Category: Gastrointestional
Keywords: TXA, GI bleeding (PubMed Search)
Posted: 12/10/2025 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
A recent study in AJEM reviewed the utility of TXA in GI bleeding
This is a PRISMA?guided systematic review and meta?analysis of 7 RCTs (13,608 adults, 1976–2024) evaluating IV TXA vs placebo in acute gastrointestinal bleeding, including upper and mixed GI sources across multiple countries. The largest contributor is HALT?IT (Roberts et al.), which accounts for nearly 90% of participants.
-Mortality: No statistically significant reduction in all?cause mortality with TXA (OR 0.77; 95% CI 0.56–1.07, P = 0.12).?
-Rebleeding: TXA significantly reduced rebleeding events (OR 0.64; 95% CI 0.45–0.91, P = 0.01).?
-"Failure to control" bleeding: TXA reduced failure of hemostasis (OR 0.55; 95% CI 0.32–0.93, P = 0.03).
-Thromboembolic events: Random?effects model showed no significant difference (OR 1.28; 95% CI 0.51–4.51, P = 0.46), but fixed?effect analysis suggested a statistically significant increase (OR 1.28; 95% CI 1.07–1.55, P = 0.009), highlighting a possible thrombotic signal.?
-Transfusion and LOS: No significant reduction in blood transfusion requirements with TXA (OR 0.94; 95% CI 0.61–1.43, P = 0.76); length of stay and other resource metrics were variably reported and not clearly improved.
Take-Aways:
TXA may be reasonable as an adjunct in GI bleeding when the goal is to reduce rebleeding or “failure to control” bleeding, but current evidence does not support it as a mortality?reducing therapy.?
Given a potential increased risk of thromboembolic events, TXA should be used cautiously in patients with high baseline thrombotic risk, and always as part of a broader package including resuscitation and timely endoscopy rather than as a standalone intervention.
Djoudjou T, Alamri O, Aljuwayr A, et al. Intravenous tranexamic acid in gastrointestinal bleeding: A systematic review and meta-analysis of randomized controlled trials. Am J Emerg Med. 2025;97:175-182. doi:10.1016/j.ajem.2025.07.050
Category: Gastrointestional
Keywords: gastroenteritis, odansetron, prescription (PubMed Search)
Posted: 11/12/2025 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
Anecdotally, we as emergency physicians are fairly comfortable prescribing odansetron to adults with nausea and vomiting. However, emergency physicians often treat pediatric gastroenteritis with a single dose of odansetron in the department. A recent study in NEJM examined effects of discharging with odansetron. Full details can be found in the study, but the take-home:
Sending children home with ondansetron after an emergency visit for gastroenteritis cut the rate of moderate-to-severe illness from 12.5% to 5.1% compared to placebo, with no uptick in adverse events. Those taking ondansetron experienced fewer vomiting episodes in the first 48 hours. Targeted, as-needed dosing helps the sickest children recover faster, while avoiding unnecessary medication for most kids.
Freedman SB, Williamson-Urquhart S, Plint AC, et al. Multidose Ondansetron after Emergency Visits in Children with Gastroenteritis. N Engl J Med. 2025;393(3):255-266. doi:10.1056/NEJMoa2503596
Category: Gastrointestional
Keywords: GI bleed, presentation, antithrombotics (PubMed Search)
Posted: 10/8/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In a retrospective observational study comparing patients both on and not on antithromotics (DOAC/warfarin or anti platelets) who presented with a GI bleed these authors found:
“Patients with anticoagulant therapy more often present with a lower source of GI bleeding than both those on antiplatelet medications and those with no antithrombotics. Overall patients on anticoagulants are also less likely to present with hematemesis, even with a later confirmed upper GI bleeding. Furthermore, results indicate that the need for endoscopic interventions and transfusions are dependent on initial presenting symptoms but not affected by antithrombotic therapy at admission.”
Forsberg-Puckett, A., Wurm Johansson, G. & Regnér, S. Presentation of gastrointestinal bleeding in patients with antithrombotic therapy, results from a consecutive retrospective cohort. Scand J Trauma Resusc Emerg Med 33, 146 (2025). https://doi.org/10.1186/s13049-025-01431-1
Category: Gastrointestional
Keywords: GI bleed, imaging (PubMed Search)
Posted: 9/10/2025 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
The TLDR:
In the ED setting, CTA for suspected GI bleeding is frequently ordered, but it’s finding less. At one center, use went up sevenfold over six years, while positive results dropped from 1 in 5 scans to about 1 in 16. Older patients are more likely to have a positive scan, and those with active cancer less so. CTA can be very useful when targeted, but widespread use may add cost, radiation, and crowding without improving care—so choosing patients carefully is key.
The longer version:
This was a retrospective cohort study involving adult patients who had undergone abdominal and pelvic CTA for suspected GIB at a large urban academic medical center between January 2017 and December 2023. The primary outcomes of interest were 1) The annual number and proportion of GIB-related CTAs among all CT scans performed in the ED, and 2) The diagnostic yield, defined as the percentage of CTAs that showed active bleeding or hemorrhage.
Findings:
CTA usage increased substantially: In 2017, there were 30 GIB-related CTAs out of 32,197 ED CT exams (0.09%). By 2023, this rose to 288 out of 44,423 (0.65%)
Diagnostic yield declined: In 2017, 6 of 30 CTAs were positive (20.0%). In 2023, only 18 of 288 were positive (6.3%)
Data of interest:
Later years (ie 2023 rather than 2017) were linked to lower odds of a positive CTA (odds ratio [OR] 0.84 per year; 95% CI, 0.73–0.96; P = .01). Older patients had higher odds of a positive result (OR 1.02 per year of age; 95% CI, 1.00–1.04; P = .02). Patients with active cancer had lower odds of positive findings (OR 0.35; 95% CI, 0.12–1.00; P = .05)
Discussion:
Despite the marked increase in CTA use for suspected GIB, its diagnostic effectiveness dropped sharply over the study period. The findings emphasize the need to balance the benefits (such as detecting active bleeding) with the downsides—including interpretation time, radiation exposure, costs, and ED crowding. The authors suggest implementing evidence-based protocols and decision-support tools to optimize CTA use in emergency settings to improve appropriateness and diagnostic yield.
Prasad S, Hood CM, Young C, et al. Computed Tomographic Angiography and Yield for Gastrointestinal Bleeding in the Emergency Department. JAMA Netw Open. 2025;8(8):e2529746. Published 2025 Aug 1. doi:10.1001/jamanetworkopen.2025.29746
Category: Gastrointestional
Keywords: PECARN, abdomen, clinical decision making (PubMed Search)
Posted: 8/13/2025 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
Most of us are probably familiar with the PECARN Algorithm for neuroimaging in pediatric head trauma. But fewer people are familiar with the PECARN Pediatric Intra-Abdominal Injury (IAI) Algorithm.
Inclusion criteria can be found in the original study, referenced below
The original study collected data from 20 studies, and found that CT imaging can be avoided (ie patients are at very low risk for IAI) if the following criteria are met:
-No visible abdominal wall trauma or seatbelt sign
-GCS > 13
-No abdominal tenderness
-No thoracic wall trauma
-No abdominal pain
-No decreased breath sounds
-No vomiting
In the original cohort, 42% of study participants met all of these criteria and the risk of IAI requiring intervention was 0.1%
This study has been validated multiple times since its introduction in 2012, with the most recent being a multicenter study published in the Lancet in 2024. This recent study looked at 7542 children with blunt abdominal trauma, and the IAI rule was fond to have a sensitivity of 100% (95% CI 98-100%) and a negative predictive value (NPV) of 100% (95% CI 99.9-100%).
I know, it seems too good to be true…but the takeaway is that these clinical decision making rules can be more reliable than clinical gestalt in the appropriate patient population.
Holmes JF, Lillis K, Monroe D, et al. Identifying children at very low risk of clinically important blunt abdominal injuries. Ann Emerg Med. 2013;62(2):107-116.e2. doi:10.1016/j.annemergmed.2012.11.009
Holmes JF, Yen K, Ugalde IT, et al. PECARN prediction rules for CT imaging of children presenting to the emergency department with blunt abdominal or minor head trauma: a multicentre prospective validation study. Lancet Child Adolesc Health. 2024;8(5):339-347. doi:10.1016/S2352-4642(24)00029-4
Algorithm: https://www.mdcalc.com/calc/3971/pecarn-pediatric-intra-abdominal-injury-iai-algorithm
Category: Gastrointestional
Keywords: admission, abdominal pain (PubMed Search)
Posted: 4/9/2025 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
Do you ever tell your patients to “follow up with your primary care physician in 3-5 days”? How many of them actually do it? And does it make a difference?
Study Overview:
This study is a retrospective analysis of 28,085 adults (?20 years) presenting with acute abdominal pain (AAP) at 15 German emergency departments (EDs) in 2016.
Key Findings:
Hospitalization rate:
39.8% were admitted to the hospital from the ED.
Outpatient Care (OC) Before ED Visit:
33.9% had an OC visit within 3 days before their ED visit.
Of these, 48.6% were hospitalized.
Outpatient Care After ED Visit:
62.7% had OC follow-up within 30 days.
Factors Increasing Hospitalization Odds:
Age ?65 years: aOR 3.05
Prior OC: aOR 1.71
Male sex: aOR 1.44
In-Hospital Mortality:
3.1%
ED Re-visits Within 30 Days:
More likely in age ?65: aOR 1.32
Less likely with prior OC: aOR 0.37
Conclusion:
Acute abdominal pain in the ED is associated with high hospitalization and mortality rates, especially in older adults and those with prior outpatient visits. Prior outpatient contact is linked with both increased admission likelihood and reduced risk of ED re-visits, highlighting its complex role in care continuity. Improving outpatient care access and coordination may reduce ED burden and enhance outcomes for AAP patients.
While there are other factors to consider ie the health care system and its infrastructure, this does provide some interesting food for thought about what happens when we discharge patients.
Verleger K, Fischer-Rosinsky A, Möckel M, et al. Health care utilization of patients with acute abdominal pain before and after emergency department visits. Scand J Trauma Resusc Emerg Med. 2024;32(1):68. Published 2024 Aug 12. doi:10.1186/s13049-024-01237-7
Category: Gastrointestional
Keywords: Appendicitis, scoring, prediction, Alvarado Score (PubMed Search)
Posted: 4/6/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Missed appendicitis leading to rupture and peritonitis leads to morbidity, mortality, and malpractice claims. Part of a longer article looking at evaluation and management of appendicitis, these authors provide three scoring systems that can be used to identify appendicitis. Use of these scores can guide imaging and surgical consultation.
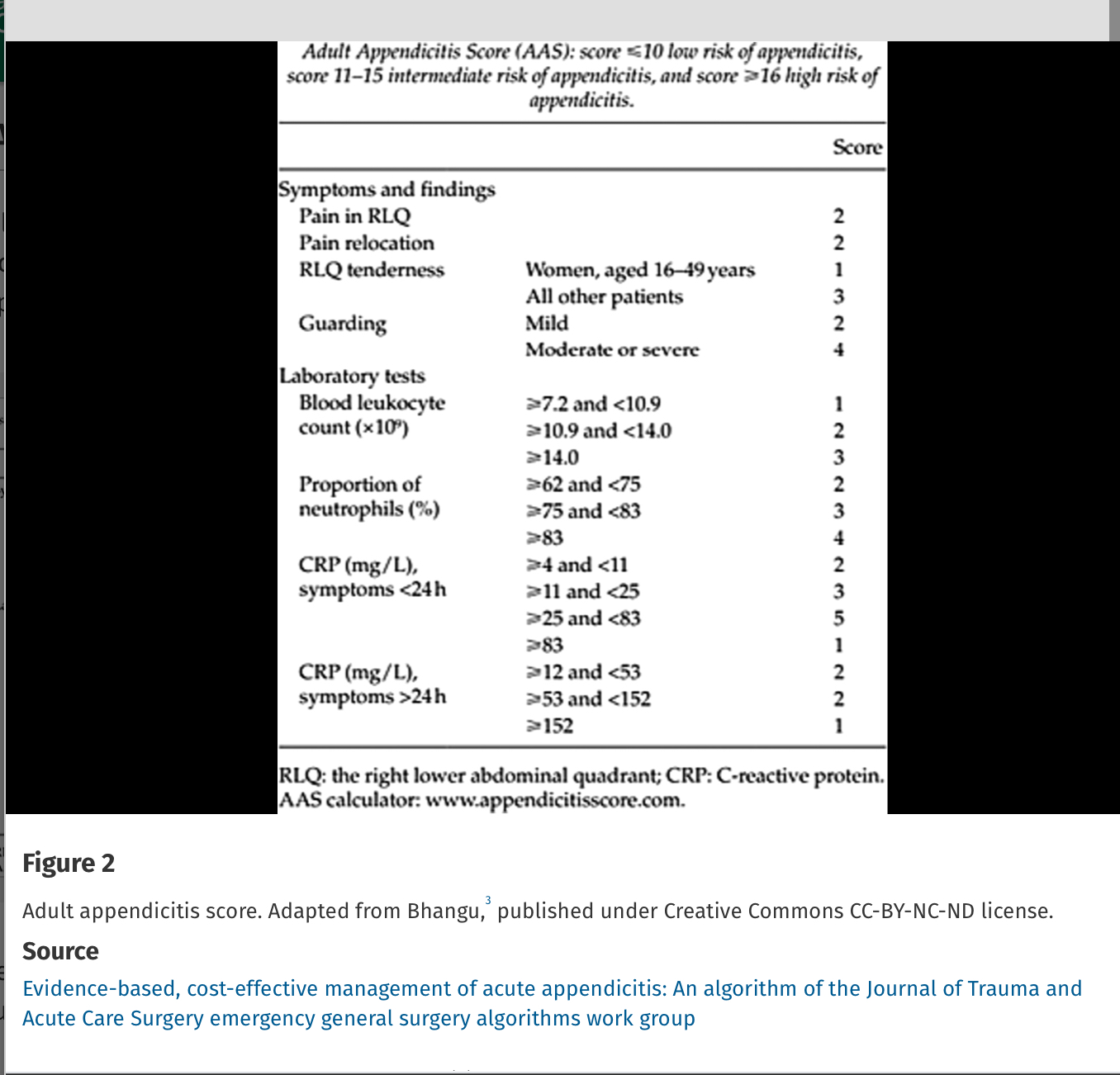
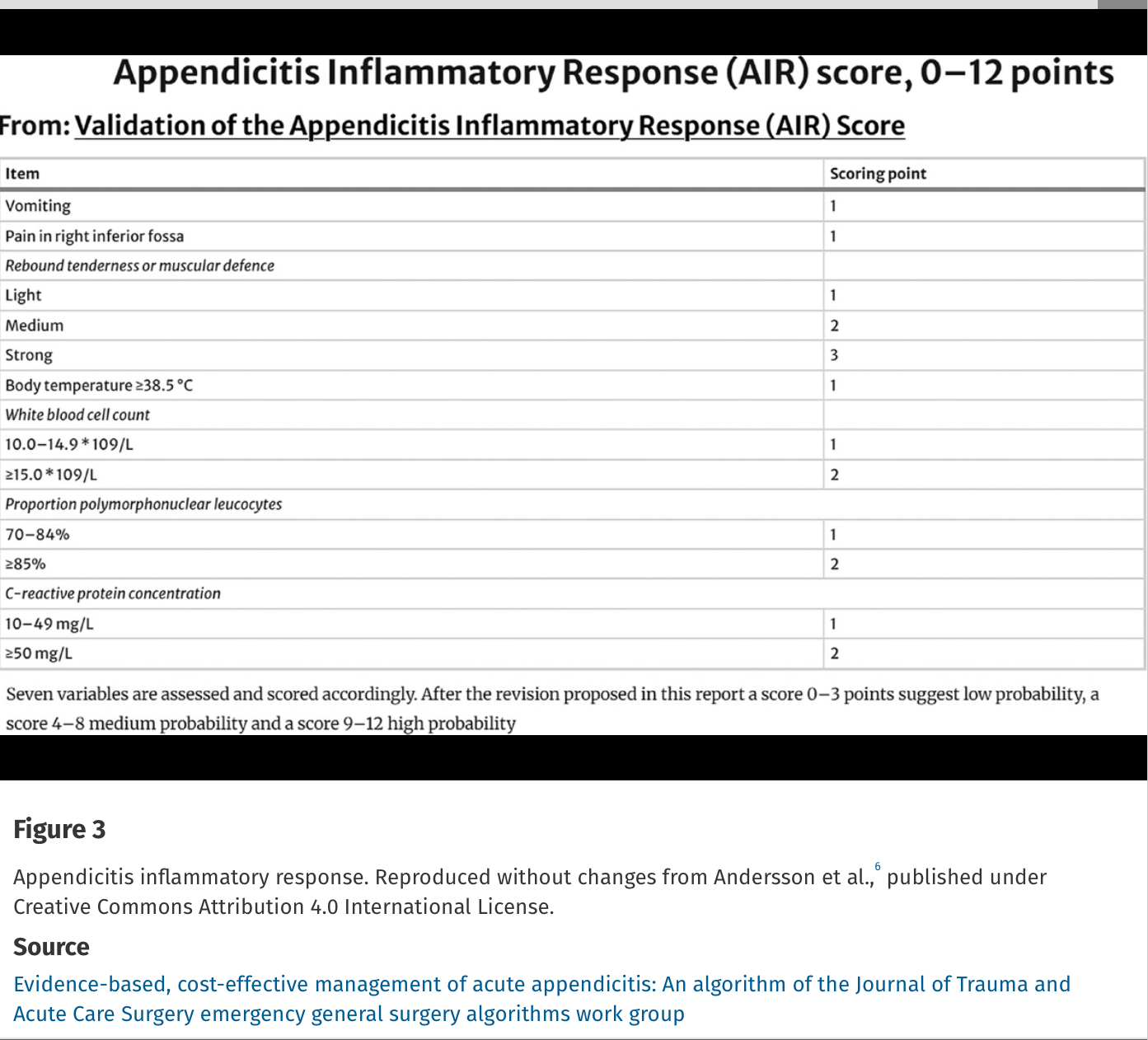
Alvarado Score: If a patient scores 1 to 4, the risk of appendicitis drops to 33%. If a patient scores >5, the risk of acute appendicitis is 66% or greater.
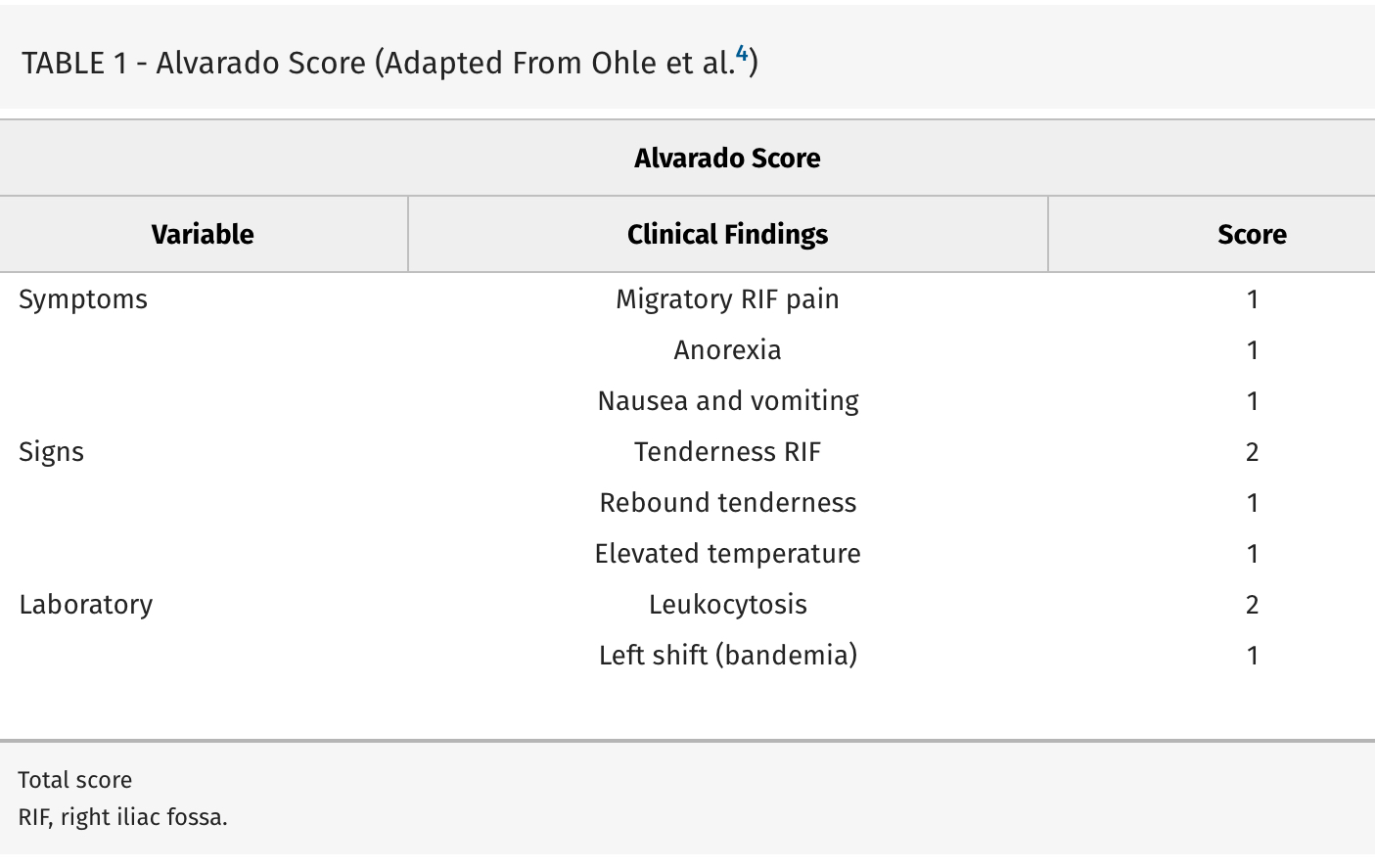
Evidence-based, cost-effective management of acute appendicitis: An algorithm of the Journal of Trauma and Acute Care Surgery emergency general surgery algorithms work group
Diaz, Jose J. MD, CPE, CNS, FACS, FCCM; Napolitano, Lena MD; Livingston, David H. MD; Costantini, Todd MD; Inaba, Kenji MD; Biffl, Walter L. MD; Winchell, Robert MD; Salim, Ali MD; Coimbra, Raul MD, PhD
Journal of Trauma and Acute Care Surgery 98(3):p 368-373, March 2025. | DOI: 10.1097/TA.0000000000004569
Category: Gastrointestional
Keywords: Droperidol, abdominal pain (PubMed Search)
Posted: 3/13/2025 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
Many of us probably use droperidol for pain relief in the ED. If you don't, two recent studies highlight it's use in multimodal pain control:
-In the DRUGS study (2023), droperidol reduced opiod use (46% vs 60%), lowered pain scores (median of 9 vs 5), and decreased the need for antiemetics (60% vs 73%). Before you ask - mean pain score wasn't reported!
-This study evaluated gastroparesis patients, with most common dose of droperidol being 1.25 mg IV
-the DREAMER study (2024) showed that pateitns receiving droperidol required fewer opiods (median 10 Morphine Milligram Equivalents vs 19.4 MME). No significant different in need for antiemetics
-This study evaluated abdominal pain patients, with 2.5 mg IV being the most common dose
Neither study found statistically significant differences in length of stay. Additionally, neither study reported major adverse effects or healthcare costs. Note that these were both single center trials as well.
With droperidol shortages ongoing, suggestions were made to directly compare droperidol to haloperidol, with hopefully more research coming soon!
-Stirrup N, Jones G, Arthur J, Lewis Z. Droperidol undermining gastroparesis symptoms (DRUGS) in the emergency department. Am J Emerg Med. 2024 Jan;75:42-45. doi: 10.1016/j.ajem.2023.10.030. Epub 2023 Oct 21. PMID: 37897920.
-Townsend BR, Malka ST, Di Paola SG, Nisly AE, Gilbert BW. DRopEridol for Abdominal pain in the emergency department for Morphine Equivalent Reduction. The DREAMER study. Am J Emerg Med. 2025 Jan 4;90:31-34. doi: 10.1016/j.ajem.2024.12.082. Epub ahead of print. PMID: 39798184.
Category: Gastrointestional
Posted: 8/13/2024 by Neeraja Murali, DO, MPH
(Updated: 8/14/2024)
Click here to contact Neeraja Murali, DO, MPH
This study, done out of Australia, examined the association between abdominal pain and severity of liver injury in patients presenting after acute acetaminophen overdose.
539 cases were identified where N-acetylcysteine was administered to patients with acetaminophen overdose. The investigators explored parameters including presence of abdominal pain, time post-ingestion, and peak ALT.
Patients less than 8 hours post overdose WITH abdominal pain were as likely to develop hepatotoxicity as those presenting WITHOUT abdominal pain. (OR=1.18 [0.07 to 19.4])
Patients presenting 8 or more hours post overdose WITH abdominal pain were as likely to develop hepatotoxicity as those WITHOUT abdominal pain (OR=1.28 [0.39 to 4.21])
Don't let lack of pain fool you! Just as we all learned in medical school - let your history be your guide!
Wang C, Wong A. The presence of abdominal pain associated with acetaminophen overdose does not predict severity of liver injury. Am J Emerg Med. 2024;79:52-57. doi:10.1016/j.ajem.2024.02.011
Category: Gastrointestional
Keywords: analgesia (PubMed Search)
Posted: 7/10/2024 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
I don't know about you, but I'm always eager to hear new and alternative methods of pain control…
This study examined the effectiveness of transcutaneous electrical nerve stilumlation (TENS) in patients with abdominal pain. Patients were randomized to TENS or sham applied to the abdomen. The primary outcome of interest was change in pain score 30 min after the intervention, and secondary outcome was percentage of patients requiring rescue analgesia. Pain scores were measured on a verbal numeric score scale with a range from 0 to 10, with any adult patients with a minimum score of 5 being eligible.
The mean reductions in pain scores after the intervention were also similar in patients treated with TENS and sham TENS (1.9 vs. 1.7 respectively, p = 0.81). THe use of rescue analgesia was 49% in patients treated with TENS and 51% in those who received sham TENS (p=0.66). No adverse events were noted.
The authors did note that there is a challenge in blinding due to toeh absence of electrical stimulation in the sham group; nonetheless, TENS was not found to be more effective than sham. It also did not reduce the need to rescue analgesia.
Guess I'll keep looking…
McMahon B, Prabhu A, Thode HC Jr, Singer A. Transcutaneous electrical nerve stimulation (TENS) versus sham TENS in adult ED patients with abdominal pain: A clinical trial. Am J Emerg Med. 2024;76:7-12. doi:10.1016/j.ajem.2023.10.035
Category: Gastrointestional
Keywords: antibiotics appendicitis (PubMed Search)
Posted: 6/12/2024 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
By now, most of us are aware that there's evidence supporting the use of an antibiotics-only approach for acute uncomplicated appendicitis. One of the major trials evaluating this is the Appendicitis Acuta II Trial. Our paper today continued longitudinal follow up of the original cohort enrolled in this study.
Patients were randomized to receive either oral antibiotic monotherapy (moxifloxacin 400 mg/d x 7 days) or IV and oral antibiotics (IV ertapenem 1 g/d x 2 days plus oral levofloxacin 500 mg/d + metronidazole500 mg q8h x 5 d).
Primary endpoint: resolution of acute appendicitis and hospital discharge without surgery and no reoccurence at time of follow up (3 years later).
There were 582 patients in the three year follow up cohort; Success was 63.4% (1-sided 95% CI, 58.8% to ?) in the oral antibiotics only group and 65.2% in the IV + oral antibiotics(1-sided 95% CI, 60.5% to ?). The difference in success rate was -1.8% (1-sided 95% CI, ?8.3 percentage points to ?; P?=?.14 for noninferiority).
No significant difference in secondary endpoints, including treatment-related adverse events, quality of life, length of hospital stay, and length of sick leave.
In this secondary analysis of the three year cohort from the APPAC II trial, there was a slightly higher appendectomy rate in patients who received oral antibiotic therapy; noninferiority of this regimen (as composed to combined) could not be demonstrated.
Selänne L, Haijanen J, Sippola S, et al. Three-Year Outcomes of Oral Antibiotics vs Intravenous and Oral Antibiotics for Uncomplicated Acute Appendicitis: A Secondary Analysis of the APPAC II Randomized Clinical Trial. JAMA Surg. Published online April 17, 2024. doi:10.1001/jamasurg.2023.5947
Category: Gastrointestional
Keywords: CT, contrast (PubMed Search)
Posted: 5/8/2024 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
Oftentimes, CT imaging is used in diagnosis of emergent abdominal pathology. However, there may be instances where there is hesitancy to use IV contrast, whether due to patient factors or extrinsic factors (remember the contrast shortage during covid?)
This study examines the diagnostic accuracy of dry CT. 3 quaternary centers with residency training programs participated, and contrasted images underwent further processing to remove any IV or oral contrast. Both residents and faculty reviewed the images, and findings were compared to both the initial read by radiologist as well as independent reads by a panel of experts. They looked for both primary findings (those that explained the abdominal pain) as well as actionable secondary findings (ie incidental findings requiring additional imaging or further management).
When compared to contasted imaging, the accuracy of dry CT was 70% (faculty, 68% to 74%; residents, 69% to 70%). Faculty had higher accuracy than residents for primary diagnoses but lower accuracy for actionable secondary diagnoses.
Thus when considering the necessity of contrast, please consider the potential for missed diagnosis.
Shaish H, Ream J, Huang C, et al. Diagnostic Accuracy of Unenhanced Computed Tomography for Evaluation of Acute Abdominal Pain in the Emergency Department. JAMA Surg. 2023;158(7):e231112. doi:10.1001/jamasurg.2023.1112
Category: Gastrointestional
Keywords: ED recidivism, abdominal pain, follow up appointments (PubMed Search)
Posted: 2/14/2024 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
How many times have you discharged a patient with a clinical impression of “abdominal pain” with no clear explanation or diagnosis?
How many of these times do you direct them to follow up with gastroenterology? And more importantly, how often do they actually do so?
This study discussed a multi-disciplinary approach to ensuring adequate follow up for patients, utilizing an EMR based transition of care (TOC) program. The study stratified patients into 2 groups, pre and post TOC program implementation, to assess rates of appointment scheduling and attendance, as well as rates of return to ED within 30 days. Patients were further stratified based on their Distressed Communities Index (DCI) score (a composite of 7 different socioeconomic metrics) into 5 tiers: Distressed Communities, At Risk Communities, Mid-Tier Communities, Comfortable Communities, and Prosperous Communities. Prior to the implementation of the TOC program, the onus was on the patient to schedule their appointment. The TOC program consisted of an order placed in EMR, which triggered review of the patient's chart by the gastroenterology attending or NP. This individual would then message the information to the appropriate GI subspecialty clinic, along with a time frame in which the patient should be seen. The clinic would then check the patient's insurance reach out to the patient directly to schedule the appointment.
While there was no signifcant difference in 30-day readmission between the pre and post TOC program patients, the post-implementation group was found to both schedule appointments (50% vs 27% p-value <0.01) AND show up to appointments (34% vs 24% p-value <0.01) at significantly higher rates compared to Pre-TOC patients. Additionally, post-TOC patients in the At-Risk and Distressed DCI groups were 22x more likely to follow up than the same groups in the pre-TOC group (OR 22.18, 95% CI 4.23–116.32).
Though the study had promising results, it did admittedly have some limitations, namely the size of the at-risk and distressed groups. Another consideration, though not mentioned in the paper, is that access to a working phone is necessary to the success of this program. Nevertheless, the idea of a TOC program is worth consideration as a means to ensure that patients are not lost to follow up and potentially reduce the risk of adverse events.
Mizrahi J, Marhaba J, Buniak W, Sun E. Transition-of-care program from emergency department to gastroenterology clinics improves follow-up. Am J Emerg Med. 2023;69:154-159. doi:10.1016/j.ajem.2023.04.030
Category: Gastrointestional
Posted: 1/10/2024 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
This retrospective cohort study examined patients over a one year period to evaluate factors associated with unfavorable outcomes in acute abdominal pain.
Unfavorable outcomes were defined as any of the following: 1) shock requiring an invasive procedure such as central line insertion or mechanical ventilation 2) emergency surgery 3) post-operative complications OR 4) in-hospital cardiac arrest
951 patients were included in the study.
Physical exam and laboratory signs associated with the above unfavorable outcomes included:
-diastolic BP < 80 mmHG
-RR ? 24/min
-RLQ tenderness
-abd distension
-hypoactive bowel sounds
-presence of specific abdominal signs (ie Murphy's sign, psoas sign, etc).
-leukocytosis
-ANC >75%
Further, ED Length of Stay of > 4 hours was also associated with unfavorable outcomes.
Food for thought when considering serial abdominal exams when diagnosis is unclear…
Dadeh AA. Factors associated with unfavorable outcomes in patients with acute abdominal pain visiting the emergency department. BMC Emerg Med. 2022 Dec 6;22(1):195. doi: 10.1186/s12873-022-00761-y. PMID: 36474160; PMCID: PMC9727909.
Category: Gastrointestional
Keywords: NG Tube (PubMed Search)
Posted: 11/9/2023 by Neeraja Murali, DO, MPH
Click here to contact Neeraja Murali, DO, MPH
Think before placing a nasogastric tube!
Multiple articles which discussed complications of NGT placement were included in this integrative review, with the majority (n=67) publishing results in English. The authors categorized adverse events into two broad categories:
1) Mechanical adverse events - including respiratory, esophageal, and pharyngeal complications, obstructed tube, intestinal and intracranial (!) perforation, and tube withdrawal
-The largest cohort (n=44) was respiratory, with displacement or placement of tube to the respiratory tract
2) Others - pressure injury and misconnection
-One study showed pressure related injury in 25%, and 5 articles discussed complications of misconnection (including extravasation of gastric fluids and inadvertent connection to central venous catheters)
16 of the 69 studies reported death as a consequence of improper placement.
One big takeaway: there is no universally accepted standard for verificaiton of tube placement. Xray is considered to be *most* accurate. Tubes should also be checked periodically and depth should be marked. Evidence-based guidelines need to be developed to improve patient safety, outcomes, and quality of care.
Motta APG, Rigobello MCG, Silveira RCCP, Gimenes FRE. Nasogastric/nasoenteric tube-related adverse events: an integrative review. Rev Lat Am Enfermagem. 2021 Jan 8;29:e3400. doi: 10.1590/1518-8345.3355.3400. PMID: 33439952; PMCID: PMC7798396.
Category: Gastrointestional
Keywords: acute diverticulitis (PubMed Search)
Posted: 10/11/2023 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
Diverticular disease is a common condition, with 60% of individuals over age 80 and 30% of those over age 45 (!) having diverticula. Recent estimates show that 10-25% of this subset with suffer at least one episode of acute diverticulitis in their lifetime. Fortunately, the majority of these cases are uncomplicated. This study provides evidence that outpatient treatment of acute diverticulitis is reasonable.
Study Design:
The DINAMO study was a multicenter randomized open-label non-inferiority trial evaluating the utility of antitbiotics in uncomplicated diverticulitis. The study included adult patients with uncomplicated diverticulitis without significant comorbities. The diagnosis was based on modified Neff classification with patients with a mNeff of 0 being included. Eligible patients were randomized to one of two treatment groups:
1) 600 mg ibuprofen q 8 h alternating with 1000 mg of acetaminophen q 8 h x7 d (Exerimental arm) OR
2) 875/125 mg amoxicillin/clavulanate q 8 h x 7 d in addition to the above (Control arm)
Outcomes of interest and Results:
Any patients who returned to the hospital underwent repeat CT. Primary of outcome of interest was admission to the hospital on revisit, with secondary outcomes being revisit itself, follow up, pain control, and recovery
There was no statistically significant difference in any of these (for numbers, please refer to article 1 linked below); further, no patients required emergency surgery.
Implications:
There is a low likelihood ot treatment failure when antibiotics are avoided in acute uncomplicated diverticulitis. This study finds this treatment regimen ot be noninferior to antibiotic treatment in terms of hospital admission, revisit rates, and recovery. Consider this treatment regimen in eligible patients.
https://journals.lww.com/annalsofsurgery/fulltext/2021/11000/efficacy_and_safety_of_nonantibiotic_outpatient.37.aspx
https://onlinelibrary.wiley.com/doi/10.1111/codi.12449
Category: Gastrointestional
Keywords: appendicitis, delayed operating room, appendectomy (PubMed Search)
Posted: 9/17/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This Scandinavian study from the Lancet says yes. They randomized 1800 patients over age 18 to appendectomy either within 8 hours or 24 hours and found no difference in perforation rate or other complications.
Karoliina Jalava, Ville Sallinen, Hanna Lampela, Hanna Malmi, Ingeborg Steinholt, Knut Magne Augestad, Ari Leppäniemi, Panu Mentula,
Role of preoperative in-hospital delay on appendiceal perforation while awaiting appendicectomy (PERFECT): a Nordic, pragmatic, open-label, multicentre, non-inferiority, randomised controlled trial,
The Lancet, 2023
Category: Gastrointestional
Keywords: Appendicitis (PubMed Search)
Posted: 8/13/2023 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
In recent years, there has been an uptick in non-operative management of acute appendicitis. This study examins outcomes in older patients (>65 years old).
The study authors evaluated retrospective data and included 474845 patients in the US with acute uncomplicated appendicitis betwen 10/2021 and 04/2022. All participants survived at least 24 hours postoperatively and none carried a diagnosis of inflammatory bowel disease; there were 43,846 patients treated nonoperatively and 430,999 who underwent appendectomy. The primary outcome was incidence of post-treatment complications, with secondary outcomes of mortality, length of stay, and inpatient costs.
In patients 65+, there was a 3.72% decrease in risk of complications, 1.82% increase in mortality, and increased LOS and costs.
Ultimately, operative management of acute appendicits was associated with reduced mortality, length of stay, and costs across all adult patients. While nonoperative management remains an option in the treatment of acute appendicits, surgical management continues to be the accepted standard.
Meier J, Stevens A, Bhat A, Berger M, Balentine C. Outcomes of Nonoperative vs Operative Management of Acute Appendicitis in Older Adults in the US. JAMA Surg. 2023;158(6):625–632. doi:10.1001/jamasurg.2023.0284
Category: Gastrointestional
Keywords: POCUS, Appendicitis, Pregnancy (PubMed Search)
Posted: 7/3/2023 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
POCUS can be used to screen for appendicitis.
A recent study showed a sensitivity of 66.7% (CI 95% 47.1–82.7), and a specificity of 96.8% (CI 95% 83.3–99.9) during pregnancy, with the highest sensitivity in the first trimester.
2 methods to locate the appendix are:
1) have your patient point to the area where it hurts the most
2) perform a lawnmower technique over the right lower quadrant looking for the right psoas mucle and the iliac vessels. The appendix will usually be near these structures.
Sometimes it is easiest to use your curvilinear probe to identify an area of inflammation and then change to the linear probe for better visualization.
On ultrasound, appendicitis is defined as a non-compressible blind pouch with an outer diameter greater than 6 mm. On short axis the inflammed appendix will look like a target sign:
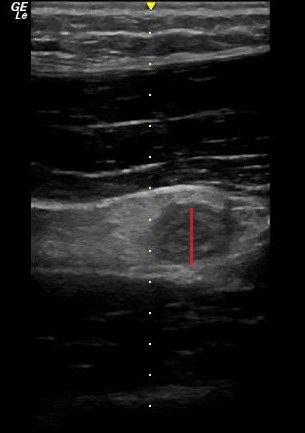
Abgottspon D, Putora K, Kinkel J, Süveg K, Widmann B, Hornung R, Minotti B. Accuracy of Point-of-care Ultrasound in Diagnosing Acute Appendicitis During Pregnancy. West J Emerg Med. 2022 Oct 23;23(6):913-918. doi: 10.5811/westjem.2022.8.56638
Category: Gastrointestional
Keywords: cannabis hyperemesis syndrome (PubMed Search)
Posted: 5/10/2023 by Neeraja Murali, DO, MPH
Click here to contact Neeraja Murali, DO, MPH
Bottom Line: With the increasing acceptance and legalization of marijuana and its derivatives, emergency departments have seen an increase in patients with cannabis hyperemesis syndrome (CHS). In this patient population, when other pathologies have been excluded, consider droperidol (0.625 mg – 2.5 mg) or haloperidol (0.05 mg/kg or 0.1 mg/kg) for management of symptoms.
Two separate articles were reviewed for this pearl. One is a systematic review of existing literature, and the other is a randomized controlled trial.
The systematic review examined 17 existing studies, including case reports, RCTs, retrospective studies, and other systematic reviews. This included adults aged 18-85 who were using recreational or medicinal cannabinoids. There was a consensus that cessation of cannabinoid use is the best way to alleviate symptoms of CHS. Other options discussed include:
As mentioned above, the HaVOC study examined various doses of haloperidol versus odansetron. This randomized controlled trial was triple blinded and had three groups: haloperidol 0.05 mg/kg or 0.1 mg/kg or odansetron 8 mg IV. The outcome of interest was reduction in abdominal pain and nausea at two hours after treatment. Either dose of haloperidol was found to be superior to odansetron, with improvements in pain and nausea (54% versus 29%; 95% CI -16% to 59%), and less use of rescue antiemetics (31% versus 59%, with 95% CI -61% to 13%). Haloperidol also resulted in shorter ED length of stay (3.1 h vs 5.6 h, 95% CI 0.1-5.0 h, p=0.03). However, 2 patients in the high dose haloperidol group had dystonic reactions precipitating return visits. The study does not specifically discuss differences in outcomes between the high and lower dose haloperidol groups.
Neither paper discussed the best alternatives when QTc prolongation is of concern. Clinicians should use their best judgment and the available information when deciding on a treatment option.
Senderovich H, Patel P, Jimenez Lopez B, Waicus S. A Systematic Review on Cannabis Hyperemesis Syndrome and Its Management Options. Med Princ Pract. 2022;31(1):29-38. doi:10.1159/000520417
Ruberto AJ, Sivilotti MLA, Forrester S, Hall AK, Crawford FM, Day AG. Intravenous Haloperidol Versus Ondansetron for Cannabis Hyperemesis Syndrome (HaVOC): A Randomized, Controlled Trial. Ann Emerg Med. 2021;77(6):613-619. doi:10.1016/j.annemergmed.2020.08.021
