Category: Critical Care
Keywords: ventilation ineffective-trigger double-trigger (PubMed Search)
Posted: 6/24/2025 by Cody Couperus-Mashewske, MD
Click here to contact Cody Couperus-Mashewske, MD
Patient-ventilator dyssynchrony is a sign of a disagreement between the patient's breathing and the ventilator's settings. Recognizing and fixing it is a critical skill to prevent lung injury and improve comfort. Ineffective triggering and double-trigger are two common types of dyssynchrony.
The patient tries to take a breath, but they are too weak to trigger the ventilator. This is the most common type of dyssynchrony. It causes increased work of breathing and discomfort.
Look for a small dip in the pressure waveform and a simultaneous scoop out of the expiratory flow waveform that is not followed by a delivered breath.
Troubleshooting options:
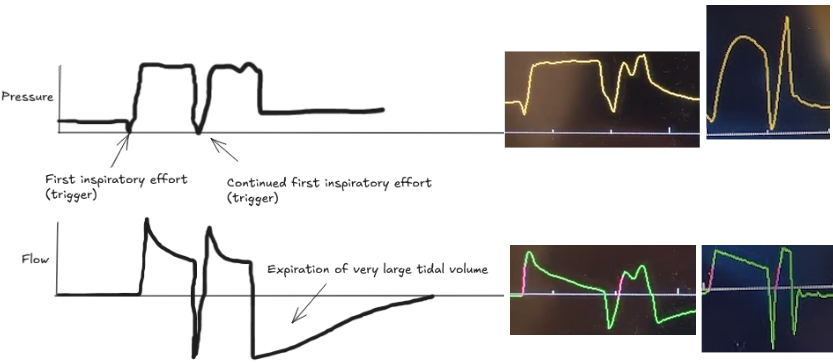
The patient's own breath outlasts the ventilator's set inspiratory time (Ti), causing one patient effort to trigger two stacked breaths. This results in delivery of large tidal volumes, risking lung injury (volutrauma).
Look for two consecutive breaths on the ventilator screen without a full exhalation in between.
Troubleshooting options:
Dyssynchrony means the ventilator settings do not match the patient's needs. Watch the waveforms to diagnose the mismatch, then either adjust the ventilator or treat the underlying problem.
Thille, A. W., Rodriguez, P., Cabello, B., Lellouche, F., & Brochard, L. (2006). Patient-ventilator asynchrony during assisted mechanical ventilation. Intensive care medicine, 32, 1515-1522.
Blanch, L., Villagra, A., Sales, B., Montanya, J., Lucangelo, U., Luján, M., ... & Kacmarek, R. M. (2015). Asynchronies during mechanical ventilation are associated with mortality. Intensive care medicine, 41, 633-641.
Category: Critical Care
Posted: 4/22/2025 by Cody Couperus-Mashewske, MD
Click here to contact Cody Couperus-Mashewske, MD
This large RCT compared High-Flow Nasal Oxygen (HFNO) against Noninvasive Ventilation (NIV) via face mask in 5 types of Acute Respiratory Failure (ARF): non-immunocompromised hypoxemia, immunocompromised hypoxemia, COPD with acidosis, acute cardiogenic pulmonary edema (ACPE), and COVID-19.
Bottom Line:
RENOVATE suggests HFNO might be a reasonable, more comfortable initial choice for non-immunocompromised hypoxemic ARF or COVID-19 ARF. However, exercise caution using HFNO first-line for COPD exacerbations with acidosis or immunocompromised hypoxemic ARF due to conflicting analyses and potential harm signals. The signal for HFNO benefit in ACPE is intriguing but needs confirmation before changing practice. Close monitoring for failure and timely escalation are essential regardless of the initial noninvasive strategy.
High-flow nasal oxygen vs noninvasive ventilation in patients with acute respiratory failure: the RENOVATE randomized clinical trial RENOVATE Investigators and the BRICNet Authors, Maia IS, Kawano-Dourado L, et al. JAMA. Published online December 10, 2024. doi:10.1001/jama.2024.26244
Category: Critical Care
Posted: 2/18/2025 by Cody Couperus-Mashewske, MD
Click here to contact Cody Couperus-Mashewske, MD
Arterial lines are essential tools in managing critically ill patients, but it is frustrating when they are not working as expected. It can be hard to tell when an unexpected waveform or pressure reflects the patient's physiology versus a problem with the line. Recognizing common issues and systematic troubleshooting will optimize your hemodynamic monitoring.
Types of arterial line problems
Troubleshooting Steps
By following these steps, you can systematically identify whether waveform or pressure abnormalities are due to technical issues or true patient physiology.
Category: Critical Care
Keywords: VExUS, IVC, POCUS, Venous Congestion (PubMed Search)
Posted: 12/10/2024 by Cody Couperus-Mashewske, MD
Click here to contact Cody Couperus-Mashewske, MD
The Venous Excess Ultrasound (VExUS) exam integrates IVC, portal, hepatic, and renal vein findings to assess venous congestion and guide management, such as diuresis, in critically ill patients.
Technique:
Tips:
Interpretation:
Sometimes when other clinical information is contradictory, having the extra data point of the VExUS exam can be extremely useful to determine the best plan for a patient. Practice looking for the portal/hepatic veins and getting the waveforms on patients with a CLEAR clinical picture of venous congestion, then practice on more difficult cases.
Assavapokee, T., Rola, P., Assavapokee, N. et al. Decoding VExUS: a practical guide for excelling in point-of-care ultrasound assessment of venous congestion. Ultrasound J 16, 48 (2024). https://doi.org/10.1186/s13089-024-00396-z
Category: Critical Care
Keywords: vascular access, micropuncture kits, procedures (PubMed Search)
Posted: 10/15/2024 by Cody Couperus-Mashewske, MD
Click here to contact Cody Couperus-Mashewske, MD
Getting reliable venous and arterial access is crucial when resuscitating critically ill patients. These lines can be difficult due to patient and situation specific variables.
Micropuncture kits contain a 21-gauge echogenic needle, a stainless-steel hard shaft/soft-tip wire, and a 4 Fr or 5 Fr sheath and introducer. The micropuncture kit offers several advantages that can help overcome difficult situations:
To use a micropuncture kit, gain vessel access with the needle and wire, railroad the sheath and introducer into the vessel, remove the wire, then remove the introducer. Now you have a 4 Fr or 5 Fr sheath in the vessel. This is typically used to introduce a normal central line wire.
For arterial lines, you can place them directly over the wire without dilation. Keep in mind that the 4 Fr sheath (1.3 mm OD) and 5 Fr sheath (1.7 mm OD) are larger than a typical arterial line catheter (18g = 1.27 mm OD). If you dilate then you will cause hematoma.
Find out where your department stores micropuncture kits and get familiar with their components. While it adds an extra step to the procedure, it could make the difference between securing the line or not.
Montrief, T., Ramzy, M., & Long, B. (2021). Micropuncture kits for difficult vascular access. The American journal of emergency medicine.
Category: Critical Care
Keywords: Euglycemic DKA (PubMed Search)
Posted: 8/20/2024 by Cody Couperus-Mashewske, MD
Click here to contact Cody Couperus-Mashewske, MD
Euglycemic DKA (eDKA) is a medical emergency requiring prompt attention. It is caused by an imbalance of insulin and glucagon leading to ketone accumulation (1-3). In addition to typical risk factors for DKA, those for eDKA include SGLT-2 inhibitor use and pregnancy, with 30% of DKA cases in pregnancy presenting euglycemic (4, 5).
eDKA presents with an anion gap metabolic acidosis, ketosis/ketonuria, & blood glucose less than 250 mg/dL.
Diagnosis requires ruling out other causes of anion gap metabolic acidosis, including toxic ingestions.
The cornerstone of eDKA management is ensuring enough dextrose to allow needed insulin administration to reverse ketone accumulation.
1. McCabe, D. E., Strollo, B. P. & Fuhrman, G. M. Euglycemic Diabetic Ketoacidosis in the Surgical Patient. Am. Surg. 89, 1083–1086 (2023).
2. Chaudhry, A., Roels, C. & Lee, J. Sodium–Glucose Cotransporter-2 Inhibitor–associated Euglycemic Diabetic Ketoacidosis: Lessons From a Case Series of 4 Patients Undergoing Coronary Artery Bypass Grafting Surgery. Can. J. Diabetes 46, 843–850 (2022).
3. Wan Azman, S. S., Sukor, N., Abu Shamsi, M. Y., Ismail, I. & Kamaruddin, N. A. Case Report: High-Calorie Glucose Infusion and Tight Glycemic Control in Ameliorating Refractory Acidosis of Empagliflozin-Induced Euglycemic Diabetic Ketoacidosis. Front. Endocrinol. 13, 867647 (2022).
4. Jaber, J. F., Standley, M. & Reddy, R. Euglycemic Diabetic Ketoacidosis in Pregnancy: A Case Report and Review of Current Literature. Case Rep. Crit. Care 2019, 1–5 (2019).
5. Algaly, G., Abdelrahman, A. & Ahmed, S. M. I. Euglycemic diabetic ketoacidosis in a pregnant woman. J. Am. Coll. Emerg. Physicians Open 4, e13089 (2023).
6. Dutta, S. et al. Euglycemic diabetic ketoacidosis associated with SGLT2 inhibitors: A systematic review and quantitative analysis. J. Fam. Med. Prim. Care 11, 927 (2022).
7. Koceva, A. & Kravos Tramšek, N. A. From Sweet to Sour: SGLT-2-Inhibitor-Induced Euglycemic Diabetic Ketoacidosis. J. Pers. Med. 14, 665 (2024).
8. Juneja, D., Nasa, P., Jain, R. & Singh, O. Sodium-glucose Cotransporter-2 Inhibitors induced euglycemic diabetic ketoacidosis: A meta summary of case reports. World J. Diabetes 14, 1314–1322 (2023).
9. Albert, S. G., Shrestha, E. & Wood, E. M. Euglycemic diabetic ketoacidosis: The paradox of delayed correction of acidosis. Diabetes Metab. Syndr. Clin. Res. Rev. 17, 102848 (2023).
