Category: Administration
Keywords: Communication, Teamwork (PubMed Search)
Posted: 1/28/2026 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
How well does your ED care team communicate? For some high yield strategies and reasons for improvement, read on…
To explore effective and ineffective communication in the ED and its impact of patient care, physician and nurses from several academic EDs completed an online anonymous survey, then attended focus group sessions. Responses highlighted the following themes:
1: Situations, built physical environment, and medium of communications all impact quality of communication.
2: Core elements of desired professional communication include respect, closed-loop communication, and attention, often conveyed through non-verbal behaviors.
3: Poor communication begets poor communication in later interactions
4: Effective communication is seen as fundamental to patient care but also has impacts beyond patient care
5: Clinician gender and gender dyads influence communication dynamics, age and experience dyads did not.
Do any of these themes resonate with you? What can you do within your department to improve physician-nurse communication and the care you provide?
Jones DC, Phillips J, Graveson A, et al. Emergency Physician and Emergency Nurse Communication in the Emergency Department: A Mixed-methods Study. West J Emerg Med. 2026;27(1)91–98.
Category: Administration
Keywords: artificial intelligence, emergency department, emergency practice, machine learning (PubMed Search)
Posted: 11/26/2025 by Mercedes Torres, MD
(Updated: 2/8/2026)
Click here to contact Mercedes Torres, MD
Food for thought on this Thanksgiving eve…
AI is rapidly being integrated into the practice of emergency medicine, as well as many other medical specialties. Similar to the adage, "you are what you eat," AI is what we feed it. See below for an introduction to the various levels of bias contributing to the machine learning process:
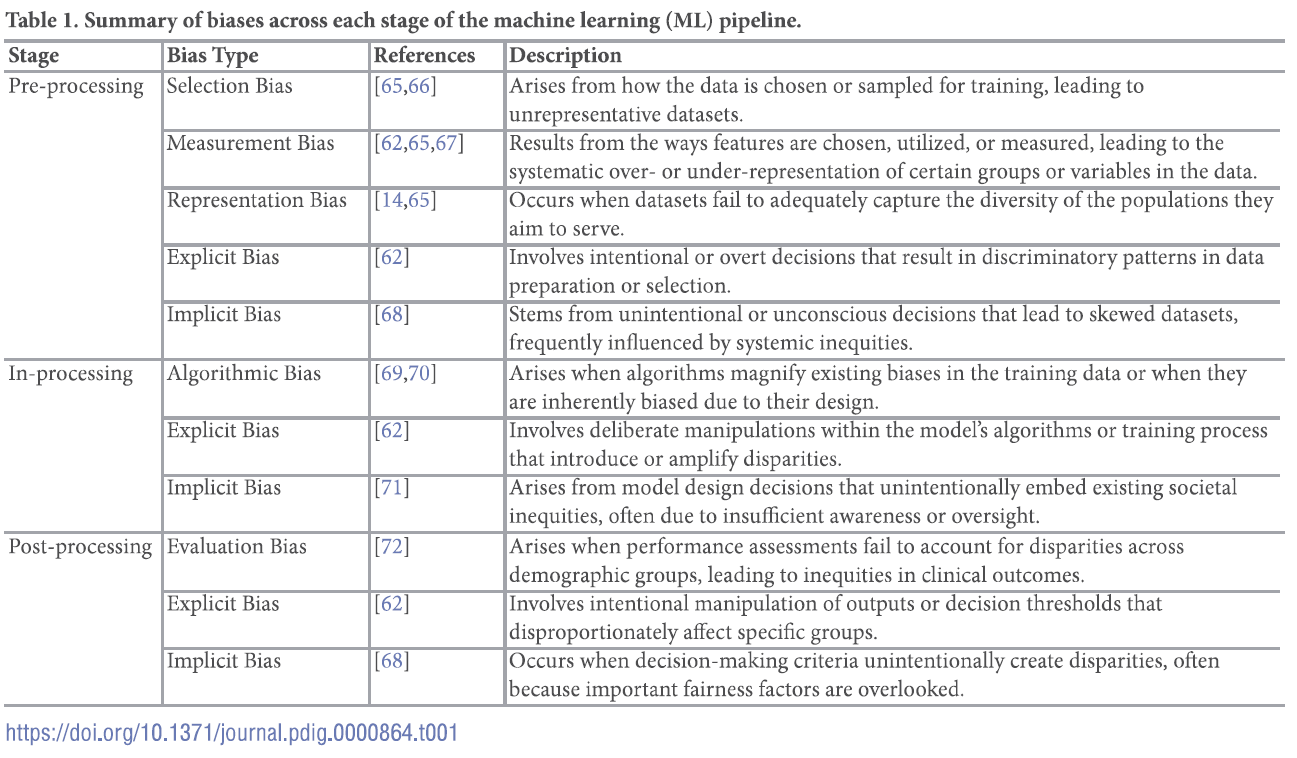
For a deep dive into the world of bias in AI, see referenced article.
Chinta SV, Wang Z, Palikhe A, Zhang X Kashif A, Smith MA, et al. (2025) AI-driven healthcare: A review on ensuring fairness and mitigating bias. PLOS Digit Health 4(5): e0000864. https://doi.org/10.1371/journal.pdig.0000864
Category: Administration
Keywords: Operations, Disposition, Decision-Making, Disparities, (PubMed Search)
Posted: 9/24/2025 by Mercedes Torres, MD
(Updated: 2/8/2026)
Click here to contact Mercedes Torres, MD
This publication is a retrospective cross-sectional study conducted based on data collected during January 1–December 31, 2019 from a large, academic ED in the Southeastern US with the following research questions and results:
Interesting point regarding how disposition decisions are different from the ample evidence on disparities within triage decisions: The presence of disparities in disposition decisions is noteworthy not only because of their potentially long-term effects on patients’ health, but also because unlike some of the other decisions made in the ED such as triage, they are typically made under relatively less time pressure with deliberation and input from multiple individuals, conditions that are known to make biases less likely.
Authors propose pursing further research to elucidate the factors that contribute to these findings, instituting systems to alert providers in real time to the presence of conditions that could exacerbate disparities in ED care, and including the measurement of disparities along sex, race and ethnicity into health care operations data.
Cheng Q, Argon NT, Evans CS, Lin P, Linthicum B, Liu Y, Mehrotra A, Patel MD and Ziya S (2024) An Investigation into Demographic Disparities in Emergency Department Disposition Decisions. Production and Operations Management 34(4): 688–696.
Category: Administration
Keywords: Patient Experience, Patient Satisfaction, CMS Evaluation, ED Evaluation, (PubMed Search)
Posted: 7/22/2025 by Mercedes Torres, MD
(Updated: 7/23/2025)
Click here to contact Mercedes Torres, MD
Shout out to UMEM alum Diane Kuhn, MD, PhD as the first author of this recent publication…
She and her colleagues examined the factors that contribute to ED patient experience scores, uncovering several which are not considered in the current CMS evaluative framework. See the editor's (our very own Stephen Schenkel, MD, MPP) capsule summary below:
What is already known on this topic? Medicare plans nationally standardized Emergency Department (ED) Patient Experience scores (ED
CAHPS) to allow comparison across sites.
What question this study addressed. Are there clinical and operational ED characteristics for which ED patient experience scores ought to be adjusted?
What this study adds to our knowledge. Based on 58,622 ED visits from one system, patients arriving in pain were less satisfied and those receiving radiologic studies had a positive experience.
How this is relevant to clinical practice. Influences on patient satisfaction are multifactorial and many are outside the control of the ED. Comparing EDs based on patient experience is complex and prone to misinterpretation.
As the authors point out, If patients placed in a hallway bed have a more negative experience simply due to the location in the department, or patients arriving in pain have a more negative experience regardless of ED care, then some EDs will face more challenges than others in achieving optimal patient experiences.
The current CMS evaluative framework may inherently disadvantage certain EDs, including those with limited physical space relative to their patient volumes, such as safety-net hospitals, or those that care for a high proportion of patients experiencing chronic pain. Is this fair? Does it reflect what CMS is trying to evaluate? Are there alternatives?
Kudos to Dr. Kuhn on her insightful publication and Dr. Schenkel for his expert editing!
Kuhn, Diane et al. Use of Hallway Beds, Radiology Studies, and Patients in Pain on Arrival to the Emergency Department Are Associated With Patient Experience, Annals of Emergency Medicine, Volume 86, Issue 2, 150 - 157. https://doi.org/10.1016/j.annemergmed.2024.11.020
Category: Administration
Keywords: Artificial intelligence, Emergency department, emergency practice (PubMed Search)
Posted: 5/27/2025 by Mercedes Torres, MD
(Updated: 5/28/2025)
Click here to contact Mercedes Torres, MD
AI is probably already being used in your ED, like it or not…
This article is an excellent review of the ways that AI can be used in emergency medicine. (See blue boxes in the figure below for a visual representation of opportunities for AI to augment emergency care from start to finish.) The authors note that there will always be a role for human physicians in EDs; AI can serve as an adjunct rather than a replacement for physician care. Physicians should strive to be informed leaders in AI development to ensure it is performed in a cautious, thoughtful, patient-centered manner.
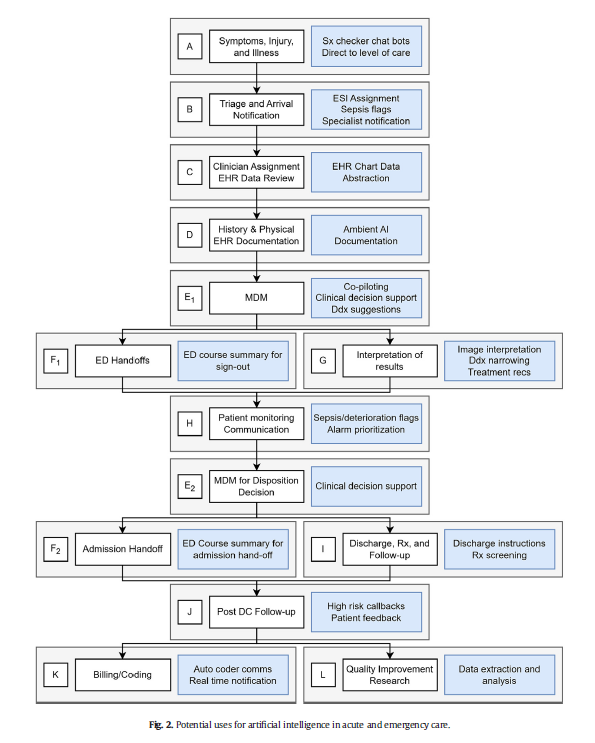
Marika M. Kachman, Irina Brennan, Jonathan J. Oskvarek, Tayab Waseem, Jesse M. Pines. How artificial intelligence could transform emergency care. The American Journal of Emergency Medicine, Volume 81, 2024, Pages 40-46, https://doi.org/10.1016/j.ajem.2024.04.024.
Category: Administration
Keywords: Team building, belonging, team dynamics, emergency physicians, emergency nurses (PubMed Search)
Posted: 3/25/2025 by Mercedes Torres, MD
(Updated: 3/26/2025)
Click here to contact Mercedes Torres, MD
Better teamwork creates better outcomes in emergency medicine. This study investigated how communication practices between physicians and nurses in the ED influence team dynamics and the sense of belonging to the healthcare team.
Methods: 38 emergency physicians and emergency nurses from EDs within a single metropolitan area participated in focus groups.
Positive Influences on Team Belonging:
Negative Influences on Team Belonging:
The findings emphasize the importance of fostering positive communication practices to enhance team dynamics, cohesiveness, and overall well-being within ED healthcare teams.
Phillips J, Jones D. Qualitative Study of Dynamics, Camaraderie, and Belonging Among Emergency Physicians and Nurses. J Emerg Med. 202569doi:10.1016/j.jemermed.2024.08.011
Category: Administration
Keywords: Burnout, Wellbeing, Workforce (PubMed Search)
Posted: 1/22/2025 by Mercedes Torres, MD
(Updated: 2/8/2026)
Click here to contact Mercedes Torres, MD
On March 18, 2022, Congress passed the Dr. Lorna Breen Health Care Provider Protection Act, named after an emergency medicine physician who died by suicide during the pandemic. This landmark legislation allocated $103 million across 45 organizations to introduce evidence-based measures to mitigate and prevent burnout.
As a result, the Impact Wellbeing Guide was developed, outlining the six key evidence-based action steps for organization leaders to address health care workers’ professional well-being listed below:
The Guide is designed to help hospital leaders and executives accelerate or supplement professional wellbeing work in their hospitals at the operational level.
A PDF of the full guide is available from the CDC: https://www.cdc.gov/niosh/docs/2024-109/
https://www.cdc.gov/niosh/healthcare/impactwellbeingguide/
Bock A. To Fix Burnout, New Initiatives Go Beyond Worker Resilience and Put Onus on Health Systems. JAMA. 2024;331(24):2067–2069. doi:10.1001/jama.2024.6216
Category: Administration
Keywords: artificial intelligence, emergency department, emergency practice, machine learning (PubMed Search)
Posted: 11/27/2024 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
Gooble, gooble,… gulp, some food for thought on the eve of Thanksgiving.
The development of artificial intelligence (AI) in emergency medicine is well under way. The schematic below and accompanying reference presents the anticipated stages in the process of AI development, including important features, considerations, and challenges as we move towards increased integration of AI in our practice of EM.
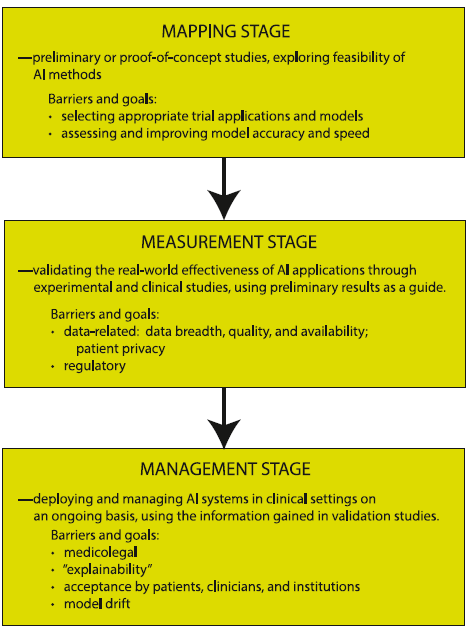
Petrella, R. The AI Future of Emergency Medicine. Ann Emerg Med. 2024;84:139-153. https://doi.org/10.1016/j.annemergmed.2024.01.031
Category: Administration
Keywords: design, workspace, handoff, interruptions, collaboration (PubMed Search)
Posted: 9/21/2024 by Mercedes Torres, MD
(Updated: 9/25/2024)
Click here to contact Mercedes Torres, MD
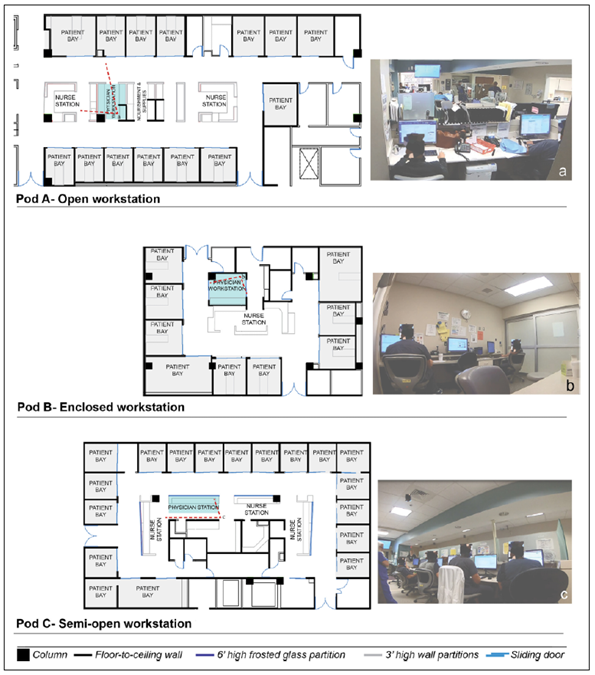
Joshi R, Joseph A, Ossmann M, et al. Emergency Physicians’ Workstation Design: An Observational Study of Interruptions and Perception of Collaboration During Shift-End Handoffs. HERD: Health Environments Research & Design Journal. 2021;14(4):174-193. doi:10.1177/19375867211001379
Category: Infectious Disease
Keywords: Mpox, monkeypox, outbreak, democratic republic of congo (PubMed Search)
Posted: 8/25/2024 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
Background:
What’s new?
Who is at risk?
Patients with epidemiologic characteristics and lesions or other signs and symptoms consistent with mpox. This includes anyone with travel to DRC or any of its neighboring countries (ROC, CAR, Rwanda, Burundi, Uganda, Zambia, Angola, Tanzania, and South Sudan) in the previous 21 days.
What to look for?
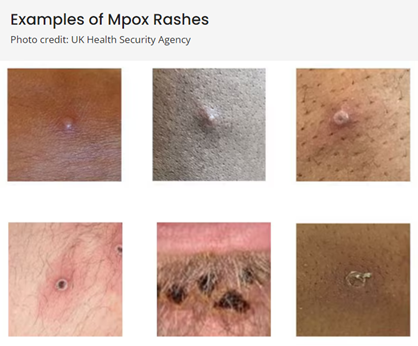
(Above photos from https://www.cdc.gov/poxvirus/mpox/clinicians/clinical-recognition.html)
What to do?
If mpox is suspected in a patient:
Duwell M. Mpox Clinician Letter. Maryland Department of Health. August 19, 2024.
Mpox Caused by Human-to-Human Transmission of Monkeypox Virus in the Democratic Republic of the Congo with Spread to Neighboring Countries. US Centers for Disease Control and Prevention. CDC Health Alert Network, August 7, 2024, 3:15 PM ET, Accessed at https://emergency.cdc.gov/han/2024/han00513.asp# on August 25, 2024.
Mpox. US Centers for Disease Control and Prevention. https://www.cdc.gov/poxvirus/mpox/index.html, Accessed on August 25, 2024.
Category: Administration
Keywords: Administration, Meetings, Workforce satisfaction (PubMed Search)
Posted: 7/24/2024 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
Participation in meetings is an expected part of most (if not all) of our jobs. How many of these meetings are necessary? Could some of the “work” of meetings be accomplished with a few emails or other asynchronous forms of communication? Are meetings cluttering your schedule and making it impossible to get any real work done?
Some answers to these questions are offered in a Harvard Business Review article from March 2022.
Key points include:
Advantages to fewer meetings:
Authors recommend holding meetings only when “absolutely” necessary. That typically includes:
Laker B, Pereira V, Malik A, and Soga L. Meeting Management: Dear Manager, You’re Holding Too Many Meetings. Harvard Business Review. March 9, 2022.
Category: Administration
Keywords: Specialty ED, Geriatric ED, Oncologic ED (PubMed Search)
Posted: 5/21/2024 by Mercedes Torres, MD
(Updated: 5/22/2024)
Click here to contact Mercedes Torres, MD
There is a growing trend toward the development of specialty-specific emergency services, such as Geriatric or Oncologic EDs.
Will this trend continue? Is the segmentation of emergency care in our future? The author of this article opines that the answer depends on future outcomes research in this area.
Brouillette M. Are Specialty Emergency Departments the Future of Emergency Care? Oncology- and Geriatric-Focused Emergency Departments Hope to Improve Care, Lower Costs. Annals of Emergency Medicine. May 2024, 83(5):9A-12A. https://doi.org/10.1016/j.annemergmed.2024.03.015
Category: Administration
Keywords: Administration, Patient Experience, Microaggression, Discrimination (PubMed Search)
Posted: 3/27/2024 by Mercedes Torres, MD
(Updated: 2/8/2026)
Click here to contact Mercedes Torres, MD
Do microaggressions and discrimination impact the patient experience in your ED? How can we address this?
This article is one of few studies to address this topic specifically in the ED. Authors used quantitative (discrimination scale) and qualitative (follow-up interviews) methods to answer this question in two urban academic EDs.
Common themes from patient responses provide food for thought and action in this regard:
Punches BE, Osuji E, Bischof JJ, et al. Patient perceptions of microaggressions and discrimination toward patients during emergency department care. Acad Emerg Med. 2023; 30: 1192-1200. doi:10.1111/acem.14767
Category: Administration
Keywords: boarding, administration, crowding (PubMed Search)
Posted: 11/22/2023 by Mercedes Torres, MD
(Updated: 2/8/2026)
Click here to contact Mercedes Torres, MD
A recently published study of ED APPs, residents, attendings, and nurses attempted to assess clinician's perspectives on how ED boarding impacts ED staff and patients. Authors performed a survey followed by focus group sessions to obtain qualitative insignts from participants.
All respondents associated boarding with feelings of burnout and self-reported poor satisfaction with communication and the process of boarding care.
Several key themes emerged which are outlined below:
This publication highlights the negative workforce and patient safety effects of ED boarding. It amplifies the voices of our colleagues who work towards change to improve both the health of our wrokforce as well as that of our patients and the communities that we serve.
Loke D, et al. Clinicians’ Insights on Emergency Department Boarding: An Explanatory Mixed Methods Study Evaluating Patient Care and Clinician Well-Being. The Joint Commission Journal on Quality and Patient Safety 2023; 000:1-8.
Category: Administration
Keywords: Workforce, Diversity, Under-represented minorities (PubMed Search)
Posted: 9/27/2023 by Mercedes Torres, MD
(Updated: 2/8/2026)
Click here to contact Mercedes Torres, MD
Physician Workforce Diversity in EM
Health inequities along racial, ethnic, and socioeconomic lines are a brutal reality of the current state of health care in the US. One way to attempt to address these inequities is to make a concerted effort to diversify our physician workforce. As authors have noted, “Having physicians from diverse backgrounds as colleagues and role models can promote understanding and tolerance in nonminority physicians, ultimately improving medical care for patients who are part of these racial and ethnic groups. Increasing the population of underrepresented minority (URM) physicians in the workforce also directly improves health care for medically underserved populations from all racial and ethnic backgrounds, as studies have shown that physicians from URM backgrounds are more likely to work with these patients.”
Administrators are often tasked with the difficult job of creating a cohesive group of emergency physicians to meet the needs of the community they serve. Strategies to diversify that workforce would benefit from a multi-level approach, including the following:
Small steps can create big changes.
Category: Administration
Keywords: age, attrition, gender, workforce (PubMed Search)
Posted: 7/26/2023 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
In a recent study of emergency physicians (EPs) who left the workforce between 2013 and 2020, authors sought to investigate their age and number of years since residency graduation for males and females.
A total of 25,839 (70.2%) male and 10,954 (29.8%) female EPs were included.
Female gender (adjusted odds ratio 2.30) was significantly associated with attrition from the workforce.
Of those who left the workforce, the median number of years after residency that males left was 17.5, as compared with only 10.5 years for females.
Furthermore, among those who exhibited attrition, one in 13 males and one in 10 females exited clinical practice within 5 years of residency graduation.
As authors emphasize, these data identify widespread gender-based disparities regarding EM workforce attrition that are critical to address to ensure stability, longevity, and diversity in the EP workforce.
Gettel CJ, Courtney DM, Agrawal P, et al. Emergency medicine physician workforce attrition
differences by age and gender. Acad Emerg Med. 2023;00:1- 9. doi:10.1111/acem.14764
Category: Administration
Keywords: patient experience, clinician wellbeing (PubMed Search)
Posted: 5/24/2023 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
Clinician Well-Being and the Patient Experience
Did you know that most patient experience responses are overwhelmingly positive? Rather than focusing all our attention on the bad, let’s focus on the good to promote clinician well-being. See below for a few key points from a recent study on this:
Consider emphasizing positive patient experiences when providing feedback to emergency physicians. It will promote clinician well-being and help improve performance in your practice.
Dudley J and Lee TH. Patient Experience and Clinician Well-Being Aren’t Mutually Exclusive. Harvard Business Review. Published online at hbr.org, July 18, 2022.
