Category: Trauma
Keywords: prehospoital, blood, survival, unexpected (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 12/25/2025)
Click here to contact Robert Flint, MD
This study demonstrated that administration of prehospital blood to trauma patients lead to a higher rate of survival in patients whose initial ED vital signs or pre-hospital shock index would have predicted death.
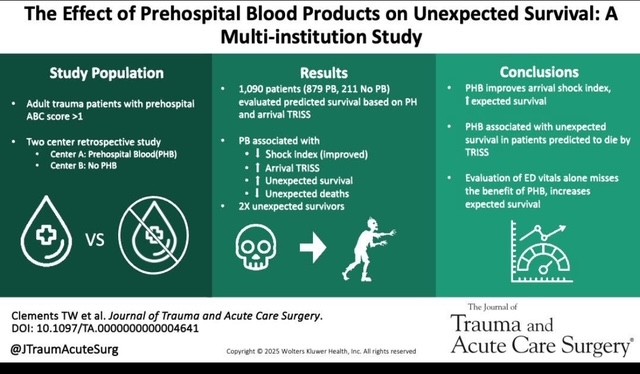
Clements TW, Van Gent JM, Krzyzaniak A, Campbell B, Carroll A, Mericle M, Sise M, Peck KA, Cotton BA. The effect of prehospital blood products on unexpected survival: A multi-institution study. J Trauma Acute Care Surg. 2025 May 2. doi: 10.1097/TA.0000000000004641. Epub ahead of print. PMID: 40312787.
Category: Administration
Keywords: holidays, scheduling, daily volumes, behavioral health (PubMed Search)
Posted: 12/18/2025 by Steve Schenkel, MPP, MD
(Updated: 12/24/2025)
Click here to contact Steve Schenkel, MPP, MD
How do ED volumes change around the winter holidays?
The anticipated US pattern is one of lower volumes on the holidays themselves followed by increased volumes on the first weekdays after.
Behavioral health visits show similar patterns – a drop before the holidays and perhaps an increase after the holiday.
Many departments adjust scheduling accordingly, reducing staff on major holidays, which has the added benefit of allowing more people to enjoy the holiday.
This pattern isn’t necessarily what happens everywhere, though. At least one Australian ED reported increased visits over the holidays.
While not perfect, the best guide to future holiday volumes remains past experience thoughtfully applied.
Agoritsas A, et al. Predicting Flow in the Pediatric Emergency Department: Are Holidays Lighter? Annals of Emergency Medicine 2015, Volume 66, Issue 4, S143
Halpern, Scott D. et al. Emergency department patterns in psychiatric visits during the holiday season. Annals of Emergency Medicine 1994, Volume 24, Issue 5, 939 – 943.
Leming, M. et al. Effect of Holidays on the Patient Severity and Census In the Emergency Department. Annals of Emergency Medicine 2010, Volume 56, Issue 3, S128
Silverman M. Holiday Scheduling: Fair and Balanced. EP Monthly, Dec 1, 2010. https://epmonthly.com/article/holiday-scheduling-fair-and-balanced/.
Zheng, W., Muscatello, D.J. and Chan, A.C. (2007), Deck the halls with rows of trolleys … emergency departments are busiest over the Christmas holiday period. Medical Journal of Australia, 187: 630-633. https://doi.org/10.5694/j.1326-5377.2007.tb01451.x
Category: Critical Care
Keywords: ventilator, extubation, critical care, respiratory, SBT (PubMed Search)
Posted: 12/22/2025 by Zachary Wynne, MD
(Updated: 12/23/2025)
Click here to contact Zachary Wynne, MD
The emergency department serves many critically ill patients that require airway management and mechanical ventilation. Most of these patients go on to require ICU care. However, some patients require only brief intubation and should be appropriate candidates considered for emergency physician-driven extubation. Early extubation can minimize the risks associated with mechanical ventilation for patients such as ventilator associated pneumonia (VAP), ventilator induced lung injury (VILI), and others. Additionally, in setting of high levels of ED boarding and limited ICU resources, extubating appropriate candidates in the ED can reduce boarding times and improve patient flow.
Who?
Screening Checklist
Testing
Prepare - depending on institution, may require consultation with the hospital intensivist
Perform - see this video courtesy of Respiratory Skills - LSC on performing extubation
Category: Quality Assurance/Quality Improvement
Keywords: Medication, pharmacist, adverse event, transitions of care (PubMed Search)
Posted: 12/15/2025 by Lena Carleton, MD
(Updated: 12/22/2025)
Click here to contact Lena Carleton, MD
Medication-related adverse events account for an estimated 2 million Emergency Department (ED) visits annually in the United States. This study evaluated whether a pharmacist-led intervention could reduce ED return visits for medication-related events.
In this open-label, parallel-group randomized clinical trial, 330 adults were enrolled at a single university hospital in France between 2018 and 2021. Medication-related events were categorized as adverse drug events without misuse (e.g., drug reactions or interactions), adverse drug events with misuse, and nonadherence-related events.
Patients were randomized to a pharmacist-led transition-of-care intervention or usual care. In the intervention group, an ED pharmacist obtained a medication history and contacted the patient’s general practitioner and community pharmacist by phone and letter with details of the event and management recommendations; estimated intervention time was approximately 60 minutes per patient. Usual care included a medication history and a standard ED discharge letter to the general practitioner.
The primary outcome was ED return visits for the same medication-related adverse event within 6 months. Secondary outcomes included all-cause ED visits, outpatient visits, hospitalizations, and death.
The intervention group had a 19% reduction in ED return visits for medication-related adverse events attributed to the same medication as the initial ED visit, with similar reductions in all medication-related ED visits and hospitalizations. There were no significant differences in all-cause hospitalization or mortality between the intervention and control groups.
Notable barriers to implementation included the time-intensive nature of the intervention (approximately 60 minutes per patient) and the absence of a shared medical record to facilitate communication between ED and outpatient pharmacists and clinicians.
Key Takeaway: Improved communication between ED teams, outpatient physicians, and pharmacists may reduce recurrent ED visits for medication-related adverse events.
Villiet M, Laureau M, Perier D, et al. Emergency Department Visits for Medication-Related Events With vs Without Pharmacist Intervention: The URGEIM Randomized Clinical Trial. JAMA Intern Med. 2025;185(6):669–678. doi:10.1001/jamainternmed.2025.0640
Anderson TS. Secondary Prevention of Medication-Related Harms. JAMA Intern Med. 2025;185(6):679. doi:10.1001/jamainternmed.2025.0651
Category: Ultrasound
Posted: 12/3/2025 by Kerith Joseph, MD
(Updated: 12/21/2025)
Click here to contact Kerith Joseph, MD
Clinically Oriented Takeaway
A single-view posterior POCUS can reliably identify anterior shoulder dislocation using the **Glenohumeral Separation Distance (GhSD)**—a simple measurement of the posterior alignment of the humeral head and glenoid.
How to Use It
Place a linear probe transversely on the posterior shoulder.
Identify the most posterior aspect of the humeral head and glenoid.
Measure the vertical offset (GhSD):
GhSD > 0 cm ? Normal alignment
GhSD < 0 cm ? Anterior dislocation
GhSD = 0 cm ? Borderline; treat as suspicious
Clinical Implications
Even minimally trained operators achieved 100% sensitivity and specificity in detecting anterior dislocation using this method.
POCUS can:
Enable rapid diagnosis when radiography is delayed.
Confirm reduction immediately at bedside, especially valuable when sedation is used.
Potentially reduce ED length of stay and radiation exposure.
Limitations to Consider
Not validated for posterior dislocations.
Does not assess associated injuries (fractures, Hill-Sachs, Bankart lesions).
Findings based on novice sonographers; performance among clinicians likely equal or better but still needs broader validation.
Single-center, small convenience sample.
No posterior dislocations occurred; technique not validated for them.
Novice sonographers could not be fully blinded to shoulder appearance.
Category: Administration
Keywords: MOUD, racial and sex disparities (PubMed Search)
Posted: 12/11/2025 by Kevin Semelrath, MD
(Updated: 12/20/2025)
Click here to contact Kevin Semelrath, MD
This study looked for differences in prescribing patterns of suboxone for different opioid related complaints- withdrawal, overdose, and other related complaints.
In the overall cohort, all racial minorities, except Native American, and female patients had a lower likelihood of being prescribed suboxone for any opioid related complaint compared to white, male patients.
However, when they did subgroup analysis, patients presented for withdrawal symptoms had increased rates of buprenorphrine administration and prescribing that eliminated the racial disparities, but the gender disparities remained.
MOUD remain a key factor in allowing patients with OUD to achieve long-term sobriety, but there are still persistent barriers to appropriate prescribing
Chhabra N, Smith D, Parde N, Hsing-Smith N, Bianco JM, Taylor RA, D'Onofrio G, Karnik NS. Racial, ethnic, and sex disparities in buprenorphine treatment from emergency departments by discharge diagnosis. Acad Emerg Med. 2025 Sep;32(9):985-993. doi: 10.1111/acem.70035. Epub 2025 Apr 25. PMID: 40277252; PMCID: PMC12353228.
Category: Pediatrics
Keywords: CPR, peds, ventilation, BVM, compression ratio (PubMed Search)
Posted: 12/19/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Pediatric CPR without an advanced airway in place requires 15 compressions to 2 ventilations per AHA and ILCOR guidelines. This can lead to a 2-4 second pause in compressions due to the time the ventilations take. The Maryland hiccup method is a novel description of two brief pauses for ventilations during the upstroke of compressions 14 and 15. This method was shown to improve the compression fraction and compressions per minute with no significant differences between standard CPR and the Maryland hiccup method in ventilation volume or compression depth determined on simulation mannequins. 38 Maryland EMS clinicians participated in this study.
A video demonstration of the Maryland Hiccup method is linked in the article and also available at: https://www.youtube.com/watch?v=RvFxhj7hzsQ .
Anders JF, Anderson C, Wright-Johnson C, O'Connell KJ. Improving the Quality of Pediatric Basic Life Support Cardiopulmonary Resuscitation With a Novel Method: The Maryland Hiccup. Cureus. 2025 Feb 9;17(2):e78783. doi: 10.7759/cureus.78783. PMID: 39931503; PMCID: PMC11808343.
Category: EMS
Keywords: altered mental status, trauma, EMS (PubMed Search)
Posted: 12/17/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
EMS is taught to assess levels of consciousness through the Glasgow Coma Scale (GCS) and AVPU (alert/responsive to verbal stimuli/responsive to painful stimuli/unresponsive).
This study aimed to find a cut off point for where GCS and AVPU scales correlate. The National EMS Information System data set was used to look at over 4 million patient encounters that had both GCS and AVPU documented.
Lower AVPU scores correlated with life-sustaining procedures, including those for airway management, seizure, and cardiac arrest. Optimal GCS cut points obtained via a grid-based search were 14 to 15 for alert (A), 11 to 13 for verbal (V), 7 to 10 for pain (P), and 3 to 6 for unresponsive (U).
Ramgopal S, Horvat CM, Cash RE, Pelletier JH, Martin-Gill C, Macy ML. Comparing AVPU and Glasgow Coma Scales Among Children Seen by Emergency Medical Services. Pediatrics. 2024;154(2):e2024066168. doi:10.1542/peds.2024-066168
Category: Critical Care
Posted: 12/16/2025 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Pitfalls in Lactate Interpretation
Levy B, et al. Lactate dynamics as a marker of perfusion: physiological interpretation and pitfalls. Intensive Care Med. 2025; 51:2145-8.
Category: Ultrasound
Keywords: dental infection; POCUS (PubMed Search)
Posted: 12/15/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
Dental pain is a common reason for emergency department visits. These patients often experience prolonged length of stay and additional radiation exposure while awaiting CT imaging of the face. A recent case study highlights the potential role of POCUS in evaluating suspected dental abscesses.
In this report, clinicians used a high-frequency linear probe placed externally along the jawline. By orienting the probe to visualize the bony cortex of the mandible or maxilla and the dental root insertion, they identified a hypoechoic collection abutting the bone. When absent on the contralateral side and interpreted in the appropriate clinical context, this finding can suggest an abscess.
For further details, including imaging examples and technique demonstrations, see the referenced article and supplemental videos.
Hoffer JT, Park R, Brenner DS. "Is My Face Swollen?"-Utilizing Point-of-Care Ultrasound to Diagnose Odontogenic Infections. J Emerg Med. 2025 Oct 25;80:165-176. doi: 10.1016/j.jemermed.2025.10.032.
Category: Trauma
Keywords: shock, CAB, resuscitation, trauma, circulation (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 12/14/2025)
Click here to contact Robert Flint, MD
This review article reminds us that circulation needs to be prioritized over airway in trauma patients. This means bleeding control (pressure on wound, tourniquet, surgery/IR intervention), correcting tension pneumothorax, correcting pericardial tamponade, as well as resuscitation to return physiologic homeostasis (blood products, vasopressors where needed, warm the patient, etc.) before intubation. Altered mental status/low GCS may be due more to hypoperfusion than neurologic injury. Correcting the hypotension may alleviate that need to intubate.
Ferrada, Paula MD, FACS, FCCM, MAMSE; Duchesne, Juan MD, FACS, FCCM, FCCP; Piehl, Mark MD, MPH. Prioritizing circulation over airway in trauma patients with exsanguinating injuries: What you need to know. Journal of Trauma and Acute Care Surgery 99(5):p 679-683, November 2025. | DOI: 10.1097/TA.0000000000004618
Category: Orthopedics
Posted: 12/13/2025 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Midshaft Clavicle Fractures
Have been in the sports headlines over the last several months
http://www.orthopaedicsone.com/wp-content/uploads/2024/06/379191373.png
About 3 - 3.5% of all adult fractures
Typical patient is young and active, usually males < 30 years old
Most clavicle fractures (up to 80%) involve the middle third
Mechanism: Typically direct impact or FOOSH
“S” shaped bone with thinnest & narrowest segment at junction between middle and distal third
Appearance: 2/3 non-displaced
Displaced fractures
Because of the effects of gravity, attempt to get clavicle series in upright position
Otherwise supine view may underestimate degree of displacement
What to look for on plain film
Displacement
Category: Pediatrics
Keywords: pediatric, bowel obstruction, ultrasound, volvulus, malrotation (PubMed Search)
Posted: 12/12/2025 by Kathleen Stephanos, MD
(Updated: 2/8/2026)
Click here to contact Kathleen Stephanos, MD
Malrotation is estimated to occur in 1 in every 500 children, and while many are asymptomatic, volvulus can occur resulting in a high rate of morbidity and mortality from ischemic bowel. Most of these patients will present within the first month of life.
Bilious emesis in an infant should immediately prompt consideration of this life-threatening condition, but what is the testing modality of choice?
While Fluoroscopic Upper GI Series (UGIS) has historically been looked to as the gold standard there are many issues with this method. It requires contrast, radiation exposure and an in-house radiologist to perform the imaging, oftentimes necessitating a transfer. Due to this, many algorithms have moved to Ultrasound (US) as the first test for these patients.
UGIS has a sensitivity for malrotation of 93-100%, but only as high as 89% for volvulus while US has a sensitivity and specificity of 94% and 100% respectively for midgut volvulus.
US findings suggestive of volvulus include the classic “whirlpool sign” with twisting of the superior mesenteric vein around the superior mesenteric artery seen on Doppler, dilated proximal duodenum, or free fluid in the abdomen.
So next time there is an infant presenting with bilious emesis, consider ultrasound as your first step to save a baby's bowel!
McCurdie FK, Meshaka R, Leung G, Billington J, Watson TA. Ultrasound for infantile midgut malrotation: Techniques, pearls, and pitfalls. Pediatr Radiol. 2024 Dec;54(13):2099-2111. doi: 10.1007/s00247-024-06067-4. Epub 2024 Oct 15. PMID: 39404889.
Category: Pharmacology & Therapeutics
Posted: 12/9/2025 by Ashley Martinelli
(Updated: 12/11/2025)
Click here to contact Ashley Martinelli
Sympathetic crashing acute pulmonary edema (SCAPE) is an acute, aggressive pulmonary edema that occurs in patients with hypertensive emergencies. Nitroglycerin (NTG) is often utilized in combination with non-invasive positive pressure ventilation to prevent decompensation; however, data is lacking regarding the optimal dosing strategy.
Study design: retrospective, single-center, cohort study at an academic medical center
Inclusion: adult patients with a primary or secondary diagnosis of pulmonary edema, acute heart failure exacerbation, hypertensive emergency, or hypertensive crisis and were initiated on NTG in the ED.
Exclusion: hypertensive emergency with different BP goals (dissection, eclampsia, ICH)
Study groups: based on initial NTG dose (<100 mcg/min = low dose, ? 100 mcg/min = high dose)
Primary outcome: time from NTG initiation to oxygen weaning (removal of necessary oxygen back to baseline or home oxygen
Baseline: 61 years old, 50% male, 97% with history of hypertension, 84% history of heart failure, and 36% with ESRD. A higher percentage of patients in the high dose group has CPAP/BIPAP (49% vs 27% p<0.001)
Results: High dose NTG group had a shorter time from NTG to oxygen wean of 2.67h compared to 3.28 hours in the low group. The high dose group also was more likely to achieve goal SBP reduction of 25% within the hour (55% v 34%, p<0.001) had a shorter duration of NTG infusion overall 4.9h vs 6.9h, p0.033) and had decreased ICU LOS by 0.5 days. There were more cases of hypotension in the high dose group which was primarily driven by acute drops in SBP >30%.
Bottom Line: Consider using NTG 100 mcg/min initially to manage patients with SCAPE in the ED.
Henry K, Pelsue B, Hartman H, Gulbis B. Low versus high dosing strategies of intravenous nitroglycerin for the management of sympathetic crashing acute pulmonary edema. Am J Emerg Med. 2025; 98:41-45.
Category: Gastrointestional
Keywords: TXA, GI bleeding (PubMed Search)
Posted: 12/10/2025 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
A recent study in AJEM reviewed the utility of TXA in GI bleeding
This is a PRISMA?guided systematic review and meta?analysis of 7 RCTs (13,608 adults, 1976–2024) evaluating IV TXA vs placebo in acute gastrointestinal bleeding, including upper and mixed GI sources across multiple countries. The largest contributor is HALT?IT (Roberts et al.), which accounts for nearly 90% of participants.
-Mortality: No statistically significant reduction in all?cause mortality with TXA (OR 0.77; 95% CI 0.56–1.07, P = 0.12).?
-Rebleeding: TXA significantly reduced rebleeding events (OR 0.64; 95% CI 0.45–0.91, P = 0.01).?
-"Failure to control" bleeding: TXA reduced failure of hemostasis (OR 0.55; 95% CI 0.32–0.93, P = 0.03).
-Thromboembolic events: Random?effects model showed no significant difference (OR 1.28; 95% CI 0.51–4.51, P = 0.46), but fixed?effect analysis suggested a statistically significant increase (OR 1.28; 95% CI 1.07–1.55, P = 0.009), highlighting a possible thrombotic signal.?
-Transfusion and LOS: No significant reduction in blood transfusion requirements with TXA (OR 0.94; 95% CI 0.61–1.43, P = 0.76); length of stay and other resource metrics were variably reported and not clearly improved.
Take-Aways:
TXA may be reasonable as an adjunct in GI bleeding when the goal is to reduce rebleeding or “failure to control” bleeding, but current evidence does not support it as a mortality?reducing therapy.?
Given a potential increased risk of thromboembolic events, TXA should be used cautiously in patients with high baseline thrombotic risk, and always as part of a broader package including resuscitation and timely endoscopy rather than as a standalone intervention.
Djoudjou T, Alamri O, Aljuwayr A, et al. Intravenous tranexamic acid in gastrointestinal bleeding: A systematic review and meta-analysis of randomized controlled trials. Am J Emerg Med. 2025;97:175-182. doi:10.1016/j.ajem.2025.07.050
Category: Critical Care
Keywords: septic shock, capillary refill time, personalized medicine, fluids, vasopressors, resuscitation (PubMed Search)
Posted: 12/9/2025 by Jessica Downing, MD
Click here to contact Jessica Downing, MD
Last month, Mark Sutherland posted an overview of a new article investigating the use of personalized MAP targets in resuscitation for septic shock (1). Now, the authors of ANDROMEDA-SHOCK-2 (2) suggest a new multimodal approach to personalize resuscitation in septic shock that largely operates outside of the traditional focus on MAP and lactate.
In 2019, the ANDROMEDA-SHOCK Trial (3) suggested that capillary refill time (CRT) may be a better resuscitation in septic shock than lactate. Now, the same group is suggesting that a stepwise algorithm to guide resuscitation may provide more optimal and “personalized” results when compared to usual care for patients with abnormal CRT:
Tier 1: If CRT is abnormal, assess pulse pressure (PP) and DBP:
Tier 2: If CRT remains abnormal despite the above, use POCUS to assess for cardiac dysfunction.
The authors found that at 6 hours, following the protocol resulted in increased use of dobutamine, lower fluid balance, and similar CVP and MAP with lower lactate levels and CRT. They reported an improvement in their composite hierarchical outcome at 28 days, primarily driven by a shorter duration of organ support (vasoactives, mechanical ventilation, renal replacement therapy) and among sicker patients. No difference in mortality was observed between groups.
Food for Thought:
Study Details:
Category: Pediatrics
Keywords: Pediatrics, CT scans, PEM (PubMed Search)
Posted: 12/5/2025 by Taylor Lindquist, DO
(Updated: 2/8/2026)
Click here to contact Taylor Lindquist, DO
A large-scale retrospective study of 3.7 million children found an association between radiation exposure from medical imaging and a small but significantly increased risk of developing hematologic cancers (primarily leukemia).
Finding: Cancer risk increased with cumulative radiation dose
Dose-Response: For the highest exposure group (50 to <100 mGy), the Relative Risk (RR) for hematologic cancer was 3.59 compared to no exposure.
Attributable Risk: An estimated 10.1% of hematologic cancers in the cohort may have been attributable to medical imaging radiation, with CT scans being a major contributor.
Vulnerability: Children are more susceptible to radiation-induced cancer due to their heightened radiosensitivity and longer life expectancy for the cancer to manifest.
Take Away: Providers should critically assess the necessity of high-dose imaging like CT scans and use the lowest effective dose or possible alternative imaging (e.g. US, MRI, etc.) to prevent unnecessary cumulative exposure.
Medical Imaging and Pediatric and Adolescent Hematologic Cancer Risk. N Engl J Med. 2025 Oct 2;393(13):1269-1278. doi: 10.1056/NEJMoa2502098. Epub 2025 Sep 17. PMID: 40961449; PMCID: PMC12445590.
Category: Ultrasound
Posted: 12/3/2025 by Kerith Joseph, MD
(Updated: 12/4/2025)
Click here to contact Kerith Joseph, MD
Summary
Objective:
The study aimed to determine how a brief educational intervention could enable emergency medicine (EM) residents to use point-of-care ultrasound (POCUS) effectively to diagnose and manage shoulder dislocations in the emergency department (ED).
Methods:
Conducted at an academic teaching hospital in Miami, Florida.
Twenty EM residents (PGY1–PGY4) with no prior shoulder ultrasound training participated.
Residents received <1 hour of in-service training, including a short lecture, video instruction, and hands-on practice using a Sonosite M-Turbo ultrasound device.
Over one year (2016–2017), residents prospectively enrolled 78 adult patients with suspected shoulder dislocation.
POCUS findings were compared with x-rays (the gold standard) for accuracy.
Time to diagnosis and reduction confirmation were recorded.
Results:
55 of 78 patients were diagnosed with dislocation; 53 anterior, 1 posterior, 1 inferior.
POCUS achieved 100% sensitivity and specificity for diagnosing and confirming successful reductions compared to x-ray.
Ultrasound results were available ~22 minutes faster for diagnosis and ~27 minutes faster for reduction confirmation than x-rays (p < 0.0001).
Residents across all training years performed equally well.
POCUS also identified 14 fractures (12 confirmed by x-ray, 2 seen only on ultrasound).
Discussion:
A short educational session enabled residents to accurately use POCUS for shoulder dislocation diagnosis and management.
POCUS reduced diagnostic time, avoided radiation exposure, and may improve ED workflow and patient comfort.
Findings support including shoulder ultrasound as a core component of EM training, filling a current gap in national ultrasound education guidelines.
Limitations:
Convenience sample and single-center design.
Some selection bias and inherent limitations of POCUS-based studies.
Conclusion:
Emergency medicine residents can learn to diagnose and manage shoulder dislocations with excellent accuracy after brief ultrasound training. POCUS should be integrated into EM residency curricula as a core skill for musculoskeletal emergencies.
Category: Toxicology
Keywords: Nitrous Oxide, Whippit, unregulated psychotropic, inhalant abuse (PubMed Search)
Posted: 12/2/2025 by Kathy Prybys, MD
(Updated: 12/3/2025)
Click here to contact Kathy Prybys, MD

Vohra V, Matthews H, Stroh-steiner G. Notes from the field: Recreational Nitrous Oxide Use-Michigan, 2019-2023. MMWR Morb Mort Wkly Rep 2025;74:210-212. DOI: http://dx.doi.org/10.15585/mmwr.mm7412a3.
Gummin D, Mowry J, Beuhler MC, et.al (17 Dec 2024): 2023 Annual Report of the National Poison Data System® (NPDS) from America’s Poison Centers®: 41st Annual Report, Clinical Toxicology, DOI: 10.1080/15563650.2024.2412423
Yockey RA, Hoopsick RA. US Nitrous Oxide Mortality. JAMA Netw Open. 2025;8(7):e2522164. doi:10.1001/jamanetworkopen.2025.22164.
https://www.fda.gov/food/alerts-advisories-safety-information/fda-advises-consumers-not-inhale-nitrous-oxide-products. FDA Advises Consumers Not to Inhale Nitrous Oxide Products 6/4/2025
Category: Critical Care
Keywords: Shock, procedures, arterial line, blood pressure, mean arterial pressure, MAP (PubMed Search)
Posted: 12/2/2025 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
We have all been there – an ED patient with circulatory shock requiring vasoactive medications and, therefore, an arterial line for accurate and close monitoring of the MAP and appropriate titration of the infusions. But does it save lives?
The recently published NEJM article by Muller et al. takes a look at noninvasive BP monitoring (NIBP) by cuff versus early arterial catheterization in patients with hypotension and evidence of tissue hypoperfusion:
Bottom Line: This trial indicates that in appropriately-selected patients with shock, such as those not on high doses of vasopressors, with BMI < 40 and an ability to consistently obtain NIBP measurements, early arterial line placement in the ED for vasopressor titration is unlikely to improve outcomes. It is important to note other potential indications for arterial line placement (severe hypoxia, inability to obtain reliable SpO2 with need for ABG monitoring, cardiac arrest, pain related to NIBP cuff monitoring, intracranial hemorrhage, etcetera) may still make arterial line placement in the ED prudent and better for overall patient care.
*France refers to norepi by the tartrate formulation dose, US refers to the base norepi dose (ratio is 2:1 tartrate: base).
Muller G, Contou D, Ehrmann S, et al.; CRICS-TRIGGERSEP F-CRIN Network and the EVERDAC Trial Group. Deferring Arterial Catheterization in Critically Ill Patients with Shock. N Engl J Med. 2025;393(19):1875-1888. doi: 10.1056/NEJMoa2502136.
