Category: Ultrasound
Keywords: POCUS, resident education, ultrasound guided nerve blocks (PubMed Search)
Posted: 2/1/2026 by Alexis Salerno Rubeling, MD
(Updated: 2/2/2026)
Click here to contact Alexis Salerno Rubeling, MD
Ultrasound Guided Nerve Blocks (UGNBs) provides targeted analgesia that can effectively alleviate pain from injuries or painful procedures while reducing opioid use.
In 2021, ACEP issued a policy statement affirming that ultrasound-guided regional anesthesia is within the scope of EM physicians and is a core component of multimodal pain management pathways in the ED. However, EM residencies have not uniformly defined nerve block requirements, resulting in a wide range of graduating resident skill levels. Recent ACGME updates may help standardize expectations and address this gap.
A recent review of the National Ultrasound-Guided Nerve Block Registry (NURVE) looked at the impact of operator training level on the analgesic effectiveness of ED-performed UGNBs. The most commonly performed block among attendings was the erector spinae block, while for residents it was the fascia iliaca block. Both resident and attending performed blocks showed a reduction in pain but there was an 80.7% meaningful pain reduction in attendings as compared to 63.4% for residents. Out of the 1595 nerve block cases reviewed there were only 2 complications which included transient episode of LAST and respiratory difficulty from suspected diaphragmatic hemiparesis.
These findings highlight the importance of experience while supporting the safety and effectiveness of UGNBs performed by supervised residents in the training environment.
Macias M, Driver L, Riscinti M, Dreyfuss A, et al. Training level and analgesic outcomes of ultrasound-guided nerve blocks in the emergency department: An analysis from the NURVE block registry, The American Journal of Emergency Medicine, 2026 doi.org/10.1016/j.ajem.2026.01.050.
Category: Ultrasound
Keywords: knee effusion, ultrasound, method (PubMed Search)
Posted: 1/21/2026 by Kerith Joseph, MD
(Updated: 1/22/2026)
Click here to contact Kerith Joseph, MD
Study Overview
Title: Identification of Knee Effusions With Ultrasound: A Comparison of Three Methods
Design: Prospective cohort study
Setting: Outpatient orthopaedic clinic
Participants: 52 adults (104 knees), including 57 painful knees
Objective
Determine whether two simple dynamic techniques improve ultrasound detection of suprapatellar knee effusions compared with static scanning.
Ultrasound Methods Compared
Static scanning: Patient relaxed; standard long- and short-axis views.
Parapatellar pressure (Method 1): Examiner compresses medial and lateral parapatellar recesses during scanning.
Quadriceps contraction (Method 2): Patient actively contracts quadriceps during scanning.
Outcome Measure
Presence of fluid in the suprapatellar recess (graded using a standardized ultrasound effusion scale).
Key Results
Effusions detected:
Static scanning: 45
Parapatellar pressure: 58
Quadriceps contraction: 77
Comparative performance:
Quadriceps contraction was superior to parapatellar pressure for detecting:
All effusions (PR 1.33; P < 0.001)
Painful knees (PR 1.24; P = 0.036)
Painless knees (PR 1.50; P = 0.006)
Both dynamic methods outperformed static scanning.
Additional detection beyond static scanning:
Parapatellar pressure: +16.9% of knees
Quadriceps contraction: +54.2% of knees
Reliability (Inter-rater Agreement)
Static scanning: ? = 0.771
Parapatellar pressure: ? = 0.686
Quadriceps contraction: ? = 0.846
All methods showed high reliability, with quadriceps contraction highest.
Conclusions
Both parapatellar pressure and patient-initiated quadriceps contraction significantly improve ultrasound detection of suprapatellar knee effusions.
Quadriceps contraction is the most effective method, especially for small or occult (grade 1) effusions.
Category: Ultrasound
Keywords: POCUS, GI, Hernia (PubMed Search)
Posted: 1/19/2026 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
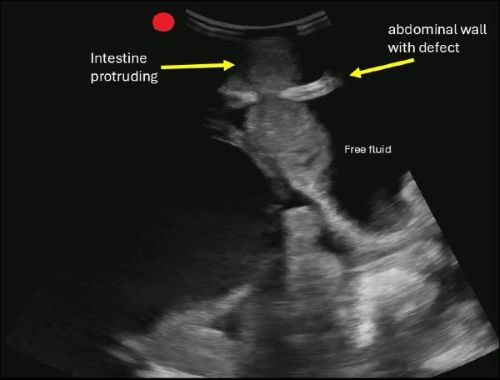
POCUS can help you identify signs of a hernia.
Begin by asking the patient to localize the point of maximal tenderness, then place a linear or curvilinear transducer over the area of concern. If there is concern for an inguinal hernia, you can have the patient perform a Valsalva maneuver while holding the probe in the area to evaluate dynamic changes.
A hernia is diagnosed when omental fat or intestinal contents are seen protruding through a defect in the abdominal wall.
If you are concerned about an incarcerated hernia, sonographic findings may include absence of peristalsis, presence of surrounding free fluid, with preserved blood flow on color Doppler. If a hernia progresses to strangulation, you may notice the absence of flow on color and power Doppler.
Boccatonda A, Brighenti A, Tiraferri V, Doglioli M, Iazzetta L, De Meis L, Safai Zadeh E, Dietrich CF, Serra C. POCUS for acute abdominal pain: practical scan protocols on gastrointestinal diseases and an evidence review. J Ultrasound. 2025 Dec;28(4):851-871. doi: 10.1007/s40477-025-01088-7.
Category: Ultrasound
Keywords: POCUS, arterial occlusion, limb ischemia (PubMed Search)
Posted: 1/5/2026 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
POCUS can be a valuable tool for screening both peripheral venous and arterial pathology.
If you suspect critical limb ischemia, you can use a similar approach to venous evaluation to assess for arterial occlusion.
Evaluate for:
Conclusion: POCUS can expedite diagnosis and resources prior to definitive testing with CT angiography.
Gonzalez AA, Brenner DS. Arterial Thrombosis Diagnosed With Point-of-Care Ultrasound. Cureus. 2024 Sep 13;16(9):e69357. doi: 10.7759/cureus.69357.
Frederick MK, Stolz LA, Duran-Gehring PE. Vascular Ultrasound. Emerg Med Clin North Am. 2024 Nov;42(4):805-818. doi: 10.1016/j.emc.2024.05.011.
Drake A, Dreyer N, Hoffer M, Boniface K. Point-of-care Ultrasound for the Evaluation of Acute Arterial Pathology in the Emergency Department: A Case Series. Clin Pract Cases Emerg Med. 2022 Feb;6(1):1-7. doi: 10.5811/cpcem.2021.11.54904.
Category: Ultrasound
Posted: 12/3/2025 by Kerith Joseph, MD
(Updated: 12/21/2025)
Click here to contact Kerith Joseph, MD
Clinically Oriented Takeaway
A single-view posterior POCUS can reliably identify anterior shoulder dislocation using the **Glenohumeral Separation Distance (GhSD)**—a simple measurement of the posterior alignment of the humeral head and glenoid.
How to Use It
Place a linear probe transversely on the posterior shoulder.
Identify the most posterior aspect of the humeral head and glenoid.
Measure the vertical offset (GhSD):
GhSD > 0 cm ? Normal alignment
GhSD < 0 cm ? Anterior dislocation
GhSD = 0 cm ? Borderline; treat as suspicious
Clinical Implications
Even minimally trained operators achieved 100% sensitivity and specificity in detecting anterior dislocation using this method.
POCUS can:
Enable rapid diagnosis when radiography is delayed.
Confirm reduction immediately at bedside, especially valuable when sedation is used.
Potentially reduce ED length of stay and radiation exposure.
Limitations to Consider
Not validated for posterior dislocations.
Does not assess associated injuries (fractures, Hill-Sachs, Bankart lesions).
Findings based on novice sonographers; performance among clinicians likely equal or better but still needs broader validation.
Single-center, small convenience sample.
No posterior dislocations occurred; technique not validated for them.
Novice sonographers could not be fully blinded to shoulder appearance.
Category: Ultrasound
Keywords: dental infection; POCUS (PubMed Search)
Posted: 12/15/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
Dental pain is a common reason for emergency department visits. These patients often experience prolonged length of stay and additional radiation exposure while awaiting CT imaging of the face. A recent case study highlights the potential role of POCUS in evaluating suspected dental abscesses.
In this report, clinicians used a high-frequency linear probe placed externally along the jawline. By orienting the probe to visualize the bony cortex of the mandible or maxilla and the dental root insertion, they identified a hypoechoic collection abutting the bone. When absent on the contralateral side and interpreted in the appropriate clinical context, this finding can suggest an abscess.
For further details, including imaging examples and technique demonstrations, see the referenced article and supplemental videos.
Hoffer JT, Park R, Brenner DS. "Is My Face Swollen?"-Utilizing Point-of-Care Ultrasound to Diagnose Odontogenic Infections. J Emerg Med. 2025 Oct 25;80:165-176. doi: 10.1016/j.jemermed.2025.10.032.
Category: Ultrasound
Posted: 12/3/2025 by Kerith Joseph, MD
(Updated: 12/4/2025)
Click here to contact Kerith Joseph, MD
Summary
Objective:
The study aimed to determine how a brief educational intervention could enable emergency medicine (EM) residents to use point-of-care ultrasound (POCUS) effectively to diagnose and manage shoulder dislocations in the emergency department (ED).
Methods:
Conducted at an academic teaching hospital in Miami, Florida.
Twenty EM residents (PGY1–PGY4) with no prior shoulder ultrasound training participated.
Residents received <1 hour of in-service training, including a short lecture, video instruction, and hands-on practice using a Sonosite M-Turbo ultrasound device.
Over one year (2016–2017), residents prospectively enrolled 78 adult patients with suspected shoulder dislocation.
POCUS findings were compared with x-rays (the gold standard) for accuracy.
Time to diagnosis and reduction confirmation were recorded.
Results:
55 of 78 patients were diagnosed with dislocation; 53 anterior, 1 posterior, 1 inferior.
POCUS achieved 100% sensitivity and specificity for diagnosing and confirming successful reductions compared to x-ray.
Ultrasound results were available ~22 minutes faster for diagnosis and ~27 minutes faster for reduction confirmation than x-rays (p < 0.0001).
Residents across all training years performed equally well.
POCUS also identified 14 fractures (12 confirmed by x-ray, 2 seen only on ultrasound).
Discussion:
A short educational session enabled residents to accurately use POCUS for shoulder dislocation diagnosis and management.
POCUS reduced diagnostic time, avoided radiation exposure, and may improve ED workflow and patient comfort.
Findings support including shoulder ultrasound as a core component of EM training, filling a current gap in national ultrasound education guidelines.
Limitations:
Convenience sample and single-center design.
Some selection bias and inherent limitations of POCUS-based studies.
Conclusion:
Emergency medicine residents can learn to diagnose and manage shoulder dislocations with excellent accuracy after brief ultrasound training. POCUS should be integrated into EM residency curricula as a core skill for musculoskeletal emergencies.
Category: Ultrasound
Keywords: POCUS, testicular pain (PubMed Search)
Posted: 12/1/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
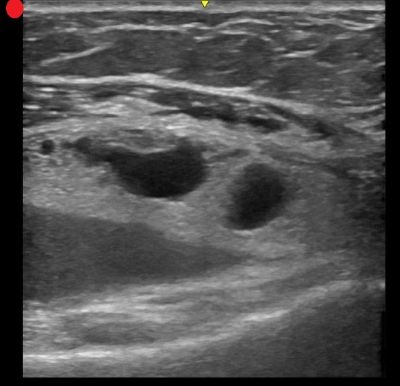
POCUS can be performed at the bedside to evaluate for acute scrotal conditions, including testicular torsion and inflammatory processes such as epididymo-orchitis.
A high-frequency linear transducer is typically used to scan the scrotum in two different planes. Additionally, a coronal "buddy view"—displaying both testes side by side—can aid in comparing echogenicity and vascularity.
On B-mode imaging, both testicular torsion and inflammatory conditions may present with testicular swelling and decreased homogeneity. However, color and power Doppler imaging can help to differentiate:
Inflammatory conditions (e.g., epididymo-orchitis) typically show increased vascular flow on color and power Doppler.
Testicular torsion usually demonstrates reduced or absent flow in the affected testis. However, in cases of intermittent torsion-detorsion, vascular flow may appear preserved or even increased. In such scenarios, repeat Doppler imaging after one hour may help clarify the diagnosis.
Kumar K, Kumari M, Kumar V, Suman SK. Evaluation of Scrotal Pathologies by Ultrasound and Color Doppler. Cureus. 2023 Mar 27;15(3):e36776. doi: 10.7759/cureus.36776
Acuña JG, Adhikari SR. Small Parts – Testicular Ultrasound. Sonoguide. American College of Emergency Physicians. Published April 1, 2025. Accessed December 1, 2025. https://www.acep.org/sonoguide/advanced/testicular
Category: Ultrasound
Keywords: Ultrasound, APPLES, bursa (PubMed Search)
Posted: 11/4/2025 by Kerith Joseph, MD
(Updated: 11/6/2025)
Click here to contact Kerith Joseph, MD
Summary:
This study evaluated whether the line-of-sight approach improves the speed and accuracy of ultrasound-guided needle placement into the subdeltoid bursa among novice operators, compared to the side approach. A secondary aim was to assess the usefulness of the APPLES mnemonic (Angle, Position, Perpendicular, Line up, Entry, Sweep) as a teaching aid.
Methods:
Medical students and residents were randomized to perform the procedure using both approaches in a crossover design. Two blinded reviewers measured procedure time, and participants completed a survey on their preferences and perceptions of APPLES. Statistical tests (paired t test, McNemar test) compared performance time and accuracy.
Results:
The line-of-sight approach significantly reduced procedure time (mean 14.4 s vs. 18.6 s; P = .00029).
Participants were more likely to hit the target within 30 s using the line-of-sight approach (P = .035).
72.7% preferred the line-of-sight approach.
88.2% found the APPLES mnemonic helpful.
Conclusions:
The operator’s positioning plays a key role in ultrasound-guided procedures. The line-of-sight approach improves both speed and accuracy for novice users, and the APPLES mnemonic is a valuable educational tool for teaching these techniques.
Kerith Joseph MD, RMSK
Clinical Associate Professor
University of Maryland School of Medicine
Baltimore Veterans Affairs Medical Center, Emergency Department
Category: Ultrasound
Keywords: POCUS; Pediatrics; Cardiology; left ventricular function (PubMed Search)
Posted: 11/3/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
E-point septal separation (EPSS)—the distance between the anterior mitral valve leaflet and the interventricular septum during early diastole—is a well-established marker of left ventricular (LV) systolic function in adults. A threshold of 7.0 mm is commonly used to screen for severely depressed LV function. But how well does this cutoff translate to pediatric populations?
A recent retrospective study set out to explore this very question. Researchers reviewed 770 pediatric echocardiograms, including 148 with abnormal LV function and a 4:1 random sample of normal studies. Using post-exam ultrasound software, blinded operators measured EPSS across three age groups: 0-3 years, 4-12 years and 13-18 years.
Results:
Among children with LV systolic dysfunction, EPSS values increased progressively with severity:
When applying the adult 7.0 mm threshold: Sensitivity: 76.4% (95% CI: 68.5–82.8%) Specificity: 95.8% (95% CI: 93.8–97.2%)
However, the study-derived optimal threshold of 6.0 mm improved sensitivity to 81.8% (95% CI: 74.4–87.4%) while maintaining high specificity at 91.4% (95% CI: 88.9–93.5%).
Special Consideration for the Youngest Patients
In children aged 0–3 years, a lower threshold of 4.9 mm outperformed the adult cutoff: Sensitivity at 4.9 mm: 77.8% (95% CI: 51.9–92.6%) vs sensitivity at 7.0 mm: 55.6% (95% CI: 31.3–77.6%)
While these findings are promising, further research is needed to validate EPSS thresholds in emergency department (ED) settings using point-of-care ultrasound (POCUS), and to assess their feasibility in real-time clinical workflows.
Bottom Line: For older children an EPSS threshold of 7.0 mm appears to be accurate in identifying children with LV systolic dysfunction, but a lower threshold may be needed for children ages 0-3. Further studies are needed.
Chen E, Ramgopal S, Lorenz D, Jone PN, Horowitz R. Use of e-point septal separation to screen for left ventricular function in children. Am J Emerg Med. 2025 Sep 6;99:39-45. doi: 10.1016/j.ajem.2025.09.013
Category: Ultrasound
Keywords: CPR, POCUS, pulse checks (PubMed Search)
Posted: 10/6/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
A recent systematic review compared the timing and diagnostic accuracy of manual pulse check versus point-of-care ultrasound (POCUS) pulse checks (this means placing an ultrasound probe on the carotid or femoral artery to evaluate for a doppler pulse).
The review included seven studies encompassing a total of 469 patients.
Six of the studies assessed the duration of pulse checks, revealing a mean time difference of –1.39 seconds (95% CI: –2.20 to –0.57) in favor of ultrasound.
Three of the studies reported the sensitivity and specificity of POCUS pulse checks, yielding pooled estimates of 99% sensitivity (95% CI: 87%–100%) and 96% specificity (95% CI: 85%–99%). In contrast, two studies evaluated manual pulse checks, with pooled sensitivity of 62% (95% CI: 22%–91%) and specificity of 91% (95% CI: 88%–93%).
As with many systematic reviews, the studies included demonstrated high heterogeneity and generally low methodological quality, indicating that further investigation may still be needed.
Neto ES, Scapin M, Lazaro-Paulina F, Campbell RL, Molinari DF, Kummer T. Duration of resuscitation interruption using point-of-care ultrasound versus traditional manual pulse check: A systematic review and meta-analysis. Am J Emerg Med. 2025 Aug 23;98:145-152. doi: 10.1016/j.ajem.2025.08.049.
Category: Ultrasound
Keywords: Bladder Ultrasound, Foley, POCUS (PubMed Search)
Posted: 9/3/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
If a patient is experiencing issues with their Foley catheter, consider using POCUS.
Using a curvilinear probe over the suprapubic region, you can obtain a transverse view of the bladder by orienting the marker towards the patient’s right side, or a sagittal view by orienting the marker towards the patient’s head.
In a properly functioning Foley, the bladder will appear decompressed, and you may only see the Foley balloon.
In cases of obstruction or malposition, you may notice a distended bladder. The next step is to attempt to visualize the Foley balloon. If you do not see a Foley balloon within the bladder, try deflating the balloon and advancing the catheter.
If you notice debris blocking the foley or heterogenous material in a patient with hematuria, you can attempt to flush the catheter, but if the patient has a large amount of hematuria, you may need to replace the current Foley with a three-way catheter for continuous bladder irrigation.
Boivin Z, Li JJ, Gottlieb M, Liu RB. Troubleshooting Foley Catheter Problems using Point-of-Care Ultrasound, Journal of Emergency Medicine (2025). doi.org/10.1016/j.jemermed.2025.07.049
Category: Ultrasound
Keywords: POCUS; Pulmonary Embolism; Cardiac Ultrasound; Doppler (PubMed Search)
Posted: 7/21/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
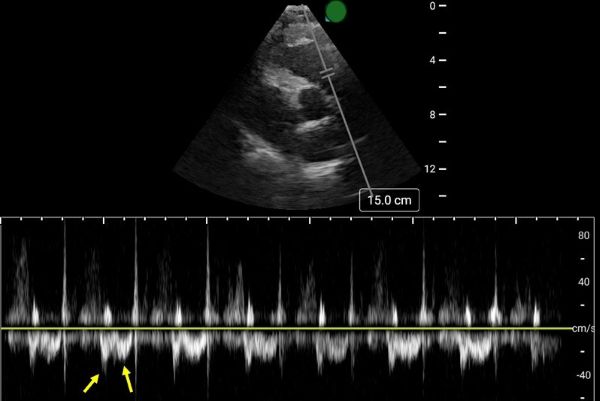
Early Systolic Notching and Pulmonary Embolism
A prospective multicenter study conducted across four academic emergency departments in Turkey evaluated the diagnostic accuracy of early systolic notching (ESN) in emergency department patients. Among the 183 patients included, 52.5% were diagnosed with pulmonary embolism (PE), while 19.7% exhibited the ESN finding. ESN demonstrated a sensitivity of 34% (95% CI: 25–45%) and a specificity of 97% (95% CI: 90–99%) for PE. Sensitivity increased to 69% in patients classified as high or intermediate-high risk. Overall, ESN exhibits moderate to high specificity but low sensitivity, consistent with other sonographic signs of PE. Notably, ESN may also be present in patients with chronic thromboembolic disease secondary to prior pulmonary hypertension.
How to Obtain ESN
To detect ESN, acquire a parasternal short axis view at the base of the heart to visualize the right ventricular outflow tract and pulmonic valve. Position the pulse wave Doppler gate just proximal to the pulmonic valve, with the cursor traversing the outflow tract. ESN is characterized by a sharp systolic spike with a notch, followed by a dome-shaped waveform
Aslaner MA, Karbek Akarca F, Aksu ?H, Yazla M, Can Ö, Ku? G, Çelik A, Özkan S, ?bze S, Yamano?lu A, Yaz?c? MM, Yürüktümen Ünal A, Demircan A. Diagnostic Accuracy of Early Systolic Notching in Pulmonary Embolism. J Ultrasound Med. 2022 Mar;41(3):637-644. doi: 10.1002/jum.15744.
Category: Ultrasound
Keywords: POCUS, MSK, finger injuries, nerve blocks (PubMed Search)
Posted: 7/7/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
Digital nerve blocks are commonly used to provide anesthesia for finger injuries such as lacerations and dislocations. However, the procedure can be painful, as it often requires multiple injections into sensitive areas.
A recent single-center, unblinded randomized study compared the subjective discomfort and analgesic efficacy of traditional digital nerve blocks with ultrasound-guided peripheral nerve blocks. The study included 106 patients, with 53 in each group.
Results showed that patients in the peripheral nerve block group reported higher satisfaction rates. They also experienced less pain during the initial injection and longer-lasting analgesia compared to those who received digital nerve blocks. While digital blocks had a faster onset of anesthesia, they were associated with a higher rate of block failure.
Chororia, Samata et al. Dorsal Digital Nerve Block vs. Ultrasound-Guided Selective Peripheral Nerve Block for Finger Analgesia: A Randomized Controlled Study. Journal of Emergency Medicine. Article in Press. doi: 10.1016/j.jemermed.2025.05.005.
Category: Ultrasound
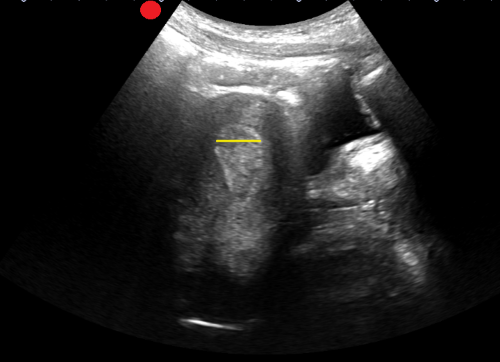
Keywords: POCUS, Hip Effusion, MSK (PubMed Search)
Posted: 6/16/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
A hip effusion can cause pain with leg movement in both pediatric and adult patients.
A recent multicenter, prospective study assessed the diagnostic accuracy of POCUS performed by pediatric emergency physicians in detecting hip effusion.
They found that POCUS had a sensitivity of 89.3% (95% CI 80.6 to 95.0%) and specificity of 99.2% (95% CI 97.0 to 99.9%).
To scan the hip:
-Position the patient supine with the patient’s hip externally rotated.
-Place the probe transversely across the patient’s leg with the marker towards the patient’s right and scan proximally.
-Upon reaching the proximal femur, rotate the probe marker so it points towards the patient’s umbilicus.
-Look for an anechoic stripe at the femoral neck, preceding the femoral head.
An anechoic stripe measuring at least 5 mm in the anterior synovial space or an asymmetry exceeding 2 mm compared to the opposite, asymptomatic hip is diagnostic for hip effusion in BOTH pediatric and adult populations.
Jones RM, Malia L, Snelling PJ, Riera A, Mak W, Moote D, Brimacombe M, Chicaiza H. Diagnostic Accuracy of Point-of-Care Ultrasound for Hip Effusion: A Multicenter Diagnostic Study. Ann Emerg Med. 2025 Jun 7:S0196-0644(25)00279-3. doi: 10.1016/j.annemergmed.2025.04.033. Epub ahead of print. PMID: 40481828.
Category: Ultrasound
Keywords: soft tissue; point of care ultrasound (PubMed Search)
Posted: 5/19/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
When evaluating foreign bodies in soft tissue, an imaging interface- such as a standoff pad- can improve imaging of superficial structures.
Common image interfaces include gel, commercial standoff pads, saline bags, and water baths.
Water baths are primarily used for imaging the hands and feet, but a recent study explored a water-filled patient belongings bag as a novel alternative. This method gives the benefit of the same elevated standoff that water baths provide, while accommodating larger extremities that may not fit in traditional setups.
The study found no significant difference between the patient belonging bag and a water bath for identifying a FB in a porcine model. Saline bags had the lowest image quality.
Vega C, Lindsay R, Shokraneh K, et al.. POCUS Standoff: Comparing Ultrasound Interfaces for Soft Tissue Foreign Body Imaging. Pediatric Emergency Care. 2025; 41 (5): 354-358. doi: 10.1097/PEC.0000000000003359.
Category: Ultrasound
Keywords: Point-of-care ultrasound; Cholecystitis; Gallbladder distention; Biliary ultrasound (PubMed Search)
Posted: 5/5/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
The normal gallbladder dimensions on ultrasound are approximately 3 cm in width by 10 cm in length.
A recent study evaluated the diagnostic test characteristics of gallbladder distension on POCUS for cholecystitis.
The authors conducted a retrospective cohort study of 227 patients who were admitted to the hospital after undergoing a POCUS biliary study in the emergency department.
They found the prevalence of gallbladder distension to be 30% in their study population. When combined with other sonographic findings, the presence of distension increased the specificity for cholecystitis to 95.6%.
Gallbladder wall distension was associated with the presence of an obstructing stone in the gallbladder neck and with acute cholecystitis.
Additionally, gallbladder wall distension was associated with longer operative times (mean 114 minutes) compared to those without distension (mean 89 minutes; p=0.03), suggesting more severe disease and potentially more complex surgical intervention.
Bottom Line: When gallbladder wall distension is present, it is important to carefully evaluate the gallbladder neck for signs of an obstructing stone.
Cannata D, Chin KA, Anslip A, et al. Association of biliary distention with a diagnosis of acute cholecystitis. Am J Emerg Med. 2024 Jul;81:130-135. doi: 10.1016/j.ajem.2024.04.056.
Category: Ultrasound
Keywords: POCUS; GI; Diverticulitis (PubMed Search)
Posted: 4/7/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
A recent systematic review and meta-analysis evaluated the diagnostic accuracy of ultrasound in detecting acute diverticulitis. The analysis included 12 studies with a total of 2,056 patients. Ultrasound demonstrated a sensitivity of 92.5% (95% CI: 86.9%–95.8%) and a specificity of 87.7% (95% CI: 75.7%–94.2%).
The most commonly used diagnostic criteria across the studies included:
Similar to prior research on POCUS for nephrolithiasis, these findings support a POCUS-first approach for patients at low risk for serious alternative diagnoses. Ultrasound is a great alternative for patients with contraindications to contrast-enhanced CT, such as those with contrast allergies.
As the authors state, while ultrasound may be effective in identifying acute diverticulitis and its complications, such as abscess, additional imaging with CT may still be required to assess the severity of complications.
Shokoohi H, Peksa GD, Hutchison A, Al Jalbout N, Montoya K, Westrick JC, Goldsmith A, Nazerian P, Gottlieb M. Ultrasound accuracy in acute diverticulitis: A systematic review and Meta-analysis. Am J Emerg Med. 2025 Mar 10;92:96-103. doi: 10.1016/j.ajem.2025.03.002.
Category: Ultrasound
Keywords: POCUS; MSK; fracture (PubMed Search)
Posted: 3/17/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
On ultrasound, lipohemarthrosis—the presence of blood and fat in the joint cavity—is a key clinical indicator of an intra-articular fracture.
Lipohemarthrosis appears as three distinct layers near the joint line.
Salerno A. Lipohemarthrosis. Floating fat in an intra-articular fracture. Visual Journal of Emergency Medicine. 2022, 26:101236.
Category: Ultrasound
Keywords: POCUS, OB, retained products of conception (PubMed Search)
Posted: 3/3/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
A recent study evaluated the accuracy of POCUS in detecting retained products of conception (RPOC) in the emergency department.
In this study, a patient was considered positive for RPOC if they had heterogenous material in the endometrium measuring 10 mm or more. Color Doppler was not used for further evaluation, though it has been cited in obstetric literature as a helpful tool.
Among the 265 patients included, the prevalence of RPOC was 21.5%. POCUS had a sensitivity of 79.0 % and a specificity of 93.8 %.
The authors caution against the use of POCUS to diagnose RPOC in the setting of early pregnancy, as the endometrium can have a variable appearance, increasing the risk of a misdiagnosis. Of the 22 false positives identified, more than half were potentially viable pregnancies. Uterine fibroids can also lead to a heterogenous appearance of the uterus and can be another potential false positive.
Boivin Z, Barber D, Chimileski B, et al. Accuracy of point-of-care ultrasound in diagnosing retained products of conception. Am J Emerg Med. 2025;90:65-70. doi:10.1016/j.ajem.2025.01.032.
