Category: EMS
Keywords: cardiac arrest, hypoxia, CPR bystander (PubMed Search)
Posted: 12/18/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
This was a review of the cardiac arrest registry of Norway between 2016-2021. The incidence of pediatric out of hospital cardiac arrests was 4.6 per 100,000 child years and significantly higher in children < 1 year (20.9 per 100,000 child years). There was an overall 18% one year survival rate in the 308 patients included.
Leading causes of arrests were choking, respiratory disease, drowning and SIDS, making up 67% of cases.
73% of the arrests were initially asystolic and 14% were PEA on EMS arrival. The presence of shockable rhythms increased with age and VT/VF were the initial rhythm in up to 15% of the 13-17 year age group.
88% of patients received bystander CPR ( with 68% receiving both chest compressions and ventilations). A minority of these patients were in a shockable rhythm, but 7 total patients were in refractory VF. Mechanical CPR devices were used in 35 patients aged 11-17. ECMO was started in 19 cases.
Bottom line: The rate of bystander CPR in this study was very high and other jurisdictions can attempt to learn from the system in place in Norway to increase their local prehospital interventions.
Kelpanides IK, Katzenschlager S, Skogvoll E, et al. Out-of-hospital cardiac arrest in children in Norway: A national cohort study, 2016-2021. Resusc Plus. 2024;18:100662. Published 2024 May 18. doi:10.1016/j.resplu.2024.100662
Category: Critical Care
Posted: 12/17/2024 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
High-Intensity NIPPV for Acute COPD Exacerbations?
Luo Z, et al. Effect of high-intensity vs low-intensity noninvasive positive pressure ventilation on the need for endotracheal intubation in patients with an acute exacerbation of chronic obstructive pulmonary disease. JAMA. Published online September 2024.
Category: Ultrasound
Keywords: POCUS, vascular access, pediatrics (PubMed Search)
Posted: 12/16/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
In adult patients, ultrasound-guided long catheter IVs for difficult venous access have been shown to provide increased duration of use, reduced complication rates, and greater cost-effectiveness.
However, there are relatively few studies examining the use of ultrasound for IV access in pediatric patients.
A recent study, the DIAPEDUS study, investigated the success rate of peripheral IV access with and without ultrasound assistance in pediatric patients with difficult venous access.
The study included 110 pediatric patients. IVs were placed by 25 nurses and 6 pediatricians, each of whom had completed departmental training involving at least 20 ultrasound-guided IV placements prior to the study.
The results showed a significantly higher success rate on the first attempt with ultrasound-guided techniques (90% vs. 18%), along with reduced procedural time and fewer attempts overall.
Bottom Line: For patients with known difficult venous access, ultrasound-guided IV placement should be the first-line approach.
D'Alessandro M, Ricci M, Bellini T, Chianucci B, Calevo MG, Piccotti E, Moscatelli A. Difficult Intravascular Access in Pediatric Emergency Department: The Ultrasound-Assisted Strategy (DIAPEDUS Study). J Intensive Care Med. 2024 Mar;39(3):217-221. doi: 10.1177/08850666231199050
Bahl A, Johnson S, Hijazi M, Mielke N, Chen NW. Cost effectiveness of ultrasound-guided long peripheral catheters in difficult vascular access patients. J Vasc Access. 2024 Jul;25(4):1204-1211. doi: 10.1177/11297298231154297.
Category: Trauma
Keywords: Trauma, oxygen, mortality (PubMed Search)
Posted: 12/14/2024 by Robert Flint, MD
(Updated: 12/15/2024)
Click here to contact Robert Flint, MD
In this randomized trial of restrictive oxygen (arterial oxygen sat of 94% ) vs. liberal oxygen (12-15 L of O2 per minute) for 8 hours after traumatic injury there was no difference in mortality or major respiratory complications at 30 days between the two groups.
Further evidence that managing hypoxia is important but over oxygenation at best offers no benefit and may add harm.
Arleth T, Baekgaard J, Siersma V, et al. Early Restrictive vs Liberal Oxygen for Trauma Patients: The TRAUMOX2 Randomized Clinical Trial. JAMA. Published online December 10, 2024. doi:10.1001/jama.2024.25786
Category: Cardiology
Posted: 12/14/2024 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Cardiovascular disease (CVD) is the leading cause of death both in the United States and globally for both men and women.
Major adverse cardiovascular events (MACE) is a commonly used composite outcome.
MACE is defined as non-fatal stroke/acute myocardial infarction/heart failure or cardiovascular death.
Physical inactivity is a leading risk factor for noncommunicable diseases and death worldwide
Up to 5 million deaths/yr could be averted with increased physical activity
Regular physical activity reduces the risk of many types of cancer by 8-28%, diabetes by 17%, heart disease and CVA by 19%, and dementia by 20%.
Many adults and children find meeting the recommended physical activity goals very challenging.
A recent observational study found that just 1.5-to-4-minute small bursts of high intensity exercise throughout the day may help lower an individual’s risk of MACE.
To clarify, this does not mean going to the gym to do a 45-minute HIIT class
Vigorous intermittent lifestyle physical activity (VILPA) involves such simple things as carrying the groceries a short distance or taking the work stairs instead of the elevator.
Such activities are more feasible for all of us vs structured exercise for obvious reasons.
Study group was >100,000 middle-aged men and women. Average age 61.
All participants wore an activity tracker continuously for a full week.
This data was used to calculate VILPA bouts throughout the day.
Female participants with no formal exercise regimen who recorded just 3.4 minutes of VILPA a day were 50% less likely to have a MI, had a 67% decreased risk for heart failure and 45% less likely to develop any type of MACE vs those who did not clock any VILPA during their day.
Female participants who recorded just 1.2-1.6 minutes of VILPA a day had a 33% lower risk of MI, 40% decreased risk of heart failure and 30% lower risk of MACE.
In male participants, those with 5.6 minutes of VILPA each day had a 16% reduced risk of having MACE than those who did not have any VILPA.
Differences may be due to women’s VILPA intensity was roughly 20% greater than men
Conclusion: Take the stairs
Stamatakis E, et al. Device-measured vigorous intermittent lifestyle physical activity (VILPA) and major adverse cardiovascular events: evidence of sex differences. Br J Sports Med. 2024 Oct 28
Category: Pediatrics
Keywords: pediatrics, seizure, infant, epilepsy, spams, infantile spasms (PubMed Search)
Posted: 12/13/2024 by Kathleen Stephanos, MD
(Updated: 2/8/2026)
Click here to contact Kathleen Stephanos, MD
Infantile Spasms (now known as Infantile Epileptic Spasms Syndrome- IESS) is a subtle, can't miss diagnosis occurring in children under the age of 2, with 90% presenting before 1 year of age.
History:
Presentation for these patients can be sporadic, recurrent, flexion or extension of the limbs or head. The patient typically remains alert during an episode, but they can be startled or appear uncomfortable from the sudden movement.
With smart phone use, parents often have videos of the events that a provider can see as they are often no events in the ED.
Prognosis is very poor with up to 50% having long-term neuro-cognitive complications or regression.
Examination:
A complete physical exam should be performed with particular attention to focal neurologic deficits which would require emergent imaging, signs of electrolyte abnormalities (eg. Chvostek's sign in hypocalcemia), and evidence of neurocutenous syndromes (eg. Neurofibromatosis, tuberous sclerosis).
Testing:
Diagnosis is made with EEG showing hypsarrhythmia. This should be done as soon as possible, most often requiring an inpatient admission.
Lab work can be done to exclude other possible causes of abnormal movements including assessing for electrolyte abnormalities.
Imaging in the ED is not typically indicated unless there is concern based on exam. MRI is the imaging modality of choice, and is often completed after EEG confirmed diagnosis.
Treatment:
Management is initiated in conjunction with a pediatric neurologist with most common therapies being corticotropin (ACTH) and vigabatrin.
Smith MS, Matthews R, Rajnik M, Mukherji P. Infantile Epileptic Spasms Syndrome (West Syndrome). 2024 Feb 1. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30725936.
Category: Pharmacology & Therapeutics
Keywords: Antibody-drug conjugates, toxicities, adverse effects (PubMed Search)
Posted: 12/11/2024 by Wesley Oliver
Click here to contact Wesley Oliver
A recent review article highlighted the adverse effects that emergency physicians should know of with the novel antineoplastic agents. The adverse effects and the associated agents are briefly summarized from the article in the table below. A link to the full article is below.
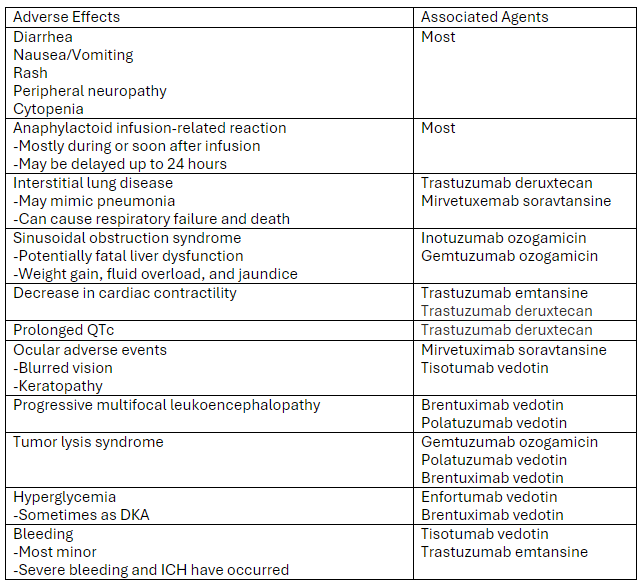
Link to article: Antibody-Drug Conjugates: The Toxicities and Adverse Effects That Emergency Physicians Must Know - Annals of Emergency Medicine
Markides DM, Hita AG, Merlin J, Reyes-Gibby C, Yeung SJ. Antibody-Drug Conjugates: The Toxicities and Adverse Effects That Emergency Physicians Must Know. Ann Emerg Med. 2024 Dec 3:S0196-0644(24)01142-9. doi: 10.1016/j.annemergmed.2024.10.015. Epub ahead of print. PMID: 39641680.
Category: Critical Care
Keywords: VExUS, IVC, POCUS, Venous Congestion (PubMed Search)
Posted: 12/10/2024 by Cody Couperus-Mashewske, MD
Click here to contact Cody Couperus-Mashewske, MD
The Venous Excess Ultrasound (VExUS) exam integrates IVC, portal, hepatic, and renal vein findings to assess venous congestion and guide management, such as diuresis, in critically ill patients.
Technique:
Tips:
Interpretation:
Sometimes when other clinical information is contradictory, having the extra data point of the VExUS exam can be extremely useful to determine the best plan for a patient. Practice looking for the portal/hepatic veins and getting the waveforms on patients with a CLEAR clinical picture of venous congestion, then practice on more difficult cases.
Assavapokee, T., Rola, P., Assavapokee, N. et al. Decoding VExUS: a practical guide for excelling in point-of-care ultrasound assessment of venous congestion. Ultrasound J 16, 48 (2024). https://doi.org/10.1186/s13089-024-00396-z
Category: Trauma
Posted: 12/8/2024 by Robert Flint, MD
(Updated: 12/9/2024)
Click here to contact Robert Flint, MD
What is the diagnosis? Treatment? Other imaging indicated?
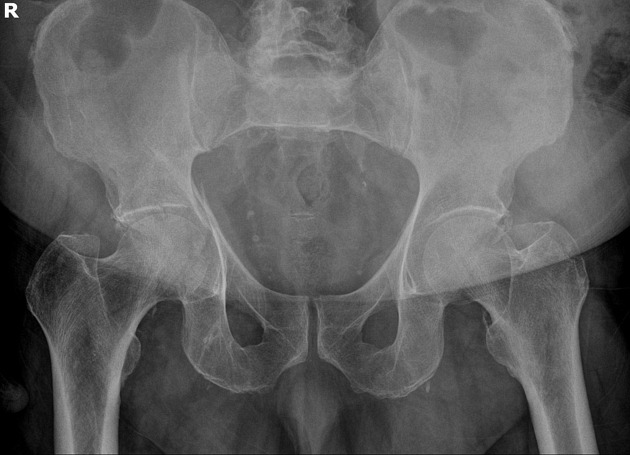
Acetabulum fracture.
Usually seen in high mechanism situations such as MVCs. Can be seen in elderly fall patients.
Treatment is usually surgical (ORIF) unless non-displaced or if it involves less than 20% of posterior column. These can be managed with 6 weeks of minimal weight bearing. CT scan is almost universally used for better visualization and operative management.
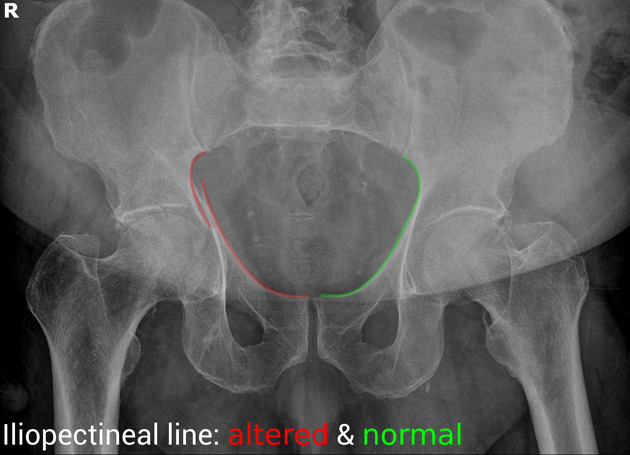
“Some landmarks of the hip are compared on the right and left sides of the pelvis:
https://radiopaedia.org/cases/acetabular-fracture-anterior-and-posterior-columns
https://www.orthobullets.com/trauma/1034/acetabular-fractures
Category: Trauma
Keywords: Liver laceration, embolization, observation. (PubMed Search)
Posted: 12/7/2024 by Robert Flint, MD
(Updated: 12/8/2024)
Click here to contact Robert Flint, MD
This prospective observational study looked at patients with liver lacerations and active contrast extravasation who either had immediate embolization vs. observation. After matching for age, injury score etc. the observation first approach did as well as those who had immediate embolization.
Journal of Trauma and Acute Care Surgery 97(5):p 764-769, November 2024. | DOI: 10.1097/TA.0000000000004372
Category: Cardiology
Keywords: Aaa (PubMed Search)
Posted: 12/7/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This study tried to expand upon what they describe as the classic triad of signs to diagnose ruptured AAA “(1) abdominal pain, (2) hypotension and (3) a pulsatile abdominal mass”. They tested these against the _modified abdominal aortic aneurysm rupture signs. “_The MARS-signs encompassed (1) the registered pain-associated symptoms or signs, (2) all hypovolemic associated signs, and (3) pulsatile abdominal mass and/or ultrasound finding”. The MARS did slightly better in identifying ruptured AAA retrospectively. For me, this doesn’t add a great deal of help in making this can’t miss diagnosis and further work is necessary.
Bergmark, P., Sadeghi, M., Talvitie, M. _et al._Initial signs in patients with ruptured abdominal aortic aneurysms: time for an expanded triad?.Scand J Trauma Resusc Emerg Med 32, 94 (2024). https://doi.org/10.1186/s13049-024-01268-0
Category: Critical Care
Keywords: Subclavian CVC (PubMed Search)
Posted: 12/2/2024 by Jordan Parker, MD
(Updated: 12/3/2024)
Click here to contact Jordan Parker, MD
Background:
Ultrasound-guided subclavian central venous catheter (CVC) placement has become a preferred site due to low risk of infection and a low risk of complication. Complications include arterial puncture, pneumothorax, chylothorax, and malposition of the catheter. Ultrasound guidance can significantly reduce the risk of these complications aside from catheter malposition. The most common sites of malposition are in the ipsilateral internal jugular vein or the contralateral brachiocephalic vein. This study sought to evaluate the rate of catheter malposition between left-and right-sided subclavian vein catheter placement using ultrasound guidance with an infraclavicular approach.
Study:
Results:
Take Home:
For infraclavicular ultrasound-guided subclavian CVC placement, consider using the left-side over the right if no contraindications for left-sided access exist.
The authors proposed anatomical differences in the subclavian veins as the etiology for the difference in malposition rates. Images are provided in the paper. Patient positioning may also play a role which the authors commented on and other clinicians have responded to the article with their thoughts.
Supraclavicular subclavian vein access is also discussed as an alternative option that can provide real-time tracking of the guidewire into the correct location to reduce malposition rates.
Read More below.
Supraclavicular approach and response to the article:
Kander, Thomas MD, PhD1,2; Adrian, Maria MD, PhD1,3; Borgquist, Ola MD, PhD1,3. Right Subclavian Venous Catheterization: Don’t Throw the Baby Out With the Bathwater. Critical Care Medicine 52(12):p e645-e646, December 2024. | DOI: 10.1097/CCM.0000000000006388
Adrian M, Kander T, Lundén R, Borgquist O. The right supraclavicular fossa ultrasound view for correct catheter tip positioning in right subclavian vein catheterisation: a prospective observational study. Anaesthesia. 2022 Jan;77(1):66-72. doi: 10.1111/anae.15534. Epub 2021 Jul 14. PMID: 34260061.
Patient position discussion:
Tokumine, Joho MD, PhD; Moriyama, Kiyoshi MD, PhD; Yorozu, Tomoko MD, PhD. Influence of Arm Abduction on Ipsilateral Internal Jugular Vein Misplacement During Ultrasound-Guided Subclavian Venous Catheterization. Critical Care Medicine 52(12):p e646-e647, December 2024. | DOI: 10.1097/CCM.0000000000006410
Shin KW, Park S, Jo WY, Choi S, Kim YJ, Park HP, Oh H. Comparison of Catheter Malposition Between Left and Right Ultrasound-Guided Infraclavicular Subclavian Venous Catheterizations: A Randomized Controlled Trial. Critical Care Medicine. 2024 Oct 1;52(10):1557-1566. doi: 10.1097/CCM.0000000000006368. Epub 2024 Jun 24. PMID: 38912886.
Category: Ultrasound
Keywords: POCUS, Lung ultrasound, EMS (PubMed Search)
Posted: 12/2/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
Early treatment of congestive heart failure (CHF) exacerbations is associated with improved mortality rates and shorter hospital length of stay. Lung ultrasound is a valuable tool in diagnosing CHF exacerbations. Recently, several studies have explored the use of lung ultrasound in the prehospital settings to expedite diagnosis and treatment.
A recent systematic review and meta-analysis evaluated the diagnostic accuracy and clinical impact of prehospital lung ultrasound. The authors found similar test characteristics to point-of-care ultrasound (POCUS) performed in the emergency department.
The eight studies included in the analysis utilized varying lung ultrasound protocols, analyzing between 2 and 8 lung zones. Notably, only two studies involved paramedics performing the ultrasounds, yet no significant difference in diagnostic accuracy was observed.
Further research is needed to evaluate the training requirements for prehospital providers and the broader impact of prehospital lung ultrasound on treatment strategies and patient outcomes.
Category: Trauma
Keywords: vetebral fracture, trauma, fall, spinal injury (PubMed Search)
Posted: 12/1/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Fall from a height of 6 feet with back pain. Plain film shown. What is the diagnosis? Any further imaging indicated? Treatment? Disposition?
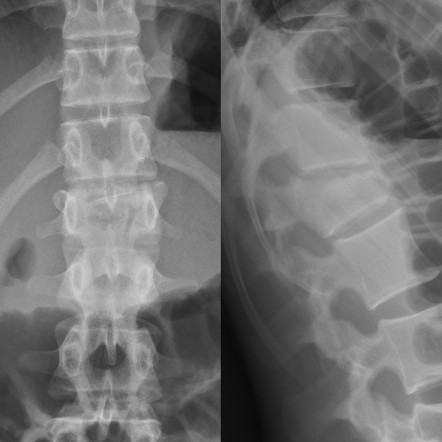
The question that must be answered is, is this a compression fracture or a burst fracture. A compression fracture without any retropulsion into the canal and any other associated injuries is a stable fracture that can be managed with pain control, out patient follow up and possible kyphosplasty for significant loss of vertebral height. A burst fracture is inherently unstable and is a risk for spinal cord injury. CT imaging answers are questions most efficiently.
To help distinguish burst from compression: “Burst fractures are a type of compression fracture related to high-energy axial loading spinal trauma that results in disruption of a vertebral body endplate and the posterior vertebral body cortex. Retropulsion of posterior cortex fragments into the spinal canal is frequently included in the definition. However, some authors, including the popular AO spine classification system, define a burst fracture as any axial compression fracture involving an endplate and the posterior cortex regardless of retropulsion." 2
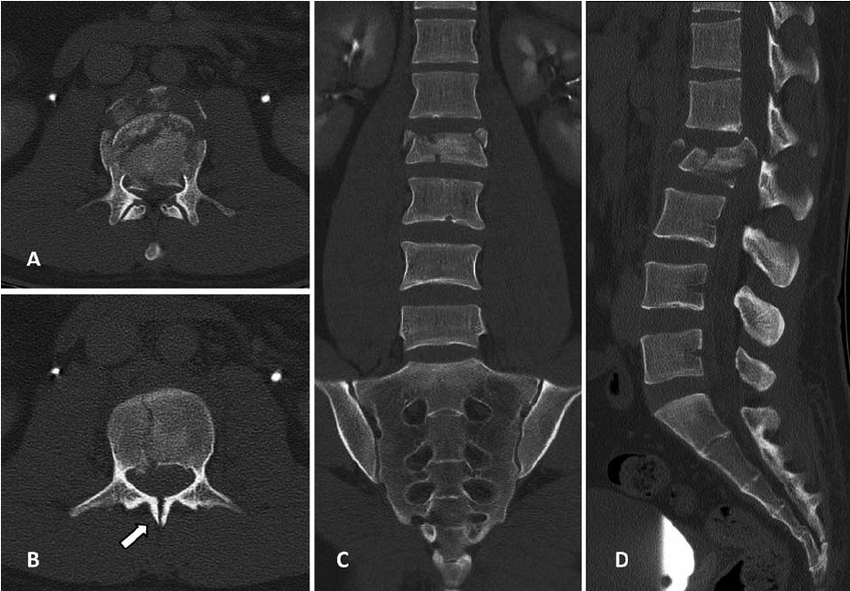
1. https://radiopaedia.org/cases/acute-l1-burst-compression-fracture
Category: Geriatrics
Keywords: Beers criteria, geriatric, prescribing, elderly, drug interaction, pharmacology (PubMed Search)
Posted: 11/30/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
As a reminder, prescribing medications to older patients should be done with caution because of changed physiology, co-morbid conditions and other currently used medications. The Beers Criteria is a helpful list of medications that may cause trouble for your older patients. https://www.guidelinecentral.com/guideline/340784/#section-2776198 is a list of medications to either avoid or prescribe carefully in this patient population.
Pay particular attention to medications that have anticholinergic properties as they cause change in mental status and increase the risk for falls.
By the 2023 American Geriatrics Society Beers Criteria® Update Expert Panel
Pages: 2052-2081
First Published: 04 May 2023 https://agsjournals.onlinelibrary.wiley.com/doi/epdf/10.1111/jgs.18372
2. https://www.carepatron.com/templates/beers-criteria-template
Category: Administration
Keywords: Thanksgiving (PubMed Search)
Posted: 11/27/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
From all of us at UMEM, Happy Thanksgiving!!
We are incredibly Thankful for each of you and all that you do to care for patients and their families.
We are Thankful for those legends who have blazed the path in EM like Greg Henry who the EM community lost yesterday. Our thoughts are with his family. Thank you Dr. Henry for inspiring so many of us. Our pearls today are two of his famous quotes:
“Medicine is show business for ugly people.”
“You don’t go to Disney and see Mickey taking a smoke break. You have to be on when you are on shift”
Category: Administration
Keywords: artificial intelligence, emergency department, emergency practice, machine learning (PubMed Search)
Posted: 11/27/2024 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
Gooble, gooble,… gulp, some food for thought on the eve of Thanksgiving.
The development of artificial intelligence (AI) in emergency medicine is well under way. The schematic below and accompanying reference presents the anticipated stages in the process of AI development, including important features, considerations, and challenges as we move towards increased integration of AI in our practice of EM.
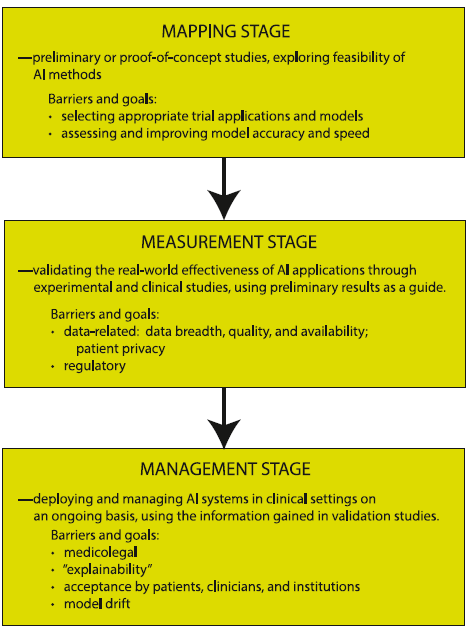
Petrella, R. The AI Future of Emergency Medicine. Ann Emerg Med. 2024;84:139-153. https://doi.org/10.1016/j.annemergmed.2024.01.031
Category: Critical Care
Keywords: ketamine, etomidate, rapid sequence intubation, hemodynamic instability, adrenal suppression (PubMed Search)
Posted: 11/26/2024 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
It’s the age-old question. We’ve read studies comparing propofol vs. etomidate, ketofol vs. etomidate, and now a meta-analysis about ketamine vs. etomidate. Etomidate is the staple induction agent for RSI, mostly used by Emergency Medicine, and to a degree in the Intensive Care Unit. However, the question about adrenal suppression was initiated in the early 2000s and researchers have been looking for other alternatives. This meta analysis attempted to look for another answer.
Settings: A meta-analysis of randomized controlled trials
Participants: 2384 patients who needed emergent intubation were included.
Outcome measurement: Peri-intubation instability
Study Results:
Compared with etomidate, ketamine was associated with higher risk of hemodynamic instability and moderate certainty (RR 1.29, 95% CI 1.07-1.57).
Ketamine was associated with lower risk of adrenal suppression, again, with moderate uncertainty (RR 0.54, 95% CI 0.45-0.66).
Ketamine was not associated with differences and risk of first successful intubation nor mortality.
Discussion:
Most studies were single center and involved small-moderate sample size, ranging from 20 patients to 700 patients.
For adrenal suppression, there were only 3 studies and a total of 1280 patients, thus, the results are still not definitive.
For an academic exercise, the Number Needed to Harm for both hemodynamic instability and adrenal suppression are calculated here.
Number Needed to Harm for hemodynamic instability: 25.
Number needed to harm for adrendal suppression: 11.
Greer A, Hewitt M, Khazaneh PT, Ergan B, Burry L, Semler MW, Rochwerg B, Sharif S. Ketamine Versus Etomidate for Rapid Sequence Intubation: A Systematic Review and Meta-Analysis of Randomized Trials
Category: Hematology/Oncology
Keywords: Cord compression, cancer, metastasis, oncologic emergency (PubMed Search)
Posted: 11/25/2024 by Sarah Dubbs, MD
(Updated: 2/8/2026)
Click here to contact Sarah Dubbs, MD
One of the many siginificant complications of cancers we encounter in the ED is cord compression. Here are pearls from a recently published systematic review focused on metastasis-associated spinal cord compression:
Vavourakis M, Sakellariou E, Galanis A, Karampinas P, Zachariou D, Tsalimas G, Marougklianis V, Argyropoulou E, Rozis M, Kaspiris A, Pneumatikos SG. Comprehensive Insights into Metastasis-Associated Spinal Cord Compression: Pathophysiology, Diagnosis, Treatment, and Prognosis: A State-of-the-Art Systematic Review. J Clin Med. 2024 Jun 19;13(12):3590. doi: 10.3390/jcm13123590. PMID: 38930119; PMCID: PMC11205147.
Category: Trauma
Keywords: collision, extrication, trauma, motor vehicle, extraction, rapid, spinal immobilization (PubMed Search)
Posted: 11/24/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
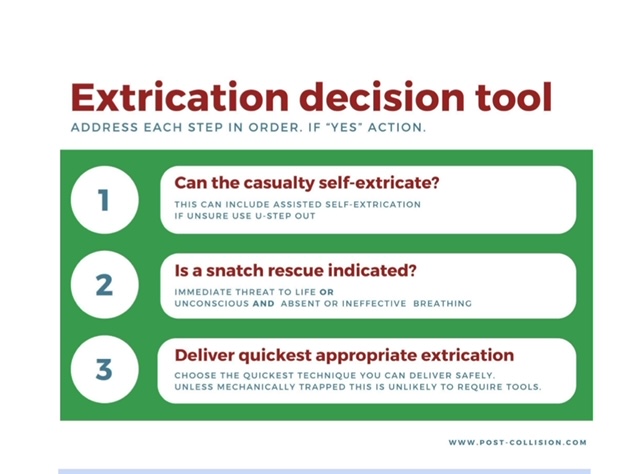
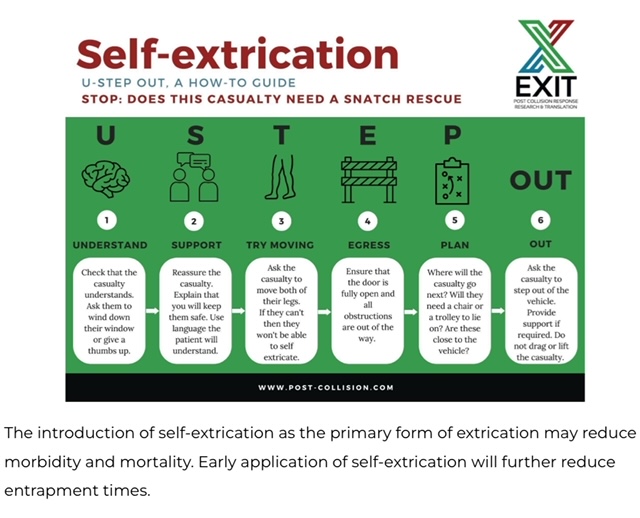
It is important for trauma and emergency care providers to understand what our patients experience prior to arrival in our clean, safe, and structured emergency department. It is also vitally important that we are involved in training and education in the pre-hospital environment. A group in the United Kingdom is challenging the age old “wisdom” that post-motor vehicle crash extrication should be slow, methodical, and work to have absolutely no movement in the spinal canal. Spinal immobilization and slow extrication instead of rapid resuscitation appears to be bad for patients. Based on several of their ground breaking papers they have published a 14 point recommendation of patient extrication post motor vehicle collision. Here are two important tenets they propose. For an in-depth discussion check out November 14, 2024 / CPD, Podcasts, Roadside to Resus.