Category: Administration
Posted: 9/20/2025 by Kevin Semelrath, MD
(Updated: 2/8/2026)
Click here to contact Kevin Semelrath, MD
Systemic racism and institutional bias affect all aspects of medicine. This position paper from 2022 highlights some of the disparities present within the EM Clinical Ultrasound community. The authors identified several areas of concern regarding the make up of the leadership of the CU community, and importantly suggest several ways to create a more equitable specialty.
Javier Rosario, Resa E. Lewiss, Lori A. Stolz, Marina Del Rios, Josie Acuña, Srikar Adhikari, David Amponsah, Almaz S. Dessie, Michael Gottlieb, Robert D. Huang, Jodi Jones, Adaira Landry, Rachel B. Liu, Lorraine Ng, Nova L. Panebianco, Anthony J. Weekes, Starr Knight,
Creating a more racial-ethnic inclusive clinical ultrasound community,
The American Journal of Emergency Medicine,
Volume 54,
2022,
Pages 208-211,
ISSN 0735-6757,
https://doi.org/10.1016/j.ajem.2022.02.015.
(https://www.sciencedirect.com/science/article/pii/S0735675722000985)
Category: Pediatrics
Keywords: SCAN, abuse, physical, sexual, triage screening tool (PubMed Search)
Posted: 9/19/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
This was a European study examining a screening tool to be used in the ED to indicate the need for further investigation into the concern for possible abuse. Four questions were taken from other commonly used abuse screening tools that were used outside of the ED. SCAN questions are as follows:
Is the injury compatible with the history, and does it correspond to the child's developmental level?
Was there an unnecessary delay in seeking medical help?
Is the behavior/interaction of the child and caregivers appropriate?
Are there other signals that make you doubt the safety of the child or family?
Any positive answer triggered further evaluation, starting with a complete head to toe assessment and complete history with additional tests added as warranted. This is only a screening tool and positive answers do NOT mean that abuse has occurred, but should cause you to pause and think further.
These questions showed a "moderate" performance among close to 25000 patients and the questions were comparable in children < 5 years to other/longer screening tools used in Europe.
Hoedeman F, Puiman PJ, van den Heuvel EAL, Affourtit MJ, Bakx R, Langendam MW, van de Putte EM, Russel-Kampschoer IMB, Schouten MCM, Teeuw AH, de Koning HJ, Moll HA. A validated Screening instrument for Child Abuse and Neglect (SCAN) at the emergency department. Eur J Pediatr. 2023 Jan;182(1):79-87. doi: 10.1007/s00431-022-04635-0. Epub 2022 Oct 5. PMID: 36198865; PMCID: PMC9534589.
Category: EMS
Keywords: NRP, cardiac arrests, newly born, prehospital (PubMed Search)
Posted: 9/17/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
There is no standardized prehospital neonatal resuscitation curriculum for EMS. The Neonatal Resuscitation Program (NRP) guidelines focus on hospital based births which may not translate to the prehospital environment.
This study was prospective and observational that used a virtual, EMS tailored newborn resuscitation curriculum. Initially, 350 EMS clinicians watched a 90 min video. This was then modified based on their feedback to a 60 minute interactive curriculum specifically designed for EMS that emphasized NRP concepts and reinforced how NRP was different from pediatric resuscitation. 17 EMS jurisdictions viewed the program and were then given a brief NRP based quiz before, after and 3 months following the training.
Feedback was overall positive and post test and 3 month follow up test scores showed improvement from the pre test scores.
Standardized neonatal resuscitation education represents an area where improvements can be made in prehospital education. This particular curriculum was well received and improved EMS clinicians knowledge based. Jurisdictional medical directors should work with their department on standardized education for the neonatal population.
Also, stay tuned for updated NRP guidelines which are due to come out this fall.
Huynh TK, Smith JD, Neth M, Overton-Harris P, Daya MR, Guise JM, Meckler GD, Hansen ML. Virtual Neonatal Resuscitation Curriculum for Emergency Medical Services (EMS) to Improve Out-of-Hospital Newborn Care. Prehosp Emerg Care. 2025 Jan 28:1-7. doi: 10.1080/10903127.2025.2450074. Epub ahead of print. PMID: 39786751.
Category: Trauma
Keywords: TXA, EMS, prehospital, consensus (PubMed Search)
Posted: 9/14/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
The National Association of EMS Physicians, the American College of Surgeons Committee on Trauma, and the American College of Emergency Physicians recommends:
• Prehospital TXA administration may reduce mortality in adult trauma patients with hemorrhagic shock when administered after lifesaving interventions.
• Prehospital TXA administration appears safe, with low risk of thromboembolic events or seizure.
• The ideal dose, rate, and route of prehospital administration of TXA for adult trauma patients with hemorrhagic shock has not been determined. Current evidence suggests EMS agencies may administer either a 1-g intravenous/intraosseous dose (followed by a hospital-based 1-g infusion over 8 hours) or a 2-g intravenous/intraosseous dose as an infusion or slow push.
• Prehospital TXA administration, if used for adult trauma patients, should be given to those with clinical signs of hemorrhagic shock and no later than 3 hours post-injury. There is no evidence to date to suggest improved clinical outcomes from TXA initiation beyond this time or in those without clinically significant bleeding.
• The role of prehospital TXA in pediatric trauma patients with clinical signs of hemorrhagic shock has not been studied, and standardized dosing has not been established. If used, it should be given within 3 hours of injury.
• Prehospital TXA administration, if used, should be clearly communicated to receiving health care professionals to promote appropriate monitoring and to avoid duplicate administration(s).
• A multidisciplinary team, led by EMS physicians, that includes EMS clinicians, emergency physicians, and trauma surgeons should be responsible for developing a quality improvement program to assess prehospital TXA administration for protocol compliance and identification of clinical complications.
Barrett, Whitney J. MD; Kaucher, Kevin A. PharmD, BCCCP; Orpet, Ross E. MD; Campion, Eric M. MD; Goodloe, Jeffrey M. MD; Fischer, Peter E. MD, MS, NRP; Colwell, Christopher B. MD; Lyng, John W. MD, NRP. Tranexamic acid in trauma: A joint position statement and resource document of NAEMSP, ACEP, and ACS-COT. Journal of Trauma and Acute Care Surgery 99(3):p 357-363, September 2025. | DOI: 10.1097/TA.0000000000004727
Category: Orthopedics
Posted: 9/13/2025 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Epidural abscess
Likely the most serious missed emergent condition in patients diagnosed with non-specific back pain.
Challenging diagnosis to make in the ED
Almost half of patients are initially misdiagnosed and average two ED visits before the diagnosis is made.
At the time of diagnosis, the most common symptom is diffuse spine pain and the most common exam finding is severe local spinal tenderness.
Fever is only present in 30% to 50% of patients at presentation.
In one study, over 65% of patients with spinal epidural abscesses were afebrile on presentation.
Also, consider that the neurological examination is normal in two-thirds of patients at their first ED visit.
Category: Pharmacology & Therapeutics
Keywords: acute ischemic stroke, tenecteplase, thrombolytic, endovascular treatment, large?vessel occlusion (PubMed Search)
Posted: 9/11/2025 by Matthew Poremba
Click here to contact Matthew Poremba
Background:
Several trials have explored the use of IV thrombolysis before endovascular thrombectomy (EVT) in ischemic stroke patients, and a pooled analysis from these trials showed no significant difference in efficacy between intravenous thrombolysis plus EVT compared to EVT alone. However, only 2.2% of patients in the trials included in this pooled analysis received tenecteplase (TNK), with the vast majority of patients receiving alteplase. (1) While a 2018 trial showed improved early reperfusion and 90-day outcomes with TNK compared to alteplase before EVT, a recent target trial emulation analysis indicated no added benefit with TNK plus EVT over EVT alone. (2-3) Lack of comparison between TNK plus EVT versus EVT alone and small sample sizes of prior trials led to the design of the BRIDGE-TNK trial, which directly compared TNK plus EVT versus EVT alone in acute ischemic stroke. (4)
Study design:
This multi-center, randomized, open-label trial conducted at 39 hospitals in China included patients with large-vessel occlusion (LVO) of the internal carotid, middle cerebral or basilar artery on CTA or MRA imaging who presented within 4.5 hours of their last known well time, and were eligible to undergo intravenous thrombolysis and EVT.
Exclusion criteria were intracranial hemorrhage on CT or MRI imaging, rapidly improving symptoms at the discretion of the investigator, pre-stroke modified Rankin scale (mRS) of > 4, contraindication to imaging with contrast agents, patients who needed interhospital transfer before thrombectomy, any terminal illness such that the patient would not be expected to survive more than 1 year, any condition that could impost hazards to the patient if study therapy is initiated in the judgement of the investigator, hypodensity in >1/3 of middle cerebral artery or basilar artery territory on non-contrast CT, and pregnant women.
The primary outcome was functional independence at 90 days, defined as an mRS score of 0 to 2.
Patient Population:
Baseline characteristics were well matched between treatment arms:
Results:
Primary outcome:
Secondary outcomes:
Study Limitations:
Key Takeaways:
While rates of symptomatic intracranial hemorrhage and mortality were higher in the TNK + EVT group, neither of these outcomes met statistical significance and bridging with TNK prior to EVT led to increased rates of functional independence at 90 days compared to EVT alone. The findings of this study reinforce current guideline recommendations for not skipping intravenous thrombolysis prior to thrombectomy for LVO stroke.
1. Majoie CB, Cavalcante F, Gralla J, et al. Value of intravenous thrombolysis in endovascular treatment for large-vessel anterior circulation stroke: individual participant data meta-analysis of six randomised trials. Lancet 2023;402:965-74
2. Campbell BCV, Mitchell PJ, Churilov L, et al. Tenecteplase versus alteplase before thrombectomy for ischemic stroke. N Engl J Med 2018;378:1573-82
3. Altersberger VL, Kaesmacher J, Churilov L, et al. Bridging thrombolysis with tenecteplase versus endovascular thrombectomy alone for large-vessel anterior circulation stroke: a target trial emulation analysis. J Neurol Neurosurg Psychiatry. 2025;96(8):775-783. Published 2025 Jul 16. Doi:10.1136/jnnp-2024-335325
4. Qiu Z, Li F, Sang H, et al. Intravenous Tenecteplase before Thrombectomy in Stroke. N Engl J Med. 2025;393(2):139-150. doi:10.1056/NEJMoa2503867d
Category: Gastrointestional
Keywords: GI bleed, imaging (PubMed Search)
Posted: 9/10/2025 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
The TLDR:
In the ED setting, CTA for suspected GI bleeding is frequently ordered, but it’s finding less. At one center, use went up sevenfold over six years, while positive results dropped from 1 in 5 scans to about 1 in 16. Older patients are more likely to have a positive scan, and those with active cancer less so. CTA can be very useful when targeted, but widespread use may add cost, radiation, and crowding without improving care—so choosing patients carefully is key.
The longer version:
This was a retrospective cohort study involving adult patients who had undergone abdominal and pelvic CTA for suspected GIB at a large urban academic medical center between January 2017 and December 2023. The primary outcomes of interest were 1) The annual number and proportion of GIB-related CTAs among all CT scans performed in the ED, and 2) The diagnostic yield, defined as the percentage of CTAs that showed active bleeding or hemorrhage.
Findings:
CTA usage increased substantially: In 2017, there were 30 GIB-related CTAs out of 32,197 ED CT exams (0.09%). By 2023, this rose to 288 out of 44,423 (0.65%)
Diagnostic yield declined: In 2017, 6 of 30 CTAs were positive (20.0%). In 2023, only 18 of 288 were positive (6.3%)
Data of interest:
Later years (ie 2023 rather than 2017) were linked to lower odds of a positive CTA (odds ratio [OR] 0.84 per year; 95% CI, 0.73–0.96; P = .01). Older patients had higher odds of a positive result (OR 1.02 per year of age; 95% CI, 1.00–1.04; P = .02). Patients with active cancer had lower odds of positive findings (OR 0.35; 95% CI, 0.12–1.00; P = .05)
Discussion:
Despite the marked increase in CTA use for suspected GIB, its diagnostic effectiveness dropped sharply over the study period. The findings emphasize the need to balance the benefits (such as detecting active bleeding) with the downsides—including interpretation time, radiation exposure, costs, and ED crowding. The authors suggest implementing evidence-based protocols and decision-support tools to optimize CTA use in emergency settings to improve appropriateness and diagnostic yield.
Prasad S, Hood CM, Young C, et al. Computed Tomographic Angiography and Yield for Gastrointestinal Bleeding in the Emergency Department. JAMA Netw Open. 2025;8(8):e2529746. Published 2025 Aug 1. doi:10.1001/jamanetworkopen.2025.29746
Category: Critical Care
Keywords: Oxygenation, Lateral Positioning, Hypoxia (PubMed Search)
Posted: 9/9/2025 by Mark Sutherland, MD
(Updated: 2/8/2026)
Click here to contact Mark Sutherland, MD
We've got supine positioning and prone positioning... what about something in-between? Ye et al studied 2,159 patients coming out of anesthesia in a PACU after extubation. As sedation wore off, they placed one group in lateral decubitus, and left the other group supine. The lateral decubitus group had less hypoxia, a higher lowest SpO2, and required fewer airway rescue maneuvers.
Of note, the investigators didn't compare lateral or supine to prone positioning, which is often felt to be the best position for oxygenation (depending on patient characteristics and pathophysiology). And of course, this study represents a very specific scenario quite different from the ED (PACU patients post-extubation), so it's not clear how broadly extrapolatable this is. But this does add to the argument that supine is a poor position for oxygenating patients.
Bottom Line: If your supine patient is oxygenating marginally and you want a small bump without going all the way to prone positioning, consider lateral positioning. May make the most sense for procedural sedation and post-extubation patients in terms of similarity to this particular study.
Ye H, Chu LH, Xie GH, Hua YJ, Lou Y, Wang QH, Xu ZX, Tang MY, Wang BD, Hu HY, Ying J, Yu T, Wang HY, Wang Y, Ye ZJ, Bao XF, Wang MC, Chen LY, Wang XX, Zhang XB, Huang CS, Wang J, Lu YP, Luo FQ, Zhou W, Wang CG, Cheng H, Liu WJ, Luo J, Wu YQ, Li RR, Wang D, Hou LQ, Shi L, Zhang J, Wang K, Pi X, Zhou R, Yang QQ, Wan PL, Li H, Wu SJ, Song SW, Cui P, Shu L, Islam N, Fang XM. Effect of lateral versus supine positioning on hypoxaemia in sedated adults: multicentre randomised controlled trial. BMJ. 2025 Aug 19;390:e084539. doi: 10.1136/bmj-2025-084539. PMID: 40829895; PMCID: PMC12362200.
Category: Obstetrics & Gynecology
Posted: 9/7/2025 by Jennifer Wang, MD
(Updated: 9/8/2025)
Click here to contact Jennifer Wang, MD
Sickle cell disease is one of the notorious inherited blood disorders, with the abnormal hemoglobin shapes creating abnormal blood cells that can create clots and cause problems in just about every organ system - so it should surprise no one that this hold true in pregnancy.
Published just in June 2025, the below article looked retrospectively at Medicaid patients in California, Georgia, Tennessee, and Michigan from 2010-2018. In total, this study included 1286 patients, 90% of whom were Black. They followed ~800 of these patients for a year postpartum to look for the most common complications.
Aside from vaso-occlusive crisis being extremely common (~40% of patients experienced at least one crisis during or in the year after pregnancy), ~25% of patients with sickle cell had antepartum hemorrhage and preterm delivery, while ~10% had preeclampsia or eclampsia.
Keep in mind that this is a retrospective cohort study that did not have any comparisons, so this is really just observational data. While we can't draw any conclusions about just how much more dangerous sickle cell disease makes pregnancy, I think the numbers are concerning enough that we should keep an even closer eye than normal on our patients who have concurrent sickle cell and pregnancy.
Kayle M, Zhou M, Attell BK, et al. Pregnancy- and Disease-Related Morbidity Among Medicaid Enrollees With Sickle Cell Disease. Pediatr Blood Cancer. 2025;72(9):e31857. doi:10.1002/pbc.31857
Category: Trauma
Keywords: brain injury, intubation, best practice, hypoxia, hypotension (PubMed Search)
Posted: 9/6/2025 by Robert Flint, MD
(Updated: 9/7/2025)
Click here to contact Robert Flint, MD
These authors reiterate principles that have been discussed previously regarding intubation in head/brain injured patients.
-Avoid hypoxia with preoxygenation
-Avoid hypotension by fluid resuscitation/vasopressors/blood in the correct clinical setting
-Use hemodynamically neutral induction agents such as Etomidate or Ketamine (it is ok use this in head injured patients!)
-Video laryngoscope gives best first pass success which minimizes hypoxia/raised ICP
-Post-Intubation aim for eucapnia (avoid hyperventilation)
-Use adequate post-intubation sedation to avoid raised ICP
Category: Cardiology
Keywords: Hypertension, treatment, (PubMed Search)
Posted: 9/6/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
From this position statement on management of HTN key points are beta blockers are a second line medication choice, dual therapy in a combination pill is often warranted and primary medications should be thiazides, long acting calcium channel blockers, ACE or Arbs.
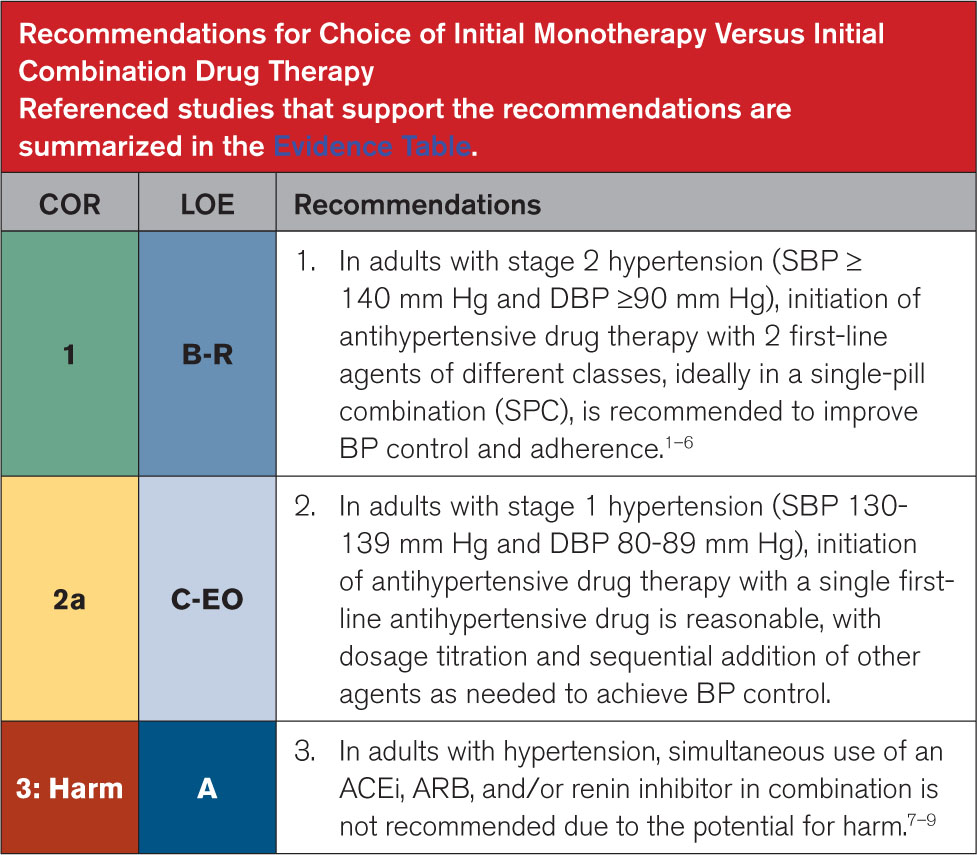
Circulation August 14,2025 https://doi.org/10.1161/CIR.0000000000001356
Category: Pediatrics
Posted: 9/5/2025 by Julie Kurek, MD
(Updated: 2/8/2026)
Click here to contact Julie Kurek, MD
Evidence shows the effectiveness of inhaled corticosteroids during pediatric asthma attacks.
A metanalysis from 2020 reviewed 7 different studies between 2009 to 2018 that included patients < 18 years. The studies compared the use of inhaled corticosteroids to placebo, inhaled corticosteroids compared to systemic corticosteroids, and inhaled corticosteroids in addition to systemic corticosteroids. Please note that in the studies children were still being treated with albuterol.
The results showed:
-Inhaled corticosteroids would significantly reduce the hospital admission rate when compared to placebo (by about 83%).
-Inhaled corticosteroids reduced hospital admission rates when compared to systemic steroids only (by 27%) for mild to moderate asthma.
-When combining systemic steroids with inhaled corticosteroids, the hospital admission rate would be reduced by 25% compared to using only systemic steroids for moderate to severe asthma attacks.
Bottom line: Consider administering inhaled corticosteroids in pediatric asthma patients.
Sawanyawisuth K, Chattakul P, Khamsai S, Boonsawat W, Ladla A, Chotmongkol V, Limpawattana P, Chindaprasirt J, Senthong V, Phitsanuwong C, Sawanyawisuth K. Role of Inhaled Corticosteroids for Asthma Exacerbation in Children: An Updated Meta-Analysis. J Emerg Trauma Shock. 2020 Apr-Jun;13(2):161-166. doi: 10.4103/JETS.JETS_116_19. Epub 2020 Jun 10. PMID: 33013097; PMCID: PMC7472813.
Category: Ultrasound
Keywords: Bladder Ultrasound, Foley, POCUS (PubMed Search)
Posted: 9/3/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
If a patient is experiencing issues with their Foley catheter, consider using POCUS.
Using a curvilinear probe over the suprapubic region, you can obtain a transverse view of the bladder by orienting the marker towards the patient’s right side, or a sagittal view by orienting the marker towards the patient’s head.
In a properly functioning Foley, the bladder will appear decompressed, and you may only see the Foley balloon.
In cases of obstruction or malposition, you may notice a distended bladder. The next step is to attempt to visualize the Foley balloon. If you do not see a Foley balloon within the bladder, try deflating the balloon and advancing the catheter.
If you notice debris blocking the foley or heterogenous material in a patient with hematuria, you can attempt to flush the catheter, but if the patient has a large amount of hematuria, you may need to replace the current Foley with a three-way catheter for continuous bladder irrigation.
Boivin Z, Li JJ, Gottlieb M, Liu RB. Troubleshooting Foley Catheter Problems using Point-of-Care Ultrasound, Journal of Emergency Medicine (2025). doi.org/10.1016/j.jemermed.2025.07.049
Category: Critical Care
Keywords: Critical Care, oxygen, ventilator, SaO2 (PubMed Search)
Posted: 9/2/2025 by Zachary Wynne, MD
Click here to contact Zachary Wynne, MD
What is the ideal oxygen saturation goal for a mechanically ventilated patient? Literature over the past decade has led away from the perfect 100% oxygen saturation due to its association with worse patient outcomes across many disease states. It is theorized that excess oxygen leads to free radical production causing a lung injury pattern. However, there is no clear guidance for the ideal range of oxygen saturation goals, particularly in the mechanically ventilated patient, despite a meta-analysis and several recent trials.
UK-ROX Trial - JAMA - June 2025
Question: Does an oxygen saturation goal of 88-92% lead to a lower 90-day mortality compared to usual care?
Population: 16,500 mechanically ventilated adult patients in 97 ICU’s across the UK, excluded patients on ECMO
Intervention: Goal oxygen saturation of 88-92%, using the lowest possible FiO2
Control: Usual care, defined as oxygen supplementation at the discretion of the treating physician (no limits set to FiO2 or SaO2)
Outcomes:
Bottom Line:
Ideal oxygenation targets remain elusive. UK-ROX adds to the growing literature of oxygenation targets in mechanically ventilated patients but does not clearly show that lower oxygen saturation targets lead to improved ICU outcomes. In your emergency department ICU boarder, avoid a 100% oxygen saturation to prevent oxygen toxicity associated lung injury and consider an oxygen saturation goal of 90-96% (88-92% if history of COPD).
Martin DS, Gould DW, Shahid T, Doidge JC, Cowden A, Sadique Z, Camsooksai J, Charles WN, Davey M, Francis-Johnson A, Garrett RM, Grocott MPW, Jones J, Lampro L, Mackle DM, O'Driscoll BR, Richards-Belle A, Rostron AJ, Szakmány T, Warren A, Young PJ, Rowan KM, Harrison DA, Mouncey PR; UK-ROX Investigators. Conservative Oxygen Therapy in Mechanically Ventilated Critically Ill Adult Patients: The UK-ROX Randomized Clinical Trial. JAMA. 2025 Aug 5;334(5):398-408. doi: 10.1001/jama.2025.9663. PMID: 40501321; PMCID: PMC12163715.
Category: Critical Care
Keywords: hyperbaric, dive medicine, evaluation, (PubMed Search)
Posted: 8/31/2025 by TJ Gregory, MD
(Updated: 2/8/2026)
Click here to contact TJ Gregory, MD
You've encountered it at ABEM General Hospital, but now a SCUBA diver actually comes into your ED and you're concerned for DCS. What next?
Evaluation:
Symptom nature and timing are key in detailed history. Transient neurocognitive symptoms at depth suggest nitrogen narcosis or oxygen toxicity. Neurological symptoms within 10 minutes of surfacing suggest AGE. Widely variable symptoms within 24 hours of surfacing suggest DCS. Symptom onset greater than 24 hours suggests alternative diagnosis (still discuss with Hyperbaric Medicine or DAN).
Thorough physical exam. DCS may manifest only as localized pain. Look for marine envenomation or trauma to the area.
Neurological exam including detailed sensation and ataxia/balance - get the patient on their feet!
Unbiased differential. E.g. DCS may cause chest pain or SOB, but divers still have heart attacks. SCUBA setting may raise alert for AGE, but divers still have strokes. People go to the tropics to dive, but they also eat local fish (Scombroid and Ciguatera for a future pearl).
Management:
Early consult to Hyperbaric Medicine. In settings with no such team available, a good resource is the Divers Alert Network (DAN) Emergency Hotline at 1-919-684-9111
100% O2 via NRB or highest available delivery. You're not titrating to spO2, you're creating a diffusion gradient for tissue inert gas washout.
IV access and isotonic Fluids. PO if tolerable and unable to obtain IV access.
NSAIDs unless otherwise contraindicated. No special regimen. Standard dosing Ibuprofen or Naproxen are fine. Toradol is ok if limitations to PO.
Horizontal positioning in bed for AGE. Trendelenburg is not recommended.
Manage end organ effects as applicable. E.g. Spinal DCS may yield bladder retention requiring foley
Give consideration to activity specific considerations: hypothermia, restrictive clothing, etc
IV lidocaine has mixed evidence for neuroprotection in AGE. Discuss with Hyperbaricist before starting.
Pre-hospital considerations:
Transport should occur via ground or pressurized air transit capable of 1.0 ATA (sea level) cabin pressure. If non-pressurized aircraft transport is absolutely necessary, maintain continuous oxygen supplementation and altitude less than 2000 feet. This also applies to the inter-hospital setting.
O2 delivery by best means available to include SCUBA regulator mouthpiece or even a rebreather apparatus if present.
PO fluids if tolerable and no IV available.
https://pubmed.ncbi.nlm.nih.gov/8378877/
[Clinical aspects, pathophysiology and therapy of decompression sickness]Abstract The primary treatment of decompression illnesses (arterial gas embolism and all types of decompression sickness) is recompression therapy, combined with hyperbaric oxygen breathing. It is essential to initiate treatment as soon as the symptoms arise. However, prior to hyperbaric oxygen therapy--particularly with any delay in starting recompression--specific supportive therapy for ...pubmed.ncbi.nlm.nih.gov
Decompression Sickness - Injuries; Poisoning - MSD Manual Professional Edition
Decompression Sickness - MSD ManualsSymptoms and Signs of Decompression Sickness Severe symptoms may manifest within minutes of surfacing, but in most patients, symptoms begin gradually, sometimes with a prodrome of malaise, fatigue, anorexia, and headache. Symptoms occur within 1 hour of surfacing in approximately 50% of patients and by 6 hours in 90%. Rarely, symptoms can manifest 24 to 48 hours after surfacing, particularly ...www.msdmanuals.com
Category: Neurology
Keywords: CVA, blood pressure management, aggressive, edema (PubMed Search)
Posted: 8/25/2025 by Robert Flint, MD
(Updated: 8/30/2025)
Click here to contact Robert Flint, MD
While this study is imperfect and may not be measuring patient important outcomes, it does fit with other literature on the topic of intensive blood pressure control in patients with acute ischemic stroke. These patients were randomized to aggressive blood pressure control (SBP 130-140 within 1 hour of TPA administration continued for 72 hours) or the standard SBP <180. Repeat imaging was performed to assess the degree of cerebral swelling that each group developed. There was no difference in swelling between the two groups.
Take away is aggressive blood pressure management in this group of ischemic stroke patients does not seem to be beneficial.
Zhang G, Chen C, Ren X, Zhao Y, Ouyang M, Billot L, Li Q, Wang X, Zhang L, Ong S, Liu L, You S, Lindley RI, Robinson TG, Li G, Chen X, Sui Y, Anderson CS, Song L; ENCHANTED Investigators. Effects of Intensive Blood Pressure Lowering on Brain Swelling in Thrombolyzed Acute Ischemic Stroke: The ENCHANTED Results. Stroke. 2025 Jun;56(6):1388-1395. doi: 10.1161/STROKEAHA.124.049938. Epub 2025 Apr 3. PMID: 40177745.
Category: Administration
Keywords: AI, LLM, large language model, artificial intelligence, search (PubMed Search)
Posted: 8/27/2025 by Steve Schenkel, MPP, MD
(Updated: 2/8/2026)
Click here to contact Steve Schenkel, MPP, MD
Have you tried using Large Language Model (LLM) driven searches in clinical practice, for example, OpenEvidence, ChatGPT, or Claude?
A recent paper, far from medicine, argues that LLM searching has changed the way we think about search and what we expect from search.
We have moved from searching for sources to searching for the information contained within sources. With this, our expectations have changed – we expect search to provide answers, not documents.
With this shift, the foundations of trust have shifted. Rather than finding a document that provides the answer, and which is supported by the integrity of the authors and publishers – and which the reader can evaluate – LLMs provide an answer, often with little evidentiary base to support that answer.
Some LLMs do a better job of referencing sources in support of their answers than others. This argument suggests how important such transparency can be.
Find the full conversation here, https://publicera.kb.se/ir/article/view/52258, in Sundin O, Theorising notions of searching, (re)sources and evaluation in the light of generative AI, Information Research 2025, vol 30.
Sundin O, Theorising notions of searching, (re)sources and evaluation in the light of generative AI, Information Research 2025, vol 30. https://publicera.kb.se/ir/article/view/52258
Category: Geriatrics
Keywords: frailty, geriatrics, troponin, syndrome (PubMed Search)
Posted: 8/25/2025 by Robert Flint, MD
(Updated: 8/27/2025)
Click here to contact Robert Flint, MD
This editorial reminds us about the use of frailty measures in the geriatric population.
The authors write that frailty “describes a state of vulnerability causing an impaired ability to maintain homeostasis due to reduced physiologic reserve. Frailty is associated with disability, multimorbidity, cognitive impairment, institutionalization, and mortality. **Analogous to troponin testing, frailty assessment has been used to risk stratify older adults.**”
They also remind us that frailty is a syndrome not a disease in and of itself. It impacts how disease affects the patient and should inform our care, but not generate ageism or therapeutic nihilism.
Once frailty is identified, it allows for further assessment looking at the “Geriatric 5M's framework: Mind, Mobility, Medications, Multicomplexity, and Matters Most.”
Is Frailty the Geriatric Troponin?
Jacqueline M. McMillan, Julian Falutz Journal of the American Geriatrics Society
First published: 12 March 2025 https://doi.org/10.1111/jgs.19423
Category: Critical Care
Posted: 8/26/2025 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Predicting NIV Failure
Frat JP, et al. Noninvasive respiratory supports in the ICU. Intensive Care Med. 2025; 51:1476-89.
Category: Trauma
Keywords: head injury, geriatric, antithrombotic, CT imaging (PubMed Search)
Posted: 8/25/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In this retrospective study at 103 hospitals of patients over age 65 who received a head CT:
5948 total patients
3177 (53%) were on at least one anti-thrombotic (warfarin, direct oral anticoag, or anti-platelet agent)
781 (13%) had inter cranial hemorrhage. (ICH)
No form of AC showed an increased risk of ICH.
Risk factors for ICH were: “a high-level fall, a Glasgow coma scale of 14, a cutaneous head impact , vomiting, amnesia, a suspected skull vault fracture or of facial bones fracture”
To me this really begs the question are we ordering head CTs on the right patients? Was there any indication of head injury in these patients or did the mere presence of a patient on AC prompt the imaging order? More work should be done to prevent needless imaging cost, patient time in the emergency department and radiologist work load/turn around time.
Benhamed A, Crombé A, Seux M, Frassin L, L'Huillier R, Mercier E, Émond M, Millon D, Desmeules F, Tazarourte K, Gorincour G. Association between antithrombotic medications and intracranial hemorrhage among older patients with mild traumatic brain injury: a multicenter cohort study. Eur J Emerg Med. 2025 Jul 1. doi: 10.1097/MEJ.0000000000001246. Epub ahead of print. PMID: 40590793.
