Category: EMS
Keywords: EMS, cardiopulmonary resuscitation, CPR, emergency medical services (PubMed Search)
Posted: 8/8/2024 by Ben Lawner, MS, DO
Click here to contact Ben Lawner, MS, DO
BACKGROUND:
Cardiac arrest is time sensitive disease. Despite significant advances in resuscitation technology such as eCPR and mechanical compression devices, early basic life support interventions (specifically bystander CPR) are strongly associated with survival. EMS systems must advocate for early initiation of bystander CPR. Dispatch Assisted CPR (DA-CPR) is one of several strategies designed to improve outcomes and encourage early compressions. To optimize survival, EMS systems should achieve a comprehensive understanding about barriers to succesful initiation of DA-CPR.
METHODS AND OUTCOMES:
49,165 patients with out of hospital cardiac arrest were eligible for inclusion the study, and over 36,000 underwent successful DA-CPR. The study's primary outcome was good neurological recovery at hospital discharge. Secondary outcomes included: prehospital return of spontaneous circulation (ROSC)and survival to hospital discharge. The authors defined successful DA-CPR when bystanders initiated compressions and continued resuscitation until the arrival of EMS.
RESULTS:
Quite a few results were consistent with prior studies. Unsuccessful DA-CPR was associated with:
Successful DA-CPR was more likely associated with the presence of family members at the scene and improved neurological recovery. Witnessed arrests were also more likely to receive successful DA-CPR. Not surpringly, patients in the successful DA-CPR group also exhibited improved survival to discharge and prehospital ROSC.
BOTTOM LINE:
Though the study is retrospective and involves a host of confounding variables, EMS systems continue to identify modifiable factors linked to the delivery of DA-CPR. Improved community CPR education and dispatcher training may contribute to higher DA-CPR rates.
BALTIMORE, MD, SPECIFIC PEARL:
Baltimore metropolitan jurisdictions are collaborating with the CPR LifeLinks program to address DA-CPR. The CPR LifeLinks program a national initiative “to help communities save more lives through implementation of telecommunicator and high performance CPR programs." https://www.911.gov/projects/cpr-lifelinks/
Park DH, Park GJ, Kim YM, Chai HS, Kim SC, Kim H, Lee SW. Barriers to successful dispatcher-assisted cardiopulmonary resuscitation in out-of-hospital cardiac arrest in Korea. Resusc Plus. 2024 Jul 19;19:100725. doi: 10.1016/j.resplu.2024.100725. PMID: 39091585; PMCID: PMC1129358
Category: Critical Care
Keywords: meropenem, continuous administration, critically ill (PubMed Search)
Posted: 8/6/2024 by Quincy Tran, MD, PhD
(Updated: 2/8/2026)
Click here to contact Quincy Tran, MD, PhD
We heard it before. Continuous administration of antibiotics might be associated with better outcomes. However, results from smaller randomized controlled trials of beta-lactam showed inconsistent conclusions. Therefore, a large RCT was conducted
Settings: 31 ICUs in Croatia, Italy, Kazakhstan, Russia between June 2018 – August 2022.
Randomized, double-blind control trial.
Participants:
Outcome measurement:
Study Results:
Discussion:
Conclusion:
In critically ill patients with sepsis, continuous administration of meropenem did not improve mortality nor reduce the emergence of pandrug resistant bacteria.
Monti G, Bradic N, Marzaroli M, Konkayev A, Fominskiy E, Kotani Y, Likhvantsev VV, Momesso E, Nogtev P, Lobreglio R, Redkin I, Toffoletto F, Bruni A, Baiardo Redaelli M, D'Andrea N, Paternoster G, Scandroglio AM, Gallicchio F, Ballestra M, Calabrò MG, Cotoia A, Perone R, Cuffaro R, Montrucchio G, Pota V, Ananiadou S, Lembo R, Musu M, Rauch S, Galbiati C, Pinelli F, Pasin L, Guarracino F, Santarpino G, Agrò FE, Bove T, Corradi F, Forfori F, Longhini F, Cecconi M, Landoni G, Bellomo R, Zangrillo A; MERCY Investigators. Continuous vs Intermittent Meropenem Administration in Critically Ill Patients With Sepsis: The MERCY Randomized Clinical Trial. JAMA. 2023 Jul 11;330(2):141-151. doi: 10.1001/jama.2023.10598. PMID: 37326473; PMCID: PMC10276329.
Category: Ultrasound
Keywords: POCUS, Trauma, Cardiac Tamponade, Pericardial Effusion, FAST exam (PubMed Search)
Posted: 8/5/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
In a critically ill trauma patient, the FAST exam is used to evaluate for potential internal injuries. Specifically, the subxiphoid view of the FAST exam helps assess for signs of pericardial tamponade. However, distinguishing between a pericardial effusion and an epicardial fat pad can be challenging.
One study indicated that the sensitivity of EPs in differentiating between effusion and fat pad was 73%, with a specificity of 44% when reviewing difficult patient video clips.
Here are some tips to help you distinguish between effusion and fat pad:
Change your view: Use the parasternal long axis view, which is more sensitive for effusion. Fat pads are usually anteriorly, and effusions tend to accumulate posteriorly in a supine patient.
Screen for other signs of tamponade: Adjust your subxiphoid view to visualize the IVC entering the right atrium, allowing better visualization of the right side of the heart.
Movement: Fat tends to move synchronously with the heart, whereas hemopericardium moves independently.
Echogenicity: Fat typically appears brighter on ultrasound, while blood tends to be less echogenic.
For further learning, refer to the supplemental Material from the referenced articles.
Bronshteyn YS, Hashmi N, Privratsky JR, Barbeito A. Blood or Fat? Differentiating Hemopericardium versus Epicardial Fat Using Focused Cardiac Ultrasound. Diagnostics (Basel). 2024 Apr 15;14(8):818. doi: 10.3390/diagnostics14080818. PMID: 38667464
Blaivas M, DeBehnke D, Phelan MB. Potential errors in the diagnosis of pericardial effusion on trauma ultrasound for penetrating injuries. Acad Emerg Med. 2000 Nov;7(11):1261-6. doi: 10.1111/j.1553-2712.2000.tb00472.x
Category: Cardiology
Keywords: Hypertension, treatment, asymptomatic (PubMed Search)
Posted: 8/4/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This article from JAMA is targeted at inpatient management of asymptomatic hypertension, however, it’s a great reminder that “hypertensive urgency” is not an entity. We should be treating the patient and not the numbers. Gradual, out patient lowering of asymptomatic hypertension is the safe and proper way to approach this. Spread the word to your friends in primary care, urgent care, dental, and other office based practices.
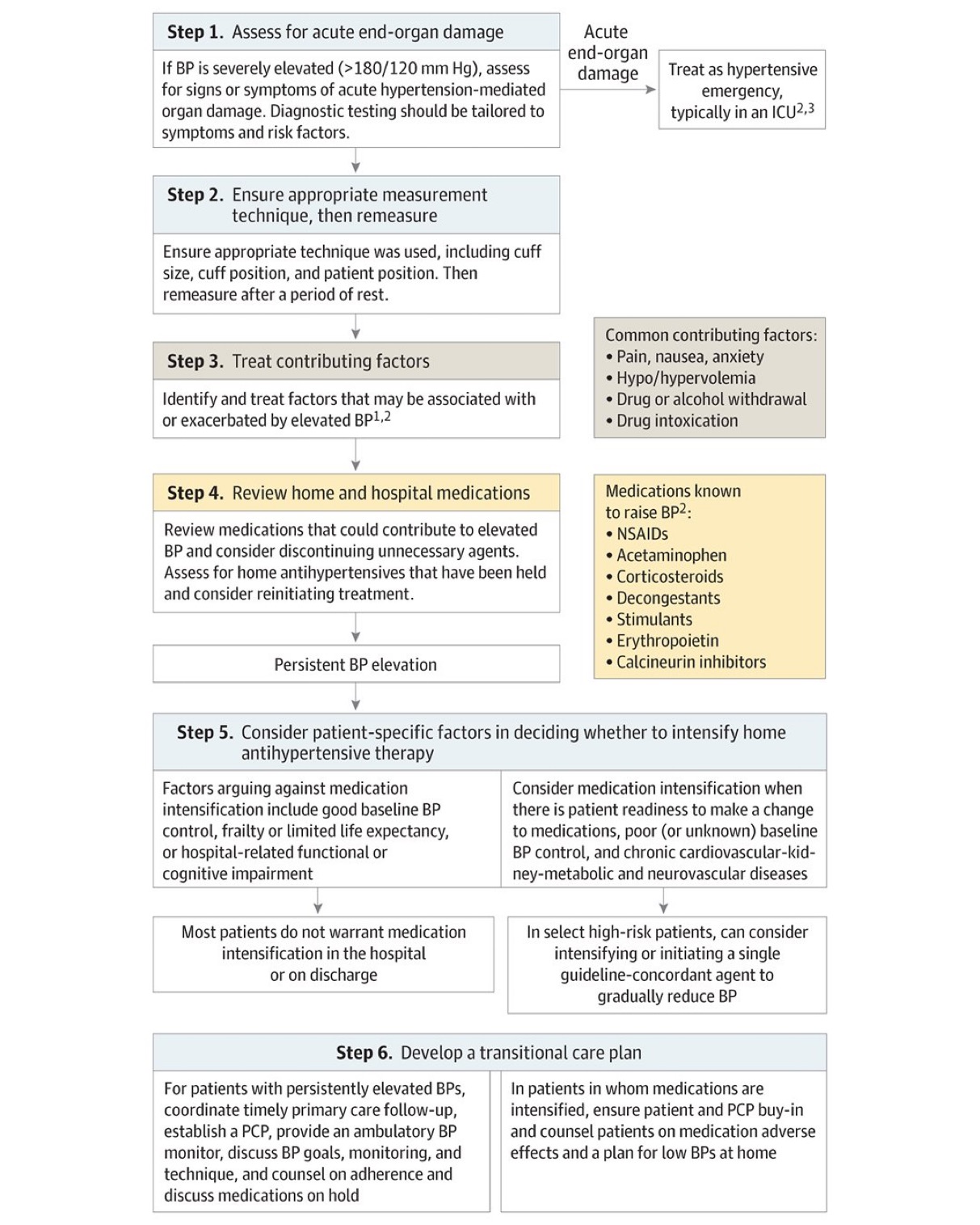
Jacobs ZG, Anderson TS. Management of Elevated Blood Pressure in the Hospital—Rethinking Current Practice. JAMA Intern Med. Published online July 22, 2024. doi:10.1001/jamainternmed.2024.3279
Category: Geriatrics
Keywords: Geriatrics, high risk medications, pharmacy (PubMed Search)
Posted: 8/3/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This article serves as a great reminder that our older patients are on a significant amount of medications and many of these medications effect cognition. Cognitively impaired patients are at risk of medication errors. High risk medications in older patients include anticoagulants, opioids, anticholinergics, hypoglycemic/insulin and sedating medications. The authors found:
It is important to ask how the patient takes (or doesn’t take) their medications as well as other social determinate of health such as living alone.
Journal of the American Geriatrics SocietyEarly View
CLINICAL INVESTIGATION
High-risk medication use among older adults with cognitive impairment living alone in the United States
Matthew E. Growdon MD, MPH, Bocheng Jing MS, Kristine Yaffe MD, Leah S. Karliner MD, MAS, Katherine L. Possin PhD, Elena Portacolone MBA, MPH, PhD, W. John Boscardin PhD, Krista L. Harrison PhD, Michael A. Steinman MD
First published: 26 July 2024
Category: Pediatrics
Keywords: pediatrics, electrolyte, potassium (PubMed Search)
Posted: 7/5/2024 by Kathleen Stephanos, MD
(Updated: 8/2/2024)
Click here to contact Kathleen Stephanos, MD
Hyperkalemia is less common than hypokalemia in pediatric patients, though it is not uncommon to have hemolysis in patients who receive heel stick lab work.
The age of the patient is critical to determining the cutoff for hyperkalemia:
Typically, levels up 6.0mmol/L are well tolerated in children, unless the shift is rapid. For any child meeting age related hyperkalemia or who have a known lower prior potassium level should receive an ECG.
Treatment for hyperkalemia is similar to adults
Calcium Chloride (20mmg/kg - Max 1g) or Calcium Gluconate (0.5ml/kg - Max 20ml) is given for cardiac stability.
Albuterol can be given based on weight
Insulin and dextrose can be used with extreme caution and close monitoring for hypoglycemia. (Dextrose should be given as D10% in children under 5 years of age, D25% can be used if > 5 years old)
Brown DH, Paloian NJ. Hypokalemia/Hyperkalemia and Hyponatremia/Hypernatremia. Pediatr Rev. 2023 Jul 1;44(7):349-362. doi: 10.1542/pir.2021-005119. PMID: 37391630.
Category: Obstetrics & Gynecology
Keywords: mastitis, breastfeeding, lactation (PubMed Search)
Posted: 8/1/2024 by Michele Callahan, MD
(Updated: 2/8/2026)
Click here to contact Michele Callahan, MD
Lactational mastitis (inflammation of the breast in individuals who are lactating) affects up to 20% of breastfeeding individuals. It is characterized by localized breast pain with erythema, edema, and systemic symptoms such as fever/chills and malaise. Supportive treatment measures include the use of NSAIDS, heat and/or ice, and continued feeding or emptying of the breast (stagnant milk can allow for progression of infection). If there is no response to supportive measures within 24 hours, pursuing antibiotic therapy is appropriate. Staphylococcus and Streptococcus species are common organisms responsible for bacterial mastitis; first-line treatment options include Dicloxacillin 500 mg QID or Cephalexin 500 mg QID for 10-14 days. If there is a concern for MRSA, Clindamycin or Bactrim may be used but are considered second-line. Bactrim should be avoided in breastfeeding individuals with infants <1 month or infants who are jaundiced or premature.
Complications of mastitis can include early termination of breastfeeding, breast abscess, and systemic infection if untreated. Ultrasound can be used to assess for breast abscess in patients who do not respond appropriately to antibiotics.
Louis-Jacques AF, Berwick M, Mitchell KB. Risk Factors, Symptoms, and Treatment of Lactational Mastitis. JAMA. 2023;329(7):588–589. doi:10.1001/jama.2023.0004
Academy of Breastfeeding Medicine Clinical Protocol #36: The Mastitis Spectrum, Revised 2022
Katrina B. Mitchell, Helen M. Johnson, Juan Miguel Rodríguez, Anne Eglash, Charlotte Scherzinger, Kyle Widmer, Pamela Berens, Brooke Miller, and the Academy of Breastfeeding Medicine. Breastfeeding Medicine 2022 17:5, 360-376
Category: Trauma
Keywords: Pneumothorax, chest X-ray, 38 mm, observation (PubMed Search)
Posted: 7/29/2024 by Robert Flint, MD
(Updated: 7/31/2024)
Click here to contact Robert Flint, MD
A cut-off of 35mm on CT scan has been shown to be predictive of which traumatic pneumothoracies require thoracostomy tube placement vs. safety of observation. This retrospective study looked at chest X-ray findings to see if there was a similar size cut-off where patients could be safely observed rather than undergo this invasive procedure. They found 38mm was the size over which observation failed. Of note, lactic acidosis and need for supplemental oxygen also predicted the need for chest tube placement
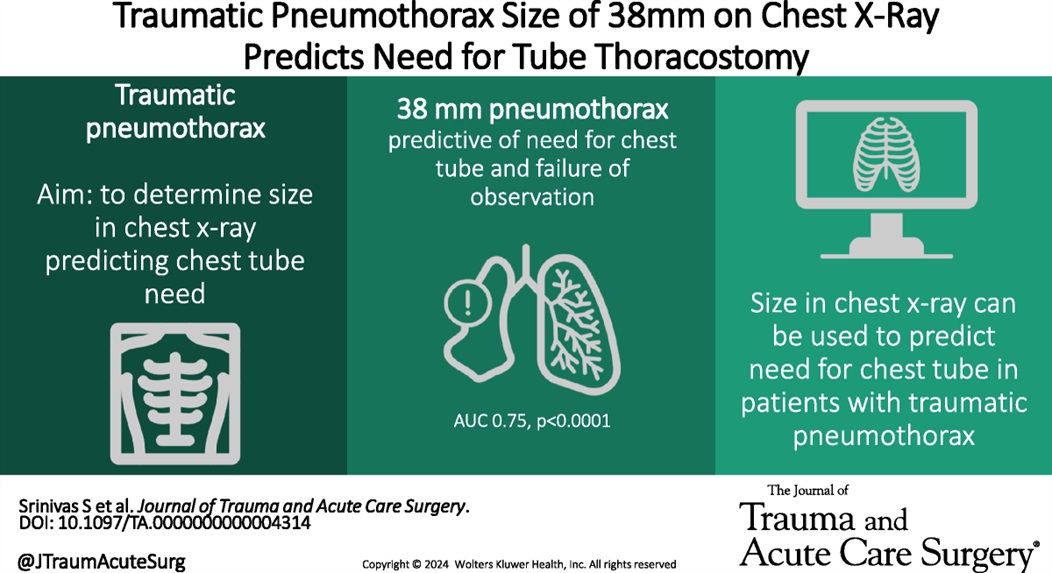
Using chest X-ray to predict tube thoracostomy in traumatic pneumothorax: A single-institution retrospective review
Srinivas, Shruthi MD; Henderson, Katelyn BS; Bergus, Katherine C. MD; Jacobs, Ayanna MD; Baselice, Holly MPH; Donnelly, Edwin MD, PhD; Valdez, Carrie MD; Tracy, Brett M. MD; Coleman, Julia R. MD, MPH
Journal of Trauma and Acute Care Surgery 97(1):p 82-89, July 2024. | DOI: 10.1097/TA.0000000000004314
Category: Ultrasound
Keywords: POCUS, dvt, vascular (PubMed Search)
Posted: 7/29/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
POCUS for DVT is a tricky examination.
Exam of positive study on transverse:
Longitudinal Image showing clot:

Category: Trauma
Keywords: TBI, hypotension, vasopressors (PubMed Search)
Posted: 7/29/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
In this prospective, observational study of trauma patients with isolated head trauma, 62% of patients developed post-intubation hypotension. Comparing patients receiving hypertonic saline, vasopressors, crystalloid, or blood those receiving hypertonic saline and vasopressors had less post-intubation hypotension.
TBI patients who develop hypotension have worse outcomes. This study reminds us the use of vasopressors in trauma patients to maintain blood pressure is appropriate in the correct circumstances.
Anand, Tanya MD, MPH, MT(ASCP); Hejazi, Omar MD; Conant, Madolyn BS; Joule, Dylan BS; Lundy, Megan MD; Colosimo, Christina DO, MS; Spencer, Audrey MD; Nelson, Adam MD; Magnotti, Lou MD; Joseph, Bellal MD
Journal of Trauma and Acute Care Surgery 97(1):p 112-118, July 2024. | DOI: 10.1097/TA.0000000000004306
Category: Infectious Disease
Keywords: Idea, cystitis, aminoglycosides, single dose (PubMed Search)
Posted: 7/27/2024 by Robert Flint, MD
(Updated: 7/28/2024)
Click here to contact Robert Flint, MD
The Infectious Disease Society of America in 2023 recommended a single dose of an aminoglycoside for uncomplicated cystitis treatment in those with resistance or other contraindications to first line oral agents who were otherwise well enough to be discharged. This very small study (13 participants) suggest this strategy works for complicated (“male sex, urinary flow obstruction, renal failure or transplantation, urinary retention, or indwelling catheters”) cystitis patients who could otherwise be discharged home.
Academic Emergency MedicineVolume 31, Issue 7 p. 649-655
Jordan E. Jenrette PharmD, Kyle Coronato PharmD, Matthew A. Miller PharmD, Kyle C. Molina PharmD, Alexander Quinones MD, Gabrielle Jacknin PharmD
First published: 07 March 2024
Category: Orthopedics
Posted: 7/27/2024 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
What is the best provocative test for the diagnosis of carpal tunnel syndrome?
A 2022 study included 37 observational studies to assess the diagnostic accuracy of these provocative maneuvers.
Meta-analysis totaling 2662 wrists of patients with carpal tunnel syndrome.
Surprisingly, the winner was a test that is less familiar to some of us who were taught the traditional tests such as the Phalen test, Tinel test or the carpal tunnel compression test.
Hand elevation has been known to reproduce the symptoms of carpal tunnel syndrome.
The hand elevation test demonstrated the best clinical performance for the diagnosis of carpal tunnel syndrome.
The beauty of the test is that it is as simple to perform as the name suggests.
Have the patient raise their hands above their head for one minute.
Hands are raised actively and without strain, keeping the elbows and shoulders relatively loose. That’s it!
A positive test reproduces the symptoms of carpal tunnel syndrome
The hand elevation test has a high sensitivity (75%-86%) and specificity (89%-98.5%)
Take home: Consider adding this bedside provocative test as the first screening test for patients with suspected carpal tunnel syndrome
Núñez de Arenas-Arroyo S, et al. Accuracy of the Most Common Provocation Tests for Diagnosing Carpal Tunnel Syndrome: A Systematic Review With Meta-analysis. J Orthop Sports Phys Ther. 2022 Aug;52(8):522-531.
Category: Misc
Keywords: sample size calculation, biostatistics (PubMed Search)
Posted: 7/25/2024 by Mike Witting, MS, MD
(Updated: 2/8/2026)
Click here to contact Mike Witting, MS, MD
Free Biostatistics Software Options
EpiCalc 2000 – available for Windows. Capabilities include sample size calculation, inferential statistics (p values, 95% CI), simple stratified analysis, paired and independent analyses. Right clicking allows you to do many things. (http://www.brixtonhealth.com/epicalc.html). I've had the most experience with this one.
Epi Info – supported by CDC. Available for Windows and for hand-held. (https://www.cdc.gov/epiinfo/index.html)
P/S – Power and Sample Size Calculation – available for Mac and Window. Supported by Vanderbilt biostatistics. (https://biostat.app.vumc.org/wiki/Main/PowerSampleSize)
Epicalc: http://www.brixtonhealth.com/epicalc.html
Epi Info: https://www.cdc.gov/epiinfo/index.html
Category: Administration
Keywords: Administration, Meetings, Workforce satisfaction (PubMed Search)
Posted: 7/24/2024 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
Participation in meetings is an expected part of most (if not all) of our jobs. How many of these meetings are necessary? Could some of the “work” of meetings be accomplished with a few emails or other asynchronous forms of communication? Are meetings cluttering your schedule and making it impossible to get any real work done?
Some answers to these questions are offered in a Harvard Business Review article from March 2022.
Key points include:
Advantages to fewer meetings:
Authors recommend holding meetings only when “absolutely” necessary. That typically includes:
Laker B, Pereira V, Malik A, and Soga L. Meeting Management: Dear Manager, You’re Holding Too Many Meetings. Harvard Business Review. March 9, 2022.
Category: Critical Care
Posted: 7/23/2024 by William Teeter, MD
(Updated: 2/8/2026)
Click here to contact William Teeter, MD
Do Sepsis Alert Systems Work?
Researchers in Korea completed a high quality systematic review and meta-analysis of sepsis alert systems for adult ED patients
Using high quality methods, they identified over 3000 studies with 22 meeting criteria.
They found these systems were associated with:
Electronic alerts were further associated with:
Summary (+ a little editorialization)
As annoying as we may find these systems in our daily practice, there is growing evidence that they do provide some benefit with impacts on task saturation and decreasing cognitive load in addition to real patient benefit. While there is also recent evidence that physician gestalt performs well against these systems, there is a suggested benefit in their inclusion in clinical decision making as a safety net or as an “assist”.
The incorporation of rule-based algorithms like these in more advance machine learning methods are covered quite well in a recent opinion piece on “The AI Future of Emergency Medicine”. However, it is important to always know the source of any “algorithm” that you are using, whether rule or mathematically based, given real concerns for bias and error.
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2821277
https://www.sciencedirect.com/science/article/pii/S019606442400043X
https://www.sciencedirect.com/science/article/abs/pii/S0196064424000994
Category: Hematology/Oncology
Keywords: Hematology, Anemia (PubMed Search)
Posted: 7/22/2024 by Sarah Dubbs, MD
Click here to contact Sarah Dubbs, MD
Iron-deficiency anemia affects 10% of women of child-bearing age. Guidelines to treat iron deficiency recommend daily oral iron, but this may decrease fractional iron absorption and increase side effects which also impacts medication adherence. A double-masked, randomized, placebo-controlled trial, which included 150 women demonstrated that:
at equal total iron doses, compared to consecutive day dosing of iron, alternate day dosing did not result in higher serum ferritin but reduced iron deficiency at 6 months and triggered fewer gastrointestinal side effects.
Take home point: Dosing iron every other day had similar effect with less side effects. Consider prescribing it this way to your patients, especially if they have had issues with side effects in the past!
von Siebenthal HK, Gessler S, Vallelian F, Steinwendner J, Kuenzi UM, Moretti D, Zimmermann MB, Stoffel NU. Alternate day versus consecutive day oral iron supplementation in iron-depleted women: a randomized double-blind placebo-controlled study. EClinicalMedicine. 2023 Nov 3;65:102286. doi: 10.1016/j.eclinm.2023.102286. PMID: 38021373; PMCID: PMC10659995.
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(23)00463-7/fulltext
Category: Trauma
Keywords: Txa, TBI, seizure, risk (PubMed Search)
Posted: 7/21/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
According to this study, no TXA 2g bolus was not found to increase the number of seizures in TBI pts.
TXA has been shown to improve mortality in inter cranial hemorrhage trauma patients if given within 2 hours. TXA is also known to lower seizure threshold. This study was a secondary analysis of a larger study comparing placebo to 1 g TXA bolus plus 8 hour infusion or 2g bolus TXA in the prehospital setting. There was no difference in the number of pts experiencing seizure or outcome in those receiving the 2g bolus of TXA.
The Association Between Tranexamic Acid and Seizures in Moderate or Severe Traumatic Brain Injury
David V. Deshpande BS a, W. Ian McKinley MD, MS b, Andrew J. Benjamin MD, MS c, Martin A. Schreiber MD, FACS, FCCM d, Susan E. Rowell MD, MBA, MCR
Volume 301, September 2024, Pages 359-364 https://doi.org/10.1016/j.jss.2024.06.035
Category: Pediatrics
Keywords: mental health, sedation, home medications (PubMed Search)
Posted: 7/19/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Emergency department visits for pediatric mental health and behavioural concerns have been increasing. This study attempted to further characterize medications, both home and for sedation, that were given to these patients.
This study included 670,911 youth with a mental or behavioral health diagnosis over a 9 year inclusion period. The most common diagnses were depressive disorder, suicide or self injury and disruptive, impulse control and conduct disorder. During this time, a total of 12.3% of patients had a psychotropic medication given while in the ED. The percentage and odds of administering these medications increased from 7.9% in 2013 to 16.3% in 2022. Those with intellectual disability and autism spectrum disorder had the highest frequency of medication administration.
Bottom line: As mental health visits in pediatrics continue to increase along with boarding times, clinicians should become more familiar with psychotropic medications used in this population and become comfortable in making sure that these patients have their home medications and have a plan for chemical sedation if other areas of de escalation fail.
Category: Pulmonary
Keywords: pulmonary embolism, intervention, scoring, out come (PubMed Search)
Posted: 7/18/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Deciding which pulmonary embolism patient needs thrombolytics/catheter based intervention is a shared decision among emergency physicians, intensivists, interventionalists, hospitalists, and the patient/family. This article provides evidence to help guide this decision. Keep in mind “The use of either CDL or catheter-based embolectomy in patients with intermediate-risk PE has, thus far, been correlated only with more rapid improvement of RV dysfunction than anticoagulation alone, not short- or long-term clinical or functional outcomes.”
"1. Massive (AHA) or high risk (ESC): Hypotension, defined as a systolic blood pressure <90 mm?Hg, a drop of >40 mm?Hg for at least 15 minutes (this latter criterion may be difficult to ascertain in some clinical circumstances), or need for vasopressor support, identifies these patients. They account for ?5% of hospitalized patients with PE and have an average mortality of ?30% within 1 month.
2.Submassive (AHA) or intermediate risk (ESC): RV strain without hypotension (see above) primarily identifies these patients. RV strain includes RV dysfunction on computed tomography pulmonary angiography or echocardiography (RV/left ventricular [LV] ratio >0.9)6,7 or RV injury and pressure overload detected by an increase in cardiac biomarkers such as troponins or brain natriuretic hormone.
3.Low risk (ESC and AHA): These patients do not meet criteria for submassive (AHA) or intermediate-risk (ESC) PE"
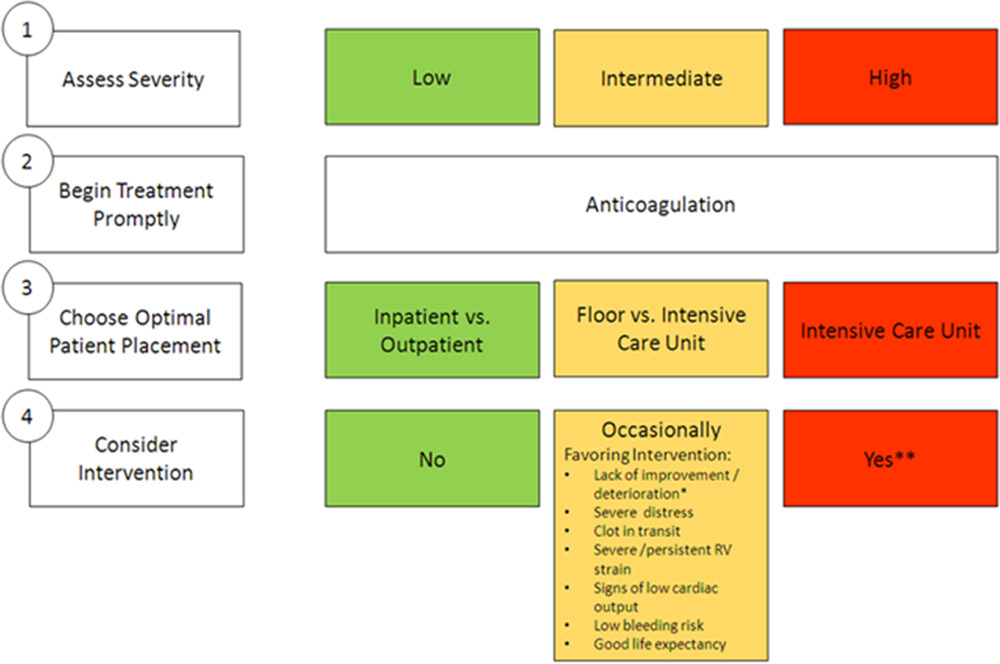
Interventional Therapies for Acute Pulmonary Embolism: Current Status and Principles for the Development of Novel Evidence: A Scientific Statement From the American Heart Association
Jay Giri, MD, MPH, FAHA, Chair, Akhilesh K. Sista, MD, FAHA, Vice Chair, Ido Weinberg, MD, MSc, Clive Kearon, MB, PhD, Dharam J. Kumbhani, MD, FAHA, Nimesh D. Desai, MD, PhD, Gregory Piazza, MD, MS, FAHA, Mark T. Gladwin, MD, FAHA, Saurav Chatterjee, MD, Taisei Kobayashi, MD, Christopher Kabrhel, MD, MPH, and Geoffrey D. Barnes, MD, MSc, FAHAAUTHOR INFO & AFFILIATIONS
Circulation
Category: Administration
Keywords: osteomyelitis, antibiotics, golden hour, trauma, open fracture (PubMed Search)
Posted: 7/17/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Early administration of antibiotics for open fractures can reduce serious bone and soft tissue infections, with a common goal being antibiotic administration within one hour of injury.
In this study, there were 523 patients treated by EMS who had an open extremity fracture.
The median time from EMS dispatch until antibiotic administration was 31 minutes. 99% of the patients who received antibiotics received them within one hour of EMS dispatch. Prehospital times were on average 10 minutes longer for those patients who received antibiotics. The majority of these patients received cefazolin, followed by ceftriaxone, ampicillin, gentamicin and piperacillin/tazobactam. None of these patients required management for an allergic reaction or anaphylaxis. Five patients (1%) who received prehospital antibiotics and 159 patients who did not (1.4%) had a subsequent infection based on ICD codes.
Bottom line: In this small group, it was safe to administer antibiotics to a patient with an isolated open extremity fracture and the medication was able to be delivered earlier. Larger studies will be needed to see the impact of this practice on the development of osteomyelitis or soft tissue infections.
Muniz AD, Gregorio DJ, Studebaker SA, et al. Time Savings and Safety of EMS Administration of Antibiotics for Open Fractures. Prehosp Emerg Care. Published online April 25, 2024. doi:10.1080/10903127.2024.2347291
