Category: Trauma
Keywords: Mussed injuries, trauma, tertiary survey, (PubMed Search)
Posted: 7/27/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
This paper looked at the literature regarding missed injuries in trauma patients. Missed injuries was defined as an injury discovered after the patient was discharged. Most of the missed injuries and causes are not novel but are worthy of remembering.
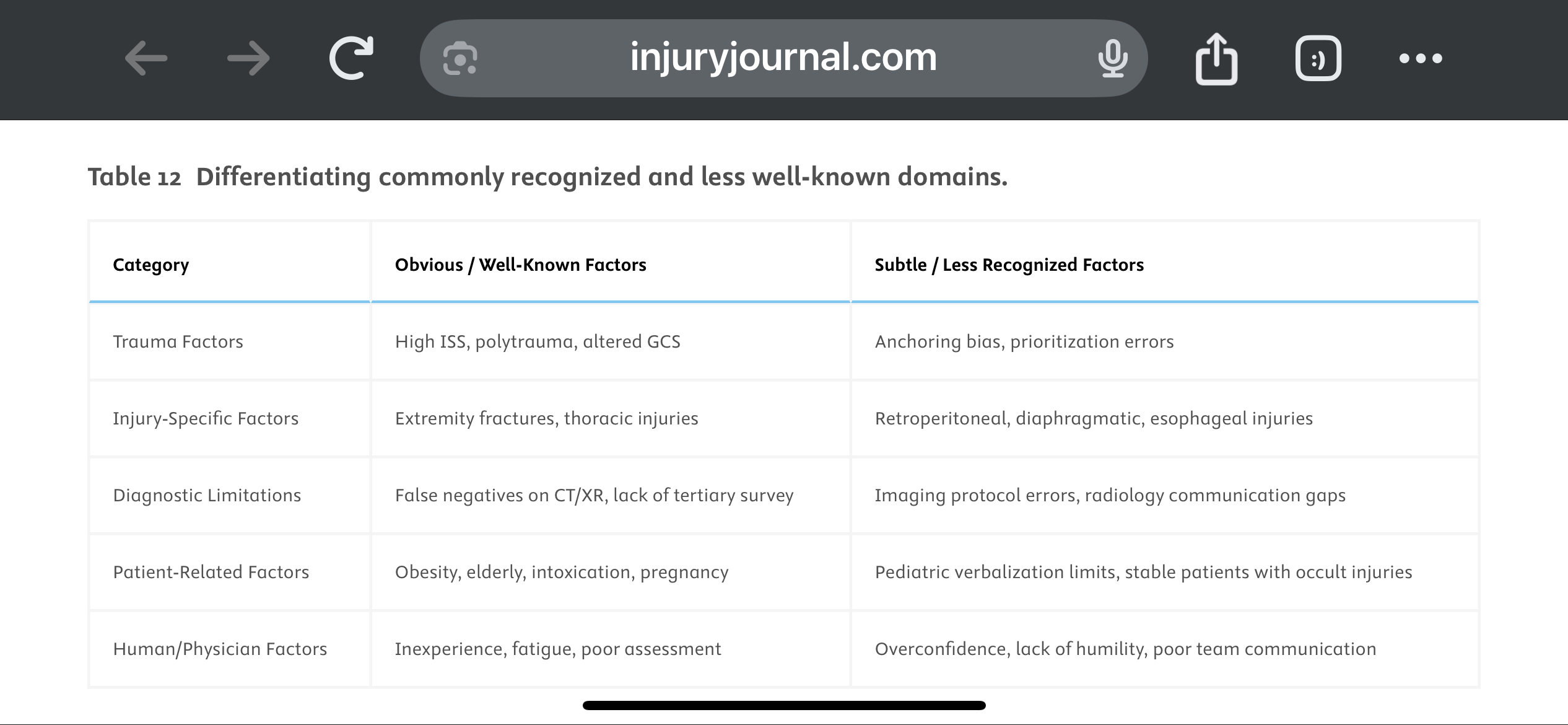
They suggest a Trauma Tertiary Survey helps prevent missed injury. “Tertiary Survey (TTS), which includes a thorough in-hospital re-examination and a review of diagnostic investigations within the first 24 h, has been shown to significantly reduce the occurrence of missed injuries (1–9 %) in severe trauma patients found after a primary and secondary survey.” This concept is similar to a discharge time out in emergency medicine where all data is reviewed, viral signals are confirmed normal and a team discharge is performed.
The paper offers these suggestions to avoid missed injuries:
1.
Standardize Tertiary Trauma Surveys (TTS).
2.
Be Cognizant of Cognitive Biases (e.g., Anchoring Bias).
3.
Repeat Imaging When Clinically Indicated.
4.
Use Protocolized Imaging Techniques (CT/MRI).
5.
Ensure Radiology-Trauma Communication.
6.
Prioritize High-Risk Populations.
7.
Implement Peer Review or Double-Check Systems.
8.
Encourage a Culture of Collaboration and Humility.
9.
Limit Provider Fatigue and Overload.
10.
Create Tailored Checklists for Subtle Injuries.
Vieira, Lucas Fontenelle et al.
Injury, Volume 56, Issue 8, 112600
Category: Orthopedics
Posted: 7/27/2025 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
A recent study investigated the impact of pain management education counseling on postoperative opioid consumption.
Patients were randomly assigned to receive opioid limiting perioperative pain management education and counseling (intervention group) with instructions to take opioids “only as a last resort if the pain became unbearable.”
The control group received instructions to take opioids as needed for “severe pain” to” stay ahead of the pain.”
The primary outcome was the total morphine equivalents (TME) consumed in the 3 months after surgery.
Secondary outcomes included pain measured with the Numeric Rating Scale, sleep quality, opioid prescription refills, and patient satisfaction.
121 patients with a mean age of 29 years.
Both groups were told about potential adverse effects of opioids and were advised of alternative methods to control pain such as over-the-counter acetaminophen and ibuprofen.
60 patients in the treatment group consumed a mean of 46 mg TME versus 63.6 mg TME in the control group ( p < 0.001). There was no difference in the average score on the numeric rating scale in the first 14 days between groups. There was no significant difference in refill prescriptions between the groups. Sleep quality and patient satisfaction was also similar between groups.
Over 1/3 of patients in the intervention group took no opioids at all after surgery. In contrast, 9 out of 10 patients in the control group used all prescribed opioids after surgery.
Conclusion: Opioid limiting pain management education and counseling reduces opioid consumption without a change in reported pain. There may be a role for pain management education and counseling in emergency department patients in whom opiates are prescribed…similar to this study in perioperative orthopedic patients.
Packer, Jonathan D. MD1,a; Aneizi, Ali MD1; Honig, Evan L. BS1; Kaveeshwar, Samir MD1; Schneider, Matheus MD1; Leong, Natalie L. MD1; Meredith, Sean J. MD1; O’Hara, Nathan N. PhD, MHA1; Henn, R. Frank III MD1. Perioperative Opioid Counseling for Patients Undergoing Anterior Cruciate Ligament Reconstruction: A Randomized Controlled Trial. The Journal of Bone and Joint Surgery 107(14):p 1546-1552, July 16, 2025
Category: Critical Care
Posted: 7/23/2025 by William Teeter, MD
Click here to contact William Teeter, MD
Secondary analysis of a multicenter, prospective, observational study ICE-CRASH study in Japan including adult patients admitted with moderate-to-severe accidental hypothermia between 2019 and 2022.
Some structural generalizability (median age 81 years!) issues with this study but well done overall.
Authors undertook some rather complex modeling to predict outcomes related to rapid rewarming, showing that “the rewarming rate and predicted probability of each outcome increased significantly up to 3°C/hr, but when the rewarming rate exceeded 3°C/hr, the predicted probability of each outcome was almost constant.”
Suggests that for those with severe hypothermia that an initially rapid rate of up to 3C/hr is a good target for a ceiling, but above this may be associated with less favorable risk:benefit ratio. Benefit in moderate hypothermia was not as clear.
Conclusion: The mode of rewarming in severe hypothermia should still be based on local protocols and capabilities (e.g. external, intravascular, extracorporeal rewarming) but the rate of rewarming up to 3C/hr is associated with better outcomes.
Category: Administration
Keywords: Patient Experience, Patient Satisfaction, CMS Evaluation, ED Evaluation, (PubMed Search)
Posted: 7/22/2025 by Mercedes Torres, MD
(Updated: 7/23/2025)
Click here to contact Mercedes Torres, MD
Shout out to UMEM alum Diane Kuhn, MD, PhD as the first author of this recent publication…
She and her colleagues examined the factors that contribute to ED patient experience scores, uncovering several which are not considered in the current CMS evaluative framework. See the editor's (our very own Stephen Schenkel, MD, MPP) capsule summary below:
What is already known on this topic? Medicare plans nationally standardized Emergency Department (ED) Patient Experience scores (ED
CAHPS) to allow comparison across sites.
What question this study addressed. Are there clinical and operational ED characteristics for which ED patient experience scores ought to be adjusted?
What this study adds to our knowledge. Based on 58,622 ED visits from one system, patients arriving in pain were less satisfied and those receiving radiologic studies had a positive experience.
How this is relevant to clinical practice. Influences on patient satisfaction are multifactorial and many are outside the control of the ED. Comparing EDs based on patient experience is complex and prone to misinterpretation.
As the authors point out, If patients placed in a hallway bed have a more negative experience simply due to the location in the department, or patients arriving in pain have a more negative experience regardless of ED care, then some EDs will face more challenges than others in achieving optimal patient experiences.
The current CMS evaluative framework may inherently disadvantage certain EDs, including those with limited physical space relative to their patient volumes, such as safety-net hospitals, or those that care for a high proportion of patients experiencing chronic pain. Is this fair? Does it reflect what CMS is trying to evaluate? Are there alternatives?
Kudos to Dr. Kuhn on her insightful publication and Dr. Schenkel for his expert editing!
Kuhn, Diane et al. Use of Hallway Beds, Radiology Studies, and Patients in Pain on Arrival to the Emergency Department Are Associated With Patient Experience, Annals of Emergency Medicine, Volume 86, Issue 2, 150 - 157. https://doi.org/10.1016/j.annemergmed.2024.11.020
Category: Ultrasound
Keywords: POCUS; Pulmonary Embolism; Cardiac Ultrasound; Doppler (PubMed Search)
Posted: 7/21/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
Early Systolic Notching and Pulmonary Embolism
A prospective multicenter study conducted across four academic emergency departments in Turkey evaluated the diagnostic accuracy of early systolic notching (ESN) in emergency department patients. Among the 183 patients included, 52.5% were diagnosed with pulmonary embolism (PE), while 19.7% exhibited the ESN finding. ESN demonstrated a sensitivity of 34% (95% CI: 25–45%) and a specificity of 97% (95% CI: 90–99%) for PE. Sensitivity increased to 69% in patients classified as high or intermediate-high risk. Overall, ESN exhibits moderate to high specificity but low sensitivity, consistent with other sonographic signs of PE. Notably, ESN may also be present in patients with chronic thromboembolic disease secondary to prior pulmonary hypertension.
How to Obtain ESN
To detect ESN, acquire a parasternal short axis view at the base of the heart to visualize the right ventricular outflow tract and pulmonic valve. Position the pulse wave Doppler gate just proximal to the pulmonic valve, with the cursor traversing the outflow tract. ESN is characterized by a sharp systolic spike with a notch, followed by a dome-shaped waveform
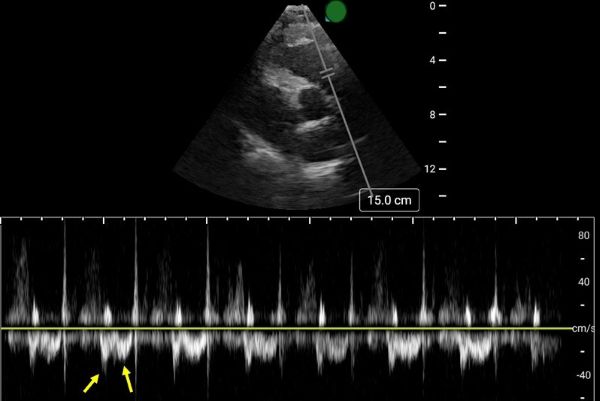
Aslaner MA, Karbek Akarca F, Aksu ?H, Yazla M, Can Ö, Ku? G, Çelik A, Özkan S, ?bze S, Yamano?lu A, Yaz?c? MM, Yürüktümen Ünal A, Demircan A. Diagnostic Accuracy of Early Systolic Notching in Pulmonary Embolism. J Ultrasound Med. 2022 Mar;41(3):637-644. doi: 10.1002/jum.15744.
Category: Trauma
Keywords: TBI, management, parameters (PubMed Search)
Posted: 7/20/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Outcomes in traumatic brain injury are improved when physiologic homeostasis is achieved as soon as possible after injury. Here are the American College of Surgeons’ recommendations. Note SBP over 110 and a hemoglobin over 7. A study looking at a more liberal transfusion target showed worse ARDS and no mortality benefit.
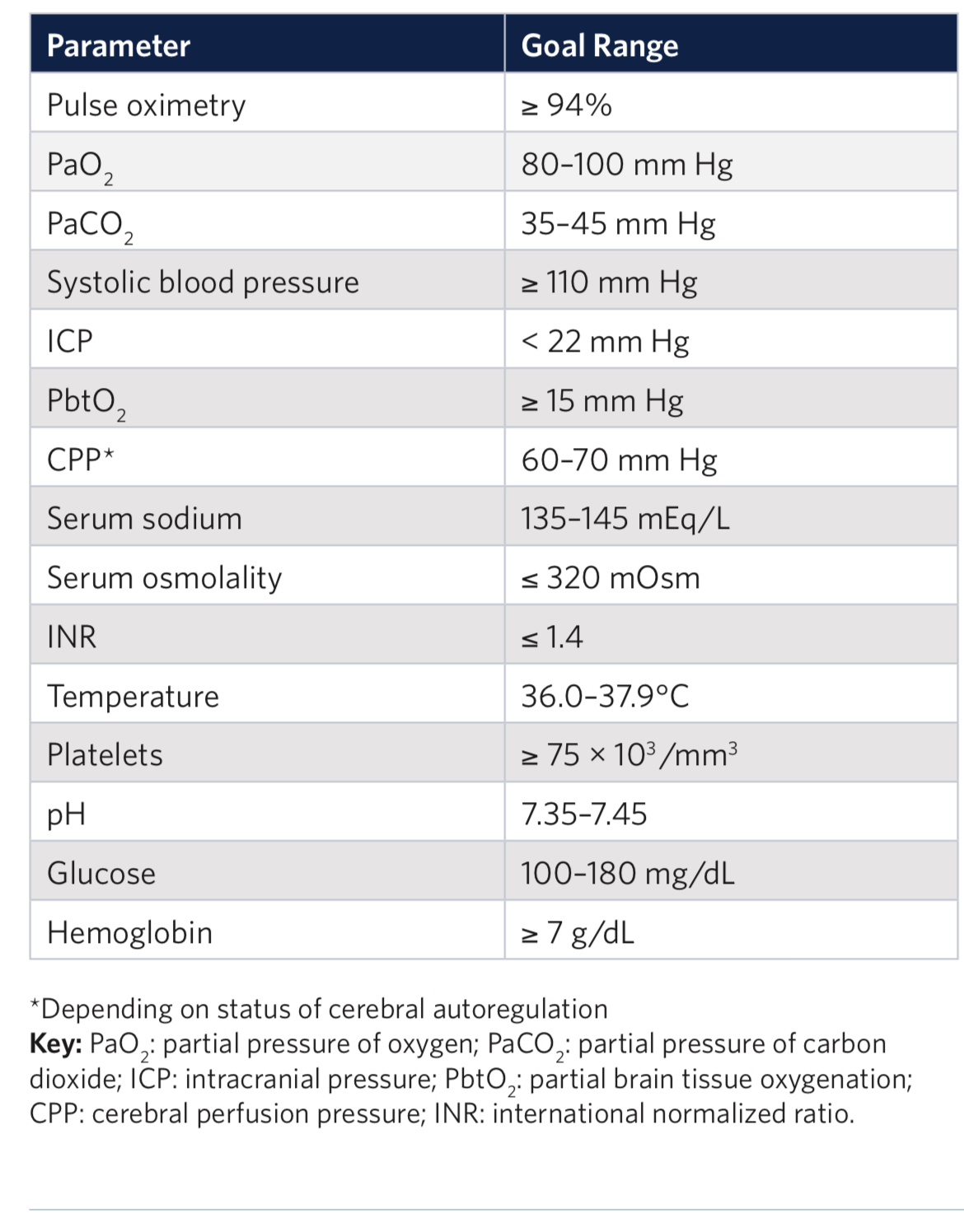
2. Liberal or Restrictive Transfusion Strategy in Patients with Traumatic Brain Injury
Authors: Alexis F. Turgeon, M.D. https://orcid.org/0000-0001-5675-8791, Dean A.Fergusson, Ph.D., Lucy Clayton, M.Sc., Marie-Pier Patton, M.Sc., Xavier Neveu, M.Sc., Timothy S. Walsh, M.D., Annemarie Docherty, M.D., Ph.D., +48 , for the HEMOTION Trial Investigators on behalf of the Canadian Critical Care Trials Group, the Canadian Perioperative Anesthesia Clinical Trials Group, and the Canadian Traumatic Brain Injury Research Consortium*
June 13, 2024N Engl J Med 2024;391:722-735DOI: 10.1056/NEJMoa2404360VOL. 391 NO. 8
Category: Pediatrics
Keywords: trauma, blood, pediatric (PubMed Search)
Posted: 7/18/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Trauma is a leading cause of death in pediatric patients. The Pediatric Traumatic Hemorrhagic Shock Consensus Conference Recommendations have stated that blood products are better than crystalloid and recommend the use of low titer type O whole blood (LTOWB) over individual components for pediatric traumatic resuscitation.
This study used the Trauma Quality Improvement Program Database to look at 1122 pediatric patients (< 18 years) over a 3 year period to retrospectively examine the impact of the ratio of whole blood and blood products given during the resuscitation of these patients. When at least 30% of the blood products delivered within the first 4 hours of resuscitation were low titer O whole blood, survival improved at the 6, 12 and 24 hour time mark.
The authors concluded that the observed survival benefit supports the greater availability and use of LTOWB during pediatric trauma resuscitation.
Fisher AD, April MD, Yazer MH, Wright FL, Cohen MJ, Maqbool B, Getz TM, Braverman MA, Schauer SG. An analysis of the effect of low titer O whole blood (LTOWB) proportions for resuscitation after trauma on 6-hour and 24-hour survival. Am J Surg. 2024 Nov;237:115900. doi: 10.1016/j.amjsurg.2024.115900. Epub 2024 Aug 13. PMID: 39168048.
Category: EMS
Keywords: survival, ROSC, trauma, arrest (PubMed Search)
Posted: 7/16/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
This was a multicenter retrospective cohort study over 6 years at 7 level one and two trauma centers.
1631 patients who had out of hospital traumatic cardiac arrest were included. The majority of the patients were adults, female, suffered penetrating trauma (64%) and were in a non-shockable rhythm. Prehospital epinephrine was given to 54% of patients.
Overall, survival to hospital discharge was lower in the epinephrine group (5% vs 16%). In the penetrating trauma subgroup, there was no statistically significant survival difference in patients who received epinephrine and those who did not.
EMS jurisdictions should examine their trauma arrest protocols and consider excluding the use of epinephrine. Several states, such as Maryland, have already removed epinephrine from the trauma arrest protocol.
Witt CE, Shatz DV, Robinson BRH, Campion EM, Shapiro ML, Bui EH, Meizoso JP, Dorlac WC. Epinephrine in Prehospital Traumatic Cardiac Arrest-Life Saving or False Hope? Prehosp Emerg Care. 2025 Feb 12:1-9. doi: 10.1080/10903127.2025.2461283. Epub ahead of print. PMID: 39889233.
Category: Critical Care
Keywords: Hypotension, Shock, Mean Arterial Pressure, Vasopressors, Elderly Patients, Geriatrics (PubMed Search)
Posted: 7/15/2025 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Following up Dr. Flint's pearl from the other day, the largest study to date looking at a lower Mean Arterial Pressure (MAP) target in elderly ICU patients is the “65” Trial, published in JAMA in 2020. This trial compared a MAP target of 60-65 to the usual goal of >65, in critically ill patients age 65 and older. It included 2,455 patients in 65 ICUs in the UK, and found no difference between the groups.
Bottom Line: Although most intensivists still target a MAP > 65 regardless of patient age, you do have some evidence to support you if you want to target 60-65 in patients over age sixty-five. However, there are some important limitations (well outlined in the PulmCrit article linked below), and therapy should always be optimized to the patient and markers of end organ perfusion.
Category: Geriatrics
Keywords: Geriatric, critical care, vasopressors. (PubMed Search)
Posted: 7/12/2025 by Robert Flint, MD
(Updated: 7/14/2025)
Click here to contact Robert Flint, MD
An open label pragmatic study in 29 Japanese hospitals randomized septic shock patients over age 65 to either a high (MAP 80-85) or control (65-70) group. They then looked at all cause 90 day mortality. The study was stopped early due to a significantly higher percentage of mortality in the higher MAP group.
The study isn’t blinded and is only done in one country, however it does raise the question of what is the ideal MAP for older septic shock patients.
Endo A, Yamakawa K, Tagami T, Umemura Y, Wada T, Yamamoto R, Nagasawa H, Takayama W, Yagi M, Takahashi K, Kojima M, Narita C, Kazuma S, Takahashi J, Shiraishi A, Todani M, Nakane M, Nagata T, Tanaka S, Yokokawa Y, Takahashi K, Ishikita H, Hisamune R, Sasaki J, Muramatsu KI, Sonobe H, Minami K, Hoshi H, Otomo Y; OPTPRESS trial investigators. Efficacy of targeting high mean arterial pressure for older patients with septic shock (OPTPRESS): a multicentre, pragmatic, open-label, randomised controlled trial. Intensive Care Med. 2025 May;51(5):883-892. doi: 10.1007/s00134-025-07910-4. Epub 2025 May 13. PMID: 40358717; PMCID: PMC12130109.
Category: Trauma
Keywords: Pedestrian, fatality, injury, cyclist (PubMed Search)
Posted: 7/12/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This study from Great Britain compared fatalities for pedestrians and cyclist struck by motor vehicles based on vehicle body type. They found :
“We conclude that in Great Britain, being hit by an SUV as opposed to a passenger car increases injury severity among pedestrians and cyclists, with the strongest effect in children.“
Goodman, Anna, Phil Edwards, and Anthony A. Laverty. 2025. “Do Sports Utility Vehicles (SUVs) Cause More Severe Injuries to Pedestrians and Cyclists than Passenger Cars, in the Case of a Crash? Findings from Great Britain, 2004-2023.” Findings, July. https:/?/?doi.org/?10.32866/?001c.141647.
Category: Orthopedics
Posted: 7/12/2025 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
https://the.emergencyphysio.com/wp-content/uploads/knee-lip-lateral.png
What do you see?
There is no clear fracture line
Much like ice floats on water, fat also floats on water/blood because it is less dense.
An intra-articular fracture may allow for blood and fat to exit the bone marrow and settle in the joint space.
This is called a lipohemarthrosis.
Best seen with a cross-table horizontal lateral view x-ray.
Go back to the image and examine the supra patellar pouch.
Most commonly seen in the knee in presence of a tibial plateau fracture.
Seen in approximately 1/3rd of tibial plateau fractures
If you see this without a clear fracture, consider CT of knee which can help detect the hidden fracture.
Remember the DDx of knee hemarthrosis with negative plain films:
Meniscal tear, ligament tear (usually ACL), patellar dislocation and osteochondral fracture.
Except for meniscal tearing (>6h) these other pathologies cause rapid onset swelling (<2h).
Category: Critical Care
Keywords: Sedation, propofol, dexmedetomidine, RASS (PubMed Search)
Posted: 7/8/2025 by Zachary Wynne, MD
Click here to contact Zachary Wynne, MD
The presence of an endotracheal tube by itself does not mandate sedation and many patients require no sedatives while intubated in the ICU. However, patients intubated in the emergency department usually require initial sedation while still paralyzed from RSI. Sedation can also help facilitate procedures and imaging in critically ill patients during initial management.
Current literature has found increased mortality and length of ventilator requirement in oversedated ED patients. The target sedation level for the general population remains a goal RASS (Richmond Agitation-Sedation Scale) of 0 to -1. Society of Critical Care Medicine guidelines from early 2025 recommend dexmedetomidine over propofol as the preferred sedative for light sedation and reducing delirium risk in intubated critically ill patients. A recent trial re-examined other clinical outcomes between these two common sedative agents.
A2B Randomized Clinical Trial - JAMA 2025
Clinical Question: Does alpha 2 adrenergic receptor agonist sedation (dexmedetomidine or clonidine) reduce duration of mechanical ventilation in mechanically ventilated patients compared to a propofol based regimen (usual care)?
Where: 41 UK ICU’s from December 2018 to October 2023
Who: 1438 adults receiving mechanical ventilation for less than 48 hours, receiving propofol and opioid for sedation/analgesia, expected to require mechanical ventilation for greater than 48 hours
Intervention: protocol driven sedation to reach a RASS score of -2 to +1 (either dexmedetomidine, clonidine, or propofol). Of note, propofol could be added to achieve deeper sedation goal if deemed necessary by care team.
Outcomes:
Bottom Line:
While either dexmedetomidine or propofol, with appropriate use of opiates for pain management, are appropriate agents in non-paralyzed mechanically-ventilated patients, propofol may be a more appropriate choice in patients with greater agitation while boarding in the emergency department. However, close attention is needed to avoid the overly deep analgosedation associated with increased mortality. Maintain a goal RASS of 0 to -1 with frequent re-evaluation of your ICU boarders.
Walsh TS, Parker RA, Aitken LM, McKenzie CA, Emerson L, Boyd J, Macdonald A, Beveridge G, Giddings A, Hope D, Irvine S, Tuck S, Lone NI, Kydonaki K, Norrie J, Brealey D, Antcliffe D, Reay M, Williams A, Bewley J, Creagh-Brown B, McAuley DF, Dark P, Wise MP, Gordon AC, Perkins GD, Reade MC, Blackwood B, MacLullich A, Glen R, Page VJ, Weir CJ; A2B Trial Investigators. Dexmedetomidine- or Clonidine-Based Sedation Compared With Propofol in Critically Ill Patients: The A2B Randomized Clinical Trial. JAMA. 2025 Jul 1;334(1):32-45. doi: 10.1001/jama.2025.7200. PMID: 40388916; PMCID: PMC12090071.
Lewis K, Balas MC, Stollings JL, et al. A focused update to the clinical practice guideline for the prevention and management of pain, anxiety, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2025 Mar 1;53(3):e711-e727.
Stephens RJ, Ablordeppey E, Drewry AM, Palmer C, Wessman BT, Mohr NM, Roberts BW, Liang SY, Kollef MH, Fuller BM. Analgosedation Practices and the Impact of Sedation Depth on Clinical Outcomes Among Patients Requiring Mechanical Ventilation in the ED: A Cohort Study. Chest. 2017 Nov;152(5):963-971. doi: 10.1016/j.chest.2017.05.041. Epub 2017 Jun 21. PMID: 28645462; PMCID: PMC5812748.
Category: Ultrasound
Keywords: POCUS, MSK, finger injuries, nerve blocks (PubMed Search)
Posted: 7/7/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
Digital nerve blocks are commonly used to provide anesthesia for finger injuries such as lacerations and dislocations. However, the procedure can be painful, as it often requires multiple injections into sensitive areas.
A recent single-center, unblinded randomized study compared the subjective discomfort and analgesic efficacy of traditional digital nerve blocks with ultrasound-guided peripheral nerve blocks. The study included 106 patients, with 53 in each group.
Results showed that patients in the peripheral nerve block group reported higher satisfaction rates. They also experienced less pain during the initial injection and longer-lasting analgesia compared to those who received digital nerve blocks. While digital blocks had a faster onset of anesthesia, they were associated with a higher rate of block failure.
Chororia, Samata et al. Dorsal Digital Nerve Block vs. Ultrasound-Guided Selective Peripheral Nerve Block for Finger Analgesia: A Randomized Controlled Study. Journal of Emergency Medicine. Article in Press. doi: 10.1016/j.jemermed.2025.05.005.
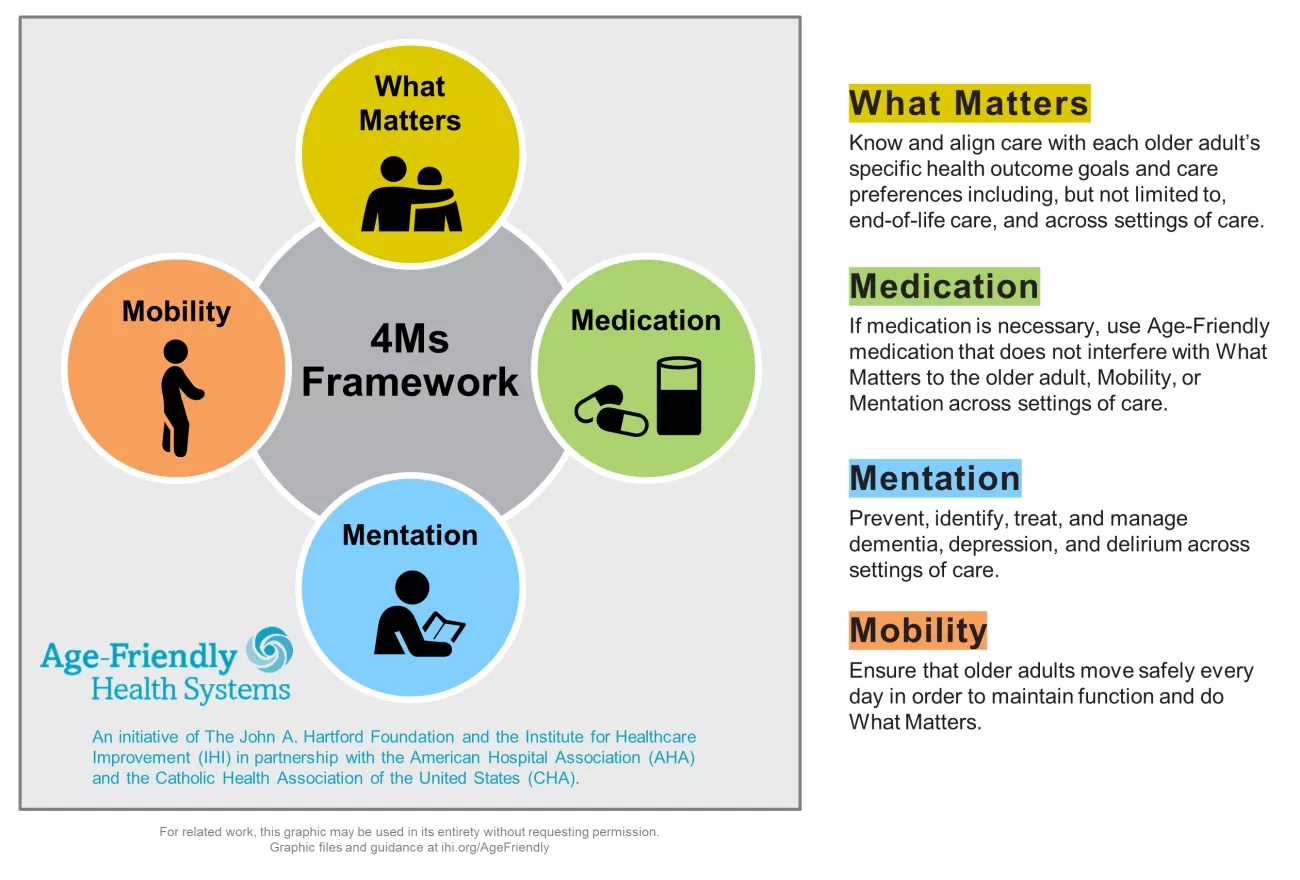
Category: Geriatrics
Keywords: Age friendly, geriatric, healthcare, quality improvement (PubMed Search)
Posted: 7/6/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In mid-2024 the Center for Medicare and Medicaid Services introduced a new quality measure entitled Age Friendly Hospital Measure. The initial phase went into effect 1/1/25. It is built around programs from the American College of Surgeons, the American College of Emergency Physicians as well as the Institute for Healthcare Improvement (IHI). It is modeled around the IHI’s 4M Framework.
Category: Trauma
Keywords: Shock index, transfusion, hypotension (PubMed Search)
Posted: 7/5/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
These authors looked at 5958 trauma patients arriving at their trauma center with a systolic blood pressure greater than 90. They calculated shock index (heart rate /sbp) for all of these and then looked at who received a blood transfusion within one hour of arrival. 211 patients received blood in that time frame. “Patients were stratified by SI using the following thresholds: ? 0.7, > 0.7 to 0.9, > 0.9 to 1.1, > 1.1 to 1.3, and > 1.3.”
“A main effect was observed for shock index with increased risk for required transfusion for patients with admission shock index >0.7 (P < 0.001). In comparison to shock index of ? 0.7, odds ratios were 2.5(1.7 - 3.8), 8.2(5.4 - 12.2), 24.9(15.1 - 41.1), 59.0(32.0 - 108.6) for each categorical increase in SI.”
Lin TM, Memon AM, Reeson EA, Tolan GC, Low TM, Kupanoff KM, Huang DD, Jones MD, Czarkowski BR, Soe-Lin H, Bogert JN, Weinberg JA. Shock index identifies compensated shock in the 'Normotensive' trauma patient. Injury. 2025 May 8:112419. doi: 10.1016/j.injury.2025.112419. Epub ahead of print. PMID: 40379507.
Category: Trauma
Keywords: facial fracture, transfer, guidelines (PubMed Search)
Posted: 6/29/2025 by Robert Flint, MD
(Updated: 7/2/2025)
Click here to contact Robert Flint, MD
Based on a review of 511 patients transferred to a level one trauma center for evaluation of facial fractures, this group developed the Facial Fracture Transfer Guidelines. they found that over half of the patients transferred to them did not require intervention and were discharged within 6 hours. These guidelines are meant to decrease unneeded transfers yet provide appropriate care to those with traumatic facial injuries.
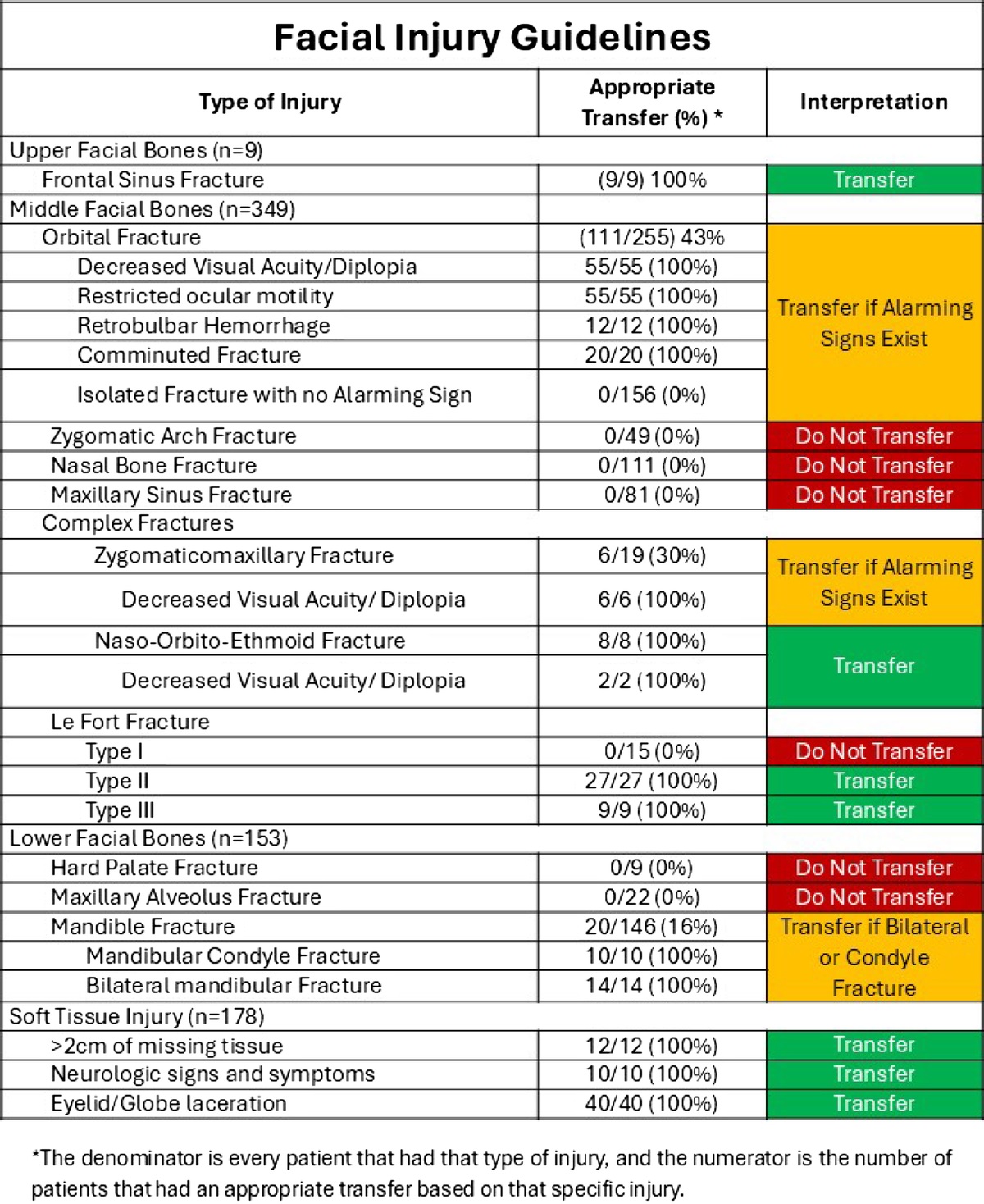
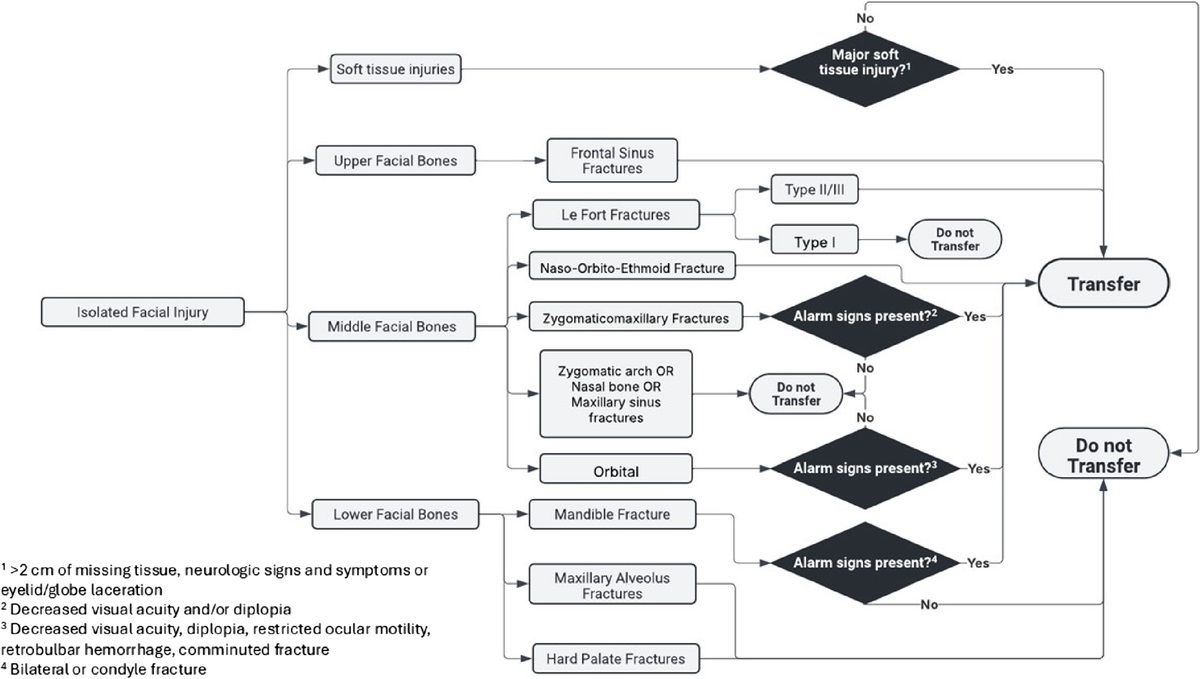
Castillo Diaz, Francisco MD; Anand, Tanya MD, MPH, FACS; Khurshid, Muhammad Haris MD; Kunac, Anastasia MD, FACS; Al Ma'ani, Mohammad MD; Colosimo, Christina DO, MS, FACS; Hejazi, Omar MD; Ditillo, Michael DO, FACS; Magnotti, Louis J. MD, MS, FACS; Joseph, Bellal MD, FACS. Look me in the face and tell me that I needed to be transferred: Defining the criteria for transferring patients with isolated facial injuries. Journal of Trauma and Acute Care Surgery ():10.1097/TA.0000000000004651, May 9, 2025. | DOI: 10.1097/TA.0000000000004651
Category: Critical Care
Posted: 7/1/2025 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
When To Initiate RRT in the Critically Ill Patient
Barbar SD, Wald R, Quenot JP. Acute kidney injury: when and how to start renal replacement therapy. Intensive Care Med. 2025;51:1172-1175.
Category: Trauma
Keywords: facial fracture, Le Fort, orbital fracture (PubMed Search)
Posted: 6/29/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
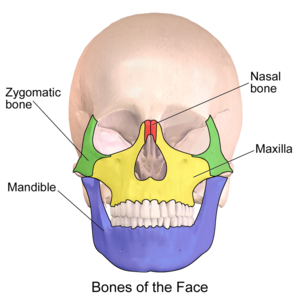
Most common facial fracture is the nasal fracture followed by the zygomatic arch fractures.
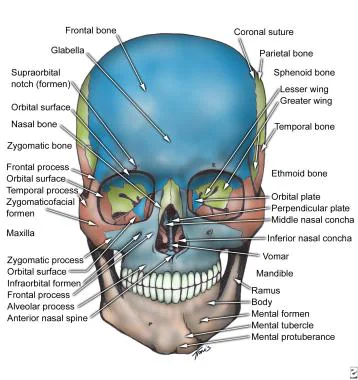
Le Fort Classification of facial fractures/facial stability. The higher the number, the more unstable.
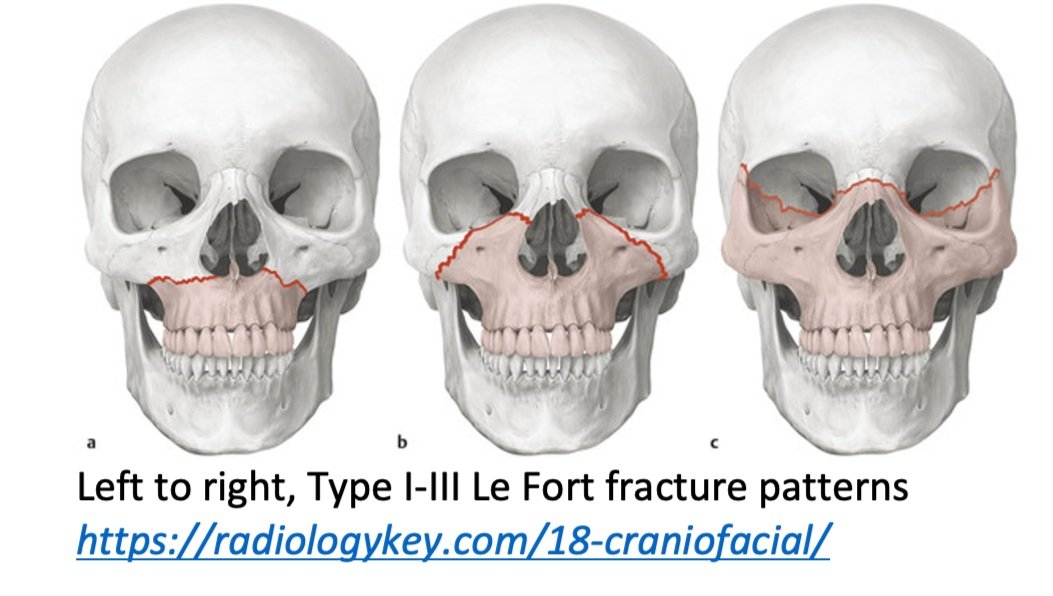
Orbital blow out fractures may entrap the ocular muscles leading to eye immobility in various directions.
Category: Orthopedics
Posted: 6/28/2025 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Haglund’s deformity
Calcaneal bony growth at the Achilles insertion
Also known as a “pump bump”
Risks: Tight & rigid shoes. Shoes with a hard heel counter. High arches. Tight Achilles tendon. Repetitive heel stress (jumping). Genetically prone bone structures.
Most common in woman between the ages of 15 and 35. Wearing heels. Runners.
Hx: Heel pain and tenderness with a noticeable bump at back of heel. Worse with walking and with certain footwear.
PE: Swelling and redness around bony prominence.
Pain and tenderness in the posterior heel, especially when pressure is applied.
Imaging: Excessive traction and abnormal biomechanics lead to insertional calcifications and bone spurs.
Over time, an exostosis may develop at posterior superior calcaneus as shown in the attached film.

Tx: Physical therapy and orthotics that alter heel height in shoe.
Surgery for chronic cases.
