Category: EMS
Keywords: Esophageal intubation, transfer of care (PubMed Search)
Posted: 8/20/2025 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
Unplanned extubation (UE) occurs in 0-25 % of patients intubated in the prehospital setting and transfer of patient care is one time where UE can occur. This EMS jurisdiction wanted to improve the rate of communication and confirmation of tube placement at the time of patient transfer. Over 5 months, the jurisdiction introduced 1) memorandums to paramedics, ED chiefs and respiratory therapist leads, 2) individualized paramedic feedback emails and 3) PCR changes that resulted in documentation of tube placement at transfer of care being a mandatory field.
Initially the rate of verbal ETT position at transfer of care was 74%. This increased to > 90% after 8 weeks. The rate of UE was 2/340 patients. The implementation of this project showed improvements in perceived accountability, interprofessional relationships and satisfaction with interventions that were noted in the post project focus group.
Kwong JL, Bourn S, Hillier M, et al. A Quality Improvement Initiative to Increase Confirmation of Prehospital Endotracheal Tube Placement at Emergency Department Transfer of Care. Prehosp Emerg Care. Published online June 20, 2024. doi:10.1080/10903127.2024.2366401
Category: Critical Care
Keywords: vasopressors, vasopressin, septic shock (PubMed Search)
Posted: 8/18/2025 by Jessica Downing, MD
(Updated: 8/19/2025)
Click here to contact Jessica Downing, MD
Norepinephrine (NE) is widely accepted as the first-line vasopressor for the management of septic shock, supported by the Surviving Sepsis Guidelines (1). The use of vasopressin as a second-line agent is also supported by the Surviving Sepsis Campaign, although the appropriate “triggers” for its addition remain vague. The SSG recommend adding vasopressin when NE infusion rates reach 0.25-0.6 mcg/kg/min, citing a catecholamine-sparing effect and potentially improved mortality (1, 2, 3).
What’s New?
The OVISS study (“Optimal vasopressin initiation in septic shock. The OVISS reinforcement learning study”) used machine learning to derive and internally validate a set of rules guiding the addition of vasopressin to NE for patients with septic shock using multiple databases of patient encounters across multiple institutions (4).
The machine learning model suggested initiation of vasopressin in more patients (87% vs 31%), earlier, and in less sick patients than was seen to be common practice:
Practice consistent with the above triggers was associated with decreased odds of in-hospital mortality (AOR 0.81, 95% CI 0.73-0.91).
Limitations
This was not a prospective study or RCT and was only internally validated. Using databases may limit the number of clinical variables available for analysis, and clinical judgment (how the patient looks) is not reflected.
Bottom Line
Consider adding vasopressin for patients with vasodilatory shock with low MAP despite NE >0.2mcg/kg/min and adequate fluid resuscitation, though more evidence is needed for a strong recommendation. As dual-pressor therapy may be riskier via peripheral IV and vasopressin does not have a direct antidote for extravasation, consider central line placement when adding vasopressin (5,6)
Category: Trauma
Keywords: Pneumothorax, cheat tube, indication (PubMed Search)
Posted: 8/17/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This review article answers the basic question: when does a traumatic pneumothorax require tube thoracostomy?
“A pneumothorax greater than 20% of the thoracic volume on chest x-ray or greater than 35 mm on CT, measured radially from the chest wall to the lung parenchyma, should be treated with tube thoracostomy. Pneumothoraces smaller than this may be observed; approximately 10% of these will fail observation and require tube thoracostomy treatment.”
Blank JJ, de Moya MA. Traumatic pneumothorax and hemothorax: What you need to know. J Trauma Acute Care Surg. 2025 Jul 3. doi: 10.1097/TA.0000000000004692. Epub ahead of print. PMID: 40604368.
Category: Pediatrics
Keywords: DL, VL, neonatal resuscitation, intubation (PubMed Search)
Posted: 8/15/2025 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
The first attempt success rates for neonatal intubation is less than 50%. Video laryngoscopy (VL) has been shown to improve state first pass success compared to direct laryngoscopy (DL) in both children and adults, but few studies have looked at the neonatal population.
This study was a randomized control trial. There was a 74% first pass success rate for VL compared to a 45% first pass success rate for DL. There were no differences in secondary outcomes which include hypoxia, bradycardia, epinephrine administration, oral trauma and correct positioning.
Geraghty LE, Dunne EA, Ní Chathasaigh CM, Vellinga A, Adams NC, O'Currain EM, McCarthy LK, O'Donnell CPF. Video versus Direct Laryngoscopy for Urgent Intubation of Newborn Infants. N Engl J Med. 2024 May 30;390(20):1885-1894. doi: 10.1056/NEJMoa2402785. Epub 2024 May 5. PMID: 38709215.
Lee MJ, Redpath S, Perry JJ. Video versus direct laryngoscopy for urgent intubation of newborn infants. CJEM. 2025 Mar 8. doi: 10.1007/s43678-025-00859-9. Epub ahead of print. PMID: 40056256.
Category: Pharmacology & Therapeutics
Keywords: steroids, asthma, copd (PubMed Search)
Posted: 8/7/2025 by Ashley Martinelli
(Updated: 8/14/2025)
Click here to contact Ashley Martinelli
There are various reasons to give corticosteroids in the emergency department. Many decisions regarding IV vs PO, and the numerous available products can lead to excessive dosing (such as 125mg methylprednisolone). Below is a reference for the most common indications as well as conversion recommendations for each product
Guideline Recommended Dosing for Common ED Indications:
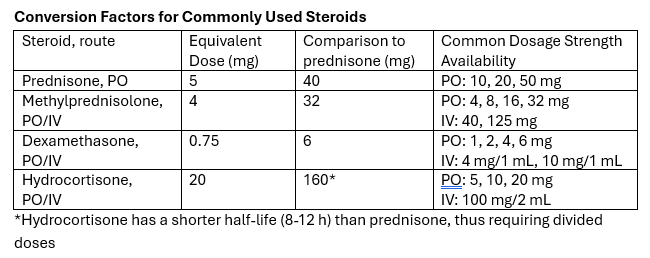
Take-away: Methylprednisolone 125mg is frequently requested but provides a dose equivalent to prednisone 150mg. Consider guideline directed dosing and conversion of products to prevent excessive initial steroid dosing.
Category: Gastrointestional
Keywords: PECARN, abdomen, clinical decision making (PubMed Search)
Posted: 8/13/2025 by Neeraja Murali, DO, MPH
(Updated: 2/7/2026)
Click here to contact Neeraja Murali, DO, MPH
Most of us are probably familiar with the PECARN Algorithm for neuroimaging in pediatric head trauma. But fewer people are familiar with the PECARN Pediatric Intra-Abdominal Injury (IAI) Algorithm.
Inclusion criteria can be found in the original study, referenced below
The original study collected data from 20 studies, and found that CT imaging can be avoided (ie patients are at very low risk for IAI) if the following criteria are met:
-No visible abdominal wall trauma or seatbelt sign
-GCS > 13
-No abdominal tenderness
-No thoracic wall trauma
-No abdominal pain
-No decreased breath sounds
-No vomiting
In the original cohort, 42% of study participants met all of these criteria and the risk of IAI requiring intervention was 0.1%
This study has been validated multiple times since its introduction in 2012, with the most recent being a multicenter study published in the Lancet in 2024. This recent study looked at 7542 children with blunt abdominal trauma, and the IAI rule was fond to have a sensitivity of 100% (95% CI 98-100%) and a negative predictive value (NPV) of 100% (95% CI 99.9-100%).
I know, it seems too good to be true…but the takeaway is that these clinical decision making rules can be more reliable than clinical gestalt in the appropriate patient population.
Holmes JF, Lillis K, Monroe D, et al. Identifying children at very low risk of clinically important blunt abdominal injuries. Ann Emerg Med. 2013;62(2):107-116.e2. doi:10.1016/j.annemergmed.2012.11.009
Holmes JF, Yen K, Ugalde IT, et al. PECARN prediction rules for CT imaging of children presenting to the emergency department with blunt abdominal or minor head trauma: a multicentre prospective validation study. Lancet Child Adolesc Health. 2024;8(5):339-347. doi:10.1016/S2352-4642(24)00029-4
Algorithm: https://www.mdcalc.com/calc/3971/pecarn-pediatric-intra-abdominal-injury-iai-algorithm
Category: Neurology
Keywords: stroke, positioning, LVO, thrombectomy (PubMed Search)
Posted: 8/12/2025 by Nicholas Contillo, MD
Click here to contact Nicholas Contillo, MD
The concept of positioning the head of bed flat in a patient with a neurologic catastrophe seems like a recipe for badness. For most neurologic emergencies, elevating the head of the bed (HOB) to 30° is standard to help control intracranial pressure and reduce aspiration risk. However, emerging evidence indicates that acute large vessel occlusion (LVO) stroke patients—particularly before thrombectomy—may be an important exception.
The ZODIAC trial, published in June of this year, was a prospective, randomized, multicenter study comparing 0° (flat) versus 30° HOB positioning in patients with confirmed LVO stroke awaiting endovascular thrombectomy. The rationale stems from physiologic studies, including transcranial Doppler ultrasonography, showing that flat positioning can improve cerebral perfusion to ischemic tissue.
The primary outcome was early neurologic deterioration (>2-point worsening in NIHSS prior to thrombectomy). Safety endpoints included hospital-acquired pneumonia and all-cause mortality at 3 months.
In the trial’s 92 enrolled patients, flat positioning markedly reduced early neurologic deterioration, which occurred in 2.2% in the 0° group versus 55.3% in the 30° group. There were no significant differences in pneumonia or 3-month all-cause mortality. The authors also found a statistically insignificant improvement in 90-day functional outcomes in the 0° group. Due to the magnitude of benefit, the study was stopped early at interim analysis.
This technique represents a simple, cost-free, and practical method of preventing neurologic decline ahead of definitive management for LVO. This may be especially beneficial for LVO patients who require interhospital transfer to a thrombectomy-capable center.
Bottom Line: For patients with LVO stroke awaiting thrombectomy, flat (0°) head positioning is safe and significantly reduces early neurologic decline by improving blood flow to ischemic brain tissue.
Category: Critical Care
Keywords: intubation, sedation, rapid sequence intubation, RSI, rocuronium, succinylcholine, etomidate, ketamine, propofol (PubMed Search)
Posted: 8/12/2025 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Whether you agree or disagree that “roc rocks and succ sucks,” evidence shows that approximately 3-4% of intubated patients experience awareness while paralyzed [1,2], and more of these patients are in the rocuronium subgroup [2,3,4]. Rocuronium acts in a dose-dependent fashion; the relatively standard 1-1.2 mg/kg in emergency department rapid sequence intubation (RSI) can result in a duration of paralysis can of up to 60-90 minutes. Commonly used sedatives in RSI, however, such as etomidate and ketamine, wear off quickly, before before rocuronium's paralytic effects have abated.
A recent single-center study showed that the majority of patients (60%) receiving rocuronium for paralysis during rapid sequence intubation (RSI) received no additional sedation until more than 15 minutes after induction, whether in the ED or ICU [5].
Patients experiencing awareness during paralysis with post-traumatic stress disorder [1,2] including distress from being restrained, feeling procedures, and feeling of impending death.
Bottom line: Start appropriate dose sedation promptly after RSI, especially with rocuronium, to avoid short- and long-term distress to patients.
Category: Obstetrics & Gynecology
Posted: 8/11/2025 by Jennifer Wang, MD
(Updated: 2/7/2026)
Click here to contact Jennifer Wang, MD
Pain, bleeding, fever - what symptoms actually mean something when it comes to ovarian torsion?
Well, in this retrospective case-control study looking at 221 patients from 2011 to 2022, Aiob et. al looked at a ton of history, physical exam, and ultrasound findings to see which ones correlated most strongly with ovarian torsion. They found that vomiting and reports of localized pain (v diffuse pain) were highly associated with surgery-confirmed ovarian torsion. In multivariate analysis, localized pain had an odds ratio of 4.36 and vomiting had an odds ratio of 2.38.
Additionally, on ultrasound findings, ovarian edema was much more likely to be present in torsion cases, with an odds ratio of 5.29.
This is a retrospective single center study that comes with all the limitations that these studies always come with, but let this be a reminder of what should trigger your Spidey-senses!
Additional note: We all know that torsion is a diagnosis that can only be confirmed by surgery, no matter what Doppler flow looks like, and this study just adds onto that pile of evidence: Doppler flow was not significantly different between patients who ended up having torsion and those who didn't. >60% of patients who ended up having torsion had normal flow, so like always, remember that a normal Doppler does not exclude torsion in a patient who you're worried about! Talk to OBGYN!
Aiob A, Shushan Marom SB, Gumin D, Lowenstein L, Sharon A. Identifying reliable predictors of ovarian torsion in acute gynecological presentations: A retrospective case-control study. Eur J Obstet Gynecol Reprod Biol. Published online August 6, 2025. doi:10.1016/j.ejogrb.2025.114627
Category: Trauma
Keywords: Gunshot, ptsd, reinjury (PubMed Search)
Posted: 8/10/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This paper outlines the long term effects of surviving a gunshot wound. The authors conclude:
“Firearm injury survivors frequently experience chronic pain, nerve injury, retained bullet fragments that may cause lead toxicity, physical limitations, and PTSD and are at risk for reinjury. In addition to supportive medical and psychiatric care, survivors of firearm injury may benefit from health care–based violence intervention programs.”
Strong BL, Lauerman MH, Scalea TM. Sequelae and Care After Firearm Injury. JAMA. Published online July 23, 2025. doi:10.1001/jama.2025.10498
Category: Orthopedics
Posted: 8/9/2025 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Scaphoid fractures
Make up almost 2/3rds of all carpal fractures
Fractures tend to be localized to 3 anatomic locations
Waist fractures make up 2/3rds. This may be diagnosed with anatomic snuffbox tenderness
Proximal pole fractures make up approximately 25%. This may be diagnosed with bone tenderness about a fingerbreadth distal to Lister’s tubercle
Distal fractures make up the remaining 10%. This may be diagnosed with tenderness at the volar prominence of the distal wrist crease
Imaging:
In addition to standard views of the wrist (PA/lateral/oblique) consider adding a scaphoid view. This imaging view is a PA film taken with the wrist in full pronation and ulnar deviation. This allows full visualization of scaphoid in its longitudinal axis. Also, this allows visualization of the area in question without the annoying overlap of adjacent carpal shadows
Category: Critical Care
Keywords: diarrhea, ICU, mechanically ventilated (PubMed Search)
Posted: 8/4/2025 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
Have you ever wondered what happened to your mechanically ventilated patients who developed diarrhea. Apparently, a multicenter study involving 2650 patients from 44 ICUs in the US, Canada and Saudi Arabia investigated the prevalence of diarrhea among these patients.
This study was the Editor’s choice for June 2025.
Results:
The mean age for the population was 59.8 (16.5) years, with APACHE II Score of 22.0 (7.8). Up to 61% of the patients received vasopressors or inotropes on day 1, which mean these patients are relatively ill.
Up to 60% of patients had diarrhea during their ICU stay, with 15% had diarrhea on day 1 or 2.
Initiating laxatives and antibiotics (who in the ICU would not receive vitamin V and Vitamin Z?) were associated with increased risk of diarrhea: HR for laxatives 1.28 (1.13–1.44), p<0.001; HR for antibiotics 1.41 (1.20–1.67), P< 0.001.
Furthermore, enteral feeding with high/moderate protein concentration was also associated with diarrhea (HR 1.13, 1.00-1.28, P=0.045.
Not surprisingly, diarrhea was associated with higher number of C. Diff testing.
Although patients with diarrhea were associated with longer ICU stay (15 [10-23] days) vs. those without diarrhea (8 [6-12] days), it was not associated with higher mortality (HR 0.70, 95% CI 0.57-0.86, P<0.001)
Discussion:
1. The authors did not report the rates of positive C. Diff. infection in these patients during ICU stay, although they did report that for another study in this population, the rate of positive C. Diff. infection during ICU stay was 2.2%. If only 2.2% had C. Diff. infection while up to 60% had diarrhea. Consequently, for every 30 patients with diarrhea, only one patient had C. Diff. infection. Therefore, do we have to check C. Diff. in those ICU patients with diarrhea every time?
2. The authors hypothesized that patients with diarrhea had longer ICU stay and lower mortality because they survived long enough to develop diarrhea. Thus, diarrhea is bad for clinicians, but may not be too bad for patients?
Conclusion:
Diarrhea is common among invasively ventilated patients. Patients who received laxatives, antibiotics, enteral feeding with high protein amount are at higher risk for diarrhea.
Dionne JC, Johnstone J, Heels-Ansdell D, Tahvildar Khazaneh P, Zytaruk N, Clarke F, Hand L, Millen T, Dechert W, Porteous R, Auld F, Hunt M, Campbell E, Bentall T, Campbell T, Smith O, Rose L, Arabi YM, Duan E, Wilcox ME, McIntyre L, Rochwerg B, Karachi T, Adhikari NK, Charbonney E, St-Arnaud C, Kristof A, Khwaja K, Marquis F, Zarychanski R, Golan E, Cook D; PROSPECT Research Coordinators Group, the PROSPECT Investigators and the Canadian Critical Care Trials Group. Diarrhea in Mechanically Ventilated Patients: A Nested Multicenter Substudy. Crit Care Med. 2025 Jun 1;53(6):e1247-e1256. doi: 10.1097/CCM.0000000000006667. Epub 2025 Apr 3. PMID: 40459385.
Category: Trauma
Keywords: Hypothermia, trauma, mortality (PubMed Search)
Posted: 8/3/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
Looking at a trauma database of over 3 million patients, 1% presented with prehospital hypothermia (<35 degrees C). These patients had longer hospital stays, higher resource utilization and higher mortality. Even isolated head injury patients with hypothermia had worse outcomes. Rewarming did increase survival slightly for all patients.
Take away: rewarm hypothermic trauma patients as soon as possible to improve mortality.
Anna Mary Jose, Aryan Rafieezadeh, Muhammad Zeeshan, Jordan Kirsch, Gabriel Froula, Kartik Prabhakaran, Bardiya Zangbar,
Hypothermia on admission predicts poor outcomes in adult trauma patients,
Injury,
Volume 56, Issue 5,
2025,
112076,
ISSN 0020-1383,
https://doi.org/10.1016/j.injury.2024.112076
Category: Geriatrics
Keywords: Anxiety, older, risk (PubMed Search)
Posted: 8/2/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
A scoping review of the literature regarding anxiety in older patients found the follow areas had the biggest impact on anxiety level:
“The variables most strongly associated with anxiety—either as risk or protective factors—are age, female gender, physical activity, physical health conditions, depression, perceived and family support, and social participation. New variables linked to anxiety include body mass index (BMI) and dietary habits.”
Asking questions related to these areas can give you a better picture of your patient’s risk for anxiety.
Geriatrics 2025, 10(4), 83; https://doi.org/10.3390/geriatrics10040083
Category: Trauma
Keywords: Gun shot, antibiotics, prophylaxis, fracture (PubMed Search)
Posted: 7/31/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
Looking at 140 patients retrospectively who had abdominal gunshot wounds with associated fractures, prophylactic antibiotics longer than three days did not offer any benefit in preventing fracture infection. Only two patients experienced fracture related infections and 65 total experienced any infection related complications.
From and ED standpoint, it appears reasonable to give a dose of antibiotics in this very rare subset of gunshot wound patients.
Kahler D, DeWitte N, Thompson M, Rehman S, Anderson J. Prophylactic antibiotics in gunshot fractures with concomitant bowel injury to prevent fracture-related infections and other infectious complications. Injury. 2025 Jun;56(6):112304. doi: 10.1016/j.injury.2025.112304. Epub 2025 Apr 8. PMID: 40279804.
Category: Geriatrics
Keywords: Geriatric l, trauma, triage (PubMed Search)
Posted: 7/30/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This prospective cohort study from Germany found an under triage rate of 58% of trauma patients over 70 years presenting to 12 trauma centers. One area that consistently lead to undertriage was not using a systolic blood pressure under 110 as a criteria for trauma team activation.
The older cohort had 3 times the mortality than younger, were more likely not to arrive by helicopter and mechanism was more commonly ground level fall. This study echos many others in USA and Australia. Better trauma triage criteria are needed for older patients.
Koch, D.A., Becker, L., Schweigkofler, U. _et al._Undertriage in geriatric trauma: insights from a multicentre cohort study. Scand J Trauma Resusc Emerg Med 33, 123 (2025). https://doi.org/10.1186/s13049-025-01432-0
Category: Critical Care
Posted: 7/29/2025 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
PEEP is often titrated up along with FiO2 to increase oxygen saturation. Although the potential negative hemodynamic effect of high PEEP is often recognized, it is important to also note that high PEEP can also paradoxically worsen oxygen saturation.
The primary physiologic explanation for this phenomenon in a patient with pulmonary disease is due to the varying impact of PEEP on the intra- vs. extra-alveolar blood vessels. PEEP preferentially distends more normal/compliant lung which causes compression of intra-alveolar vessel at excessively high levels of PEEP. This causes pulmonary blood to be diverted to areas of lower vascular resistance (e.g. consolidated lung which is less distended due to its worsened compliance) and lower VQ matching. Essentially, blood flow to normal/healthy lung is decreased and is instead increased to diseased lung, worsening hypoxemia.
Bottom line:
High PEEP can potentially worsen hypoxemia and should be considered as an etiology for worsening oxygen saturation, particularly when the hypoxemia is out of proportion to the patient’s radiographic findings.
Çoruh B, Luks AM. Positive end-expiratory pressure. When more may not be better. Annals ATS. 2014;11(8):1327-1331.
Category: Trauma
Keywords: Bcvi, stroke, CVA (PubMed Search)
Posted: 7/28/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
A retrospective, single Australian center review of 300 patients who had blunt cerebral vascular injuries found:
-9.8% had an inpatient CVA
-Most occurred in first 72 hours
-Those receiving no anti coagulation or antiplatelets had 28% CVA incidence.
-Those treated had a 3.6% CVA incidence (anti platelets were better than anti coagulation)
-Carotid artery injury was less common than vertebral artery but had higher frequency of CVA
-associated factors: low GCS, rib fractures, severe trauma
Take away: non-treatment of blunt cerebral vascular injuries had higher inpatient stroke risk. Antiplatelet agents such as aspirin and Clopidogrel performed better than anticoagulants
Stanislaus V, Zhang WW, Chen Z, et al. Inpatient stroke outcomes in patients with blunt cerebrovascular injuries according to risk factors and treatment. Trauma. 2025;0(0). doi:10.1177/14604086251333569
Category: Trauma
Keywords: Mussed injuries, trauma, tertiary survey, (PubMed Search)
Posted: 7/27/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
This paper looked at the literature regarding missed injuries in trauma patients. Missed injuries was defined as an injury discovered after the patient was discharged. Most of the missed injuries and causes are not novel but are worthy of remembering.
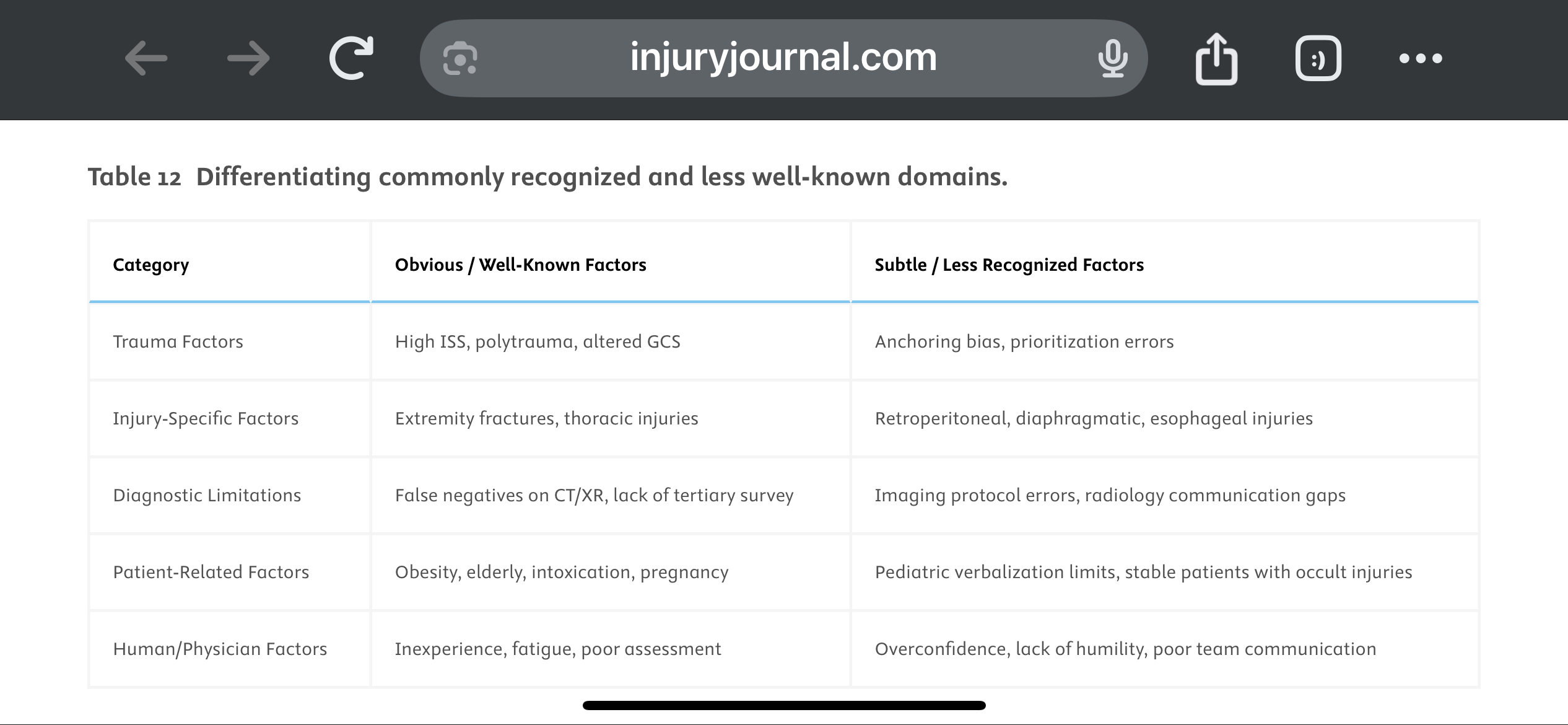
They suggest a Trauma Tertiary Survey helps prevent missed injury. “Tertiary Survey (TTS), which includes a thorough in-hospital re-examination and a review of diagnostic investigations within the first 24 h, has been shown to significantly reduce the occurrence of missed injuries (1–9 %) in severe trauma patients found after a primary and secondary survey.” This concept is similar to a discharge time out in emergency medicine where all data is reviewed, viral signals are confirmed normal and a team discharge is performed.
The paper offers these suggestions to avoid missed injuries:
1.
Standardize Tertiary Trauma Surveys (TTS).
2.
Be Cognizant of Cognitive Biases (e.g., Anchoring Bias).
3.
Repeat Imaging When Clinically Indicated.
4.
Use Protocolized Imaging Techniques (CT/MRI).
5.
Ensure Radiology-Trauma Communication.
6.
Prioritize High-Risk Populations.
7.
Implement Peer Review or Double-Check Systems.
8.
Encourage a Culture of Collaboration and Humility.
9.
Limit Provider Fatigue and Overload.
10.
Create Tailored Checklists for Subtle Injuries.
Vieira, Lucas Fontenelle et al.
Injury, Volume 56, Issue 8, 112600
Category: Orthopedics
Posted: 7/27/2025 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
A recent study investigated the impact of pain management education counseling on postoperative opioid consumption.
Patients were randomly assigned to receive opioid limiting perioperative pain management education and counseling (intervention group) with instructions to take opioids “only as a last resort if the pain became unbearable.”
The control group received instructions to take opioids as needed for “severe pain” to” stay ahead of the pain.”
The primary outcome was the total morphine equivalents (TME) consumed in the 3 months after surgery.
Secondary outcomes included pain measured with the Numeric Rating Scale, sleep quality, opioid prescription refills, and patient satisfaction.
121 patients with a mean age of 29 years.
Both groups were told about potential adverse effects of opioids and were advised of alternative methods to control pain such as over-the-counter acetaminophen and ibuprofen.
60 patients in the treatment group consumed a mean of 46 mg TME versus 63.6 mg TME in the control group ( p < 0.001). There was no difference in the average score on the numeric rating scale in the first 14 days between groups. There was no significant difference in refill prescriptions between the groups. Sleep quality and patient satisfaction was also similar between groups.
Over 1/3 of patients in the intervention group took no opioids at all after surgery. In contrast, 9 out of 10 patients in the control group used all prescribed opioids after surgery.
Conclusion: Opioid limiting pain management education and counseling reduces opioid consumption without a change in reported pain. There may be a role for pain management education and counseling in emergency department patients in whom opiates are prescribed…similar to this study in perioperative orthopedic patients.
Packer, Jonathan D. MD1,a; Aneizi, Ali MD1; Honig, Evan L. BS1; Kaveeshwar, Samir MD1; Schneider, Matheus MD1; Leong, Natalie L. MD1; Meredith, Sean J. MD1; O’Hara, Nathan N. PhD, MHA1; Henn, R. Frank III MD1. Perioperative Opioid Counseling for Patients Undergoing Anterior Cruciate Ligament Reconstruction: A Randomized Controlled Trial. The Journal of Bone and Joint Surgery 107(14):p 1546-1552, July 16, 2025
