patients treated with 2.4 million units of benzathine penicillin G developed a short lived JHR. Those who developed the reaction were more likely HIV negative, had secondary syphillis and had successful treatment at 6 months.
Dionne JA, Zhu C, Mejia-Galvis J, et al. Jarisch-Herxheimer Reaction After Benzathine Penicillin G Treatment in Adults With Early Syphilis: Secondary Analysis of a Randomized Clinical Trial. JAMA Netw Open. 2025;8(2):e2459490. doi:10.1001/jamanetworkopen.2024.59490
Category: Administration
Posted: 3/29/2025 by Brian Corwell, MD
(Updated: 3/30/2025)
Click here to contact Brian Corwell, MD
A recent cohort study performed by the NCAA and US Department of Defense looked at NCAA athletes and military cadets who had suffered a concussion.
The study included 1661 NCAA athletes and military cadets, mean age was about 18 years, and 45% were women.
In these groupings, 813 people took over-the-counter pain relievers after their concussion and 848 people did not take any pain relievers.
Analgesics used included medications such as acetaminophen or NSAIDs such as ibuprofen.
Acetaminophen (n = 600), NSAIDs (n = 75), and those taking both (n = 78).
1) 50% recovery
Category: Trauma
Keywords: ASA score, trauma, head injury, prognostication (PubMed Search)
Posted: 3/29/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
The American Society of Anesthesia score was an independent predictor of 90-day mortality as
well as low functional status at one year in 720 patients presenting to a single center with
moderate to severe brain injury. When used in conjunction with other prognosticating tools such
as the Trauma and Injury Severity Score, it increased the prognostic value of these scales.
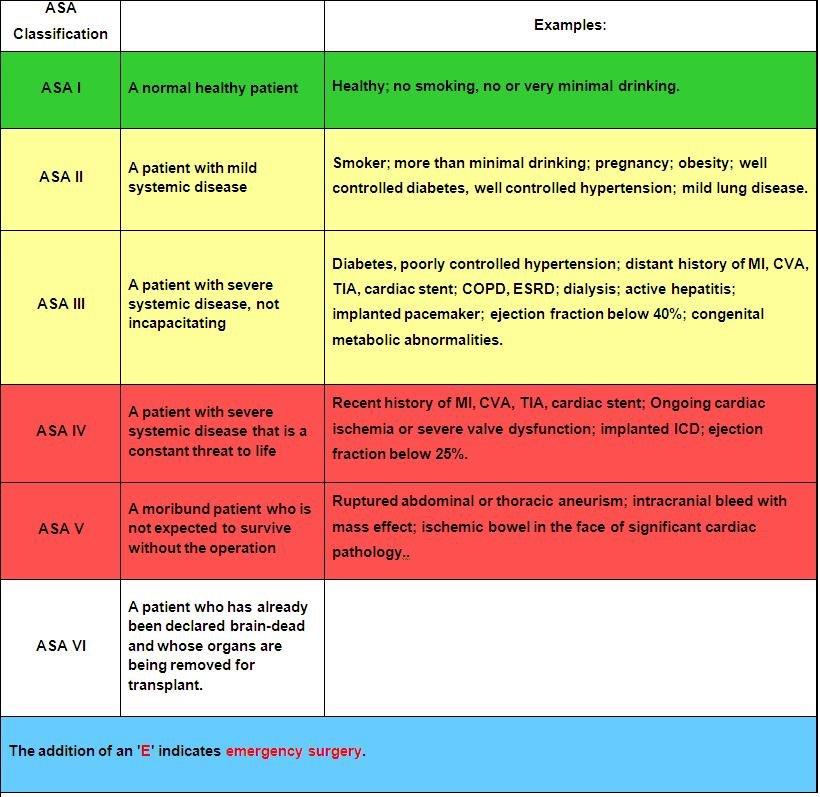
1. Kiwanuka, O., Lassarén, P., Fletcher-Sandersjöö, A. et al. ASA score is an independent
predictor of 1-year outcome after moderate-to-severe traumatic brain injury. Scand J Trauma
Resusc Emerg Med 33, 25 (2025). https://doi.org/10.1186/s13049-025-01338-x
2.Statement on ?ASA Physical Status Classification System.
Category: Neurology
Keywords: Cerebral Venous Sinus Thrombosis, CVST, Low-Molecular-Weight Heparin, Unfractionated Heparin (PubMed Search)
Posted: 3/27/2025 by Nicholas Contillo, MD
Click here to contact Nicholas Contillo, MD
Anticoagulation is the mainstay of treatment of cerebral venous sinus thrombosis, irrespective of whether associated venous hemorrhage is present. Anticoagulant selection is variable, with physicians opting for unfractionated heparin (UFH) about 72% of the time in one international study. However, recent evidence favors the use of low-molecular-weight heparin (LMWH), with meta-analytic data showing trends towards lower mortality rates and improved functional outcomes in LMWH cohorts. UFH is often viewed more favorably due to the ability to rapidly discontinue the infusion in the event of major bleeding; however, risk of major bleeding complications were actually found to be lower in patients treated with LMWH compared to UFH. Further, LMWH has many pharmacological and practical benefits compared to UFH, including more predictable pharmacokinetics, reduced risk of heparin-induced thrombocytopenia (HIT), lack of need for frequent aPTT monitoring, ease of administration (daily subcutaneous injection), and ease of transition to outpatient therapy.
Takeaway: Consider LMWH (1.5mg/kg subcutaneously once daily) as first-line treatment for CVST in patients with acceptable renal function.
Category: Administration
Keywords: Team building, belonging, team dynamics, emergency physicians, emergency nurses (PubMed Search)
Posted: 3/25/2025 by Mercedes Torres, MD
(Updated: 3/26/2025)
Click here to contact Mercedes Torres, MD
Better teamwork creates better outcomes in emergency medicine. This study investigated how communication practices between physicians and nurses in the ED influence team dynamics and the sense of belonging to the healthcare team.
Methods: 38 emergency physicians and emergency nurses from EDs within a single metropolitan area participated in focus groups.
Positive Influences on Team Belonging:
Negative Influences on Team Belonging:
The findings emphasize the importance of fostering positive communication practices to enhance team dynamics, cohesiveness, and overall well-being within ED healthcare teams.
Phillips J, Jones D. Qualitative Study of Dynamics, Camaraderie, and Belonging Among Emergency Physicians and Nurses. J Emerg Med. 202569doi:10.1016/j.jemermed.2024.08.011
Category: Critical Care
Keywords: community acquired pneumonia; CAP; corticosteroids; mortality; adjuvant therapy (PubMed Search)
Posted: 3/25/2025 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
If you watch those medical drama (House MD, ER, Grey’s Anatomy, Resident…), the doctors and residents are always faced with a dilemma – is it a rare autoimmune disorder or is it an infection? They are worried that if they give steroid to a patient with infections, that would kill the patients.
Well, it might not be the case for Community acquired pneumonia.
A meta-analysis of randomized control trials involving 3224 patients to look into the efficacy of adjuvant corticosteroids for CAP. The authors assessed the heterogeneity of treatment effect (different groups should have different response to treatment).
For patients who were anticipated to benefit (those who had CRP > 240 mg/L), corticosteroids were associated with lower odds of 30-day mortality (OR 0·43 [0·25–0·76], p=0·026).
When stratifying by risk, there was no significant effect between those with Pneumonia Severity Index (PSI) I-III versus those with PSI IV-V.
However, corticosteroids increased odds of hyperglycemia (OR 2·50 [95% CI 1·63–3·83], p<0·0001), odds of hospital readmissions (1·95 [1·24–3·07], p=0·0038)
Discussion:
There were different regiments for corticosteroids in the included studies. However, hydrocortisone appeared to be more effective than other corticosteroids.
Furthermore, the time intervals for treatment is still debatable. The data suggested that the ideal treatment is within 24 hours of hospital admission, but patients can still benefit from treatment in up to 48 hours.
A response-dependent treatment is also recommended: 8 days or 14 days, depending on how patients respond to treatment by day 4.
Conclusion:
Adjuvant treatment with corticosteroids among hospitalized patients with CAP was significantly associated with reduction of 30-day mortality. The treatment effect, however, varied according to patients CRP concentrations at baseline.
Smit JM, Van Der Zee PA, Stoof SCM, Van Genderen ME, Snijders D, Boersma WG, Confalonieri P, Salton F, Confalonieri M, Shih MC, Meduri GU, Dequin PF, Le Gouge A, Lloyd M, Karunajeewa H, Bartminski G, Fernández-Serrano S, Suárez-Cuartín G, van Klaveren D, Briel M, Schönenberger CM, Steyerberg EW, Gommers DAMPJ, Bax HI, Bos WJW, van de Garde EMW, Wittermans E, Grutters JC, Blum CA, Christ-Crain M, Torres A, Motos A, Reinders MJT, Van Bommel J, Krijthe JH, Endeman H. Predicting benefit from adjuvant therapy with corticosteroids in community-acquired pneumonia: a data-driven analysis of randomised trials. Lancet Respir Med. 2025 Mar;13(3):221-233. doi: 10.1016/S2213-2600(24)00405-3. Epub 2025 Jan 29. PMID: 39892408.
Category: Trauma
Keywords: Trauma, rib fracture, multimodal (PubMed Search)
Posted: 3/23/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Controlling pain from rib fractures impacts morbidity and mortality. Over the past decade there has been a focus on decreasing opiate use and approaching this painful condition in a multimodal way. “The multimodal approach utilizes a combination of delivery methods including oral, parenteral, and regional single-shot or catheter-based techniques. Oral medications include opioids, non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, skeletal muscle relaxants, alpha-2 agonists, mood stabilizers, and neuropathic pain medications. Parenteral medications encompass most of the oral options in addition to ketamine and lidocaine. Regional anesthesia includes epidural analgesia (EA), paravertebral blocks, intercostal blocks, and myofascial plane blocks.”
This study is a single center in Canada looking at medication used for patients admitted over 10 years with rib fractures along with demographics, injury severity and outcomes. The authors concluded:
“Although multimodal pain management strategies have improved over time, a large proportion of patients, even among those with flail chest, still do not receive multimodal pain management. Elderly patients, at highest risk of adverse outcomes, were less likely to receive multimodal pain management strategies and should be the target of performance improvement initiatives.”
Naveed A, Adams-McGavin RC, Ladha K, et al. A 10-year review of pain management practices for rib fractures at a lead trauma hospital: Are we adopting all multimodal pain management strategies? Trauma. 2025;27(1):18-23. doi:10.1177/14604086231198764
Category: Trauma
Keywords: Whole blood, trauma (PubMed Search)
Posted: 3/22/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Achieving faster homeostasis in trauma patients leads to lower mortality, less coagulopathy, and lower total blood volume transfusion requirements. This study looked at time to achieving homeostasis as defined by transfusion requirements as well as laboratory measurements in critically ill trauma patients who either received whole blood or component therapy transfusion as part of their resuscitation. Those receiving whole blood achieved statistically significant faster homeostasis.
Chipman, Amanda M. MD; Luther, James F. MA; Guyette, Francis X. MD, MPH; Cotton, Bryan A. MD; Cannon, Jeremy W. MD; Schreiber, Martin A. MD; Moore, Ernest E. MD; Namias, Nicholas MD, MBA; Minei, Joseph P. MD; Yazer, Mark H. MD; Vincent, Laura MS, RN; Cotton, Abigail L. BS, MPH; Agarwal, Vikas MD; Brown, Joshua B. MD, MSc; Leeper, Christine M. MD; Neal, Matthew D. MD; Forsythe, Raquel M. MD; Wisniewski, Stephen R. PhD; Sperry, Jason L. MD, MPH; the SWAT Study Group. Early achievement of hemostasis defined by transfusion velocity: A possible mechanism for whole blood survival benefit. Journal of Trauma and Acute Care Surgery 98(3):p 393-401, March 2025. | DOI: 10.1097/TA.0000000000004507
Category: Pediatrics
Keywords: CPR, pediatric cardiac arrest, termination, TOR (PubMed Search)
Posted: 3/21/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
This was a retrospective analysis of pediatric cardiac arrests that occurred out of hospital in Japan, where no pediatric termination of resuscitation is allowed. 1007 arrests were included. Patients that were placed on ECMO were excluded. This study included both medical and traumatic arrests looking at a primary outcome of 1 month moderate or better neurological disability. CPR time for both EMS and the hospital prior to ROSC were included. Bystander CPR was not included in these calculations. Possible downtime prior to CPR was not taken into consideration.
Overall, less than 1% of pediatric patients exhibited one-month moderate disability or better neurological outcome when total CPR duration is more than 64 minutes.
Yasuda M, Amagasa S, Kashiura M, Yasuda H, Uematsu S. Duration of prehospital and in-hospital cardiopulmonary resuscitation and neurological outcome in paediatric out-of-hospital cardiac arrest. Emerg Med J. Published online October 15, 2024. doi:10.1136/emermed-2023-213730
Category: EMS
Keywords: TOR, pediatric cardiac arrest (PubMed Search)
Posted: 3/19/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
A few states have pediatric out of hospital termination of resuscitation protocols. This study used CARES data to create a termination protocol that was not only linked to ROSC, but also to neurological outcomes. This study only included medical arrests.
21240 children were included in the study where 2326 patients survived to hospital discharge. A total of 1894 survived with a favorable neurological outcome. The criteria developed for pediatric TOR in this study had a specificity of 99.1% and a PPV of 99.8% for patient death. Another set of criteria had a 99.7% specificity and PPV of 99.9% for predicting death or survival with poor neurological outcome.
TOR criteria of death consisted of:
unwitnessed arrest
asystole
arrest not due to drowning or electrocution
no sustained ROSC
TOR criteria of death or survival with poor neurological outcome:
unwitnessed arrest
asystole
arrest not due to drowning or electrocution
no sustained ROSC
no bystander CPR
Bottom line: Pediatric termination of resuscitation in the out of hospital setting can be appropriate under the right set of conditions.
Shetty P, Ren Y, Dillon D, et al. Derivation of a clinical decision rule for termination of resuscitation in non-traumatic pediatric out-of-hospital cardiac arrest. Resuscitation. Published online September 18, 2024. doi:10.1016/j.resuscitation.2024.110400
Category: Ultrasound
Keywords: POCUS; MSK; fracture (PubMed Search)
Posted: 3/17/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
On ultrasound, lipohemarthrosis—the presence of blood and fat in the joint cavity—is a key clinical indicator of an intra-articular fracture.
Lipohemarthrosis appears as three distinct layers near the joint line.
Salerno A. Lipohemarthrosis. Floating fat in an intra-articular fracture. Visual Journal of Emergency Medicine. 2022, 26:101236.
Category: Trauma
Keywords: kidney trauma, grading, (PubMed Search)
Posted: 3/16/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Unless a patient is unstable, renal injuries are managed non-operatively or endovascularly. Here is the
2025 Kidney Injury Grading Scale from AAST.
AAST AIS
Grade Severity Imaging Criteria
I 2 –Subcapsular hematoma <3.5 cm without active bleeding
– Parenchymal contusion without laceration
II 2 – Parenchymal laceration length <2.5 cm
– HRD <3.5 cm without active bleeding
III 3 – Parenchymal laceration length ?2.5 cm
– HRD ?3.5 cm without active bleeding
– Partial kidney infarction
– Vascular injuries without active bleeding
– Laceration extending into urinary collecting system and/or urinary extravasation
IV 4 – Active bleeding from kidney
– Pararenal extension of hematoma
– Complete/near-complete kidney infarction without active bleeding
– MFK without active bleeding
– Complete/near-complete ureteropelvic junction disruption
V 5 – Main renal artery or vein laceration or transection with active bleeding
– Complete/near-complete kidney infarction with active bleeding
– MFK with active bleeding
Keihani, Sorena MD, MSCI; Tominaga, Gail T. MD; Matta, Rano MD; Gross, Joel A. MD; Cribari, Chris
MD; Kaups, Krista L. MD, MSc; Crandall, Marie MD, MPH, FACS; Kozar, Rosemary A. MD; Werner,
Nicole L. MD, MS; Zarzaur, Ben L. MD; Coburn, Michael MD, FACS; Myers, Jeremy B. MD, FACS. Kidney
organ injury scaling: 2025 update. Journal of Trauma and Acute Care Surgery 98(3):p 448-451, March
2025. | DOI: 10.1097/TA.0000000000004509
