Category: Trauma
Keywords: Hypothermia, fall, height, injury (PubMed Search)
Posted: 1/31/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
An English study describes 30 patients that jumped from a single bridge of 30 meters (98 feet) over the course of 12 years. Twenty six landed in the water. The injury pattern for those landing in water was described as “Hypothermia was the most common presentation (n = 23), followed by pneumothoraces (n = 14), rib fractures (n = 10), thoracic vertebral fractures (n = 9) and lung contusions (n = 8). Lower water temperatures at the time of the incident (p = 0.008) and lower patient body temperatures on arrival to hospital (p = 0.002) were significantly associated with increased 30-day mortality.”
The small group landing on land had more pelvic and extremity fractures than the water group and none had hypothermia.
Remember to start aggressive rewarming in patients who fall into water!
Harvey T, Nottingham T, Owen P, Hannah J, Plumb J. Injury patterns and clinical outcomes following falls from a medium-height bridge: A retrospective study. Trauma. 2025;28(1):44-53. doi:10.1177/14604086251404739
Category: Trauma
Keywords: Stab wound, chest radiograph, pneumothorax (PubMed Search)
Posted: 1/31/2026 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This small study from South Africa shows stab wounds to the chest with a pneumothorax less than 0.5 cm that were managed conservatively had completely resolved on 12 hour repeat chest X-ray. This could facilitate earlier discharge of these patients. It also supports conservative (non-tube placement) approach to asymptomatic small pneumothoraces from stab wounds.
Kong V, Cheung C, Lee D, et al. Defining the optimal timing of interval chest radiograph in conservatively managed small pneumothorax from thoracic stab wounds – a South African experience. Trauma. 2025;28(1):14-17. doi:10.1177/14604086251396434
Category: Trauma
Keywords: Pelvic fracture, EMS (PubMed Search)
Posted: 1/25/2026 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
A reminder from a recent position paper on pelvic trauma that we should not be doing stability testing to evaluate pelvic trauma
“EMS clinicians should recognize the challenges in accurately identifying pelvic fractures by physical exam alone. Manual stability testing of the pelvis is neither sensitive nor specific and may cause harm.”
Lyng, J. W., Corsa, J. G., Raetzke, B. D., Wilson, B. R., McCoy, A., Patterson, S. C., … Bosson, N. (2025). Prehospital Trauma Compendium: Evaluation and Management of Suspected Pelvis Fractures – An NAEMSP Position Statement and Resource Document. Prehospital Emergency Care, 1–35. https://doi.org/10.1080/10903127.2025.2540420
Category: Trauma
Keywords: Prehospital, transfusion, non-trauma (PubMed Search)
Posted: 1/11/2026 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
Much has been written about the benefits of prehospital blood transfusion for traumatic hemorrhage. Can this success be ascribed to non-traumatic hemorrhage as well? This small study (50 patients over 10 years!) says there were improvements in patient physiology (shock index) for those patients receiving blood for GI bleed, etc. Much more research is needed however this could be a beneficial practice in the future.
Kodakadath, H., Dillane, S., Griggs, J. et al. Pre-hospital blood transfusion in non-traumatic major haemorrhage: a retrospective observational study. Scand J Trauma Resusc Emerg Med 33, 191 (2025). https://doi.org/10.1186/s13049-025-01495-z
Category: Trauma
Keywords: Ketamine, nebulized, pain control (PubMed Search)
Posted: 1/3/2026 by Robert Flint, MD
(Updated: 1/4/2026)
Click here to contact Robert Flint, MD
This systematic review found improved pain scale at 15 and 120 minutes in 495 patients who received nebulized ketamine. Dosing at 0.75 mg/kg was as effective as 1.5 mg/kg and the nebulized ketamine was non-inferior to IV morphine and ketamine with fewer side effects.
Kirk, D., Whiles, E., Jones, A. et al. Breathing new life into pain management: a systematic review of nebulised ketamine for analgesia. Scand J Trauma Resusc Emerg Med 33, 196 (2025). https://doi.org/10.1186/s13049-025-01501-4
Category: Trauma
Keywords: hypocalcemia, trauma, mortaility, rate (PubMed Search)
Posted: 12/27/2025 by Robert Flint, MD
(Updated: 12/28/2025)
Click here to contact Robert Flint, MD
Previous small studies had put the prevalence of hypocalcemia in trauma patients at 23-56%. This single center study of 2200 patients looked at prevalence and outcome and found a much lower prevalence however worse outcomes than those who were not hypocalcemic.
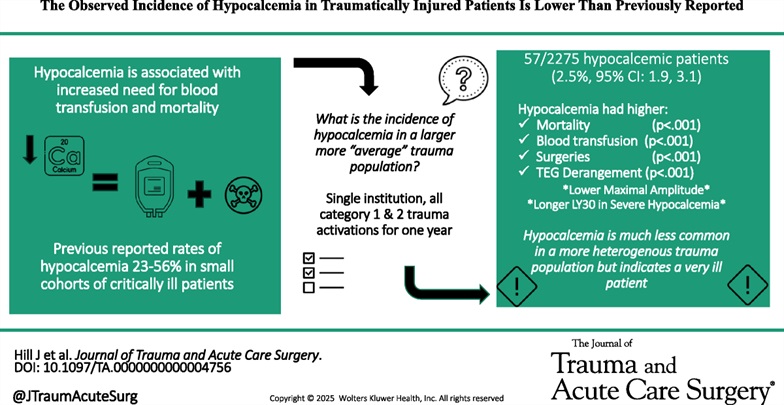
Hill, Joshua H. MD; Shah, Bhairav DO; Rady, Emily MD; Lieber, Michael MS; Lauria, Julia DO; Lee, Katarina DO; Wierzbicki, Katrina BS; Kashikar, Tanisha DO; Kincaid, Michelle MD. The observed incidence of hypocalcemia in traumatically injured patients is lower than previously reported. Journal of Trauma and Acute Care Surgery 99(6):p 920-927, December 2025. | DOI: 10.1097/TA.0000000000004756
Category: Trauma
Keywords: prehospoital, blood, survival, unexpected (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 12/25/2025)
Click here to contact Robert Flint, MD
This study demonstrated that administration of prehospital blood to trauma patients lead to a higher rate of survival in patients whose initial ED vital signs or pre-hospital shock index would have predicted death.
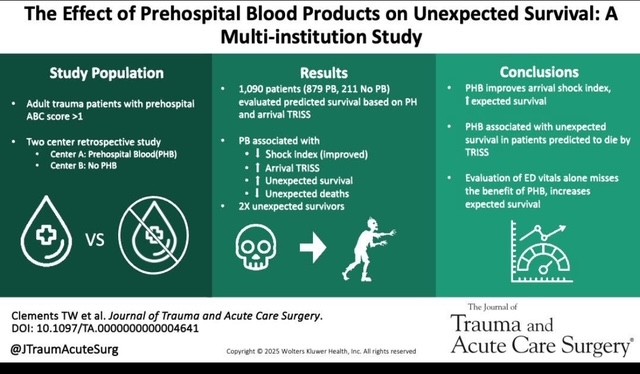
Clements TW, Van Gent JM, Krzyzaniak A, Campbell B, Carroll A, Mericle M, Sise M, Peck KA, Cotton BA. The effect of prehospital blood products on unexpected survival: A multi-institution study. J Trauma Acute Care Surg. 2025 May 2. doi: 10.1097/TA.0000000000004641. Epub ahead of print. PMID: 40312787.
Category: Trauma
Keywords: shock, CAB, resuscitation, trauma, circulation (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 12/14/2025)
Click here to contact Robert Flint, MD
This review article reminds us that circulation needs to be prioritized over airway in trauma patients. This means bleeding control (pressure on wound, tourniquet, surgery/IR intervention), correcting tension pneumothorax, correcting pericardial tamponade, as well as resuscitation to return physiologic homeostasis (blood products, vasopressors where needed, warm the patient, etc.) before intubation. Altered mental status/low GCS may be due more to hypoperfusion than neurologic injury. Correcting the hypotension may alleviate that need to intubate.
Ferrada, Paula MD, FACS, FCCM, MAMSE; Duchesne, Juan MD, FACS, FCCM, FCCP; Piehl, Mark MD, MPH. Prioritizing circulation over airway in trauma patients with exsanguinating injuries: What you need to know. Journal of Trauma and Acute Care Surgery 99(5):p 679-683, November 2025. | DOI: 10.1097/TA.0000000000004618
Category: Trauma
Keywords: brain injury, score, prediction (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/23/2025)
Click here to contact Robert Flint, MD
In 252 mild traumatic brain injury patients seen at 3 level I centers that were given the Rivermead Post Concussion Symptoms Questionnaire within 24 hours of arrival, 3 month post concussive symptoms were significantly correlated with their score on the questionnaire. This questionnaire take 3 minutes to complete. This may be helpful in prognosticating who will have post-concussive symptoms and who will need additional follow up.
Gray, Samuel et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Trauma
Keywords: rsi, neck injury, penetrating, airway (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/16/2025)
Click here to contact Robert Flint, MD
This group looked at 88 patients intubated for penetrating neck injury and found 95% received neuromuscular blocking agents, 73% were intubated using a bougie, and 95% were intubated on first pass.
The authors concluded; “Rapid sequence intubation with bougie use was an effective default approach to definitive airway management in ED patients with penetrating neck trauma.”
Lee, Daniel H. et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Trauma
Keywords: primary care, hypertension, diabetes, trauma (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/9/2025)
Click here to contact Robert Flint, MD
These authors followed 250 consecutive trauma activation patients over a one year period. In hospital elevated blood pressure and glucose level correlated with a new diagnosis of hypertension and diabetes respectively over that 1 year time line. Some of these patients also had a new diagnosis of HIV, substance use disorder and hepatitis C. Using their contact with the health system due to trauma can be a way to screen for undiagnosed medical problems such as diabetes and hypertension. Assuring outpatient follow up for these patients will have an effect on their long term morbidity and mortality.
Banks, Kian C. et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Trauma
Keywords: Analgesia, trauma, prehospital, multimodal (PubMed Search)
Posted: 11/1/2025 by Robert Flint, MD
(Updated: 11/2/2025)
Click here to contact Robert Flint, MD
In a German study comparing one EMS jurisdiction which used IV paracetamol (acetaminophen) in combination with nalbuphine (Nubian, opiate agonist/antagonist) to another jurisdiction which used piritramide (synthetic opioid similar to fentanyl) for prehospital traumatic pain, the combination worked better to decrease pain on a numerical scale. There were no differences in typical safety measures.
The use of an antagonist/agonist theoretically could precipitate withdrawal in non-opiate naive patients and could influence in hospital analgesic choices. The literature on this is mixed.
This study offers further evidence of the efficacy of multi-modal pain control, the feasibility of paramedics using IV paracetamol and the possibility of using rapid onset opioid agonist/antagonist in the prehospital setting.
Lohmann, J., Deicke, M., Deslandes, M. et al. Prehospital analgesia for trauma-related pain by paramedics: a comparative retrospective observational study of paracetamol, nalbuphine plus paracetamol, and piritramide. Scand J Trauma Resusc Emerg Med 33, 152 (2025). https://doi.org/10.1186/s13049-025-01470-8
Category: Trauma
Keywords: brain injury, evidence, eucapnia, normotensive, care (PubMed Search)
Posted: 10/25/2025 by Robert Flint, MD
(Updated: 10/26/2025)
Click here to contact Robert Flint, MD
Another paper emphasizing care for brain injured patients should include:
-pre-intubation preoxygenation to avoid hypoxia
-pre-intubation avoid extremes in blood pressure (hypotension kills)
-use hemodynamically neutral induction agents such as ketamine or etomidate
-post intubation target eucapnia on the ventilator. (do not aim for low CO2)
-post intubation maintain adequate sedation to avoid increased intercranial pressure
Hoyne J, Edlow J. Airway Management in Patients With Acute Brain Injury or Ischemia. J Emerg Med. 2025 Jul;74:125-133. doi: 10.1016/j.jemermed.2024.12.015. Epub 2025 Jan 6. PMID: 40348691.
Category: Trauma
Keywords: head injury, trauma, geriatric (PubMed Search)
Posted: 10/4/2025 by Robert Flint, MD
(Updated: 10/5/2025)
Click here to contact Robert Flint, MD
This paper reminds us older patients have higher mortality and worse outcomes overall if their injury includes a head injury. Any mechanism that results in head injury, including fall from standing, has a higher potential for death, disability, and long term cognitive decline in older patients. Triaging these patients to trauma centers can lead to better outcomes. The difficulty is knowing which patients to send to trauma centers vs. emergency departments. The authors write:
"clinicians should consider transporting to a trauma center in geriatric patients with head trauma, if feasible. However, given the frequency with which head injury occurs, transportation to a trauma center for all patients with head trauma is likely to overwhelm EMS systems and hospitals. Unfortunately, the existing literature does not delineate the subset of patients whose condition will benefit from this evaluation . Given these considerations, we recommend EMS clinicians consider abnormal mental status, presence of anti-coagulation, and loss of consciousness as considerations to transport to a trauma center in cases where the need for trauma center evaluation is not clear.”
Haussner, W. K., Breyre, A. M., Bascombe, K., Barrett, W. J., Camacho, M. A., Overton-Harris, P., … Colwell, C. (2025). Prehospital Trauma Compendium: Management of Geriatric Trauma Patients – A Position Statement and Resource Document of NAEMSP. Prehospital Emergency Care, 1–10. https://doi.org/10.1080/10903127.2025.2557006
Category: Trauma
Keywords: Head injury, geriatric, interracial hemorrhage (PubMed Search)
Posted: 9/21/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This systematic review of the literature found four findings associated with intercranial hemorrhage in older patients after a fall. They were: focal neurologic findings, external signs of trauma on the head, loss of consciousness, and male sex.
We still need better studies as this is completely based on the quantity and quality of literature available to review. This information is not enough to change liberal CT imagining in older patients after a fall. It is the beginning of the study process.
Dubucs X, Gingras V, Boucher V, Carmichael PH, Ruel M, De Wit K, Grewal K, Mercier É, Blanchard PG, Benhamed A, Charpentier S, Émond M. Risk Factors for Traumatic Intracranial Hemorrhage in Older Adults Sustaining a Head Injury in Ground-Level Falls: A Systematic Review and Meta-analysis. Ann Emerg Med. 2025 Jul 22:S0196-0644(25)00313-0. doi: 10.1016/j.annemergmed.2025.05.021. Epub ahead of print. PMID: 40699169.
Category: Trauma
Keywords: TXA, EMS, prehospital, consensus (PubMed Search)
Posted: 9/14/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
The National Association of EMS Physicians, the American College of Surgeons Committee on Trauma, and the American College of Emergency Physicians recommends:
• Prehospital TXA administration may reduce mortality in adult trauma patients with hemorrhagic shock when administered after lifesaving interventions.
• Prehospital TXA administration appears safe, with low risk of thromboembolic events or seizure.
• The ideal dose, rate, and route of prehospital administration of TXA for adult trauma patients with hemorrhagic shock has not been determined. Current evidence suggests EMS agencies may administer either a 1-g intravenous/intraosseous dose (followed by a hospital-based 1-g infusion over 8 hours) or a 2-g intravenous/intraosseous dose as an infusion or slow push.
• Prehospital TXA administration, if used for adult trauma patients, should be given to those with clinical signs of hemorrhagic shock and no later than 3 hours post-injury. There is no evidence to date to suggest improved clinical outcomes from TXA initiation beyond this time or in those without clinically significant bleeding.
• The role of prehospital TXA in pediatric trauma patients with clinical signs of hemorrhagic shock has not been studied, and standardized dosing has not been established. If used, it should be given within 3 hours of injury.
• Prehospital TXA administration, if used, should be clearly communicated to receiving health care professionals to promote appropriate monitoring and to avoid duplicate administration(s).
• A multidisciplinary team, led by EMS physicians, that includes EMS clinicians, emergency physicians, and trauma surgeons should be responsible for developing a quality improvement program to assess prehospital TXA administration for protocol compliance and identification of clinical complications.
Barrett, Whitney J. MD; Kaucher, Kevin A. PharmD, BCCCP; Orpet, Ross E. MD; Campion, Eric M. MD; Goodloe, Jeffrey M. MD; Fischer, Peter E. MD, MS, NRP; Colwell, Christopher B. MD; Lyng, John W. MD, NRP. Tranexamic acid in trauma: A joint position statement and resource document of NAEMSP, ACEP, and ACS-COT. Journal of Trauma and Acute Care Surgery 99(3):p 357-363, September 2025. | DOI: 10.1097/TA.0000000000004727
Category: Trauma
Keywords: brain injury, intubation, best practice, hypoxia, hypotension (PubMed Search)
Posted: 9/6/2025 by Robert Flint, MD
(Updated: 9/7/2025)
Click here to contact Robert Flint, MD
These authors reiterate principles that have been discussed previously regarding intubation in head/brain injured patients.
-Avoid hypoxia with preoxygenation
-Avoid hypotension by fluid resuscitation/vasopressors/blood in the correct clinical setting
-Use hemodynamically neutral induction agents such as Etomidate or Ketamine (it is ok use this in head injured patients!)
-Video laryngoscope gives best first pass success which minimizes hypoxia/raised ICP
-Post-Intubation aim for eucapnia (avoid hyperventilation)
-Use adequate post-intubation sedation to avoid raised ICP
Category: Trauma
Keywords: head injury, geriatric, antithrombotic, CT imaging (PubMed Search)
Posted: 8/25/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
In this retrospective study at 103 hospitals of patients over age 65 who received a head CT:
5948 total patients
3177 (53%) were on at least one anti-thrombotic (warfarin, direct oral anticoag, or anti-platelet agent)
781 (13%) had inter cranial hemorrhage. (ICH)
No form of AC showed an increased risk of ICH.
Risk factors for ICH were: “a high-level fall, a Glasgow coma scale of 14, a cutaneous head impact , vomiting, amnesia, a suspected skull vault fracture or of facial bones fracture”
To me this really begs the question are we ordering head CTs on the right patients? Was there any indication of head injury in these patients or did the mere presence of a patient on AC prompt the imaging order? More work should be done to prevent needless imaging cost, patient time in the emergency department and radiologist work load/turn around time.
Benhamed A, Crombé A, Seux M, Frassin L, L'Huillier R, Mercier E, Émond M, Millon D, Desmeules F, Tazarourte K, Gorincour G. Association between antithrombotic medications and intracranial hemorrhage among older patients with mild traumatic brain injury: a multicenter cohort study. Eur J Emerg Med. 2025 Jul 1. doi: 10.1097/MEJ.0000000000001246. Epub ahead of print. PMID: 40590793.
Category: Trauma
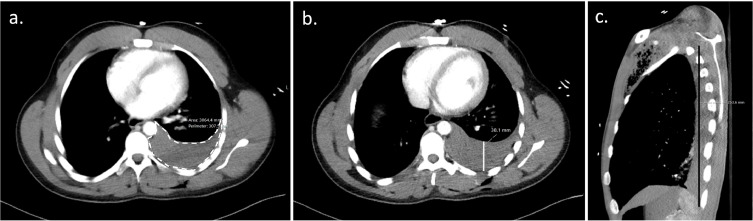
Keywords: chest tube, tube thoracostomy, hemothorax, volume (PubMed Search)
Posted: 8/23/2025 by Robert Flint, MD
(Updated: 8/24/2025)
Click here to contact Robert Flint, MD
Over 300 ml of blood on a chest CT in a traumatically injured patient requires a tube thoracostomy. How do you calculate 300 ml of blood on a chest CT?
You use Mergo's formula.
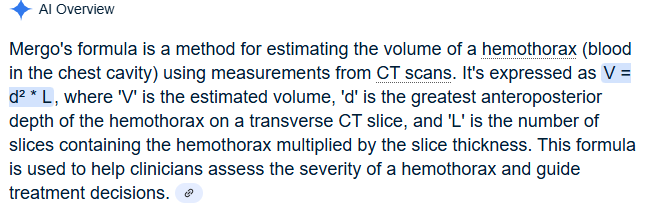
Image B the AP line is what would represent d
1. Blank JJ, de Moya MA. Traumatic pneumothorax and hemothorax: What you need to know. J Trauma Acute Care Surg. 2025 Jul 3. doi: 10.1097/TA.0000000000004692. Epub ahead of print. PMID: 40604368.
2. CT-based pleural effusion volume estimation formula demonstrates low accuracy and reproducibility for traumatic hemothorax
Tewkesbury, Grace et al. Injury, Volume 55, Issue 1, 111112
Category: Trauma
Keywords: Pneumothorax, cheat tube, indication (PubMed Search)
Posted: 8/17/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This review article answers the basic question: when does a traumatic pneumothorax require tube thoracostomy?
“A pneumothorax greater than 20% of the thoracic volume on chest x-ray or greater than 35 mm on CT, measured radially from the chest wall to the lung parenchyma, should be treated with tube thoracostomy. Pneumothoraces smaller than this may be observed; approximately 10% of these will fail observation and require tube thoracostomy treatment.”
Blank JJ, de Moya MA. Traumatic pneumothorax and hemothorax: What you need to know. J Trauma Acute Care Surg. 2025 Jul 3. doi: 10.1097/TA.0000000000004692. Epub ahead of print. PMID: 40604368.
