Category: Cardiology
Keywords: Hypertension, treatment, (PubMed Search)
Posted: 9/6/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
From this position statement on management of HTN key points are beta blockers are a second line medication choice, dual therapy in a combination pill is often warranted and primary medications should be thiazides, long acting calcium channel blockers, ACE or Arbs.
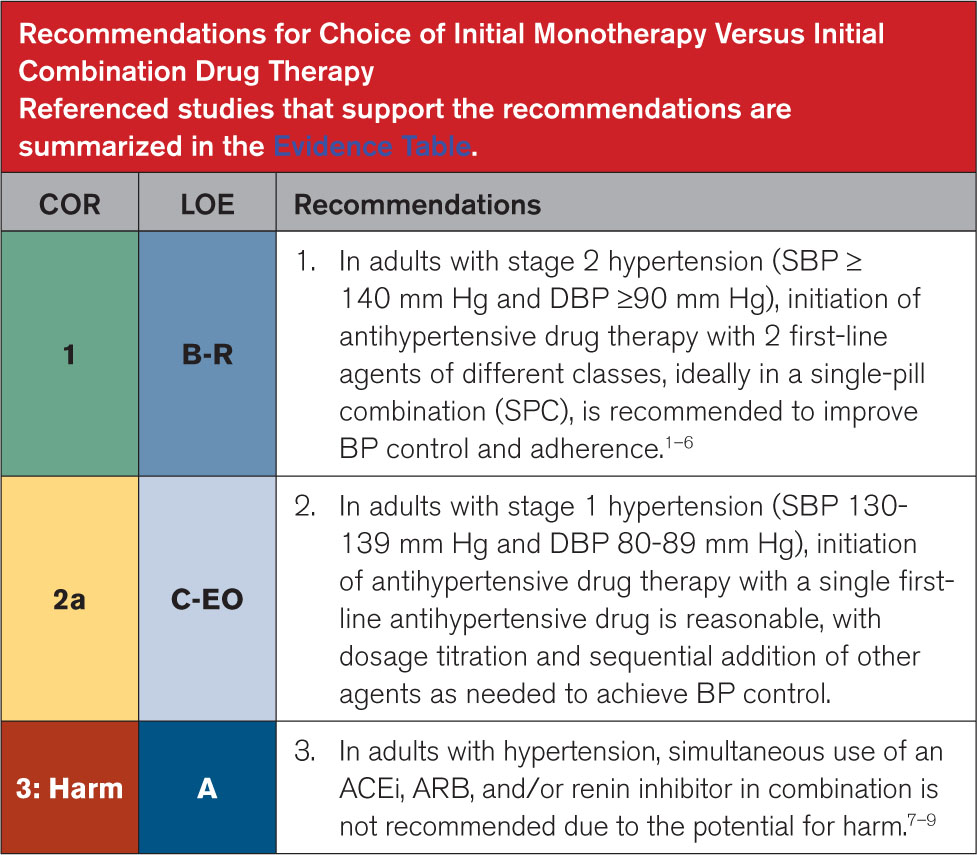
Circulation August 14,2025 https://doi.org/10.1161/CIR.0000000000001356
Category: Cardiology
Keywords: aorta, dissection (PubMed Search)
Posted: 5/3/2025 by Robert Flint, MD
(Updated: 5/4/2025)
Click here to contact Robert Flint, MD
Aortic dissection remains a difficult diagnosis to make. This article is a nice review. The pathology behind this involves an intimal flap in the aortic wall. Death occurs due to aortic rupture or obstruction of branching artery.
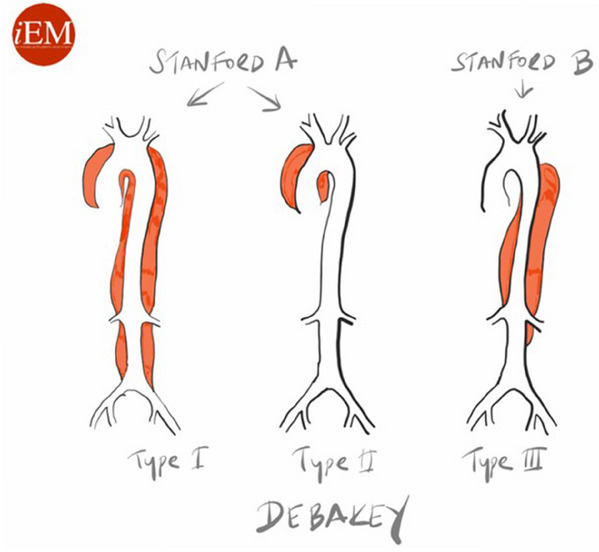
Risk factors: male 2:1 female, Marfan Syndrome, HTN, aortic aneurysm, cocaine and methamphetamine use, pregnancy
Pain is variable however tearing, ripping migrating, maximum at onset, and sharp are all associated with Aortic Dissection. Think about Dissection with atypical CP with ECG changes as well as in stroke like presentations along with chest pain.
Gold standard for diagnosis is CT angiogram. Decision rules with the use of D-Dimer have been proposed however there is still not sufficient evidence to use these. ACEP guidelines currently give use of decision rules a long with DDImer a level C recommendation.
Briggs, Blake et al.
JACEP Open, Volume 5, Issue 4, e13225
Category: Cardiology
Keywords: Brugada, ECG, hyperkalemia (PubMed Search)
Posted: 4/26/2025 by Visiting Speaker
(Updated: 2/7/2026)
Click here to contact Visiting Speaker
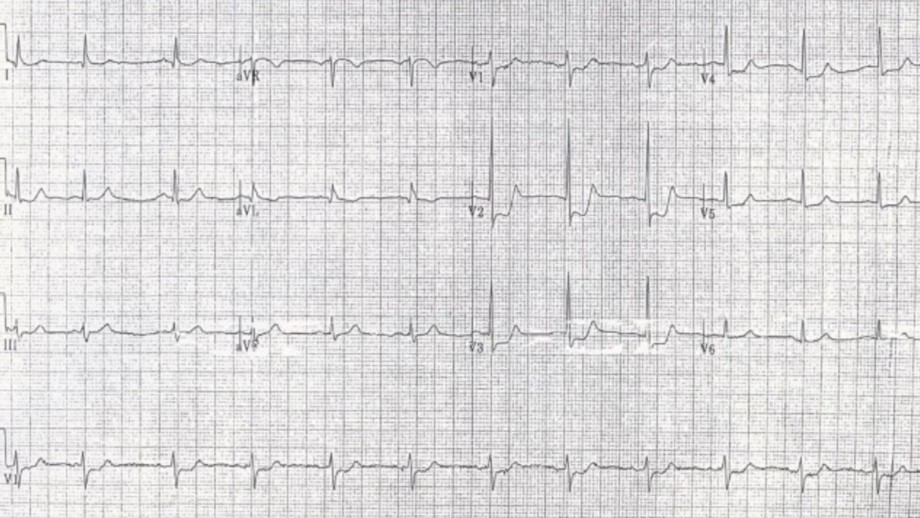
Pseudo-Brugada pattern in hyperkalemia
Category: ECG
By: Chuck Siegel
Keywords: Brugada sign, hyperkalemia, ECG, arrhythmia
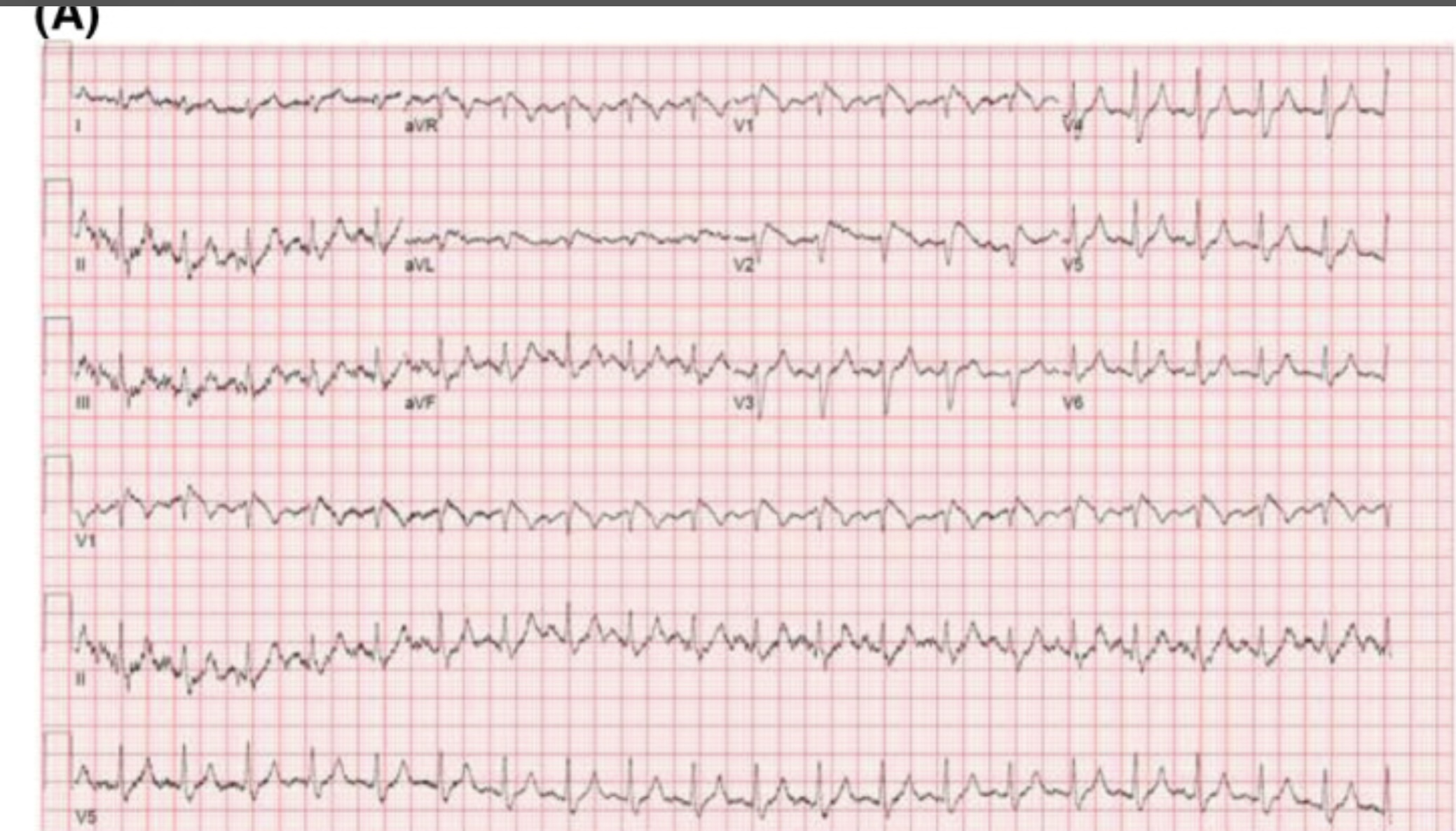
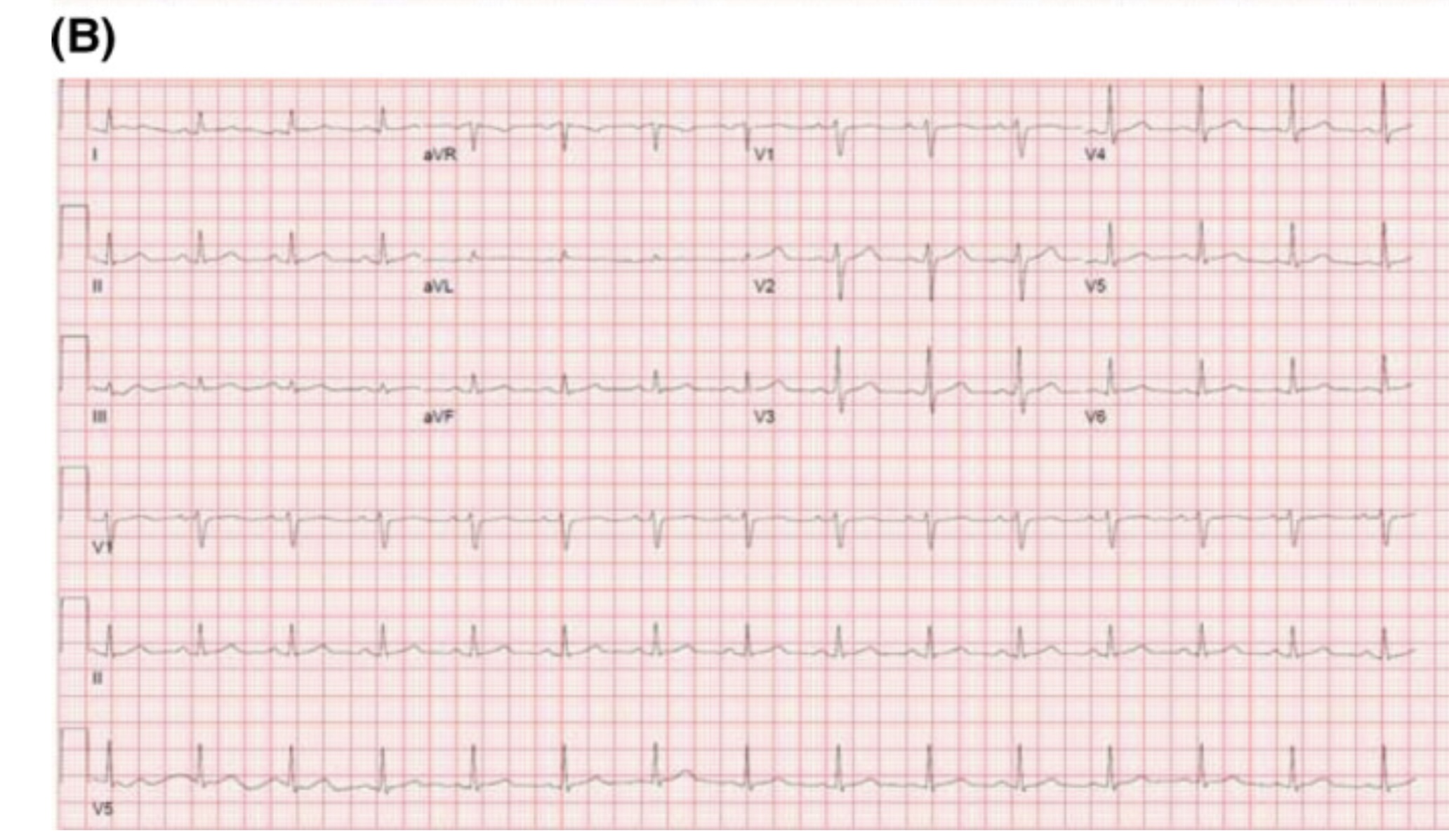
Hyperkalemia can produce a variety of ECG changes, including well-known changes such as peaked t-waves, QRS widening, PR-interval prolongation, loss of the p-waves, and the sine wave morphology. One change not as commonly seen is coved ST-elevation in V1-V3 that mimics the ECG changes associated with Brugada sign. Unlike Brugada syndrome, these ECG changes are transient and resolve upon treatment of the hyperkalemia.
The mechanism of these ECG findings relate to the elevated extracellular potassium’s inactivating effect on sodium channels, similar to the sodium channelopathy found in Brugada syndrome. The mean serum potassium concentration of reported cases is often above 6.5 mEq/L. Importantly, hyperkalemia-induced Brugada pattern has not been associated with sudden cardiac death or ventricular arrhythmias.
An example of a hyperkalemia-induced pseudo Brugada pattern in a patient with a K of 7.2 mEq/L (A) as well as that same patient’s ECG following treatment of their hyperkalemia (B).
References
Manne JRR, Garg J. Hyperkalemia induced Brugada phenocopy. J Arrhythm. 2021 Jan 7;37(1):249-250. doi: 10.1002/joa3.12498. PMID: 33664911; PMCID: PMC7896447.
Alnajjar AZ, Ibrahim AI, Ellebedy M. Hyperkalemia-induced Brugada phenocopy: a systematic review of case reports. Clin Res Cardiol. 2025 Feb 18. doi: 10.1007/s00392-025-02607-6. Epub ahead of print. PMID: 39964614.
Xu G, Gottschalk BH, Anselm DD, Benditt DG, Maheshwari A, Sreenivasan S, Shama RA, Dendramis G, Barajas-Martínez H, Rubio Campal JM, Aznaurov SG, Baranchuk A. Relation of the Brugada Phenocopy to Hyperkalemia (from the International Registry on Brugada Phenocopy). Am J Cardiol. 2018 Mar 15;121(6):715-717. doi: 10.1016/j.amjcard.2017.12.008. Epub 2017 Dec 29. PMID: 29397883.
Rivera-Juárez A, Hernández-Romero I, Puertas C, Zhang-Wang S, Sánchez-Álamo B, Martins R, Figuera C, Guillem MS, Climent AM, Fernández-Avilés F, Tejedor A, Jalife J, Atienza F. Clinical Characteristics and Electrophysiological Mechanisms Underlying Brugada ECG in Patients With Severe Hyperkalemia. J Am Heart Assoc. 2019 Feb 5;8(3):e010115. doi: 10.1161/JAHA.118.010115. PMID: 30675825; PMCID: PMC6405573.
Category: Cardiology
Keywords: Hypertension, as needed, acute kidney injury (PubMed Search)
Posted: 2/9/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
A retrospective look at veterans who received oral and/or IV as needed blood pressure medications while hospitalized in a non-ICU setting found an association with as needed meds and acute kidney injury, greater than 25% blood pressure drop in 3 hours, and death, stroke and MI while hospitalized. IV medications had a higher association.
While needing prospective validation, this appears to be more evidence to treat the patient not the number.
Canales MT, Yang S, Westanmo A, Wang X, Hadley D, Ishani A, Mohandas R, Shorr R, Lo-Ciganic W. As-Needed Blood Pressure Medication and Adverse Outcomes in VA Hospitals. JAMA Intern Med. 2025 Jan 1;185(1):52-60. doi: 10.1001/jamainternmed.2024.6213. PMID: 39585709; PMCID: PMC11589853.
Category: Cardiology
Keywords: Hypertension, MACE, end organ (PubMed Search)
Posted: 1/4/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This study followed patients presenting to the ED with elevated (SBP>180, DBP>120) blood pressure without evidence of end organ dysfunction for one year. The patients were followed for major adverse cardiac events. They found:
“A total of 12,044 patients were enrolled. The prevalence of MACE within one year was 1,865 (15.5%). Older age, male gender, history of cardiovascular disease, cerebrovascular disease, diabetes, smoking, presentation with chest pain, altered mental status, dyspnea, treatment with intravenous and oral hydralazine, and oral metoprolol were independent predictors for one-year MACE. Additionally, discharge with an SBP ?160 mm Hg was not associated with 30-day MACE-free survival after propensity matching (hazard ratio 0.99, 95% confidence interval 0.78–1.25, P?=?0.92).”
Treating to reach a magic number did not help. Most likely, long term control of blood pressure is a more important factor than attempts to lower in the ED. While this is a high risk group, there is no evidence that acute lowering of blood pressure impacts long term survival.
Category: Cardiology
Posted: 12/14/2024 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Cardiovascular disease (CVD) is the leading cause of death both in the United States and globally for both men and women.
Major adverse cardiovascular events (MACE) is a commonly used composite outcome.
MACE is defined as non-fatal stroke/acute myocardial infarction/heart failure or cardiovascular death.
Physical inactivity is a leading risk factor for noncommunicable diseases and death worldwide
Up to 5 million deaths/yr could be averted with increased physical activity
Regular physical activity reduces the risk of many types of cancer by 8-28%, diabetes by 17%, heart disease and CVA by 19%, and dementia by 20%.
Many adults and children find meeting the recommended physical activity goals very challenging.
A recent observational study found that just 1.5-to-4-minute small bursts of high intensity exercise throughout the day may help lower an individual’s risk of MACE.
To clarify, this does not mean going to the gym to do a 45-minute HIIT class
Vigorous intermittent lifestyle physical activity (VILPA) involves such simple things as carrying the groceries a short distance or taking the work stairs instead of the elevator.
Such activities are more feasible for all of us vs structured exercise for obvious reasons.
Study group was >100,000 middle-aged men and women. Average age 61.
All participants wore an activity tracker continuously for a full week.
This data was used to calculate VILPA bouts throughout the day.
Female participants with no formal exercise regimen who recorded just 3.4 minutes of VILPA a day were 50% less likely to have a MI, had a 67% decreased risk for heart failure and 45% less likely to develop any type of MACE vs those who did not clock any VILPA during their day.
Female participants who recorded just 1.2-1.6 minutes of VILPA a day had a 33% lower risk of MI, 40% decreased risk of heart failure and 30% lower risk of MACE.
In male participants, those with 5.6 minutes of VILPA each day had a 16% reduced risk of having MACE than those who did not have any VILPA.
Differences may be due to women’s VILPA intensity was roughly 20% greater than men
Conclusion: Take the stairs
Stamatakis E, et al. Device-measured vigorous intermittent lifestyle physical activity (VILPA) and major adverse cardiovascular events: evidence of sex differences. Br J Sports Med. 2024 Oct 28
Category: Cardiology
Keywords: Aaa (PubMed Search)
Posted: 12/7/2024 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This study tried to expand upon what they describe as the classic triad of signs to diagnose ruptured AAA “(1) abdominal pain, (2) hypotension and (3) a pulsatile abdominal mass”. They tested these against the _modified abdominal aortic aneurysm rupture signs. “_The MARS-signs encompassed (1) the registered pain-associated symptoms or signs, (2) all hypovolemic associated signs, and (3) pulsatile abdominal mass and/or ultrasound finding”. The MARS did slightly better in identifying ruptured AAA retrospectively. For me, this doesn’t add a great deal of help in making this can’t miss diagnosis and further work is necessary.
Bergmark, P., Sadeghi, M., Talvitie, M. _et al._Initial signs in patients with ruptured abdominal aortic aneurysms: time for an expanded triad?.Scand J Trauma Resusc Emerg Med 32, 94 (2024). https://doi.org/10.1186/s13049-024-01268-0
Category: Cardiology
Keywords: Hypertension, emergency, asymptomatic (PubMed Search)
Posted: 10/30/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
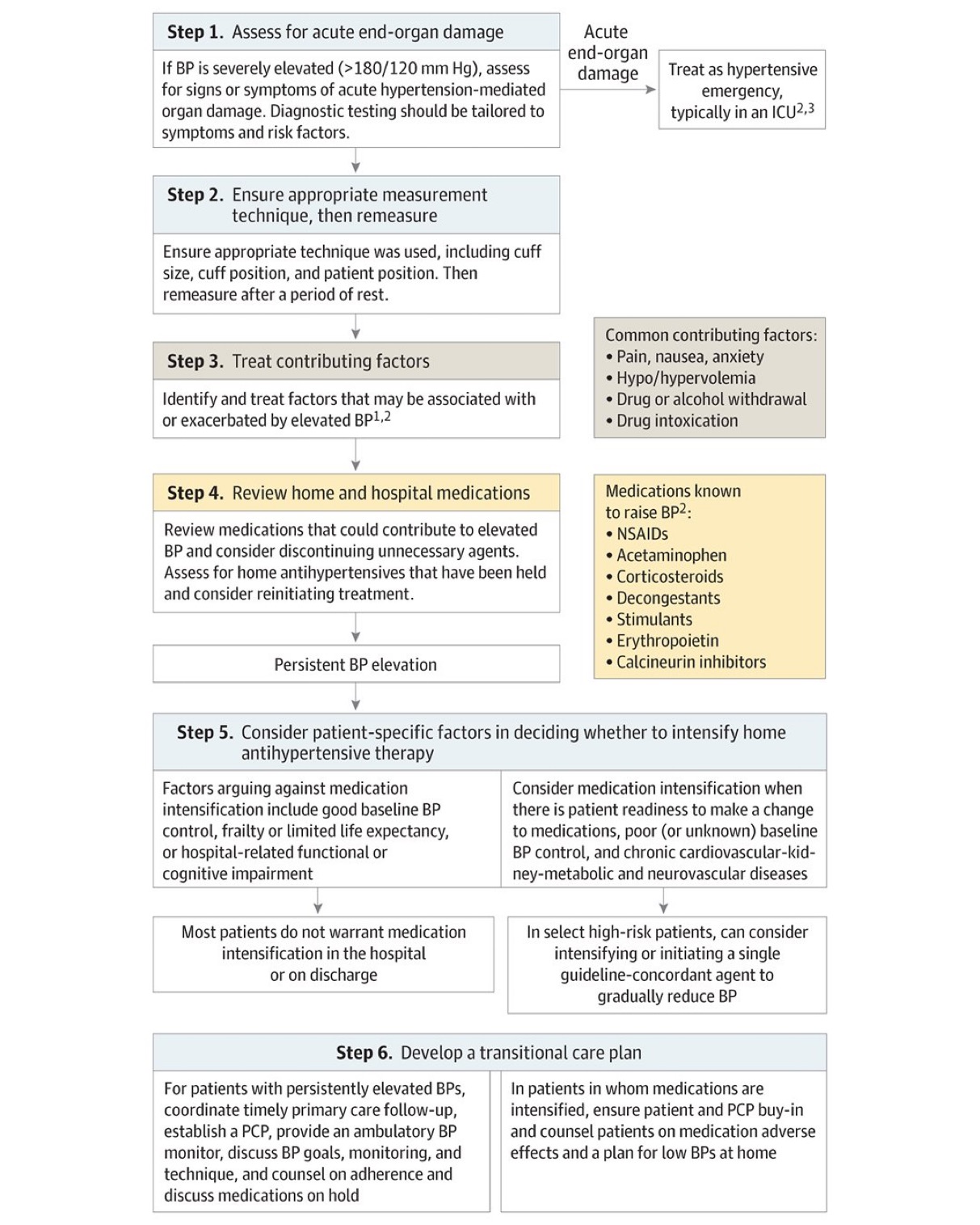
Hypertension in the ED comes in two varieties: emergency and asymptomatic (not urgency!). From this position statement: “Hypertensive emergency involves acute target-organ damage and should be treated swiftly, usually with intravenous antihypertensive medications, in a closely monitored setting.”
Conversely, asymptomatic does not require urgent, aggressive management. “Recent observational studies have suggested potential harms associated with treating asymptomatic elevated inpatient BP, which brings current practice into question.”
Without target organ involvement, we do not need to be initiating IV medications or trying to treat the numbers
Bress AP, Anderson TS, Flack JM, Ghazi L, Hall ME, Laffer CL, Still CH, Taler SJ, Zachrison KS, Chang TI; American Heart Association Council on Hypertension; Council on Cardiovascular and Stroke Nursing; and Council on Clinical Cardiology. The Management of Elevated Blood Pressure in the Acute Care Setting: A Scientific Statement From the American Heart Association. Hypertension. 2024 Aug;81(8):e94-e106. doi: 10.1161/HYP.0000000000000238. Epub 2024 May 28. PMID: 38804130.
Category: Cardiology
Keywords: Hypertension, treatment, asymptomatic (PubMed Search)
Posted: 8/4/2024 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This article from JAMA is targeted at inpatient management of asymptomatic hypertension, however, it’s a great reminder that “hypertensive urgency” is not an entity. We should be treating the patient and not the numbers. Gradual, out patient lowering of asymptomatic hypertension is the safe and proper way to approach this. Spread the word to your friends in primary care, urgent care, dental, and other office based practices.
Jacobs ZG, Anderson TS. Management of Elevated Blood Pressure in the Hospital—Rethinking Current Practice. JAMA Intern Med. Published online July 22, 2024. doi:10.1001/jamainternmed.2024.3279
Category: Cardiology
Keywords: syncope, pre-syncope (PubMed Search)
Posted: 6/27/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
The systematic review of presyncope literature found that presyncope should be treated the same as syncope in terms of work up and disposition.
“In conclusion, the prevalence of short-term serious outcomes among ED patients with presyncope ranges from one in four to one in 20, with arrhythmia being the most common serious outcome. Our review indicates that presyncope may carry a similar risk to syncope, and hence, the same level of caution should be exercised for ED presyncope management as that of ED syncope.”
Serious outcomes among emergency department patients with presyncope: A systematic review
Hadi Mirfazaelian MD, MSc, Ian Stiell MD, MSc, FRCPC, Rasoul Masoomi PhD, Khazar Garjani MD, Venkatesh Thiruganasambandamoorthy MBBS, CCFP-EM, MSc
First published: 09 June 2024 Academic Emergency Medicine
Category: Cardiology
Posted: 5/24/2024 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
Category: Cardiology
Posted: 4/28/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
In a cohort of 93,512 ED patients discharged with a diagnosis of hypertension there were 4400 who received a prescription for antihypertensives. The group receiving a prescription had fewer 30 day revisits and adverse events such as MI, CHF, etc.
Previous study’s have found it is safe to prescribe antihypertensives from the ED.
This study is limited by the fact it is not a randomized control trial and there are many variables as to why the select patients received prescriptions
The authors conclude: “Prescription antihypertensive therapy for discharged ED patients is associated with a 30-day decrease in severe adverse events and ED revisit rate.”
Brett R. Todd MD, Yuying Xing PhD, Lili Zhao PhD, An Nguyen MD, Robert Swor DO, Lauren Eberhardt, Amit Bahl MD
Journal of the American College of Emergency Physicians OpenVolume 5, Issue 2 e13138
Category: Cardiology
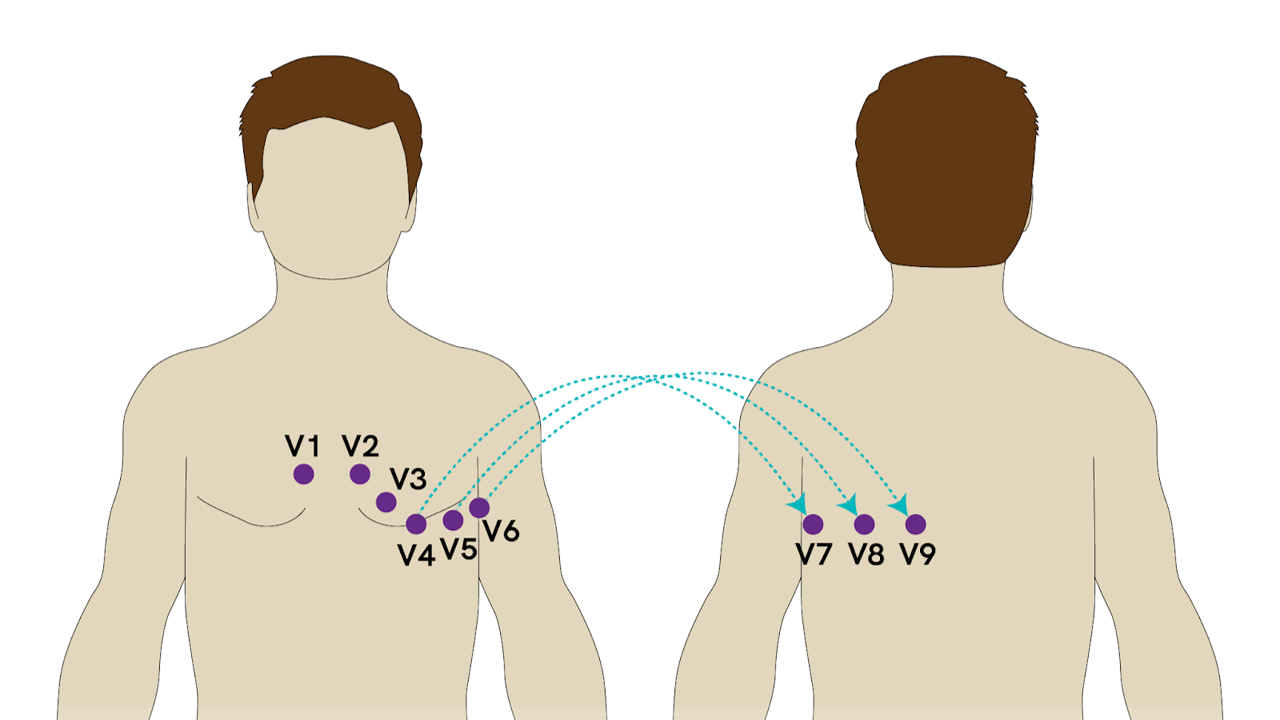
Keywords: Posterior MI, ECG (PubMed Search)
Posted: 5/8/2023 by Leen Alblaihed, MBBS, MHA
Click here to contact Leen Alblaihed, MBBS, MHA
52 yo M with chest pain and shortness of breath, ECG as shown, do you activate cath lab?
The posterior descending artery (PDA) supplies the posterior third of the interventricular septum, including the posterior and inferior walls of the left ventricle. The vessel most commonly originates from either the right coronary artery (right dominant), left circumflex artery (left dominant), or both (codominant).
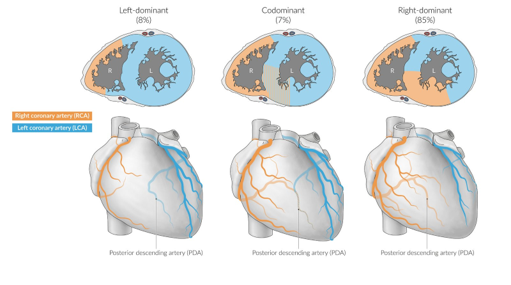
Posterior MI frequently occurs as an extension of an inferior or lateral infarct. Isolated posterior MI occurs in 3 - 5% of cases (1), and is frequently missed on ECGs.
The posterior myocardium is not directly visualized on a standard 12 lead ECG, but reciprocal changes of STEMI in the anteroseptal leads (V1- V3) are seen (the posterior electrical activity is recorded from the anterior side of the heart)
If in V1- V3 you see
* ST segment depression
* Tall R wave
* Upright T waves
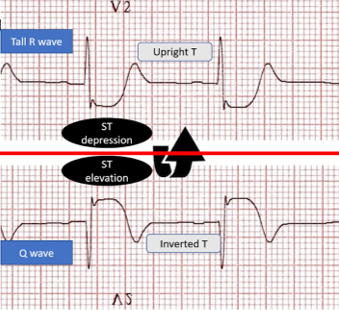
Consider posterior MI as a cause. You need to then obtain an ECG with posterior leads. If there is 0.5 mm elevation in any posterior lead this is diagnostic of posterior MI.
van Gorselen EO, Verheugt FW, Meursing BT, Oude Ophuis AJ. Posterior myocardial infarction: the dark side of the moon. Neth Heart J. 2007 Jan;15(1):16-21
Category: Cardiology
Keywords: POCUS, ACS, Regional Wal Motion Abnormality, Ultrasound (PubMed Search)
Posted: 5/1/2023 by Alexis Salerno Rubeling, MD
(Updated: 2/7/2026)
Click here to contact Alexis Salerno Rubeling, MD
In this study the researchers looked at patients presenting to the emergency department with high suspicion for ACS and explored if Regional Wall Motion Abnormality (RWMA) evaluation by EPs was associated with occlusion myocardial ischemia (OMI).
FOCUS identified RWMA in 87% of patients with coronary angiography proven OMI. With a sensitivity of 94%, specificity 35%, and overall accuracy of 78%.
The authors concluded that using FOCUS can have good utility when a patient is high risk for OMI and has an equivocal ekg. However, if RWMA is not present, physicians should still continue with work up such as cardiac catheterization.
To evaluate RWMA it is easiest to:
For more information check out this ACEPnow article: https://www.acepnow.com/article/detect-cardiac-regional-wall-motion-abnormalities-point-care-echocardiography/?singlepage=1
Bracey A, Massey L, Pellet AC, Thode HC, Holman TR, Singer AJ, McClure M, Secko MA. FOCUS amay detect wall motion abnormalities in patients with ACS, A retrospective study. Am J Emerg Med. 2023 Apr 2;69:17-22. doi: 10.1016/j.ajem.2023.03.056. Epub ahead of print. PMID: 37037160.
Category: Cardiology
Posted: 7/19/2015 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Opiates Causing Cardiac Toxicity
- Opiates are well known in their ability to cause sedation, euphoria, and respiratory depression, however are classically considered devoid of cardiac properties.
- Methadone a synthetic central-acting μ-opioid receptor agonist has been associated with dose-dependent QTc interval prolongation and torsade de pointes (TdP).
- Utilization of other less known drugs of abuse, specifically loperamide (peripherally acting μ-opioid receptor agonist) has been increasing in popularity.
- A surge in recent case reports has shown a potential causal association of loperamide with prolongation of the QTc interval and subsequent TdP.
- Toxic ingestion of loperamide leading to TdP has been successfully managed with standard TdP therapies (magnesium, isoproterenol, and pacing).
Marzec LN, Katz DF, Peterson PN, Thompson LE, Haigney MC, Krantz MJ. Torsade de pointes associated with high dose loperamide ingestion. J Innov Cardiac Rhythm Manage 2015; 6:1897–1899.
Marraffa JM, Holland MG, Sullivan RW, et al. Cardiac conduction disturbance after loperamide abuse. Clin Toxicol (Phila) 2014; 52:952–957.
Category: Cardiology
Posted: 6/28/2015 by Semhar Tewelde, MD
(Updated: 2/7/2026)
Click here to contact Semhar Tewelde, MD
Giant Cell Myocarditis
Giant cell myocarditis (GCM) is an infrequent, but often fatal form of acute myocarditis that has been shown to respond to cyclosporine-based immunosuppressive therapy
Even after heart transplantation GCM recurrence in the donor heart has been cited as high as 20% to 25%
Patients are surviving longer without transplantation because of efficacious medical therapy
A multi-institutional prospective data set revealed several novel findings in GCM:
· Long-term immunosuppression appears capable of lengthening transplantation-free survival ~19 years beyond initial diagnosis
· Cessation and/or reduction of immunosuppression are associated with GCM recurrence
· Patients who developed cyclosporine associate renal failure were able to be switched to a sirolimus-based regimen
Maleszewski J, Orellana V, et al. Long-Term Risk of Recurrence, Morbidity and Mortality in Giant Cell Myocarditis. Am J Cardiol 2015;115:1733e1738
Category: Cardiology
Posted: 5/24/2015 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Reperfusion Ventricular Fibrillation
Ventricular fibrillation during reperfusion in STEMI is an infrequent, but serious complication.
Among ~4000 with STEMI between 2007-2012, 71 (1.9%) had reperfusion Vfib.
Increased risk for reperfusion Vfib is associated with: history of MI, aspirin and b-blocker use, Vfib before PCI, left main CAD, inferior MI, symptom-to-balloon time <360 minutes, maximal ST-segment elevation in a single lead >300 μV, and sum of ST-segment deviations in all leads >1,500 μV.
The sum of ST-segment deviations in all leads >1500 μV was an independent predictor of reperfusion Vfib.
Demidova M, Carlson J , et al. Am J Cardiol 2015;115:417e422
Category: Cardiology
Posted: 5/10/2015 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Ischemic ECG Findings: Significance of the U-wave
The U-wave is a small deflection immediately following the T-wave, commonly with the same polarity as the T-wave and most prominently seen in precordial leads V2–V3.
Prominent U-waves are most often seen with bradycardia and hypokalemia, but can also be secondary to other electrolyte imbalances and medications.
Typically, T- and U-wave polarities are concordant; discordant U-waves have been identified several hours prior to other ECG changes in acute myocardial infarction.
Some studies note that exercise induced U-wave inversion is highly predictive of CAD; negative U -waves in the precordial leads during exercise had a higher specificity (88% vs. 70%) & positive predictive value (77% vs. 61%) for ischemia than ST-depression.
Reinig et al. 2005 showed that negative concordance of T- and U-waves have poor prognosis & is quite specific for ischemia.
· ECG’s were divided into 3 groups:
o Type 1 T-U discordance (negative T waves + positive U waves)
o Type 2 T-U discordance (positive T waves + negative U waves)
o Negative T-U concordance (both T & U waves negative)
* Significantly higher rate of CAD (88% vs. 58%) (P-value <. 0001) in the negative T-U concordance group
Sovari AA, Farokhi F, et al. Inverted U-wave, a specific electrocardiographic sign of cardiac ischemia. Am J Emerg Med. 2007 Feb;25(2):235-7.
Reinig MG, Harizi R, et al. Spodick Electrocardiographic T- and U-wave discordance. Ann Noninvasive Electrocardiol. 10 (1) (2005), pp. 41–46.
Category: Cardiology
Posted: 4/19/2015 by Semhar Tewelde, MD
(Updated: 2/7/2026)
Click here to contact Semhar Tewelde, MD
Cardiac Sarcoidosis
- Cardiac Sarcoidosis (CS) is reported to involve ~2-5% of patients with systemic sarcoidosis. An increasing proportion of patients are presenting with isolated CS.
- Isolated CS is associated with a higher female predominance; severe LV involvement, heart failure, and poor prognosis.
- Manifestations range from symptomatic conduction disturbances, dysrhythmias, progressive heart failure, and silent myocardial granulomas - leading to sudden cardiac death.
- CS is a serious condition with a quoted 5-year survival ~60-75%.
- Corticosteroid therapy is considered cornerstone in management, but evidence is largely observational and no randomized trials have been performed to date.
Kandolin R, Lehtonen J, et al. Cardiac Sarcoidosis. Circulation 131 (7) Feb. 2015.
Category: Cardiology
Posted: 4/5/2015 by Semhar Tewelde, MD
(Updated: 2/7/2026)
Click here to contact Semhar Tewelde, MD
The Heart Is Just a Muscle
- Heart failure and peripheral myopathies share similar symptoms such as exertional fatigue, weakness, and dyspnea.
- The role of endomyocardial biopsy (EMB) to aid in the diagnosis of new-onset heart failure is controversial and major society guidelines recommend against this procedure in the routine evaluation of patients with heat failure.
- Nevertheless when symptoms of heart failure persist despite conventional imaging modalities and treatment one must consider uncommon conditions, such as mitochondrial disorders.
- Mitochondrial disorders are characterized as clinical syndromes and patients can present with any one of the following: ophthalmoplegia, proximal muscle weakness, isolated myopathy with exercise intolerance and myalgia, severe myopathy of infancy or childhood, or multisystem involvement with myopathy.
- Myocardial tissue is highly dependent on mitochondria for energy production and is therefore susceptible to defects in mitochondrial function. Cardiac manifestations of these syndromes include both arrhythmias and cardiomyopathy.
McGarrah R. et al. The Heart is Just a Muscle. Circulation. March 2015.
