Category: Neurology
Keywords: Seizure, pediatrics, ketamine (PubMed Search)
Posted: 5/31/2025 by Visiting Speaker
(Updated: 2/8/2026)
Click here to contact Visiting Speaker
Author: Matthew Jackson, MD
The Ket-Mid Study (1) is a recent RCT out of a tertiary center in a largely rural region of Egypt that evaluated combined ketamine (2 mg/kg) and midazolam (0.2 mg/kg) (ket-mid) to midazolam plus placebo (pla-mid) as the first line seizure abortive therapy. Children in the ket-mid group achieved 76% termination at 5 minutes compared to 21% of those in the pla-mid group (p<0.001). Adverse outcomes were rare, though the pla-mid group did have more hypotension.
Notably, the population included differed from that typically seen in the US. These kids were seizing for a long time, with a median seizure duration before IV meds of 34 minutes, and the benefit of ketamine on subgroup analysis seemed to shrink for those that were treated in less than 30 minutes. CNS infections were also much more common, accounting for the underlying pathology in 11% of cases. Important exclusion criteria also included trauma, inborn errors of metabolism, underlying CNS malignancy, and others not always known to EMS or ED clinicians at the time therapy begins.
1. Othman AA, Sadek AA, Ahmed EA, Abdelkreem E. Combined Ketamine and Midazolam Versus Midazolam Alone for Initial Treatment of Pediatric Generalized Convulsive Status Epilepticus (Ket-Mid Study): A Randomized Controlled Trial. Pediatr Neurol. 2025 Jun;167:24-32. doi: 10.1016/j.pediatrneurol.2025.03.011. Epub 2025 Mar 22. PMID: 40186980.
Category: Trauma
Keywords: geriatric, trauma, CT scan (PubMed Search)
Posted: 5/29/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This literature search from 1946-2023 looking at comparing selective use of CT scans vs whole body scans in geriatric trauma found no benefit of whole body CT in mortality, hospital length of stay or ED discharge. This study only included 15,000 pts over that very long time line. More robust, current work needs to be done on this important topic.
Tang P, Elkington O, Stevens S. Whole body CT-scan vs. selective CT-scan in geriatric trauma: Systematic review and meta-analysis. Trauma. 2025;0(0). doi:10.1177/14604086241304629
Category: Administration
Keywords: Artificial intelligence, Emergency department, emergency practice (PubMed Search)
Posted: 5/27/2025 by Mercedes Torres, MD
(Updated: 5/28/2025)
Click here to contact Mercedes Torres, MD
AI is probably already being used in your ED, like it or not…
This article is an excellent review of the ways that AI can be used in emergency medicine. (See blue boxes in the figure below for a visual representation of opportunities for AI to augment emergency care from start to finish.) The authors note that there will always be a role for human physicians in EDs; AI can serve as an adjunct rather than a replacement for physician care. Physicians should strive to be informed leaders in AI development to ensure it is performed in a cautious, thoughtful, patient-centered manner.
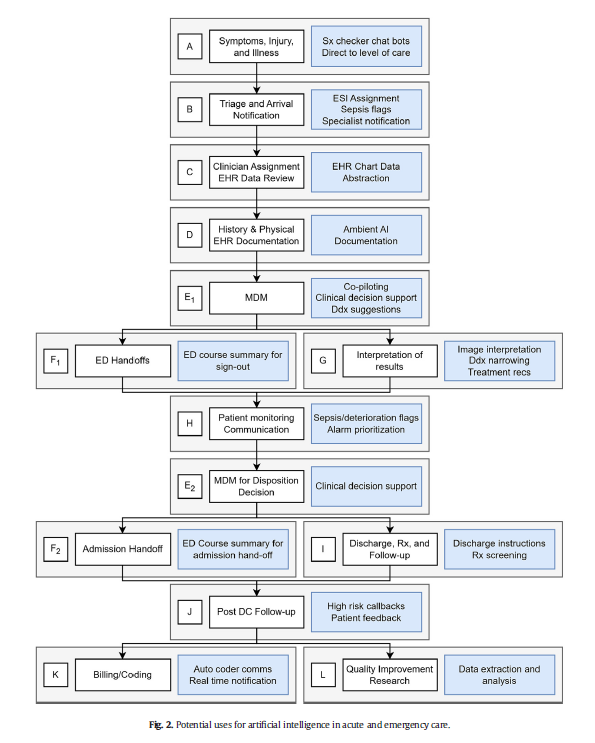
Marika M. Kachman, Irina Brennan, Jonathan J. Oskvarek, Tayab Waseem, Jesse M. Pines. How artificial intelligence could transform emergency care. The American Journal of Emergency Medicine, Volume 81, 2024, Pages 40-46, https://doi.org/10.1016/j.ajem.2024.04.024.
Category: Critical Care
Posted: 5/27/2025 by Quincy Tran, MD, PhD
(Updated: 2/8/2026)
Click here to contact Quincy Tran, MD, PhD
We have known that resuscitation with balanced crystalloids was associated with better outcomes, than normal saline. However, I have believed that in the early phase of resuscitation, volume of any crystalloids is still better than little volume. Thus, a couple of liters of normal saline (0.9% saline) would not hurt. However, the recent secondary analysis from the Crystalloid Liberal or Vasopressors Early Resuscitation in Sepsis (CLOVERS) trial might have changed my practice.
-----
Settings:
60 ICU in the United States between 2018 to 2022. This is the secondary analysis of the Crystalloid Liberal or Vasopressors Early Resuscitation in Sepsis (CLOVERS) trial population
Participants: Patients with sepsis-induced hypotension after receiving fluid resuscitation (from 1-3 litters). Participants who received lactate ringers (622 patients) were compared with patients who received normal saline (690 patients).
Outcome measurement:
Death before discharge home by day 90.
Hospital-free days at 28 days
Study Results:
Dead occurred in 12.2% of LR group (76/622) vs. 15.9% (110/690) patients of the NS group, Adjusted Hazard Ratio 0.71 (95% CI 0.51-0.99, p=0.043)
Patients receiving LR had more hospital-free days at 28 days than those receiving 0.9% saline (16.6 ± 10.8 vs. 15.4 ± 11.4 d, respectively). The mean difference was 1.6 days (95% CI, 0.4–2.8; p = 0.009).
Discussion:
This study confirms that not only early resuscitation is important, but the fluid choice during the early resuscitation phase is also important, especially in patients with signs and symptoms of sepsis.
Thus, even during pre-hospital phase and in the ED, clinicians should consider to use LR or other balanced solutions if available.
Conclusion:
Among patients with sepsis-induced hypotension, resuscitation with Lactate Ringer was associated with better outcomes than normal saline.
Gelbenegger G, Shapiro NI, Zeitlinger M, Jilma B, Douglas IS, Jorda A. Lactated Ringer's or Normal Saline for Initial Fluid Resuscitation in Sepsis-Induced Hypotension. Crit Care Med. 2025 May 1;53(5):e1140-e1144. doi: 10.1097/CCM.0000000000006601. Epub 2025 Feb 19. PMID: 39969246; PMCID: PMC12047640.
Category: Infectious Disease
Keywords: Coccidioidomycosis, climate change (PubMed Search)
Posted: 5/26/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Typically Coccidioidomycosis is seen in the Southwestern US. The authors of this study, using climate modeling predict endemic areas will spread across the US to include Idaho, the Dakotas, Nebraska and Wyoming.
Clinically, “Patients with pulmonary Coccidioides infection frequently experience fever, cough, and shortness of breath. Chest radiographic imaging may demonstrate lobar, segmental, or multifocal consolidations; cavitary lesions; and lung nodules. Given these nonspecific findings, patients with coccidioidomycosis are often treated for community-acquired pneumonia. Coccidioidomycosis should be considered in patients not improving with antibiotic treatment or in those who have exposure to or reside in endemic areas. Up to 50% of patients with pulmonary coccidioidomycosis have erythema nodosum, approximately 25% to 30% have peripheral eosinophilia, and approximately 25% have arthralgias (particularly symmetric knee and ankle arthralgia). Up to 10% of patients diagnosed with coccidioidomycosis develop disseminated disease, including skin, central nervous system, and bone and joint infection.”
Lee PS, Swain DL, Johnson R. Climate Change and Coccidioidomycosis. JAMA. 2025;333(11):997–998. doi:10.1001/jama.2024.27274
Category: Orthopedics
Posted: 5/25/2025 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Distal Radius Fractures
One of the most common fracture locations seen in EM (1/6th of all fractures)
Surgical rates are approximately 15-20%
Bimodal injury distribution:
Younger patients (10-14yo)
Usually involved in sport and usually high energy mechanism
Sport associated injury: Artificial turf increase risk by 5x.
Increased risk with skiing and rugby
Increased risk with novice and intermediate snowboarders who don’t wear protective equipment.
Older patients (>50yo)
Associated with osteoporotic bone from low energy fall
Risk factors among older patients: Hx of recurrent falls, prior fragility fracture, decreased bone density, corticosteroid use, and also dementia when patient reaches age 75.
Encourage your older patients who sustain this injury to discuss bone density testing with their PCP. Patients at higher risk of hip fractures (which carries high morbidity and mortality)
Check and document median nerve function in all patients esp. in high energy injuries
Median nerve involved in up to 21-30%.
Check “A-OK sign” against resistance
Iatrogenic median nerve injury can also occur if patient splinted in position of flexion
Category: Orthopedics
Posted: 5/6/2025 by Brian Corwell, MD
(Updated: 5/24/2025)
Click here to contact Brian Corwell, MD
Metformin, most widely used for type 2 diabetes, has shown promising early results in several different health outcomes.
A recent study, published in JAMA, investigated whether metformin could reduce knee pain in patients with symptomatic knee OA who were overweight or obese.
This was a small double-blind, placebo-controlled clinical trial involving 107 participants.
Background: There is some evidence (both preclinical and preliminary human) that metformin can reduce cartilage degradation and increase chondrocyte viability.
Intervention: Participants received metformin 2000 mg/day (n=54), or identical placebo (n=53) for 6 months.
Mean age, 58.8 [SD, 9.5] years. 68% female.
Patients had symptomatic radiologic knee OA and a body mass index > 25.
Adverse effects: Diarrhea (8 [15%] in the metformin group and 4 [8%] in the placebo group) and abdominal discomfort (7 [13%] in the metformin group and 5 [9%] in the placebo group).
Despite this, there were high levels of medication adherence.
The study found significant differences in primary and secondary outcome measures: Knee pain, stiffness and function.
There was some weight loss in both groups (mean change, 4 lbs in the metformin group and 2.6 lbs in the placebo group). Unlikely to explain outcome differences.
Conclusion: In patients with symptomatic knee osteoarthritis who were overweight or obese, metformin, had a moderate and statistically significant reduction in knee pain compared with placebo. Because of the small sample size, confirmation in a larger clinical trial is warranted.
Pan F, Wang Y, Lim YZ, et al. Metformin for Knee Osteoarthritis in Patients With Overweight or Obesity: A Randomized Clinical Trial. JAMA. Published online April 24, 2025.
Category: Neurology
Keywords: CVA, TIA, prediction, one year (PubMed Search)
Posted: 5/21/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
How likely is your TIA pt to go on to have a stroke? This study in JAMA gives us some answers. While EM providers aren’t as interested in 5 and 10 year prediction, it provides more evidence TIAs need to be evaluated and are risk factors for future events.
“In this systematic review and meta-analysis of 171?068 patients with TIA or minor stroke from 38 studies, the risk of subsequent stroke was 5.9% within 1 year, 12.8% within 5 years, and 19.8% within 10 years.”
Category: EMS
Keywords: ultrasound, EMS, COPD, pulmonary edema (PubMed Search)
Posted: 5/21/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
33 paramedics had a short course in thoracic point of care ultrasound. There was a pre and post test that included the history and physical exam for patient scenarios with COPD and CHF exacerbations. Paramedics were asked to select the appropriate treatments. The post test included ultrasound images. Diagnostic accuracy in the post test improved by 17% and appropriate treatment selection improved by 23%. Paramedics were also able to correctly identify ultrasound images 90% of the time.
Bottom line: Introducing thoracic ultrasound to paramedics can improve patient care.
Fitzgerald E, Parker S, Hancock S, et al. Thoracic ultrasound may improve paramedic diagnostic and management accuracy in undifferentiated respiratory distress. J Am Coll Emerg Physicians Open. 2024;5(2):e13164. Published 2024 Apr 16. doi:10.1002/emp2.13164
Category: Critical Care
Posted: 5/21/2025 by Caleb Chan, MD
(Updated: 2/8/2026)
Click here to contact Caleb Chan, MD
DeMasi et al. published a review on the current evidence surrounding peri-intubation and intubation practices. While the actual approach and context to each patient will be different it is good to be aware of the actual evidence base for medical decision-making.
Preoxygenation
Between Induction and Laryngoscopy
During Laryngoscopy and Intubation of the Trachea
Medications
Interventions to Prevent Hypotension
DeMasi SC, Casey JD, Semler MW. Evidence-based emergency tracheal intubation. Am J Respir Crit Care Med. Published online April 16, 2025.
Category: Ultrasound
Keywords: soft tissue; point of care ultrasound (PubMed Search)
Posted: 5/19/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
When evaluating foreign bodies in soft tissue, an imaging interface- such as a standoff pad- can improve imaging of superficial structures.
Common image interfaces include gel, commercial standoff pads, saline bags, and water baths.
Water baths are primarily used for imaging the hands and feet, but a recent study explored a water-filled patient belongings bag as a novel alternative. This method gives the benefit of the same elevated standoff that water baths provide, while accommodating larger extremities that may not fit in traditional setups.
The study found no significant difference between the patient belonging bag and a water bath for identifying a FB in a porcine model. Saline bags had the lowest image quality.
Vega C, Lindsay R, Shokraneh K, et al.. POCUS Standoff: Comparing Ultrasound Interfaces for Soft Tissue Foreign Body Imaging. Pediatric Emergency Care. 2025; 41 (5): 354-358. doi: 10.1097/PEC.0000000000003359.
Category: ENT
Keywords: Epistaxis prophylaxis (PubMed Search)
Posted: 5/18/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This large retrospective database study compared those receiving antibiotics after anterior nasal packing to those that did not. There was no difference in clinically significant infection between the groups leading the authors to conclude prophylactic antibiotics after anterior nasal packing is not required.
Tran QK, Vashee I, Vanga R, Camp S, Rallo MK, Najafali D, Bontempo LJ, Pourmand A. Is antibiotic prophylaxis necessary for anterior epistaxis with packing? Insights from a large database. Am J Emerg Med. 2025 Mar 19;93:64-72. doi: 10.1016/j.ajem.2025.03.040. Epub ahead of print. PMID: 40147155.
Category: Administration
Posted: 5/16/2025 by Kevin Semelrath, MD
(Updated: 5/17/2025)
Click here to contact Kevin Semelrath, MD
We talk a lot about the efforts within our profession at increasing diversity, inclusion and equity, but this study grants a unique perspective on that by surveying our patients on their experience of DEI in the ED.
The authors surveyed about 1700 patients, with 800 responding, at a large ED in Detroit. The population was majority black, and had a wide degree of variability in socioeconomic status.
Overall the patients felt that the staff had no biased or prejudiced interactions with people of different races. However, they felt that people from lower socioeconomic levels, transgender patients, and those that had mental health issues were treated unfairly. They also noted (about17% of respondents) harassment of ED staff by another patient.
Kavya Davuluri 1,?, Nikhil Goyal 2,3, Harold Gomez Acevedo 4, Jason Folt 2, Namita Jayaprakash 2,5, Michelle Slezak 2, Martina T Caldwell 2
PMCID: PMC9482342 PMID: 36176501
Category: Pediatrics
Keywords: Infant, hypothermia, sepsis screen (PubMed Search)
Posted: 5/16/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
While there are numerous evidence-based recommendations for the management of febrile infants, there are not clear guidelines for the management of hypothermic infants (0-90 days).
A recent review article offered the following summary points from the literature:
The World Health Organization defines hypothermia as a temperature < 36.4 degrees Celsius while the International Pediatric Sepsis Consensus Conference uses < 36.0 degrees Celsius. A multicenter study attempted to empirically derive a threshold for hypothermia but was not successful.
One study looking at the age of presentation of hypothermic patients showed that > 50% of the infants that presented were < 7 days old.
There are numerous reasons that an infant can be hypothermic, including bacterial infections such as urinary tract infections, bacteremia or meningitis, viral infections (herpes simplex virus) or environmental factors. Premature infants can also have temperature instability as can those with insufficient caloric intake.
Serious bacterial infection (defined as urinary tract infections, bacteremia or meningitis ) occurred less frequently in hypothermic infants compared to febrile infants, but the rates of invasive bacterial infections (defined as bacteremia and meningitis) were the same between the two groups.
In 112 patients with neonatal HSV, 5.2% of the cases were hypothermic, 30.9% had fever and 63.9% had no change in temperature.
Important questions/exam findings to raise suspicion for a pathological cause of hypothermia:
Perinatal history: Gestational age, GBS and HSV status of mom, perinatal antibiotics, and potential exposures to HSV.
Weight change, activity change, interest in feeding, abnormal movements, changes in breathing pattern, ill appearance
Some institutions will group the evaluation of hypothermic infants into the febrile infant guidelines, but there are currently no evidence-based pathway's. Striking a balance between over testing and not missing a serious bacterial infection is difficult and an area that requires additional research.
Ramgopal S, Lo YHJ, Potisek NM, Money NM, Halvorson EE, Cruz AT, Rogers AJ. Current Evidence on the Care of Young Infants With Hypothermia in the Emergency Department. Pediatr Emerg Care. 2025 Feb 1;41(2):146-151. doi: 10.1097/PEC.0000000000003259. PMID: 39883795.
Category: Critical Care
Posted: 5/15/2025 by William Teeter, MD
(Updated: 2/8/2026)
Click here to contact William Teeter, MD
Reversal of Factor Xa Inhibitor-Related Intracranial Hemorrhage: A Multicenter, Retrospective, Observational Study Comparing the Efficacy and Safety of Andexanet and PCCs
This study compared patients with a wide variety of intracranial hemorrhage types taking direct oral anticoagulants (e.g. apixaban or rivaroxaban) who then received andexanet versus prothrombin complex concentrates (PCCs)
Patients receiving andexanet (87.8%) had higher odds of achieving excellent/good hemostasis (odds ratio [OR] 1.60; 95% CI, 1.00-2.56; p = 0.048) compared with PCCs (81.8%). Patients treated with andexanet (7.9%) had higher odds of a thrombotic event (OR 1.91; 95% CI, 1.13-3.20; p = 0.014) compared to those treated with PCCs (4.2%).
This study found similar results to the previous ANNEXA-1 trial but included GCS < 7 or Neurosurgery within 12 hours of enrollment, which ANNEXA did not. This study was not designed to prove non-inferiority and should not change practice, especially given the eye-watering cost of Andexanet ($25,000+) versus PCCs (~$4000-6000)…. but betting they are working on one that will.
Category: Obstetrics & Gynecology
Posted: 5/11/2025 by Jennifer Wang, MD
(Updated: 5/12/2025)
Click here to contact Jennifer Wang, MD
Despite its name, we're not really sure what's happening in amniotic fluid embolisms. We think that some amniotic fluid and fetal cells gets into the parental blood vessels, and this causes a cytokine storm that leads to systemic vascular collapse, but we're still figuring it out. This is a clinical diagnosis, and while rare (1-3/100000), it can be extremely fatal, ranging anywhere from 10%-60% mortality depending on what study you're looking at. Even worse, some studies show that up to 80% of patients arrest at some point after their diagnosis, many within 5 minutes of their symptoms beginning.
Key times to look for this are postpartum AND post-abortion (though post-abortion is even rarer).
What you're looking for:
Often times, there will be neurological symptoms like AMS, seizures, and confusion.
There is no cure, so we treat the symptoms: use your vasopressors! Norepinephrine is our go-to, but keep your inotropic agents close, because of your right heart failure (dobutamine, milrinone). You can also try iNO therapy, MTP, and ECMO if you're at a facility capable of it.
Coggins AS, Gomez E, Sheffield JS. Pulmonary Embolism and Amniotic Fluid Embolism. Obstet Gynecol Clin North Am. 2022;49(3):439-460. doi:10.1016/j.ogc.2022.02.015
Category: Trauma
Keywords: Incarcerated, trauma, mortality, disparity (PubMed Search)
Posted: 5/11/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Looking at a year’s worth of data from the National Trauma Databank, the authors found incarcerated trauma patients were more likely to be stabbed, male, persons of color and have a higher adjusted mortality rate.
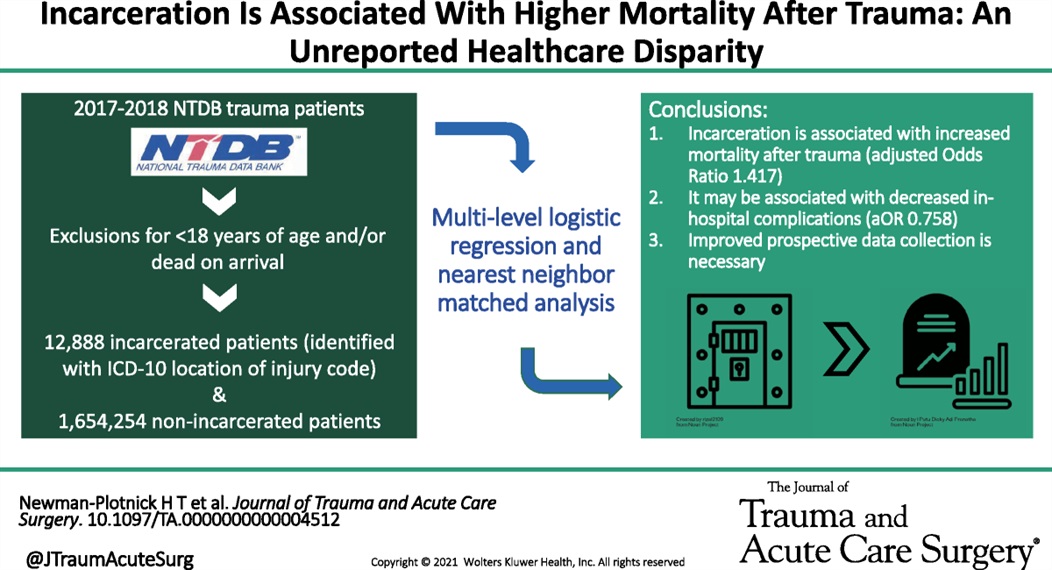
Newman-Plotnick, Harry MD, MPH; Byrne, James P. MD, PhD; Haut, Elliott Richard MD, PhD, FACS; Hultman, Charles Scott MD, MBA, FACS
Journal of Trauma and Acute Care Surgery 98(5):p 785-793, May 2025. | DOI: 10.1097/TA.0000000000004512
Category: Pediatrics
Keywords: Pediatrics, trauma (PubMed Search)
Posted: 5/8/2025 by Kathleen Stephanos, MD
(Updated: 5/9/2025)
Click here to contact Kathleen Stephanos, MD
2024 brought us an excellent new decision tool to prevent excessive radiation for children. NOTE: These are vastly different than adult criteria.
In children with traumatic injuries, most will NOT require CT imaging.
This study included over 22,000 patients (age 0-17 years) who were evaluated following blunt trauma. A rate of <1% were found to have c-spine injuries. Excluded from the study were strangulation patients, intoxicated patients, and predisposing conditions including prior fracture.
Indications for considering CT C-spine include ANY of the following:
Indications for consider C-spine XRs include ANY of the following:
Abnormal XR findings should receive further evaluation as per standard of care.
The remaining patients may have their c-spine cleared.
Leonard JC, Harding M, Cook LJ, Leonard JR, Adelgais KM, Ahmad FA, Browne LR, Burger RK, Chaudhari PP, Corwin DJ, Glomb NW, Lee LK, Owusu-Ansah S, Riney LC, Rogers AJ, Rubalcava DM, Sapien RE, Szadkowski MA, Tzimenatos L, Ward CE, Yen K, Kuppermann N. PECARN prediction rule for cervical spine imaging of children presenting to the emergency department with blunt trauma: a multicentre prospective observational study. Lancet Child Adolesc Health. 2024 Jul;8(7):482-490. doi: 10.1016/S2352-4642(24)00104-4. Epub 2024 Jun 4. Erratum in: Lancet Child Adolesc Health. 2024 Dec;8(12):e17. doi: 10.1016/S2352-4642(24)00311-0. PMID: 38843852; PMCID: PMC11261431.
Category: Pharmacology & Therapeutics
Keywords: urinary tract infection, pyelonephritis, cephalosporins, fluoroquinolones, antimicrobial resistance (PubMed Search)
Posted: 5/8/2025 by Matthew Poremba
Click here to contact Matthew Poremba
Background:
The 2010 Infectious Diseases Society of America (IDSA) cystitis and pyelonephritis guidelines recommend fluoroquinolones (FQs) as first line agents for pyelonephritis treatment and also support trimethoprim-sulfamethoxazole (TMP-SMX) usage if the urinary pathogen is known to be susceptible. However, alternative regimens need to be evaluated as FQs are increasingly associated with serious adverse events, and E coli resistance rates to both FQs and TMP-SMX are rising nationally. The Cephalosporins for Outpatient Pyelonephritis in the Emergency Department (COPY-ED) study aimed to evaluate the effectiveness of oral cephalosporins in acute pyelonephritis treatment when compared to IDSA guideline-endorsed first line treatments.
Study design:
This multicenter, retrospective observational cohort study screened patients with a primary diagnosis of uncomplicated or complicated pyelonephritis using ICD-10 codes. They included all patients >18 years of age who reported symptoms of a UTI and were discharged home on oral antimicrobial therapy. Exclusion criteria included pregnancy, acute or chronic prostatitis, orchitis, epididymitis, or urinary tract surgery within 7 days prior to ED visit or surgery planned during the study period.
The primary outcome was rate of outpatient treatment failure within 14 days of discharge from the emergency department with cephalosporins compared to FQs and TMP-SMX.
Patient Population:
Results:
Rates of treatment failure at 14 days were not statistically significant between groups, with a rate of 17.2% in the cephalosporin group and a rate of 22.5% in the FQ + TMP/SMX group. After adjusting for gender, complicated infections, previous use of intravenous or oral antibiotics, and urinary tract abnormality, the odds of treatment failure at 14 days were still not significantly different in patients who received fluoroquinolone or TMP/SMX (adjusted OR 1.275 [95% CI 0.86 to 1.9]) compared to cephalosporins.
Secondary outcomes included rates of treatment failure with first generation cephalosporins (cephalexin, cefadroxil, cefuroxime) and third generation cephalosporins (cefpodoxime, cefuroxime), rates of appropriate therapy selected based on urine culture susceptibilities, and rates of treatment failure compared to duration of treatment prescribed. None of these outcomes found statistically significant differences between groups.
Study Limitations:
Key Takeaways:
Category: Orthopedics
Keywords: Hip fractures, geriatrics, complications (PubMed Search)
Posted: 5/7/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This article reminds us that hip fractures have a one year mortality rate of 12-25% and 50% of hip fracture patients develop complications while in the hospital. “Almost half of individuals hospitalized with hip fractures experience complications, such as delirium, pneumonia, acute kidney injury, urinary tract infection, and deep vein thrombosis”
Because of these complications, multidisciplinary teams should be caring for these patients and great care should be exercised when evaluating these patients.
JAMA Insights
March 24, 2025
Yiju Teresa Liu, MD1,2; Eva Tovar Hirashima, MD, MPH3; Kabir Yadav, MDCM, MS, MSHS1,4
JAMA. Published online March 24, 2025. doi:10.1001/jama.2025.0999
