Category: Trauma
Keywords: Fall, EMS, injury prevention (PubMed Search)
Posted: 9/30/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This meta analysis looked for studies involving community EMS (CEMS) interventions trying to reduce falls. The authors found:
“CEMS fall prevention interventions reduced all-cause and fall-related emergency department encounters, subsequent falls and EMS calls for lift assist. These interventions also improved patient health-related quality of life, independence with activities of daily living, and secondary health outcomes.”
Further, prospective work needs to be done to look at this on a larger scale. We know falls in elderly patients lead to significant morbidity and mortality. This could be one way to improve fall mortality.
Friend TH, Thomas HM, Ordoobadi AJ_, et al_
Community emergency medical services approaches to fall prevention: a systematic review
Injury Prevention Published Online First:22 July 2024. doi: 10.1136/ip-2023-045110
Category: Orthopedics
Posted: 9/28/2024 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
A northeast university was recently in the news when several members of the lacrosse team were hospitalized with rhabdomyolysis. 9 of 50 players who participated in the workout required hospitalization. This occurred after a single intense 45-minute workout led by an alum and recent graduate of the Navy Seal training program.
It was surprising to many that young, fit, athletes would be so affected from a single workout.
Nontraumatic exertional rhabdomyolysis occurs following intense physical activity especially in untrained individuals or those unaccustomed to the particular activity (for example a group of runners performing an intense HIIT workout).
Prolonged strenuous activity can result in rhabdomyolysis even in trained individuals in the absence of known risk factors or prior history.
Increased risk when natural cooling mechanisms are affected such as when the individual is taking medications with anticholinergic properties, or the individual is wearing heavy military gear or football equipment.
Increased risk with sickle cell trait.
Increased risk when that activity is performed in environments of severe heat and humidity.
Exercise routines that have a heavy eccentric focus increases risk of rhabdomyolysis.
An Eccentric exercise involves slow lengthening of muscles under load
Examples: the lowering phase of a barbell while performing a bench press or the downward phase of a pull up
Helpful kinetics:
Following the exertional event, the serum CK will rise within 2-12 hours, reaching its maximum in 1-3 days.
CK has a serum half-life of approximately 36 hours.
CK levels decrease at approximately 40% per day.
Category: Administration
Keywords: design, workspace, handoff, interruptions, collaboration (PubMed Search)
Posted: 9/21/2024 by Mercedes Torres, MD
(Updated: 9/25/2024)
Click here to contact Mercedes Torres, MD
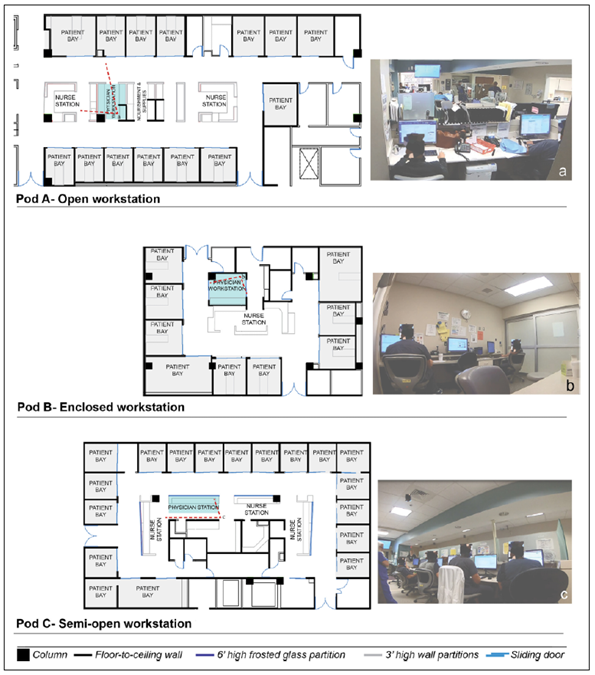
Joshi R, Joseph A, Ossmann M, et al. Emergency Physicians’ Workstation Design: An Observational Study of Interruptions and Perception of Collaboration During Shift-End Handoffs. HERD: Health Environments Research & Design Journal. 2021;14(4):174-193. doi:10.1177/19375867211001379
Category: Critical Care
Posted: 9/24/2024 by Caleb Chan, MD
(Updated: 2/8/2026)
Click here to contact Caleb Chan, MD
Some points from this narrative review:
Take home pearls:
van Eijk JA, Doeleman LC, Loer SA, Koster RW, van Schuppen H, Schober P. Ventilation during cardiopulmonary resuscitation: A narrative review. Resuscitation. 2024;203:110366.
Category: Hematology/Oncology
Posted: 9/24/2024 by Sarah Dubbs, MD
(Updated: 2/8/2026)
Click here to contact Sarah Dubbs, MD
The FDA approved two cell-based gene therapies for the treatment of Sickle Cell Disease in December, 2023. These therapies show potential to dramatically improve the outcomes and quality of life for patients with SCD. You may soon encounter patients who received one of these treatments in the ER, so here is an intro to what they are:
Casgevy is an FDA-approved gene therapy for sickle cell disease in patients 12 and older with recurrent vaso-occlusive crises. It uses CRISPR/Cas9 genome editing to modify blood stem cells, increasing fetal hemoglobin (HbF) production, which prevents red blood cell sickling.
Lyfgenia, also a gene therapy for sickle cell disease, uses a lentiviral vector to modify stem cells to produce HbAT87Q, a hemoglobin that reduces sickling. Both therapies involve modifying the patient's own stem cells, followed by myeloablative chemotherapy, and are given as a single infusion.
Long-term safety and effectiveness is still being studied. More to come in the future!
Frangoul H, Altshuler D, Cappellini MD, Chen YS, Domm J, Eustace BK, Foell J, de la Fuente J, Grupp S, Handgretinger R, Ho TW, Kattamis A, Kernytsky A, Lekstrom-Himes J, Li AM, Locatelli F, Mapara MY, de Montalembert M, Rondelli D, Sharma A, Sheth S, Soni S, Steinberg MH, Wall D, Yen A, Corbacioglu S. CRISPR-Cas9 Gene Editing for Sickle Cell Disease and ?-Thalassemia. N Engl J Med. 2021 Jan 21;384(3):252-260. doi: 10.1056/NEJMoa2031054. Epub 2020 Dec 5. PMID: 33283989. https://www.nejm.org/doi/10.1056/NEJMoa2031054?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
Interesting read from NPR featuring the first patient to receive this therapy:
Category: Geriatrics
Keywords: Geriatric fever score (PubMed Search)
Posted: 9/22/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This study attempts to validate the use of the Geriatric Fever Score to predict 30 day mortality in patients over age 65 presenting to an emergency department with fever.
The Geriatric Fever Score uses: leukocytosis, severe coma, and thrombocytopenia. One point is award for each abnormality.
Not surprisingly, mortality went up with the higher the score (33%, 42% and 57% for 0,1,2 points)
For me, I’m not discharging anyone with severe coma, leukocytosis or thrombocytopenia in this patient population therefore I’m not sure this scale has much utility for the practicing emergency physician.
Akbari, H., Mirfazaelian, H., Safaei, A. _et al._Predicting mortality in geriatric patients with fever in the emergency departments: a prospective validation study. BMC Geriatr 24, 758 (2024). https://doi.org/10.1186/s12877-024-05346-x
Category: Pediatrics
Keywords: IO, intraosseous, access, tibial, femoral (PubMed Search)
Posted: 9/20/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
This study looked at the success rates of femoral vs proximal tibial IOs in the prehospital setting. Over a 9 year period, there were 163 pediatric patients who received either a tibial or femoral IO. Femoral IOs were introduced into the EMS protocol in this study area in 2015 as a location option and were the recommended site starting in 2019. The success rate of femoral IO placement was 89% and for proximal tibial sites was 84.7%. After further data analysis the study found an adjusted odds ratio of 2 for successful IO placement in the distal femur compared to the proximal tibia. The complication rates for both sites were similar.
Bottom line: This study suggests that the distal femur is a reasonable site for IO access in the pediatric population.
Zitek T, Antevy P, Garay S, Thorn M, Buckley E, Coyle C, Scheppke KA, Farcy DA. Evaluating the Success Rate of Distal Femur Intraosseous Access Attempts in Pediatric Patients in the Prehospital Setting: A Retrospective Analysis. Prehosp Emerg Care. 2024 Sep 4:1-8. doi: 10.1080/10903127.2024.2398185. Epub ahead of print. PMID: 39230342.
Category: Trauma
Keywords: seizure, head trauma, levetiracetam (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/19/2024)
Click here to contact Robert Flint, MD
The use of seizure prophylaxes in moderate to severe head injury has been recommended for 7 days post-injury. In general, levetiracetam is used for seizure prophylaxes in this group of patients. This study looked retrospectively at high (over 500 mg BID) vs. low (500 mg bid) dosing and found there was no difference in seizure events in either group. Overall 6% of patients had a seizure in this seven day window even with medication given.
Mann A, Livers K, Frick CD, et al. Evaluation of levetiracetam dosing for seizure prophylaxis in traumatic brain injury. Trauma. 2024;0(0). doi:10.1177/14604086241230598
Category: EMS
Keywords: excited delirium, sedation, intubation (PubMed Search)
Posted: 9/18/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
This study looks at the efficacy of ketamine vs. midazolam for the prehospital sedation of acutely agitated patients, examining the need for repeat sedation (by EMS or in the ED), adverse events and length of stay.
A greater number of patients required repeat sedation within 90 minutes with initial ketamine dosing compared to midazolam. There was no difference in patients receiving repeat sedation within 20 minutes between the two groups.
There were no significant differences in time to repeat sedation, total sedation doses (by EMS or in the ED), use of bag valve mask ventilation or intubation, use of physical restraints, admission location/level of care, or length of stay in the Emergency Department (ED), hospital, or Intensive Care Unit.
Holland D, Glober N, Christopher S, Zahn E, Lardaro T, O'Donnell D. Prehospital sedation with ketamine vs. midazolam: Repeat sedation, intubation, and hospital outcomes. Am J Emerg Med. 2020;38(9):1748-1753. doi:10.1016/j.ajem.2020.05.011
Category: Critical Care
Posted: 9/17/2024 by William Teeter, MD
Click here to contact William Teeter, MD
I wanted to send out two websites curated in part by UMEM current and past faculty/residents/fellows which have a wealth of critical care lectures and resources:
Disclosure: *I am one of the webmasters for the STCMTCC, but have no affiliation with MCCP other than as an enthusiastic reader.
Category: Trauma
Keywords: c-spine, fracture, Burst (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/16/2024)
Click here to contact Robert Flint, MD
Identify this radiographic finding:
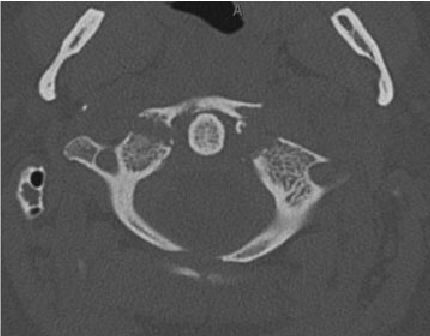
"Jefferson fracture is the eponymous name given to a burst fracture of the atlas. It was originally described as a four-part fracture with double fractures through the anterior and posterior arches, but three-part and two-part fractures have also been described.
50% are associated with other cervical spine injuries
33% are associated with a C2 fracture
25-50% of young children have a concurrent head injury
blunt cerebrovascular injury (BCVI): vertebral artery injury
extracranial cranial nerve injury" 1.
Category: Pharmacology & Therapeutics
Keywords: hyperkalemia, calcium, cardiac conduction, resting membrane potential (PubMed Search)
Posted: 9/11/2024 by Alicia Pycraft
(Updated: 9/12/2024)
Click here to contact Alicia Pycraft
The benefits of calcium treatment for hyperkalemia have historically been attributed to “membrane stabilization,” as it has been hypothesized to restore cardiac resting membrane potential. However, the true mechanism by which calcium improves cardiac function in this setting remains unclear. This has led to inconsistencies in the clinical threshold for treating hyperkalemia with calcium.
Piktel et al. recently conducted an experimental study investigating the adverse electrophysiologic effects of hyperkalemia and therapeutic effects of calcium treatment in isolated canine myocytes using ex vivo tissue and in vivo cellular techniques.
Key study findings:
Effects of hyperkalemia:
Effects of calcium treatment in the setting of hyperkalemia:
Limitation:
Bottom line: Findings of this study suggest that calcium's beneficial effects in hyperkalemia are not attributed to “membrane stabilization,” but rather to restoration of conduction velocity through L-type calcium channels and subsequent narrowing of the QRS complex. This supports calcium treatment in hyperkalemia when the ECG shows conduction slowing and QRS widening.
Piktel JS, Wan X, Kouk S, Laurita KR, wilson LD. Beneficial effect of calcium treatment for hyperkalemia is not due to “membrane stabilization” Crit Care Med. 2024; 52(00): 1-10.
Category: Critical Care
Keywords: RSI, intubation, critical care, out of hospital cardiac arrest (PubMed Search)
Posted: 9/10/2024 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Airway management in the pre-hospital setting is a matter of much controversy, and overall I will defer to my EMS colleagues, but several previous studies have failed to show a benefit to endotracheal intubation in the field as opposed to alternate approaches like a supraglottic airway. Another nod in this direction has recently come out, with Battaglini et al performing a post-hoc analysis of one of the larger studies in the history of cardiac arrest, TTM-2, looking specifically at outcomes stratified by pre-hospital airway management strategy.
Do patients who undergo endotracheal intubation in the field do better than those who get a supraglottic airway?
No, they don't. TTM-2 included 1900 patients, of whom 1702 had enough data to be included in this re-analysis. 28% got supraglottic airways, and 72% got endotracheal intubation. The groups were reasonably well matched on most characteristics, and if anything most well-known prognostic factors favored the endotracheal intubation group (very slightly). It should be noted that several outcome metrics, including modified Rankin scale, did show slight signs of benefit for the endotracheal intubation group, even sometimes in a statistically significant fashion, but fell out when a multi-regression analysis, which was the primary endpoint, was done.
Bottom Line: In pre-hospital cardiac arrest, there remains limited data to support the notion that endotracheal intubation results in better outcomes than supraglottic airway placement. You should defer to your local protocols and continue to work with your paramedics and EMS directors as evidence continues to evolve. For now, I don't think there's sufficient data to suggest that a given patient should be intubated vs undergoing supraglottic airway placement, and it is probably best to defer to the judgement, training, and protocols of your folks on scene.
Battaglini D, Schiavetti I, Ball L, Christian Jakobsen J, Lilja G, Friberg H, David Wendel-Garcia P, Young PJ, Eastwood G, Chew MS, Unden J, Thomas M, Joannidis M, Nichol A, Lundin A, Hollenberg J, Hammond N, Saxena M, Martin A, Solar M, Silvio Taccone F, Dankiewicz J, Nielsen N, Morten Grejs A, Wise MP, Hängghi M, Smid O, Patroniti N, Robba C; TTM2 trial investigators§. Association between Early Airway Intervention in the Pre-Hospital setting and Outcomes in Out of Hospital Cardiac Arrest Patients: a post-hoc analysis of the Target Temperature Management-2 (TTM2) trial. Resuscitation. 2024 Sep 5:110390. doi: 10.1016/j.resuscitation.2024.110390. Epub ahead of print. PMID: 39244144.
Category: Trauma
Keywords: fracture, spine, x-ray (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/9/2024)
Click here to contact Robert Flint, MD
Identify this injury and other associated injuries:
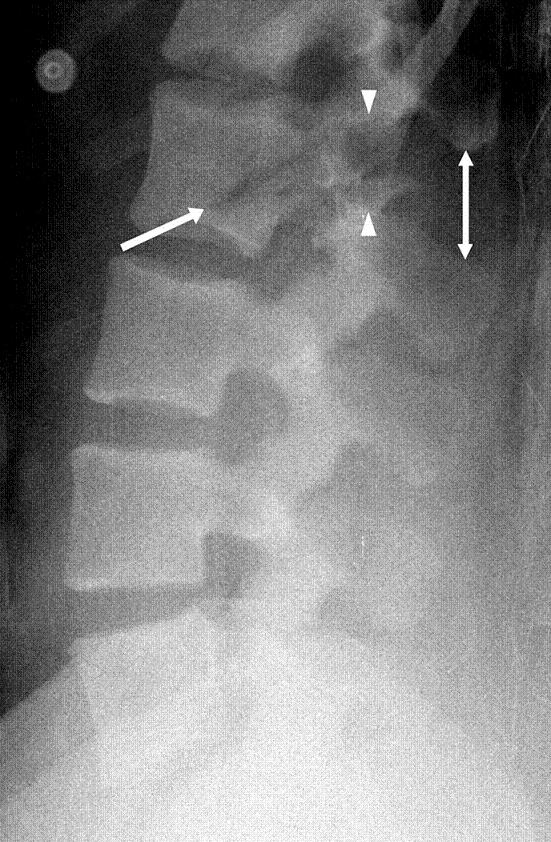
“Chance fractures also referred to as seatbelt fractures, are flexion-distraction type injuries of the spine that extend to involve all three spinal columns. These are unstable injuries and have a high association with intra-abdominal injuries. There is a high incidence of associated intra-abdominal injuries (especially the pancreas, duodenum, and abdominal aorta) that can result in increased morbidity and mortality. Associated intra-abdominal injuries appear to be more common in the pediatric age group with an incidence approaching 50%.” 2.
1.Chance Fracture - Medicalopedia
2. Jones J, Kogan J, Vadera S, et al. Chance fracture. Reference article, Radiopaedia.org (Accessed on 06 Sep 2024) https://doi.org/10.53347/rID-10186
Category: Trauma
Keywords: blunt bowel injury, BIPS, prediction, blunt trauma (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/8/2024)
Click here to contact Robert Flint, MD
Predicting which blunt abdominal trauma patients have mesenteric or bowel wall injuries early in their ED course will decrease morbidity and mortality. It is also a challenge even in the age of advanced CT imaging. This study from India looks at the Bowel Injury Prediction Score as a possible means to catch these injuries early in the course of care. The score uses white blood cell count over 17,000 (1 point), abdominal tenderness at the time of presentation(1 point), as well as a McNutt's scoring scale grade 4 (1 point) (table). The study found those with a score greater than 2 (out of 0-3) were much more likely to have bowel or mesenteric injury at time of laparotomy. Tenderness and CT findings were more likely to be predictive of bowel injury than WBC greater than 17,000. “BIPS had 94.5% sensitivity, 72% specificity, 88% PPV, and 86% NPV for identifying patients with sBBMI.”
My take away is an abnormal CT scan or significant tenderness of presentation warrant concern for mesenteric or bowel wall injury and surgical evaluation is appropriate for these patients. An elevated or normal white blood cell count isn't helpful in these patients. Surgeons may use this scale to help them decide if a patient warrants a trip to the operating room
| GRADE | FINDING |
|---|---|
| 1 | Isolated mesenteric contusion without associated bowel wall thickening or adjacent interloop fluid collection |
| 2 | Mesenteric hematoma?<?5 cm without associated bowel wall thickening or adjacent interloop fluid collection |
| 3 | Mesenteric hematoma?>?5 cm without associated bowel wall thickening or adjacent interloop fluid collection |
| 4 | Mesenteric contusion or hematoma (any size) with associated bowel wall thickening or adjacent interloop fluid collection |
| 5 | Active vascular or oral contrast extravasation bowel transaction or pneumoperitoneum |
Gupta SK, Singh PK, Sharma S, Gupta SK. Prospective validation of Bowel Injury Prediction Score for early diagnosis of surgically significant blunt bowel and mesenteric injury. Trauma. 2023;0(0). doi:10.1177/14604086231187523
Category: Med-Legal
Keywords: adverse event, vital signs, tachycardia, hypotension (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/7/2024)
Click here to contact Robert Flint, MD
This review reminds us that discharging emergency department patients with abnormal vital signs is a risk for the patient and the provider. The more abnormal vital signs that are present, the higher the risk of adverse event and subsequent return to the emergency department.
“Hypotension at discharge was associated with the highest odds of adverse events after discharge. Tachycardia was also a key predictor of adverse events after discharge and may be easily missed by ED clinicians.”
Always address abnormal vital signs in your medical decision making portion of the chart and be very wary of discharging anyone with tachycardia or other abnormal vital signs.
Can I Discharge This Adult Patient with Abnormal Vital Signs From the Emergency Department?
Long, Brit et al. Journal of Emergency Medicine, Volume 0, Issue 0 Articles in Press May 18, 2024 DOI: 10.1016/j.jemermed.2024.05.009
Category: Pediatrics
Keywords: pediatrics, electrolyte, sodium (PubMed Search)
Posted: 7/5/2024 by Kathleen Stephanos, MD
(Updated: 9/6/2024)
Click here to contact Kathleen Stephanos, MD
Continuing with the electrolyte derangements in children: Hyponatremia
Hyponatremia is defined as a Sodium of less than 135 mmol/L and does not depend on patient age.
This is the most common electrolyte abnormality in pediatric patients. Excessive free water is often the culprit and is usually thought of in the neonate or infant whose guardians are mixing formula incorrectly. * Additional causes include inappropriate ADH (Antidiuretic hormone) secretion, or in the case of dehydrated patients appropriate ADH secretion. Sodium wasting is rare.
Total body water (TBW) is important to consider, and preterm neonates have higher TBW (80%) than full term (70%) and 1 year old infants (~60%) putting them at higher risk of hyponatremia.
Recognizing the volume status of the patient aids in determining the etiology of the hyponatremia and allows for appropriate treatment. This may require obtaining urine sodium.
Treatment:
Hypertonic saline should be used only for patients with severe neurologic complications including seizures or altered mentation. In these patients, a hypertonic saline bolus should be given at 3-5 ml/kg of 3% NaCl over 10-15 minutes.
In hypovolemic patients without neurologic symptoms, fluid resuscitation is the mainstay with caution to increase sodium levels by no more than 6-8mmol/L/day. For euvolemic or hypervolemic patients, fluid restriction is advised.
Prevention:
Importantly, when children receive IV fluids, the choice should be made to select isotonic fluids (0.9% NaCl) rather than hypotonic fluids (0.45% NaCl) to avoid iatrogenic development of hyponatremia.
*Reminder: 2 ounces (about 60 ml) of water should be placed in the bottle, and then 1 full scoop of formula, unless directed to have higher caloric content by their doctor- in which case the amount of formula in the mixture should be higher
Saba L, Hanna C, Creo AL. Updates in hyponatremia and hypernatremia. Curr Opin Pediatr. 2024 Apr 1;36(2):219-227. doi: 10.1097/MOP.0000000000001324. Epub 2024 Jan 4. PMID: 38174733.
Brown DH, Paloian NJ. Hypokalemia/Hyperkalemia and Hyponatremia/Hypernatremia. Pediatr Rev. 2023 Jul 1;44(7):349-362. doi: 10.1542/pir.2021-005119. PMID: 37391630.
Category: Obstetrics & Gynecology
Keywords: Mycoplasma genitalium, PID, cervicitis (PubMed Search)
Posted: 9/5/2024 by Michele Callahan, MD
Click here to contact Michele Callahan, MD
Mycoplasma genitalium (M.genitalium, or Mgen) is a pathogen that is increasingly associated with cervicitis, pelvic inflammatory disease, preterm labor, spontaneous abortion, and infertility. Although many are asymptomatic, M.genitalium can be found in 10-30% of women with symptoms/exam findings of cervicitis.
NAAT testing for M.genitalium is FDA-approved for use with urine and urethral, penile meatal, endocervical, and vaginal swab samples.
According to CDC guidelines, women with recurrent or persistent cervicitis should be tested for M.genitalium, and testing should be considered among women with PID. It is not recommended to test for asymptomatic infections at this time, even in pregnancy.
High rates of macrolide resistance in this pathogen make 1 g of Azithromycin insufficient. The recommended regimen for NAAT-positive M.genitalium infections is: Doxycycline 100 mg PO BID x 7 days to reduce bacterial load, followed by moxifloxacin 400 mg PO daily x 7 days.
Overall, more studies are needed to truly determine the clinical relevance of this pathogen.
Consider testing for M.genitalium in patients presenting with recurrent or persistent cervicitis or pelvic inflammatory disease, as this may not respond to typical antibiotic regimens.
https://www.cdc.gov/std/treatment-guidelines/toc.htm
Hufstetler, K., Llata, E., Miele, K., & Quilter, L. A. S. (2024). Clinical Updates in Sexually Transmitted Infections, 2024. Journal of women's health (2002), 33(6), 827–837. https://doi.org/10.1089/jwh.2024.0367
Category: Critical Care
Keywords: OHCA, opioid, opiates, fentanyl, overdose, cardiac arrest (PubMed Search)
Posted: 9/2/2024 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
The incidence of opioid-overdose-related deaths has clearly increased in the past decade, with recent estimates of up to 17% of OHCA being opioid-related in 2023. [1,2] The use of naloxone for opiate reversal in overdose is well-established, with reasonable inference but no formal proof that its use could help in opioid-associated out of hospital cardiac arrest (OA-OHCA). [3] The August publication of two trials [4,5] retrospectively examining naloxone administration in OHCA offers some perspectives…
and
[View “Visual Diagnosis” for slightly more detail on the referenced studies.]
Bottom Line: While prospective trials are absolutely needed to offer more definitive evidence regarding the use of empiric naloxone in nontraumatic OHCA, the rising incidence of OA-OHCA in the U.S. and current findings are convincing enough to encourage early naloxone administration, especially in populations with higher incidence of opioid use.
U.S. Mortality due to Opioid Overdose (CDC data)
Dillon et al, JAMA
Strong et al, Resuscitation
Category: Trauma
Keywords: IPV, violence, injury, ulna, orthopedics (PubMed Search)
Posted: 9/1/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In this systemic literature review of orthopedic injuries identified in intimate partner violence (IPV) the authors remind us that finger, hand, and especially isolated ulnar fractures are very commonly associated with IPV. When we see these injury patterns extra effort is required to determine if IPV is involved.
| Citation | **Bhandari et al.**3 | **Khurana et al.**18 | **Loder et al.**12 | **Porter et al.**13 | **Kavak et al.**7 | **Thomas et al.**17 |
|---|---|---|---|---|---|---|
| Division of injury locations | Fingers, wrist, shoulder dislocation, humerus fracture | Finger, hand, wrist, forearm, elbow, humerus, shoulder | Finger, hand, wrist, forearm, elbow, humerus, shoulder | Radius/ulna, humerus, upper extremity, right/left | Phalanx, radius, ulna (diaphysis/metaphysis, distal/proximal) | Phalanges (distal/medial/proximal), hand/finger, forearm, arm/shoulder right/left |
| Most common UEF location | Fingers (n = 11) | Finger (34.3%) | Finger (9.9%) | Radius and ulna (n = 80; 5.9%) | Ulna (14.5%) | Finger (46%) |
| Most common injury type‡ | Musculoskeletal sprains (all n = 21; 28% back n = 7; neck n = 6) | UEF (27.2%) | Contusions/abrasion (43.4%) | Rib fracture (17.5%) | Soft-tissue lesions (n = 1,007, 82.2%) | UEF (52%) |
* IPV = intimate partner violence, UEF = upper extremity fracture, and UEI = upper extremity injury.
† Summary table demonstrating the location prevalence of UEIs caused by cases of IPV. Fractures were quantified separately from other UEIs in this specific table.
‡ In all included articles the most common injury type was an injury to the head or neck; these are excluded because of the study aim.
Orthopaedic Injury Patterns in Intimate Partner Violence: Defensive Wounds and Fracture PatternsA Systematic Literature Review
Roan Willson, BS Erika Roddy, MDHolly Martinson, PhDCaitlin Farrell Skelton, MPHLisa Taitsman, MD, MPH
The Journal of Bone and Joint Surgery
August 2024; 12 (8): e24.00082
DOI 10.2106/JBJS.RVW.24.00082
