Category: Orthopedics
Posted: 11/23/2024 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Ankle sprains are frequently lateral.
They occur less frequently to the medial or “high” ankle.
High ankle sprains without fracture occur in 5-6% of ankle injuries presenting to the ED
Rates of injury are much higher in college and professional hockey and football players
The tibiofibular syndesmosis is primarily injured in high ankle sprains
Mechanism: Typically, external rotation or eversion on a dorsiflexed ankle
Example: When a player’s leg is forcefully rotated while foot is planted
Hx: anterior lateral ankle pain. Frequently significant pain with weight bearing.
PE: local tenderness over the syndesmosis ligaments
Two specialized tests may aid in the diagnosis
https://wikism.org/Squeeze_Test#/media/File:Squeeze_test_example.jpg
2. Dorsiflexion-external rotation test – This test attempts to reproduce the forces commonly involved in the original injury. Positive test is reproduction of pain. Position patient similar to above test. Grasp the upper calf with one hand while the other hand grasps the midfoot and places the foot in dorsiflexion and external rotation.
https://www.dralexjimenez.com/wp-content/uploads/2017/07/external-rotation-test-1.png
Category: Trauma
Keywords: Immobilization cervical spine, intubation (PubMed Search)
Posted: 11/21/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
The authors looked at 51 patients intubated with both anterior and posterior cervical collar in place and measured the degree of movement within the spine during intubation. They repeated this process in 51 additional patients with just the posterior portion of the collar in place. They found there was one degree of difference in movement between the two groups. This adds evidence that removing the anterior portion of the collar is safe when intubating trauma patients.
Jo, WY., Choi, JH., Kim, J. et al. Cervical spine motion during videolaryngoscopic intubation using a Macintosh-style blade with and without the anterior piece of a cervical collar: a randomized controlled trial. Can J Anesth/J Can Anesth (2024). https://doi.org/10.1007/s12630-024-02849-4
Category: Ultrasound
Keywords: POCUS; MSK; Achilles tendon (PubMed Search)
Posted: 11/18/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
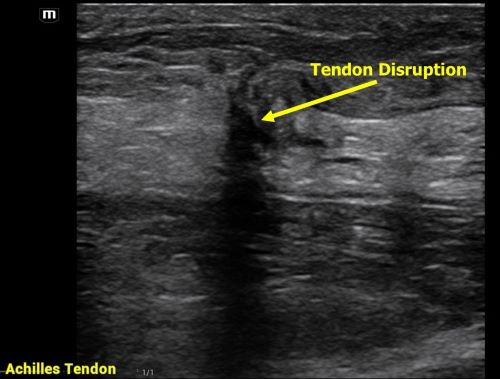
Achilles tendon injuries are commonly encountered in the emergency department. While MRIs are often unavailable, POCUS offers a quick and effective alternative for evaluating such injuries. In one review, the sensitivity of ultrasound for detecting complete Achilles tendon ruptures was 94.8%.
For the POCUS evaluation of the Achilles tendon:
- Place the patient in a prone position with their foot relaxed.
-Begin distally at the tendon’s insertion on the calcaneus and scan proximally, keeping the probe marker oriented toward the patient’s head.
-Next, obtain a transverse view by rotating the probe marker toward the patient’s right side.
-You can even do a sonographic Thompson’s Test!
Findings:
Complete Rupture: Displays as a full disruption of the tendon fibers.
Partial Tear: Shows intact tendon tissue with surrounding edema.
Tendinitis: Appears as a thickened tendon with increased vascularity on color Doppler imaging.
Aminlari A, Stone J, McKee R, Subramony R, Nadolski A, Tolia V, Hayden SR. Diagnosing Achilles Tendon Rupture with Ultrasound in Patients Treated Surgically: A Systematic Review and Meta-Analysis. J Emerg Med. 2021 Nov;61(5):558-567. doi: 10.1016/j.jemermed.2021.09.008.
Category: Trauma
Keywords: Trauma, CT scan, gunshot wound (PubMed Search)
Posted: 11/10/2024 by Robert Flint, MD
(Updated: 11/17/2024)
Click here to contact Robert Flint, MD
This retrospective study illustrates that the use of CT scanning to identify injury in gun shot wounds to the abdomen is not sensitive or specific enough to obviate the need for laparotomy. “Admission hypotension, abdominal pain and/or peritonitis, evisceration, and a transabdominal trajectory were considered clear indications for laparotomy.” If there is clear indication to go to the OR, stopping in CT does not add any benefit.
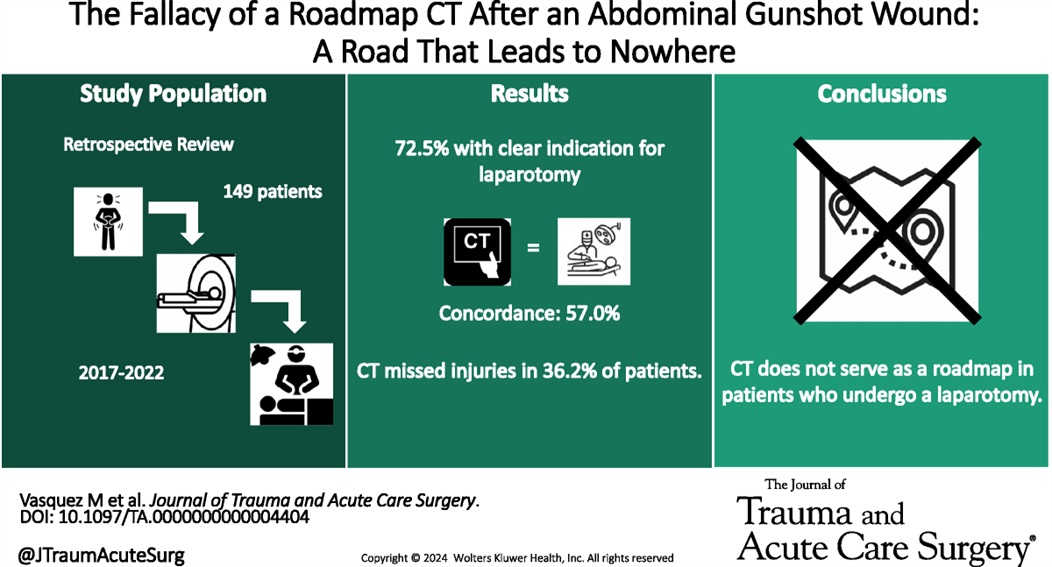
Vasquez, Matthew MD; Dhillon, Navpreet K. MD; Feliciano, David V. MD, FACS, MAMSE†; Scalea, Thomas M. MD, FACS, MCCM
Journal of Trauma and Acute Care Surgery 97(5):p 785-790, November 2024. | DOI: 10.1097/TA.0000000000004404
Category: Pediatrics
Keywords: IN, intranasal, pain control (PubMed Search)
Posted: 11/15/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
This article was a review of randomized control trials using intranasal (IN) fentanyl. There were 8 studies included that showed IN fentanyl was superior to controlling pain compared to other pain medications at the 15-20 minute mark, but not at the 30 and 60 minute marks. There were less reports of nausea and vomiting with IN fentanyl, but no difference in dizziness or hallucinations compared to the other medications included in the various trials (ie morphine, ketamine, po narcotics, ect)
The bioavailability of IN fentanyl ranges from 71-89% with effects noted in 2 minutes with maximal concentrations noted at 7 minutes. The half life is approximately 60 minutes.
Bottom line: Consider IN fentanyl for quick acute pain management in the pediatric patient.
Alsabri M, Hafez AH, Singer E, Elhady MM, Waqar M, Gill P. Efficacy and Safety of Intranasal Fentanyl in Pediatric Emergencies: A Systematic Review and Meta-analysis. Pediatr Emerg Care. Published online April 12, 2024. doi:10.1097/PEC.0000000000003187
Category: Trauma
Keywords: ketamine, trauma (PubMed Search)
Posted: 11/14/2024 by Ashley Martinelli
Click here to contact Ashley Martinelli
An out-of-hospital, randomized, placebo-controlled, blinded, parallel group study was conducted in adult patients under the care of the city fire-based emergency medical services and the local level one trauma center. Adult male patients experiencing moderate to severe pain due to traumatic injuries received either 50mg of intranasal ketamine or placebo in addition to fentanyl after randomization in the field by the paramedic (a novel approach). The primary outcome was reduction of pain by 2 points 30 minutes after study drug administration.
199 patients were randomized with 107 receiving ketamine and 92 with placebo. Patients were young (30-40), and had a median weight of 83 kg. Pretreatment pain scores were 10/10 and patients presented to the ED 14 minutes after receiving study medication. The most common injuries were falls, MVC, and GSW. Half of the patients received IV fentanyl but others had IM or IN routes.
Ketamine receipt did not lead to a 2 point reduction in pain scores (36% vs 44.7% p = 0.22). There was no difference in pain at 3 hours, additional medications received, or total amount of analgesia received. Notably, there were no differences in adverse events.
McMullan JT, Droege CA, Chard KM, Otten EJ, Hart KW, Lindsell CJ, Strilka RJ. Out-of-Hospital Intranasal Ketamine as an Adjunct to Fentanyl for the Treatment of Acute Traumatic Pain: A Randomized Clinical Trial. Ann Emerg Med. 2024 Oct;84(4):363-373. doi: 10.1016/j.annemergmed.2024.04.018. Epub 2024 Jun 12. PMID: 38864781.
Category: Trauma
Keywords: Trauma,blood, TXA, prehospital (PubMed Search)
Posted: 11/10/2024 by Robert Flint, MD
(Updated: 11/11/2024)
Click here to contact Robert Flint, MD
Administration of prehospital TXA was found to improve 28 day mortality and decrease the amount of blood required to be transfused without any increased risk of thromboembolism or seizure. Two grams of TXA was superior to one gram and no TXA.
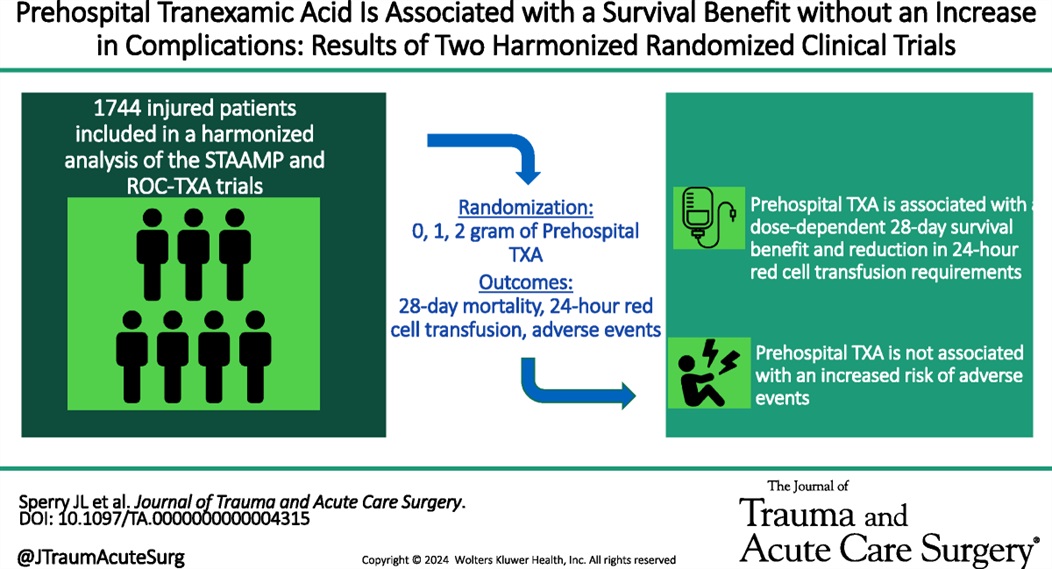
Mazzei, Michael MD, MPH?; Donohue, Jack K. BA?; Schreiber, Martin MD; Rowell, Susan MD, MBA; Guyette, Francis X. MD; Cotton, Bryan MD; Eastridge, Brian J. MD; Nirula, Raminder MD; Vercruysse, Gary A. MD; O'Keeffe, Terence MD; Joseph, Bellal MD; Brown, Joshua B. MD, MSc; Neal, Matthew D. MD; Sperry, Jason L. MD, MPH
Journal of Trauma and Acute Care Surgery 97(5):p 697-702, November 2024. | DOI: 10.1097/TA.0000000000004315
Category: Trauma
Keywords: Trauma, blood, Txa, prehospital (PubMed Search)
Posted: 11/10/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In this small retrospective study comparing outcomes before and after a prehospital blood administration protocol for penetrating trauma was initiated, the authors found improved survival in those receiving prehospital blood despite a five minute longer on scene time in those receiving blood. Also note TXA was part of the blood protocol but not the control group.
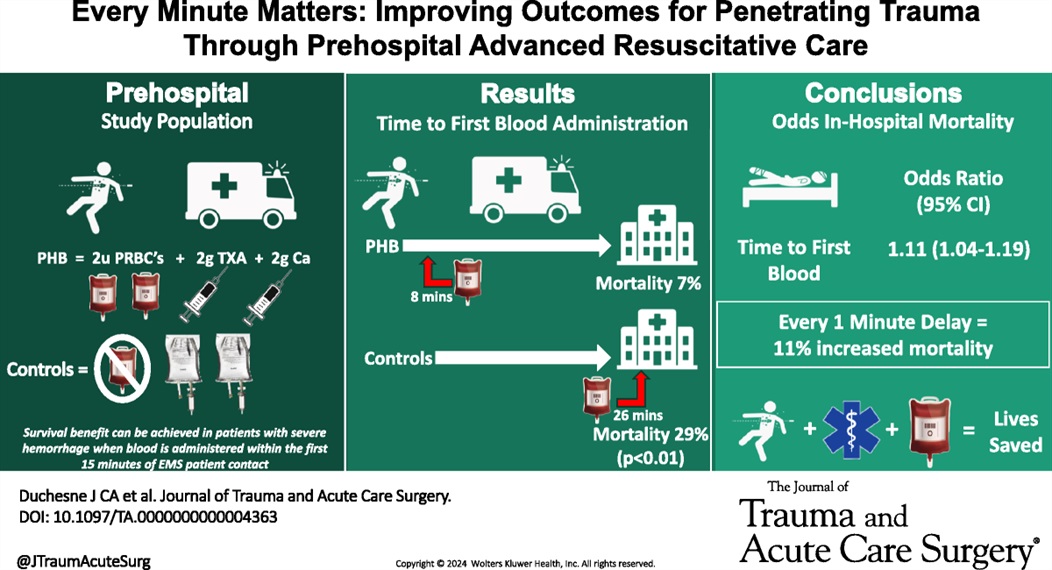
Duchesne, Juan MD; McLafferty, Bryant J. BS; Broome, Jacob M. MD; Caputo, Sydney BS; Ritondale, Joseph P. BS; Tatum, Danielle PhD; Taghavi, Sharven MD, MPH; Jackson-Weaver, Olan PhD; Tran, Sherman MS; McGrew, Patrick MD; Harrell, Kevin N. MD; Smith, Alison MD, PhD; Nichols, Emily MD; Dransfield, Thomas NRP; Marino, Megan MD; Piehl, Mark MD, MPH
Journal of Trauma and Acute Care Surgery 97(5):p 710-715, November 2024. | DOI: 10.1097/TA.0000000000004363
Category: Orthopedics
Posted: 11/9/2024 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Trigger finger/thumb
Occurs from mechanical impingement
-Stenosing tenosynovitis
Much more common in patients with diabetes
Causes clicking, catching, locking and pain
Occurs at the A1 pulley
Flexor tendon “catches” as it attempts to glide through a stenotic flexor tendon sheath
Initially, patient's report painless catching or locking of the affected digit during flexion
During finger flexion and extension, pain is caused by inflamed tendon passing through a relatively constricted tendon sheath
Occurs most often in the ring and middle digits
May improve over the course of the day
Diagnoses with active triggering (with digit flexion and extension) and tenderness to palpation at the first annular pulley (A1) which overlies the first MCP joint
-Ask patient to place hand on table face up and gradually fully flex and extend the fingers
May note a palpable nodule of the flexor tendon
Treatment: Activity modification, NSAIDs and splinting (3-6 weeks)
Corticosteroid injection is very effective
https://www.ahta.com.au/client_images/2553101.png
Category: Pediatrics
Keywords: pediatrics, seizure, neonate, epilepsy (PubMed Search)
Posted: 11/8/2024 by Kathleen Stephanos, MD
Click here to contact Kathleen Stephanos, MD
Neonates are more prone to seizures than children of other ages. Ultimately, a cause of seizures is more likely to be identified in the newborn. Neonatal seizures are subtle and careful attention to repetitive motions of the face, arms or legs should be considered worrisome for seizure. Generalized tonic clonic seizures are rare in this patient population.
Common Causes:
Hypoxic ischemic encephalopathy (most common), infection, stroke, non-accidental trauma, intracranial hemorrhage (including from vitamin K deficiency), metabolic disorders, and structural abnormalities.
Guidelines for Treatment:
Phenobarbital should be used as first line, unless there is concern for channelopathy based on family history. Some literature does suggest possible benefits of a benzodiazepine in conjunction with phenobarbital for seizure cessation, but care should be given due to high risk for respiratory suppression in neonates.
For seizures that are unresponsive to first line treatment, consider phenytoin, levetiracetam, midazolam, or lidocaine.
A trial of pyridoxine can be attempted in patients who are unresponsive to initial measures
Evaluation:
Neonatal seizures require a full evaluation, including labs, head imaging (MRI preferred), low threshold for LP post imaging, concern for trauma
Disposition:
Neonates presenting with seizures require admission to the hospital for ongoing evaluation and monitoring.
Pressler RM, Abend NS, Auvin S, Boylan G, Brigo F, Cilio MR, De Vries LS, Elia M, Espeche A, Hahn CD, Inder T, Jette N, Kakooza-Mwesige A, Mader S, Mizrahi EM, Moshé SL, Nagarajan L, Noyman I, Nunes ML, Samia P, Shany E, Shellhaas RA, Subota A, Triki CC, Tsuchida T, Vinayan KP, Wilmshurst JM, Yozawitz EG, Hartmann H. Treatment of seizures in the neonate: Guidelines and consensus-based recommendations-Special report from the ILAE Task Force on Neonatal Seizures. Epilepsia. 2023 Oct;64(10):2550-2570. doi: 10.1111/epi.17745. Epub 2023 Sep 1. PMID: 37655702.
Category: Critical Care
Keywords: cardiac arrest, ACLS, IV access (PubMed Search)
Posted: 11/5/2024 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
In out of hospital cardiac arrest (OHCA), does it matter if you choose an intraosseous (IO) vs intravenous (IV) approach to getting access and giving meds?
No, according to a recent study by Couper et al, just published in NEJM. No significant difference in any clinically meaningful outcome including survival, neurologically intact discharge, etc. Technically the IV group had slightly higher rates of ROSC, which just met statistical significance, and to be fair that group did trend very slightly towards better outcomes in some categories, but really well within the range expected by statistical noise.
Interestingly, the median time from EMS arrival to access being established was the same in both groups (12 minutes), which I think raises some face validity questions. Furthermore, of course, previous trials have raised questions as to whether ACLS meds even work or impact outcomes anyways, so naturally if they don't, the method by which they are given isn't likely to matter either.
Bottom Line: This large, well conducted trial continues to support the notion that either an IV-focused, or IO-focused approach to access and medication delivery in OHCA is reasonable. You and your prehospital colleagues can likely continue to make this decision based on personal comfort, local protocols, and patient/case circumstances. At the very least, this continues to support the notion that if an IV is proving challenging, pursuing an IO instead is a very appropriate thing to do.
Couper K, Ji C, Deakin CD, Fothergill RT, Nolan JP, Long JB, Mason JM, Michelet F, Norman C, Nwankwo H, Quinn T, Slowther AM, Smyth MA, Starr KR, Walker A, Wood S, Bell S, Bradley G, Brown M, Brown S, Burrow E, Charlton K, Claxton Dip A, Dra'gon V, Evans C, Falloon J, Foster T, Kearney J, Lang N, Limmer M, Mellett-Smith A, Miller J, Mills C, Osborne R, Rees N, Spaight RES, Squires GL, Tibbetts B, Waddington M, Whitley GA, Wiles JV, Williams J, Wiltshire S, Wright A, Lall R, Perkins GD; PARAMEDIC-3 Collaborators. A Randomized Trial of Drug Route in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2024 Oct 31:10.1056/NEJMoa2407780. doi: 10.1056/NEJMoa2407780. Epub ahead of print. PMID: 39480216; PMCID: PMC7616768.
Category: Ultrasound
Keywords: POCUS; ocular; neurology (PubMed Search)
Posted: 11/4/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
If significant orbital edema prevents visual assessment of the pupillary light reflex, ocular ultrasound can be a useful alternative.
Ocular Ultrasound Made Easy: Step-By-Step Guide - POCUS 101
Ramamoorthy T, Manu Ayyan S, Deb AK. Diagnostic Value of Point-of-Care Ultrasound-Guided Assessment of Relative Afferent Pupillary Defect in Adult Ocular Trauma Patients Presenting to the Emergency Department: A Prospective Cohort Study. J Ultrasound Med. 2024 Jul;43(7):1343-1351. doi: 10.1002/jum.16458.
Category: Trauma
Keywords: Repeat, gun violence, Black, revictimization (PubMed Search)
Posted: 11/2/2024 by Robert Flint, MD
(Updated: 11/3/2024)
Click here to contact Robert Flint, MD
This study used the New York State hospital discharge database to look for factors associated with being the victim of repeat gun violence.
Unanswered questions include: is it similar in other areas, what interventions at the patient level could prevent this, what other patient level factors (substance use, etc) are involved, however, this is a good start in looking at this preventable disease.
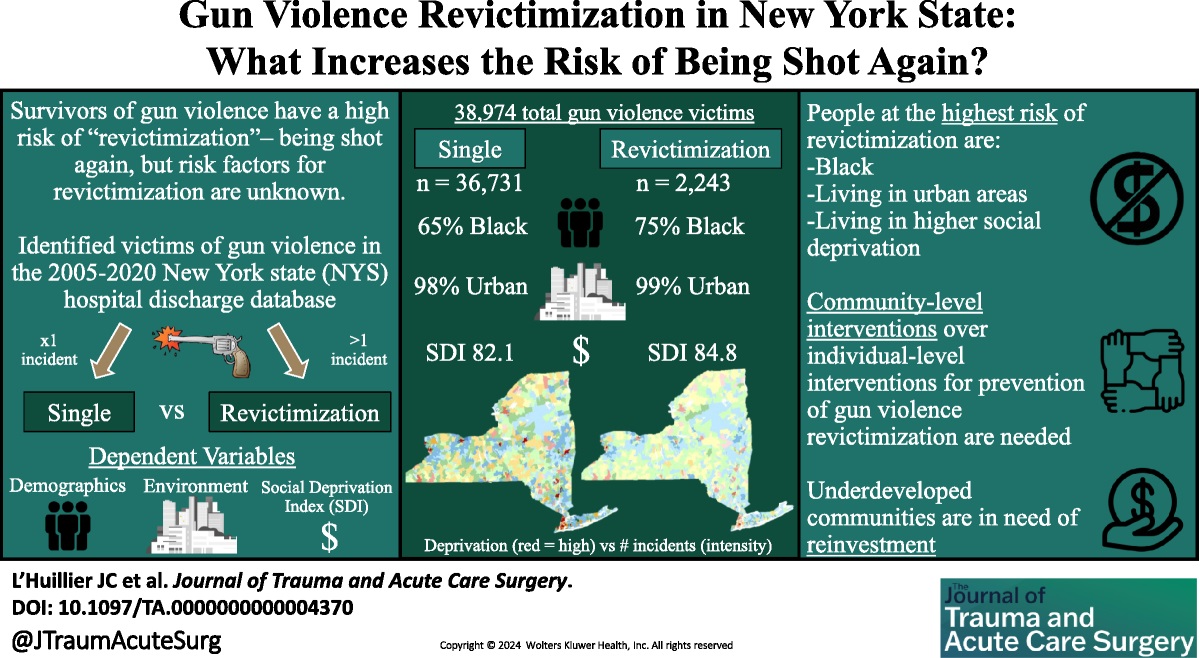
L’Huillier, Joseph C. MD; Boccardo, Joseph D. MS; Stewart, Morgan MUP; Wang, Suiyuan MS; Myneni, Ajay A. MBBS, PhD, MPH; Bari, ASM Abdul MUP; Nitsche, Lindsay J. BS; Taylor, Henry L. Jr PhD; Lukan, James MD, FACS; Noyes, Katia PhD, MPH
Journal of Trauma and Acute Care Surgery 97(4):p 604-613, October 2024. | DOI: 10.1097/TA.0000000000004370
Category: Trauma
Keywords: Adolescent, screening, alcohol, substance use (PubMed Search)
Posted: 11/2/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Recent studies continue to highlight that Black, Native American, female, uninsured and Medicaid patients receive disproportionately more substance use screening when they are trauma patients. The authors of this paper point out that this inappropriate application of screening leads to missed opportunities.
“Screening patients for drug and alcohol use following injury is an evidence-based practice that can trigger wraparound care, such as brief substance use interventions, to prevent reinjury. Adolescents who consume alcohol but are not screened for alcohol use have 2- to 3- fold greater likelihood of reinjury compared with those who were screened and received a brief intervention.”
Sanchez JE, Stey AM. Persistent Inequity Plaguing Pediatric Trauma—An Opportunity for Health Equity Framework. _JAMA Netw Open._2024;7(10):e2436308. doi:10.1001/jamanetworkopen.2024.36308
Category: Infectious Disease
Keywords: avian, influenza, infectious (PubMed Search)
Posted: 10/31/2024 by Visiting Speaker
(Updated: 2/8/2026)
Click here to contact Visiting Speaker
By Bobbi-Jo Lowie, MD
Assistant Professor
Emergency Medicine
University of Maryland School of Medicine
Since April of 2024 there have been 36 confirmed cases of avian influenza A across the United States. Avian influenza, primarily caused by influenza viruses that infect birds, can pose significant health risks to both animals and humans. The most notable strains include H5N1 and H7N9, with H5N1 being particularly alarming due to its high mortality rate among infected humans. The virus primarily spreads from birds to humans through direct contact with infected birds, their droppings, or contaminated environments. Although there have been recorded cases of human-to-human transmission, this usually occurs only in close-contact situations.
In humans, avian influenza can present with symptoms ranging from mild respiratory illness to severe pneumonia. Patients may experience fever, cough, sore throat, muscle aches, and in severe cases, gastrointestinal symptoms. Those that have more moderate or severe illness may develop shortness of breath, altered mental status, or seizures. Complications include acute respiratory failure, pulmonary hemorrhage among others, with respiratory failure being the most common cause of death in this patient population.
Diagnosing avian influenza involves a combination of clinical presentation, travel history, and exposure to birds and confirmation through PCR testing of upper respiratory tract samples like a nasopharyngeal swab.
Treatment for avian influenza focuses on antiviral medications such as oseltamivir which is most effective when administered early in the course of the illness but still administered after 48 hours of illness. Supportive care is essential for managing severe cases, especially those that progress to acute respiratory distress syndrome.
Category: Cardiology
Keywords: Hypertension, emergency, asymptomatic (PubMed Search)
Posted: 10/30/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
Hypertension in the ED comes in two varieties: emergency and asymptomatic (not urgency!). From this position statement: “Hypertensive emergency involves acute target-organ damage and should be treated swiftly, usually with intravenous antihypertensive medications, in a closely monitored setting.”
Conversely, asymptomatic does not require urgent, aggressive management. “Recent observational studies have suggested potential harms associated with treating asymptomatic elevated inpatient BP, which brings current practice into question.”
Without target organ involvement, we do not need to be initiating IV medications or trying to treat the numbers
Bress AP, Anderson TS, Flack JM, Ghazi L, Hall ME, Laffer CL, Still CH, Taler SJ, Zachrison KS, Chang TI; American Heart Association Council on Hypertension; Council on Cardiovascular and Stroke Nursing; and Council on Clinical Cardiology. The Management of Elevated Blood Pressure in the Acute Care Setting: A Scientific Statement From the American Heart Association. Hypertension. 2024 Aug;81(8):e94-e106. doi: 10.1161/HYP.0000000000000238. Epub 2024 May 28. PMID: 38804130.
Category: Hematology/Oncology
Posted: 10/28/2024 by Sarah Dubbs, MD
(Updated: 2/8/2026)
Click here to contact Sarah Dubbs, MD
Cardiovascular disease (CVD) and cancer are leading global causes of illness and death, and evidence increasingly shows they are interconnected. There is strong epidemiological data that the two disease entities share modifiable risk factors such as hypertension, hyperlipidemia, diabetes, obesity, smoking, diet, physical activity, and social determinants of health.
Shared mechanisms underlying both CVD and cancer include:
Take home points:
Keep all this in mind especially when seeing cancer and CVD patients in your ED!
Wilcox NS, Amit U, Reibel JB, Berlin E, Howell K, Ky B. Cardiovascular disease and cancer: shared risk factors and mechanisms. Nat Rev Cardiol. 2024 Sep;21(9):617-631. doi: 10.1038/s41569-024-01017-x. Epub 2024 Apr 10. PMID: 38600368; PMCID: PMC11324377.
Koene RJ, Prizment AE, Blaes A, Konety SH. Shared Risk Factors in Cardiovascular Disease and Cancer. Circulation. 2016 Mar 15;133(11):1104-14. doi: 10.1161/CIRCULATIONAHA.115.020406. PMID: 26976915; PMCID: PMC4800750.
Category: Trauma
Keywords: Cryopercipitate, mass transfusion hemorrhage (PubMed Search)
Posted: 10/27/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
There is uncertainty if adding cryopercipitate empirically to all mass hemorrhage protocols has any benefit to mortality, need for transfusion, or any other meaningful outcome. This small study suggests it does not and that we should save the addition of cryopercipitate to those with lab proven low fibrinogen levels.
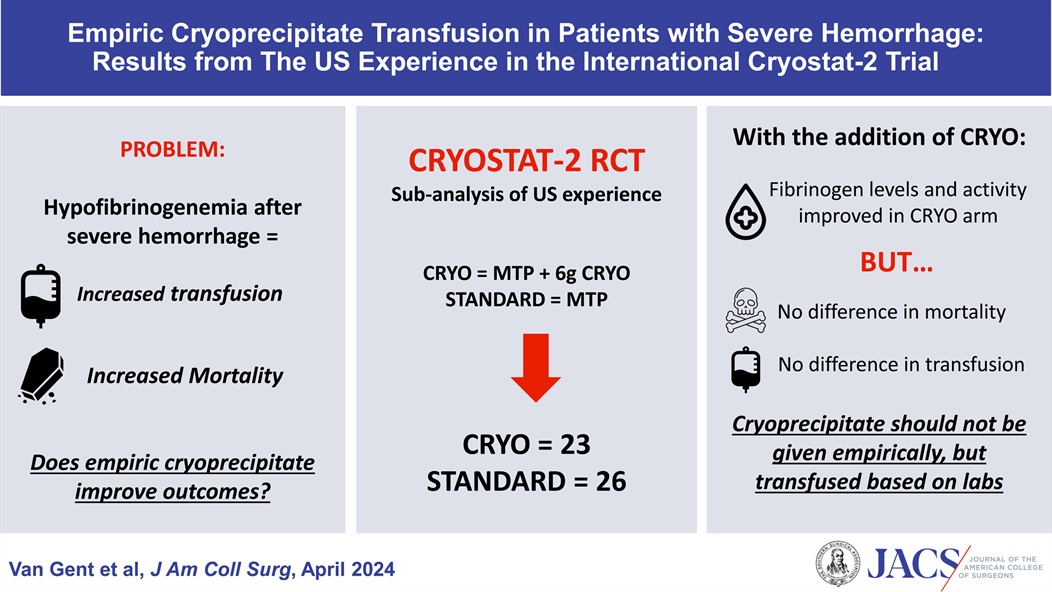
Van Gent, Jan-Michael DO, FACS; Kaminski, Carter W DO; Praestholm, Caroline BS; Pivalizza, Evan G MD; Clements, Thomas W MD; Kao, Lillian S MD, MS, FACS; Stanworth, Simon MD; Brohi, Karim MD; Cotton, Bryan A MD, MPH, FACS
Journal of the American College of Surgeons 238(4):p 636-643, April 2024. | DOI: 10.1097/XCS.0000000000000938
Category: Orthopedics
Posted: 10/26/2024 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Olecranon bursitis
Superficial synovial membrane located overlying the proximal ulna/olecranon allows for easy irritation and inflammation
Swelling does not involve the joint
Most common bursitis (approx. 4x more common than prepatellar)
Male>>Female
Prone to trauma, inflammation or infection
-RA, gout, overlying break in skin
Chronic inflammation results from excessive leaning on the elbow such as with certain occupations (plumber, military recruit)
Inflammation may be septic or aseptic
Usual cause is traumatic
Approximately 20% of acute cases may have a septic origin
Classically appears as a “goose egg” area on posterior elbow
Well-demarcated and fluctuant
Small amount of swelling and/or those with minimal symptoms should be left alone and treated with activity modification, NSAIDS, ice. Suggest an elbow pad for protection.
If this does not resolve symptoms after approximately 4 weeks, consider referral for aspiration and steroid injection
If aspiration is ED performed for evaluation of possible septic bursitis, recommend a compressive elbow sleeve to help prevent reaccumulating
If a recurrent issue for patient and aspirated, consider a posterior elbow splint for approx. 10 days and refer to orthopedics.
Category: Trauma
Keywords: Neck trauma (PubMed Search)
Posted: 10/24/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
For penetrating neck trauma:
Does it violate the platysma if no, close wound and discharge
If yes, are there any hard signs of injury like enlarging hematoma, air from the wound, difficulty swallowing, blood in the airway, respiratory distress then to the OR
If no, Ct angio of the neck. If negative and no other findings admit for observation or discharge. If positive, to the OR. If equivocal, endoscopy and broncoscopy.
No longer think about the zones of the neck. Treat them all the same.

