Category: Ultrasound
Keywords: POCUS, testicular pain (PubMed Search)
Posted: 12/1/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
POCUS can be performed at the bedside to evaluate for acute scrotal conditions, including testicular torsion and inflammatory processes such as epididymo-orchitis.
A high-frequency linear transducer is typically used to scan the scrotum in two different planes. Additionally, a coronal "buddy view"—displaying both testes side by side—can aid in comparing echogenicity and vascularity.
On B-mode imaging, both testicular torsion and inflammatory conditions may present with testicular swelling and decreased homogeneity. However, color and power Doppler imaging can help to differentiate:
Inflammatory conditions (e.g., epididymo-orchitis) typically show increased vascular flow on color and power Doppler.
Testicular torsion usually demonstrates reduced or absent flow in the affected testis. However, in cases of intermittent torsion-detorsion, vascular flow may appear preserved or even increased. In such scenarios, repeat Doppler imaging after one hour may help clarify the diagnosis.
Kumar K, Kumari M, Kumar V, Suman SK. Evaluation of Scrotal Pathologies by Ultrasound and Color Doppler. Cureus. 2023 Mar 27;15(3):e36776. doi: 10.7759/cureus.36776
Acuña JG, Adhikari SR. Small Parts – Testicular Ultrasound. Sonoguide. American College of Emergency Physicians. Published April 1, 2025. Accessed December 1, 2025. https://www.acep.org/sonoguide/advanced/testicular
Category: Infectious Disease
Keywords: sepsis, intrabdominal, source control (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 11/30/2025)
Click here to contact Robert Flint, MD
Intraabdominal infections leading to sepsis can come from cholecystitis, small bowel perforation, gastric perforation, left sided colonic diverticulitis, right sided diverticulitis and appendicitis. When to initiate source control and antibiotics is controversial. These authors propose breaking patient populations into three groups:
From this they propose algorithms to treat these intraabdominal infections such as (note the different approach to right and left diverticulitis):
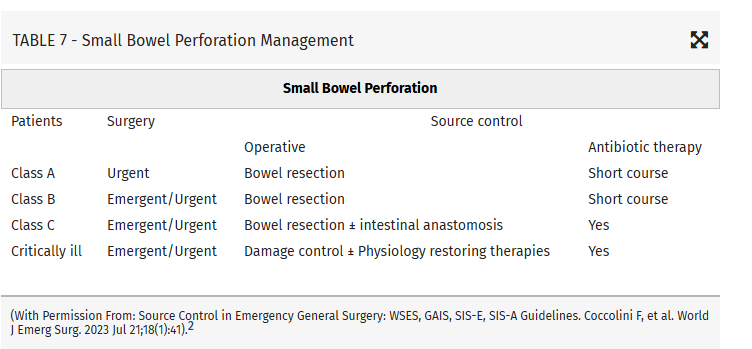
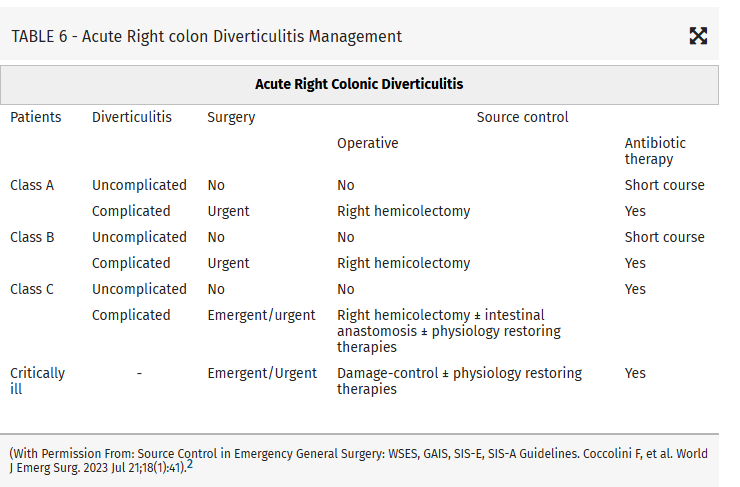
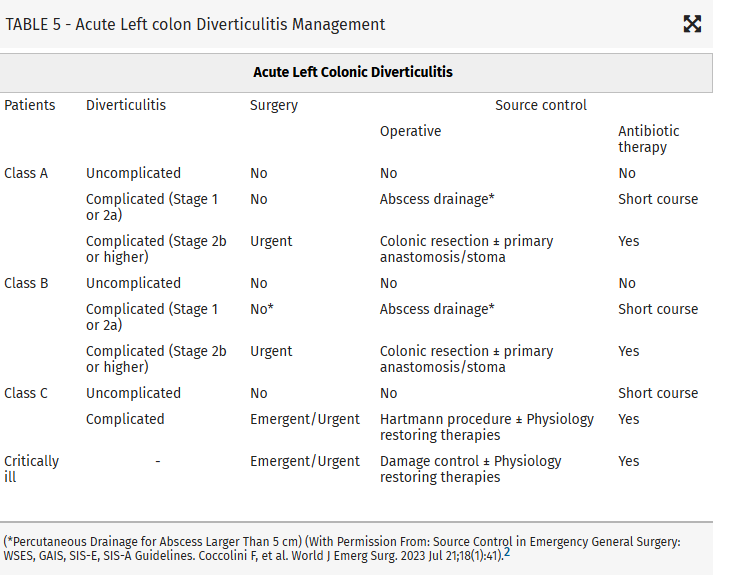
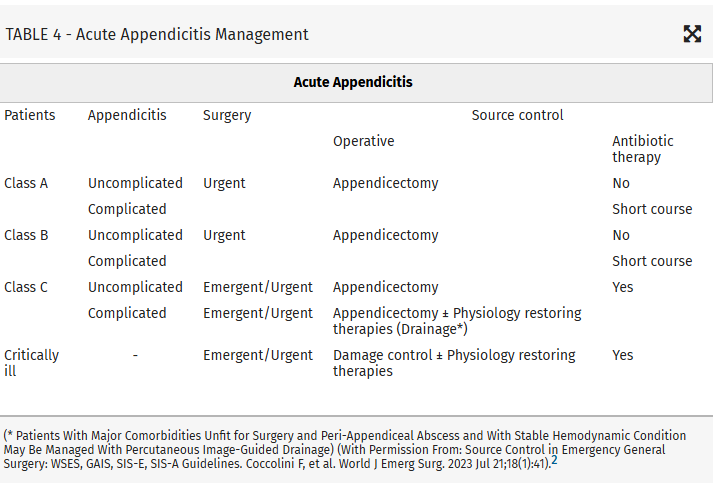
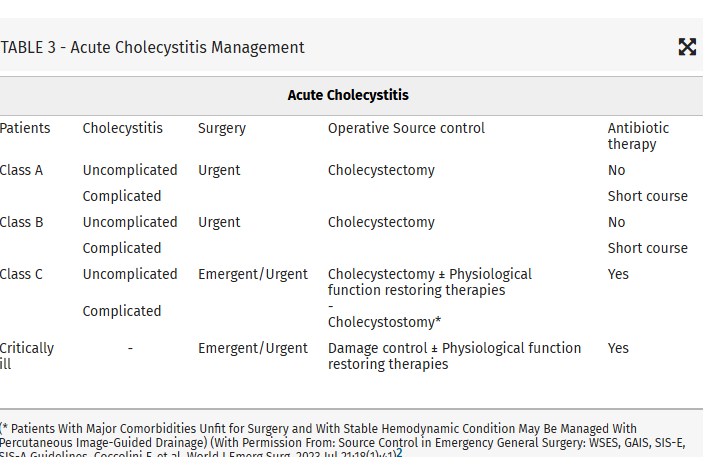
Coccolini, Federico MD, PhD; Kirkpatrick, Andrew W. CD, MD, MHSc, FRCSC, FACS; Cremonini, Camilla MD, PhD; Sartelli, Massimo MD, PhD. Source control in intra-abdominal infections: What you need to know. Journal of Trauma and Acute Care Surgery 99(5):p 669-678, November 2025. | DOI: 10.1097/TA.0000000000004654
Category: Infectious Disease
Keywords: sepsis, intrabdominal source, source control (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 11/29/2025)
Click here to contact Robert Flint, MD
This article looks at source control as it relates to intrabdominal sources for sepsis. Key take aways are:
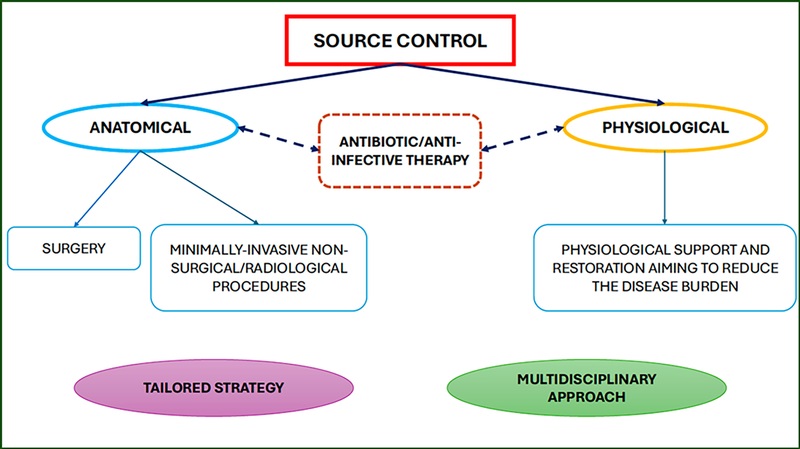
Those at high risk of morbidity and mortality from intraabdominal infection associated sepsis include:
Mild–moderate immune deficiency: Elderly (according to the age and general status of the patient), Malnourished, Diabetic, Burns, Trauma, Uremic, Active malignancy, not on chemotherapy, HIV with CD4+ count >200/mm3, Splenectomized, Severe immune deficiencyAIDS HIV with CD4+ count <200/mm3, Transplant (solid organ, bone marrow), High-dose steroids (more than 20 mg/day prednisone), Malignancy on chemotherapy, Neutrophil count <1,000/mm3
High-risk population (medical or surgical causes)Low serum albumin concentration Older age Obesity Smoking Diabetes mellitus Ischemia secondary to vascular disease or irradiation Prolonged or delayed/late procedures
Coccolini, Federico MD, PhD; Kirkpatrick, Andrew W. CD, MD, MHSc, FRCSC, FACS; Cremonini, Camilla MD, PhD; Sartelli, Massimo MD, PhD. Source control in intra-abdominal infections: What you need to know. Journal of Trauma and Acute Care Surgery 99(5):p 669-678, November 2025. | DOI: 10.1097/TA.0000000000004654
Category: Misc
Keywords: prescribing, racial, disparity (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/28/2025)
Click here to contact Robert Flint, MD
Comparing prescribing patterns from early 2000s to late 2010s in the National Hospital Ambulatory Medical Care Survey, these authors found we continue to under prescribe pain medications to non-white patients for traumatic injuries.
Day, Jessica et al.
Journal of Emergency Medicine, Volume 78, 184 - 191
Category: Geriatrics
Keywords: frail, frailty scale, geriatrics, critical care (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/27/2025)
Click here to contact Robert Flint, MD
A prospective cohort of South Korean patients over 65 years admitted from the ED with critical illness had Clinical Frailty Scale (CFS) performed on them. Those with a high CFS had increased 3 month mortality. CFS helps us prognosticate morbidity and mortality in our older critically ill patients.
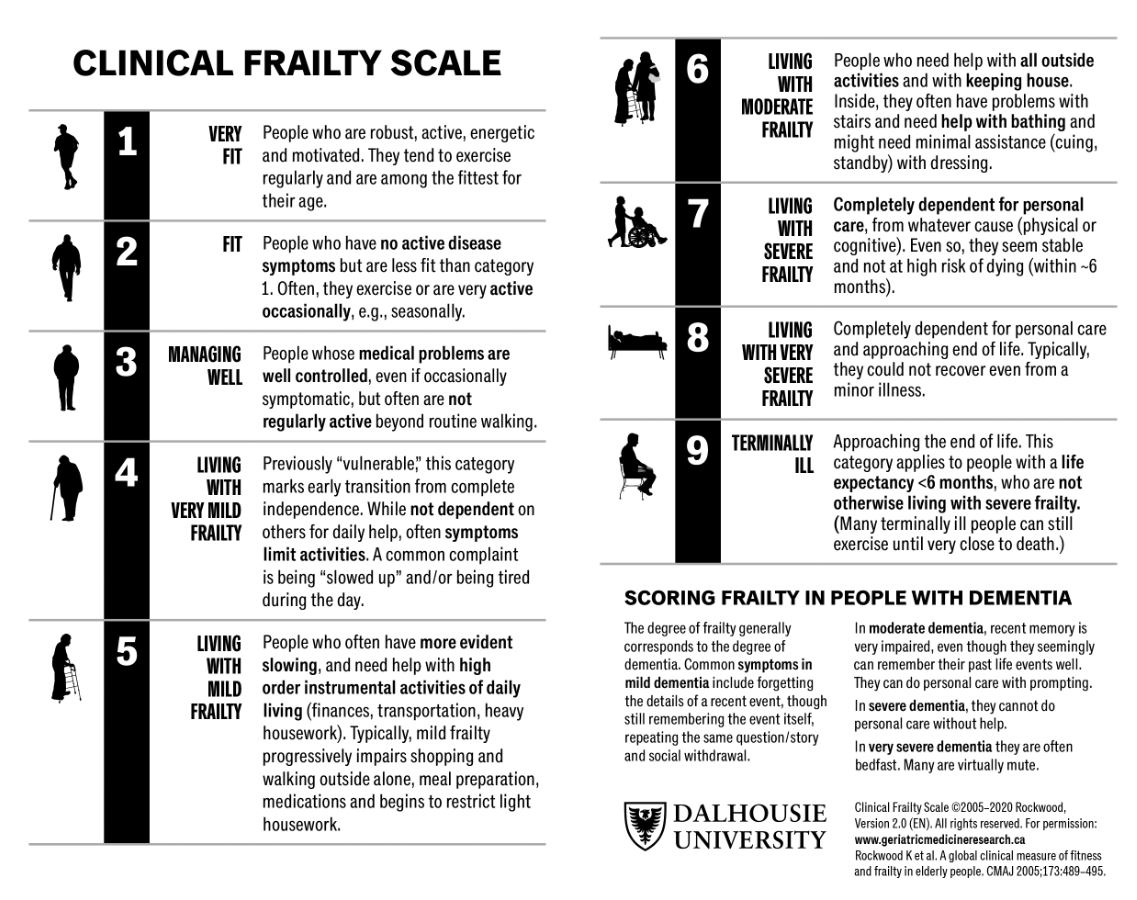
Um, Young Woo et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Administration
Keywords: artificial intelligence, emergency department, emergency practice, machine learning (PubMed Search)
Posted: 11/26/2025 by Mercedes Torres, MD
(Updated: 2/8/2026)
Click here to contact Mercedes Torres, MD
Food for thought on this Thanksgiving eve…
AI is rapidly being integrated into the practice of emergency medicine, as well as many other medical specialties. Similar to the adage, "you are what you eat," AI is what we feed it. See below for an introduction to the various levels of bias contributing to the machine learning process:
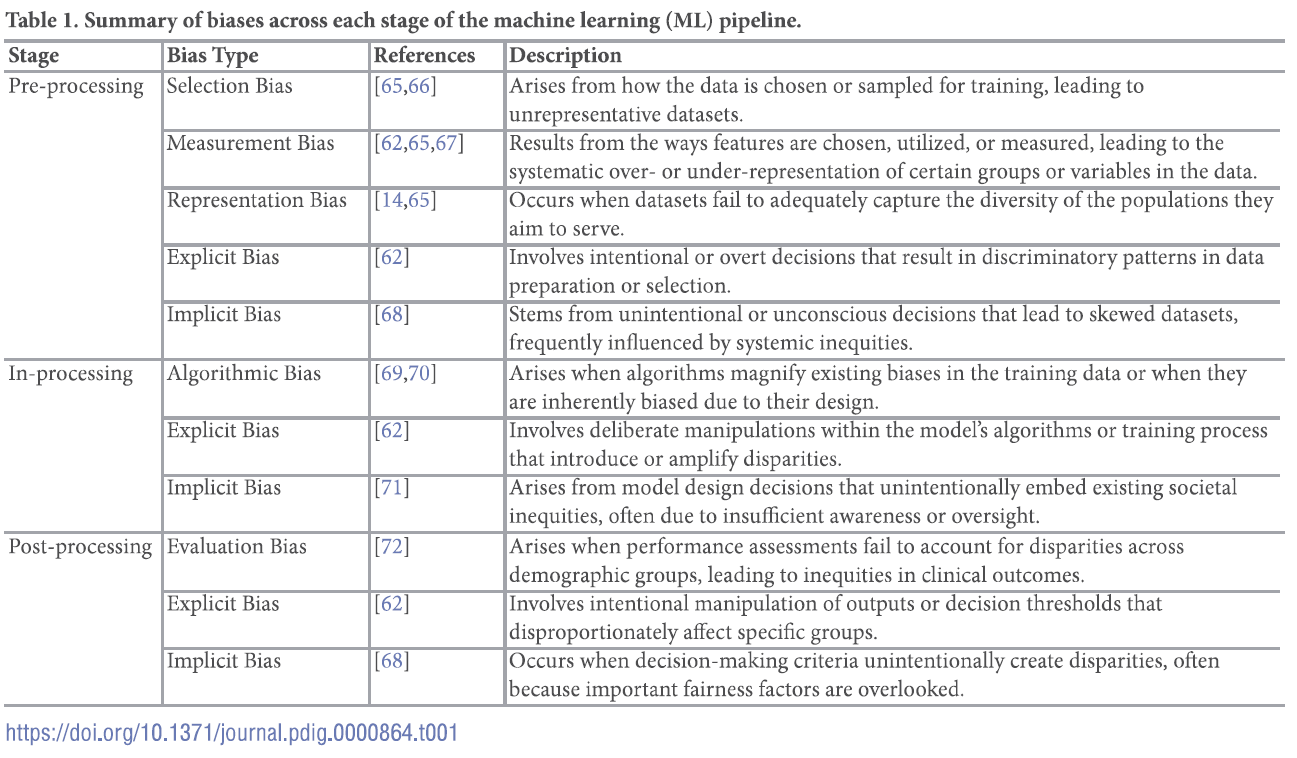
For a deep dive into the world of bias in AI, see referenced article.
Chinta SV, Wang Z, Palikhe A, Zhang X Kashif A, Smith MA, et al. (2025) AI-driven healthcare: A review on ensuring fairness and mitigating bias. PLOS Digit Health 4(5): e0000864. https://doi.org/10.1371/journal.pdig.0000864
Category: Critical Care
Keywords: critically ill, ED, boarding, outcome (PubMed Search)
Posted: 11/25/2025 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
Settings: this is a meta-analysis of 17 observational studies about boarding of critically ill patients in US Emergency Departments. All studies were from urban, academic centers.
Participants:
Outcome measurement: all cause mortality, as reported by the authors of the original studies.
Study Results:
Discussion:
Conclusion:
Critically ill patients boarding in the U.S. Emergency Departments were associated with a non-statistically signi?cant increase in odds of mortality and hospital length of stay compared to non-boarded patients
Htet NN, Walker JA, Jafari D, Rech MA, Hintze T, Moran M, Bai J, Dinh K, Essaihi A, Wilairat S, Huddleson B, Tran QK. Outcomes of boarding critically ill patients in U.S. EDs: A systematic review and meta-analysis. Am J Emerg Med. 2025 Oct 17;99:339-347. doi: 10.1016/j.ajem.2025.10.036. Epub ahead of print. PMID: 41151219.
Category: Critical Care
Keywords: bicarbonate, metabolic acidosis, renal replacement therapy, acute kidney injury (PubMed Search)
Posted: 11/25/2025 by Jessica Downing, MD
Click here to contact Jessica Downing, MD
The role of sodium bicarbonate in the treatment of severe acidemia has been controversial, with some studies suggesting no benefit, and others indicating that it may help reduce need for renal replacement therapy (RRT) and even improve mortality. The BICARICU-2 Trial was an open-label multicenter RCT conducted in France that evaluated the impact of a bicarb infusion among patients with metabolic acidosis and moderate to severe AKI.
There was no difference in 90 day mortality, but patients in the bicarb group were less likely to be started on RRT (38% vs 47% in the control group) using pre-defined criteria for RRT initiation, and had a 50% lower rate of bloodstream infections. Patients in the bicarb group who were started on RRT met criteria for RRT later than those in the control group (median 31h vs 15.5h).
Study Details:
Patient Population:
Intervention:
RRT Triggers:
Jung B, Jabaudon M, De Jong A, Bitker L, Audard J, Klouche K, Sarton B, Guitton C, Lasocki S, Rieu B, Canet E, Jeantrelle C, Roquilly A, Mayaux J, Verdonk F, Pottecher J, Ferrandiere M, Riu B, Garcon P, Assefi M, Detouche P, Forel JM, Roger C, Bourenne J, Jacquier S, Bougon D, Rolle A, Corne P, Benchabane N, Richard JC, Asehnoune K, Chanques G, Reignier J, Belafia F, Fosset M, Huguet H, Futier E, Molinari N, Jaber S; BICARICU-2 Study Group. Sodium Bicarbonate for Severe Metabolic Acidemia and Acute Kidney Injury: The BICARICU-2 Randomized Clinical Trial. JAMA. 2025 Oct 29:e2520231. doi: 10.1001/jama.2025.20231. Epub ahead of print. PMID: 41159812; PMCID: PMC12573113.
Category: Infectious Disease
Keywords: Dalbavancin, bacteremia, antibiotics, transitions of care (PubMed Search)
Posted: 11/17/2025 by Lena Carleton, MD
(Updated: 11/24/2025)
Click here to contact Lena Carleton, MD
Treatment of Staphylococcus aureus bacteremia has traditionally required several weeks of intravenous antibiotics. This approach carries medical risks, such as catheter-associated infection or thrombosis, as well as significant social and financial burdens for patients. Dalbavancin, a long-acting intravenous lipoglycopeptide with activity against S. aureus (including MRSA), has been proposed as a more convenient alternative. This study evaluated the efficacy and safety of dalbavancin compared with standard therapy for S. aureus bacteremia.
Two hundred adults were enrolled in this open-label, randomized clinical trial, which was conducted in the United States and Canada. After blood cultures cleared, participants were randomized to complete therapy with dalbavancin (administered on Days 1 and 8) or with standard treatment (cefazolin for MSSA and vancomycin or daptomycin for MRSA).
The primary outcome was the Desirability of Outcome Ranking (DOOR) at Day 70, incorporating five domains: clinical success, infectious complications, safety events, mortality, and health-related quality of life.
Dalbavancin was not superior to standard therapy for treating S. aureus bacteremia, and adverse events were similar between groups. A key strength of this study was the inclusion of people who inject drugs, a population at high risk for S. aureus bacteremia and often underrepresented in trials. A major limitation was that the DOOR metric did not account for important social and economic factors, such as disposition (home versus skilled nursing facility), caregiver burden, or treatment cost.
Key Takeaway: Dalbavancin may be a suitable alternative to traditional therapy for Staphylococcus aureus bacteremia, offering less frequent dosing and a shorter treatment course. Further research is needed to identify which patients benefit most and to evaluate its impact on social and economic factors such as discharge disposition, caregiver burden, and treatment costs.
Turner NA, Hamasaki T, Doernberg SB, et al. Dalbavancin for Treatment of Staphylococcus aureus Bacteremia: The DOTS Randomized Clinical Trial. JAMA. 2025;334(10):866–877. doi:10.1001/jama.2025.12543
McCreary EK, Malani PN. New Pathways to Treat Staphylococcus aureus Bacteremia: Connecting the DOTS. JAMA. 2025;334(10):861–863. doi:10.1001/jama.2025.13717
Category: Trauma
Keywords: brain injury, score, prediction (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/23/2025)
Click here to contact Robert Flint, MD
In 252 mild traumatic brain injury patients seen at 3 level I centers that were given the Rivermead Post Concussion Symptoms Questionnaire within 24 hours of arrival, 3 month post concussive symptoms were significantly correlated with their score on the questionnaire. This questionnaire take 3 minutes to complete. This may be helpful in prognosticating who will have post-concussive symptoms and who will need additional follow up.
Gray, Samuel et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Orthopedics
Posted: 11/22/2025 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Turf Toe:
Increased recent attention due to injuries in high profile athletes
Sprain of the first MTP joint
Mechanism: Forced hyperextension of the great toe (most common)
https://briandorfman.com/wp-content/uploads/2015/11/b_12_3_6a.jpg
Causes injury to the MTP joint capsule and surrounding ligaments
Presents as pain, swelling, discoloration, tenderness to palpation, possible joint laxity
Pain with active and passive ROM (both flexion and extension)
Graded 1-3 (Sprain, partial rupture, significant/complete rupture)
Most commonly seen in athletes who compete on artificial turf.
More rigid than natural grass
Synthetic surfaces do not release cleats as easily as natural grass
Improved synthetic surfaces perform more similar to natural grass
Much higher incidence in games vs practices.
In football, quarterbacks and running backs at highest risk
Between 30 and 45% of professional football players claim that they have experienced a turf toe injury, with over 80% of those injuries occurring on artificial turf
The combination of more rigid synthetic surfaces and lighter, more flexible shoes, increase risk of hyperextension injuries
Treatment: usually non operative
Rest/ice/taping after acute swelling decreased/stiff sole shoe/crutches/NSAIDs.
Consider walking boot or short leg splint for severe injuries
Less than 2% of injuries require surgery
Category: Pediatrics
Keywords: Community EDs, pediatric patients, mortality (PubMed Search)
Posted: 11/21/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Children account for up to 20% of emergency department visits. In the US, up to 90% of children’s visits to emergency departments are to general EDs. The weighted pediatric readiness score (WPRS) was developed to assess the level of readiness of emergency departments to care for pediatric patients. The last assessment was in 2013 showed a mean score of 68.9. High readiness scores have been associated with decreased mortality. The same holds true for children with injuries presenting to trauma centers. The higher the WPRS score, the lower the risk of in hospital death. There was no difference if the patient presented in cardiac arrest. A 10 point increase in WPRS is associated with a lower odds of potentially avoidable transfers in both trauma and medical patients. More recent data has been collected, but has not yet been published. More information on pediatric readiness (for hospitals and EMS) can be found at: https://emscimprovement.center/domains/pediatric-readiness/.
Bottom line: Being Pediatric Ready improves the care of children.
Harper JA, Coyle AC, Tam C, Skakum M, Ragheb M, Wilson L, Lê ML, Klassen TP, Aregbesola A. Readiness of emergency departments for pediatric patients and pediatric mortality: a systematic review. CMAJ Open. 2023 Oct 17;11(5):E956-E968. doi: 10.9778/cmajo.20210337. PMID: 37848258; PMCID: PMC10586495.
Category: Geriatrics
Keywords: hip fracture, nerve block, mortality, delerium (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/20/2025)
Click here to contact Robert Flint, MD
In reviewing the limited literature available, the authors found that fascia iliaca blocks did not improve mortality but did improve hospital length of stay, decreased opiate use, and decreased delirium rates. More research is needed, however this tool should be added to our multimodal pain control toolbox.
Finch, Alexander S. et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: EMS
Keywords: VF, AED, CPR, public health (PubMed Search)
Posted: 11/19/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Early defibrillation is a key step in the cardiac arrest chain of survival. Public Access AEDs may be available more readily than waiting for first responders. Outside of simple awareness of where AEDs are located, there are newer ways to become aware of public AEDs near a cardiac arrest including cell phone apps or information given by 911. A British study showed that only 5.9% of AEDs were within 100 meters of the patient and 35% were within 500 meters. The distance between the AED and arrest may be a barrier for bystander AED use. This study looked to determine the time required to retrieve an AED and they hypothesized that a distance > 400 meters would be longer than the EMS response times.
This study used 15 women and 15 men to perform different runs in various environments in different seasons, retrieving AEDs at 200m through 600m and bringing it back to the patient. In these scenarios, only the 200m distance (400 m round trip) times were deemed to allow enough time to apply and use the AED prior to EMS arrival. Barriers to AED retrieval included traffic lights, cars, weather and pedestrians.
Gramm ER, Gumucio JA, Flickinger K, Salcido DD, Menegazzi JJ. Improving Bystander Response: How Long Does It Take to Retrieve an AED From Varying Distances. Prehosp Emerg Care. 2025 Apr 1:1-5. doi: 10.1080/10903127.2025.2475323. Epub ahead of print. PMID: 40126392.
Category: Critical Care
Posted: 11/18/2025 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
This is an actual patient case:
65 y/o pt intubated for hemoptysis and started on nebulized transexamic acid. Overnight, the pt is found to have severe breath stacking/auto-PEEPing and consequently is started on neuromuscular blockade. The pt has no history of asthma or COPD and the ETT is clear without obstruction.
Ventilator waveforms are as shown. What is the issue?
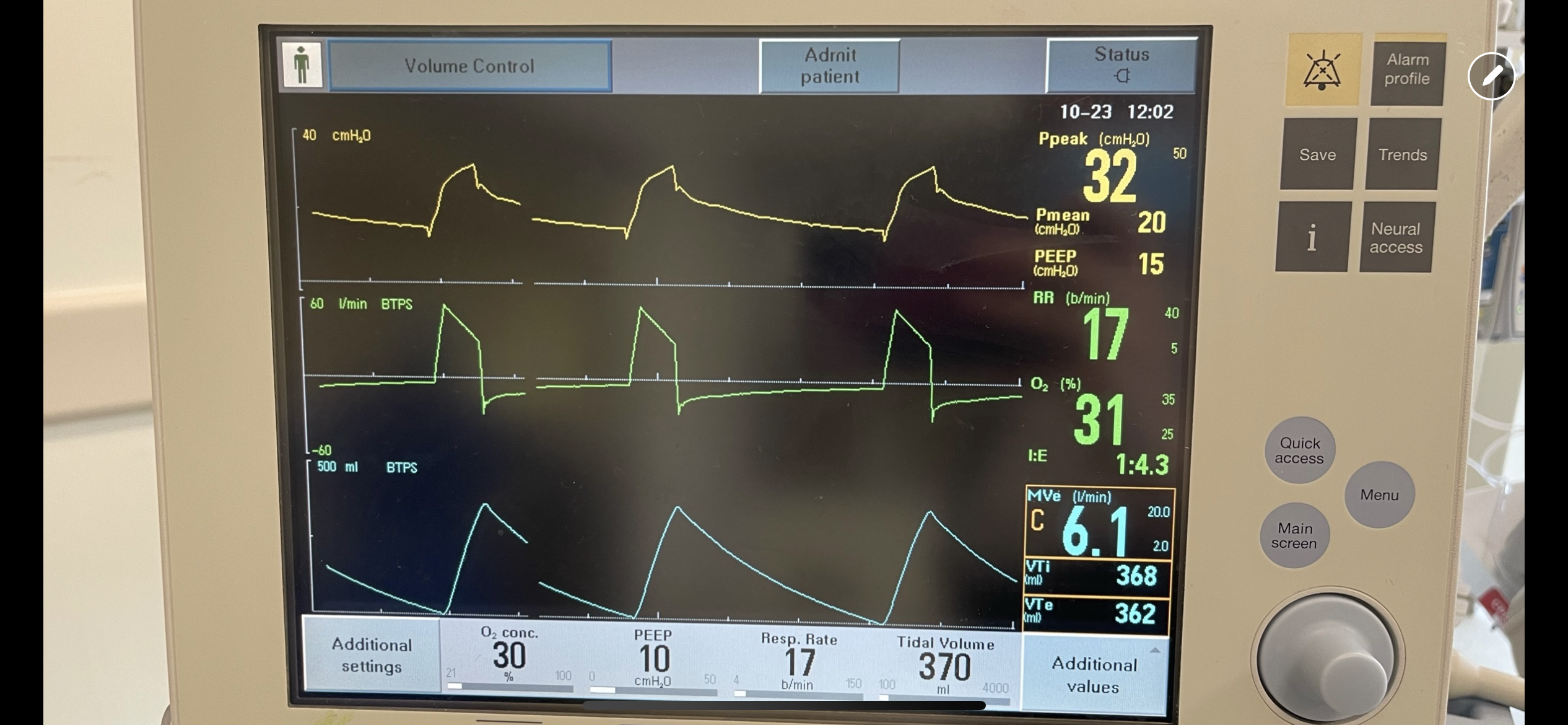
Explanation:
On expiration, the ventilator pressure (and the pressure curve waveform on the ventilator) should drop to the set PEEP (10 cm H2O in this case) immediately. This is true regardless of whether it is volume control, pressure control, PRVC etc. For this patient, the pressure curve is not dropping to the set PEEP immediately on expiration, rather, it slowly decays and does not even reach the set PEEP before the beginning of the next breath. This is not due to a patient issue, but rather an obstruction at the level of the ventilator. In particular, an obstruction in the expiratory limb of the tubing where flow returns to the ventilator from the patient. TXA is known to crystallize on the expiratory filter which can cause this type of obstruction if it is not changed frequently enough, preventing the pressure from dropping to PEEP and the patient from fully exhaling.
In this case, the obstruction was localized to the expiratory filter based on the ventilator waveforms and the filter was exchanged. The waveforms normalized, the patient had no obstruction or breath stacking, the neuromuscular blockade discontinued, and the patient was subsequently extubated without issue.
Category: Trauma
Keywords: rsi, neck injury, penetrating, airway (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/16/2025)
Click here to contact Robert Flint, MD
This group looked at 88 patients intubated for penetrating neck injury and found 95% received neuromuscular blocking agents, 73% were intubated using a bougie, and 95% were intubated on first pass.
The authors concluded; “Rapid sequence intubation with bougie use was an effective default approach to definitive airway management in ED patients with penetrating neck trauma.”
Lee, Daniel H. et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Administration
Posted: 11/15/2025 by Kevin Semelrath, MD
(Updated: 2/8/2026)
Click here to contact Kevin Semelrath, MD
This abstract from ACEP's most recent research forum looked at the effect a patient's preferred language had on ED LOS, rate of admission, hospital length of stay and resource utilization both in the ED and the hospital.
Overall, those patients who spoke English as their primary language had lower ED LOS, less testing done in the ED, but if they got admitted they had the longest hospital LOS. Patients who preferred Spanish language had the shortest hospital LOS and were most likely to be discharged home with no services. Non-English/non-Spanish languages had the longest ED LOS and highest admission rates and had similar resource use as patients who preferred Spanish
This abstract opens the door for further research into what the underlying cause of these disparities are.
Zimmerman, T. et al.
Annals of Emergency Medicine, Volume 86, Issue 3, S3 - S4
Category: Pharmacology & Therapeutics
Keywords: andexanet alfa, 4F-PCC, Kcentra, ICH, thrombosis (PubMed Search)
Posted: 11/13/2025 by Wesley Oliver
(Updated: 2/8/2026)
Click here to contact Wesley Oliver
This pearl was adapted from a literature update presented by Castin Schulz, PharmD on November 13, 2025.
A 2025 study in the American Journal of Emergency Medicine provides new real-world data on the two most common reversal agents for factor Xa (fXa) inhibitor-related intracranial hemorrhage (ICH).
This national retrospective cohort study evaluated 350 Veterans who received either andexanet alfa (AA) or 4-factor prothrombin complex concentrate (4F-PCC) for fXa inhibitor-related ICH.
Key Findings (Propensity-Matched Analysis)
Clinical Takeaway
In this study of Veterans with fXa inhibitor-related ICH, andexanet alfa did not improve 90-day mortality compared to 4F-PCC. However, its use was associated with a significantly increased risk of 30-day thrombotic events, particularly ischemic stroke.
This study adds to a growing body of literature questioning the safety profile of AA. The authors conclude that the selection of AA should be carefully weighed against the patient's underlying risk of thrombotic events.
Rech MA, Budde E, Evans CT, et al. Andexanet alfa increases 30-day thrombotic events relative to four-factor prothrombin complex concentrate for factor Xa inhibitors-related intracerebral hemorrhage in veterans. Am J Emerg Med. 2025;97:97-102. doi:10.1016/j.ajem.2025.07.037
Category: Gastrointestional
Keywords: gastroenteritis, odansetron, prescription (PubMed Search)
Posted: 11/12/2025 by Neeraja Murali, DO, MPH
(Updated: 2/8/2026)
Click here to contact Neeraja Murali, DO, MPH
Anecdotally, we as emergency physicians are fairly comfortable prescribing odansetron to adults with nausea and vomiting. However, emergency physicians often treat pediatric gastroenteritis with a single dose of odansetron in the department. A recent study in NEJM examined effects of discharging with odansetron. Full details can be found in the study, but the take-home:
Sending children home with ondansetron after an emergency visit for gastroenteritis cut the rate of moderate-to-severe illness from 12.5% to 5.1% compared to placebo, with no uptick in adverse events. Those taking ondansetron experienced fewer vomiting episodes in the first 48 hours. Targeted, as-needed dosing helps the sickest children recover faster, while avoiding unnecessary medication for most kids.
Freedman SB, Williamson-Urquhart S, Plint AC, et al. Multidose Ondansetron after Emergency Visits in Children with Gastroenteritis. N Engl J Med. 2025;393(3):255-266. doi:10.1056/NEJMoa2503596
Category: Critical Care
Keywords: Critical Care, Surgical Critical Care, Fellowship, Training, Medical education, Emergency Medicine-Critical Care, EM-CC (PubMed Search)
Posted: 11/12/2025 by William Teeter, MD
Click here to contact William Teeter, MD
This study surveyed 111 emergency medicine (EM) trainees to identify factors influencing their choice of critical care (CC) fellowship pathways, particularly surgical critical care (SCC). Respondents included 42 fellows and 69 residents, with most pursuing anesthesiology or medicine CC; only 15 intended SCC.
Key determinants of pathway selection were:
Limited exposure to EM-SCC during residency was noted—only 28% had access to such fellowships, and 42% interacted with surgical intensivists, despite 41% envisioning SCC practice.
Intellectual appeal ranked highest for entering CC, above job prospects or lifestyle.
Fellowship components most valued were:
While descriptive, the authors noted many respondents cited the "preliminary surgical year" as a reason that the Surgical Critical Care pathway is less attractive.
The authors conclude that respondents pursued a career in CC for "intellectual appeal and desire for additional expertise" and that improving EM-SCC matriculation requires targeted interventions.
Hynes AM, Carver TW, Owodunni OP, et al. Attracting Emergency Medicine-Trained Residents to Surgical Critical Care: The Implications From a Nationwide Survey of Emergency Medicine Trainees Interested in Critical Care. Crit Care Med. 2025 Oct 31. doi: 10.1097/CCM.0000000000006935.
