Category: Trauma
Keywords: occipital, condyles, fracture, cervical spine (PubMed Search)
Posted: 1/19/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
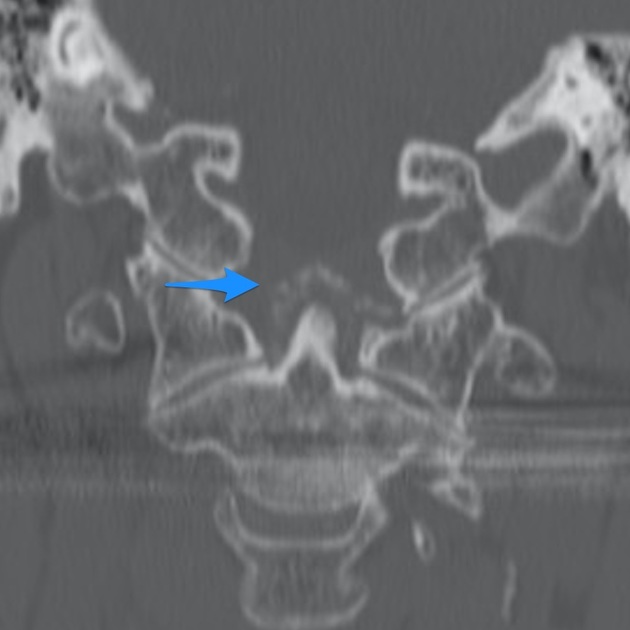
Fractures of the occipital condyles are a relatively rare injury that occur in high energy blunt mechanisms (IE roll over MVC) most commonly. Physical exam will show signs of basilar skull fracture and significant pain at the base of the skull/upper C-spine. CT scan is the gold standard to make the diagnosis. Look for signs of upper extremity weakness on physical exam or cranial nerve injuries. Those type of findings should also prompt emergent MRI evaluation. Treatment generally is long term immobilization in a collar however Type 3 and those with neurologic findings may require surgical intervention.
Anderson and Montesano Classification
Type I 3% of occipital condyle fracturesImpaction-type fracture with comminution of the occipital condyle
Due to compression between the atlantooccipital joint
Stable injury due to minimal fragment displacement into the foramen magnum
Type II 22% of occipital condyle fracturesBasilar skull fracture that extends into one or both occipital condyles
Due to a direct blow to skull and a sheer force to the atlantooccipital joint
Stable injury as the alar ligament and tectorial membrane are usually preserved
Type III 75% of occipital condyle fractures Avulsion fracture of condyle in region of the alar ligament attachment (suspect underlying occipitocervical dissociation)
Due to forced rotation with combined lateral bending
Has the potential to be unstable due to craniocervical disruption

Category: Pediatrics
Keywords: sedation, airway, preoxygenation (PubMed Search)
Posted: 1/17/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
This was a retrospective, multicenter cross-sectional study of pediatric sedations over 3 years using the Pediatric Sedation Research Consortium database.
85,599 pediatric sedations were included. These sedations did include the operating rooms.
8.7% of sedations required an intervention for airway/breathing/circulation in patients who did NOT have procedural oxygenation while 10.1% of patients in the group that did have procedural oxygenation required an intervention. The majority of these interventions were minor, ie airway repositioning. The group that did have procedural oxygenation did have a lower rate of hypoxia compared to the group without procedural oxygenation (2.5% vs 4.5%).
The authors concluded that preemptive procedural oxygenation did NOT decrease the overall need for interventions in the ABCs compared to no procedural oxygenation.
Li J, Krauss B, Monuteaux MC, Cavallaro S, Fleegler E. Preprocedural Oxygenation and Procedural Oxygenation During Pediatric Procedural Sedation: Patterns of Use and Association With Interventions. Ann Emerg Med. Published online June 12, 2024. doi:10.1016/j.annemergmed.2024.04.014
Category: Neurology
Keywords: Baclofen withdrawal, baclofen pump, dysautonomia (PubMed Search)
Posted: 1/16/2025 by Nicholas Contillo, MD
Click here to contact Nicholas Contillo, MD
Intrathecal baclofen pumps are increasingly used to manage spasticity in patients with conditions such as cerebral palsy, spinal cord injury, multiple sclerosis, traumatic brain injury, and other dystonias. The most common causes of baclofen pump dysfunction include pump-related issues (e.g., programming errors, battery failure), catheter problems (e.g., extra-thecal dislodgement, kinking, leaks), and medication depletion (e.g., overdue or insufficient refills). Symptoms of dysfunction can be nonspecific, ranging from mild (spasticity, dysphoria, dysesthesias) to severe (e.g., rigidity, rhabdomyolysis, seizures, fever, autonomic dysfunction, cardiomyopathy).
Once dysfunction is recognized, management involves stabilizing vital functions (ABCs, temperature management, fluids), administering multimodal antispasmodics (enteral or parenteral baclofen, benzodiazepines, dexmedetomidine, tizanidine), and performing pump interrogation, often in collaboration with neurology or PM&R specialists. Restoration of intrathecal flow is the preferred and definitive therapy; however, patients with severe withdrawal may require aggressive temporizing measures including intubation. Some authors describe intrathecal baclofen administration via lumbar puncture as a rescue measure for severe cases with limited access to definitive care. Imaging with plain radiographs, fluoroscopy, or CT may be indicated in select cases where there is concern for catheter displacement or kinking, and some patients may require surgical revision.
Takeaway: Consider baclofen withdrawal in patients on chronic baclofen therapy who present with nonspecific symptoms that may mimic conditions such as alcohol withdrawal, delirium, sympathomimetic toxicity, neuroleptic malignant syndrome, serotonin syndrome, thyrotoxicosis, rhabdomyolysis, sepsis, or status epilepticus. In cases of intrathecal pump dysfunction, the definitive treatment is restoration of baclofen flow, so involve consultants early for pump interrogation while temporizing with supportive measures.
Category: EMS
Keywords: CPR, on scene time, TOR, termination of resuscitation (PubMed Search)
Posted: 1/15/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Previous studies have shown that an on scene time of 10-35 minutes was associated with improved survival in pediatric out of hospital cardiac arrests compared to an on scene time of > 35 minutes. There was no significant difference in overall survival between < 10 minutes and 10-35 minutes of on scene time.
This study involved a total of 2854 pediatric cardiac arrests in the US and Canada. The patients who had a cardiac arrest during transport were compared to patients who received on scene CPR by equal minutes.
Among patients < 1 year, intra-arrest transport was associated with lower survival to hospital discharge compared to those that were resuscitated on scene. There was no association for patients > 1 year.
Bottom line: This study supports resuscitating in place for pediatric cardiac arrests, especially in patients < 1year.
Okubo M, Komukai S, Izawa J, et al. Survival After Intra-Arrest Transport vs On-Scene Cardiopulmonary Resuscitation in Children. JAMA Netw Open. 2024;7(5):e2411641. Published 2024 May 1. doi:10.1001/jamanetworkopen.2024.11641
Category: Critical Care
Posted: 1/14/2025 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
These 2 papers challenge management dogmas in critical care that have persisted despite low-quality/absent evidence.
In particular, one explores the dogma, “bicarbonate improves ventricular contractility in severe metabolic acidosis,” with the following points:
-intracellular pH (which has a large impact on myocardial contractility) correlates poorly with blood gas pH
-many of the studies regarding bicarbonate in severe metabolic acidosis and hemodynamics are done on animal shock models
-two studies in patients with lactic acidosis showed increase in pH with bicarb administration without beneficial impact on hemodynamics (even in pts with pH < 7.1)
-bicarb administration is associated with hypernatremia, hypokalemia, and decreased ionized calcium levels
Hofmaenner DA, Singer M. Challenging management dogma where evidence is non-existent, weak or outdated. Intensive Care Med. 2022;48(5):548-558.
Hofmaenner DA, Singer M. Challenging management dogma where evidence is non-existent, weak, or outdated: part II. Intensive Care Med. 2024;50(11):1804-1813.
Category: Pharmacology & Therapeutics
Keywords: tpa, frostbite, iloprost, therapy (PubMed Search)
Posted: 1/13/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This meta analysis of studies looking at thrombolytics and prostaglandins in treating significant frost bite offers some insight into the possibilities these therapeutics offer. Unfortunately, the studies available are not high quality and most are case reports.
“Our results suggest that thrombolysis or intravenous iloprost is effective when administered promptly to treat severe frostbite. For grade 3–4 frostbite the Wilderness Medical Society frostbite guidelines recommend the use of intravenous iloprost within 48 h of injury, and thrombolysis within 24 h of injury. The Helsinki protocol recommends the use of tPA for patients with grade 3–4 frostbite presenting within 48 h of injury with angiographic evidence of thrombosis."
“Iloprost is a synthetic prostaglandin I2 that has been used to treat frostbite . Like other prostacyclins, it inhibits platelet aggregation and promotes vasodilation. Iloprost may stimulate the release of endogenous tissue plasminogen activator or counteract its inhibitory effects [35]. Iloprost reduces vasoconstriction induced by thromboxane A2 , and may reduce oxidative stress from free radicals, moderating reperfusion injury [37, 38]. The effect on platelet aggregation may be reversed within two hours), but prostacyclin effects may disrupt the vicious cycle of activated platelets and leukocytes that damages endothelium .”
More research in this area is needed. Transfer to a center with these capabilities seems worth a discussion in the case of severe frostbite.
Regli, I.B., Oberhammer, R., Zafren, K. et al. Frostbite treatment: a systematic review with meta-analyses. Scand J Trauma Resusc Emerg Med 31, 96 (2023). https://doi.org/10.1186/s13049-023-01160-3
Category: Trauma
Keywords: Frail, trauma, mortality, outcome (PubMed Search)
Posted: 1/12/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
The Trauma Frailty Index has been validated to predict inpatient mortality, major complications and discharge to rehab facility. “In addition, frailty was significantly associated with higher adjusted odds of mortality, major complications, readmissions, and fall recurrence at 3 months postdischarge ( p < 0.05).”
It is a simple 15 variable index.

Joseph B, Saljuqi AT, Amos JD, Teichman A, Whitmill ML, Anand T, Hosseinpour H, Burruss SK, Dunn JA, Najafi K, Godat LN, Enniss TM, Shoultz TH, Egodage T, Bongiovanni T, Hazelton JP, Colling KP, Costantini TW, Stein DM, Schroeppel TJ, Nahmias J; AAST Frailty MIT Study Group. Prospective validation and application of the Trauma-Specific Frailty Index: Results of an American Association for the Surgery of Trauma multi-institutional observational trial. J Trauma Acute Care Surg. 2023 Jan 1;94(1):36-44. doi: 10.1097/TA.0000000000003817. Epub 2022 Oct 17. PMID: 36279368.
Category: Orthopedics
Posted: 1/11/2025 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Calcium pyrophosphate deposition disease (CPPD), AKA pseudogout.
Calcium crystal deposits form on articular surfaces.
This MAY trigger an inflammatory synovitis. Also can be asymptomatic.
Degenerative changes occur to the affected joint over time
CC: Moderate to severe pain, tenderness to palpation, stiffness, redness, warmth and decreased ROM.
May appear as punctate linear densities within the articular cartilage.
Joint fluid analysis: Weakly positive birefringent rhomboid shaped crystals.
Differential diagnosis: Calcified meniscus and Septic knee
Category: Pharmacology & Therapeutics
Keywords: olanzapine, benzodiazepine, drug interaction (PubMed Search)
Posted: 1/10/2025 by Alicia Pycraft
Click here to contact Alicia Pycraft
Background
Treatment of acute agitation often involves combining antipsychotics and benzodiazepines. Injectable olanzapine, a second-generation antipsychotic, uniquely carries a warning against concomitant use with parenteral benzodiazepines. The olanzapine prescribing information states that “concomitant administration of intramuscular (IM) olanzapine and parenteral benzodiazepines is not recommended due to the potential for excessive sedation and cardiorespiratory compromise”. The European Medicines Agency (similar to the United States FDA) cautions against use of the two within 60 minutes of each other using similar language.
The above warnings were based on a 2010 publication of 160 adverse event reports from a post-marketing database maintained by the drug manufacturer, and have resulted in many institutions prohibiting co-administration of IM olanzapine and parenteral benzodiazepines. The publication cited 29 fatal adverse events involving injectable olanzapine, concluding that caution should be exercised when using IM olanzapine and parenteral benzodiazepines simultaneously. However, 25 of the 29 patients received other sedating medications in addition to olanzapine and benzodiazepines, and the majority of fatalities were >12 hours after the last dose of olanzapine. Following this publication, a 2013 randomized controlled trial by Chan et al. found no difference in adverse event rates between patients receiving IV midazolam alone and patients receiving IV midazolam plus IV olanzapine for acute agitation.
This December 2024 study by Cole et al. aimed to re-evaluate the risks of cardiorespiratory compromise with concomitant injectable olanzapine and injectable benzodiazepine administration.
Study design
This was a single-center retrospective cohort study of 693 patients who received 2 parenteral doses of eligible sedating medications within 60 minutes of each other. A total of 549 patients received 2 doses of olanzapine, and 144 received olanzapine and a benzodiazepine (midazolam, lorazepam, or diazepam). To avoid cohorts with a higher baseline risk of sedation, patients who received other sedating medications and patients who received more than 2 doses of olanzapine or 1 dose of a benzodiazepine were excluded.
Patient Population
Results

*One death during hospitalization was due to missed occlusion myocardial infarction
Study Critique:
Key Takeaways
Category: Critical Care
Posted: 1/8/2025 by William Teeter, MD
Click here to contact William Teeter, MD
Extracorporeal cardiopulmonary resuscitation (ECPR) is a type of extracorporeal support following cardiac arrest available at a small, but growing number of ECMO centers around the world. After some initial promising results, more recent data have been mixed. There is a nice narrative review in JACEP Open recently which summarizes the most recent evidence. Implementation considerations and patient selection seemingly drive the variance seen in the studies reviewed.
To this point, a new article from Critical Care Medicine was just published looking at the outcomes of eCPR with respect to age using 5 years of ELSO patient data. Unsurprisingly, advancing age is associated with worse outcomes, with significantly reduced odds of survival above the age of 65.
Category: Critical Care
Keywords: Frailty, morbidity, mortality, geriatric (PubMed Search)
Posted: 1/5/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
The level of fitness/health a patient has entering the marathon of recovery from critical illness or trauma has a major impact on morbidity and mortality. Frailty is a measure of this fitness level. The clinical frailty scale can be used to assess your patients ability to survive critical illness. Age is a number. Frailty is more useful.


Category: Cardiology
Keywords: Hypertension, MACE, end organ (PubMed Search)
Posted: 1/4/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This study followed patients presenting to the ED with elevated (SBP>180, DBP>120) blood pressure without evidence of end organ dysfunction for one year. The patients were followed for major adverse cardiac events. They found:
“A total of 12,044 patients were enrolled. The prevalence of MACE within one year was 1,865 (15.5%). Older age, male gender, history of cardiovascular disease, cerebrovascular disease, diabetes, smoking, presentation with chest pain, altered mental status, dyspnea, treatment with intravenous and oral hydralazine, and oral metoprolol were independent predictors for one-year MACE. Additionally, discharge with an SBP ?160 mm Hg was not associated with 30-day MACE-free survival after propensity matching (hazard ratio 0.99, 95% confidence interval 0.78–1.25, P?=?0.92).”
Treating to reach a magic number did not help. Most likely, long term control of blood pressure is a more important factor than attempts to lower in the ED. While this is a high risk group, there is no evidence that acute lowering of blood pressure impacts long term survival.
Category: Critical Care
Keywords: post-intensive care syndrome, PICS, PICS-F (PubMed Search)
Posted: 12/31/2024 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Post-Intensive Care Syndrome (PICS) is an increasingly recognized phenomenon of impairment of physical, cognitive, and/or mental health after intensive care admission. Even more recently, similar deficits in caregivers of patients admitted to the ICU, often called Post-Intensive Care Syndrome Family (PICS-F) is increasingly recognized. A study recently published by Watland et al in Critical Care Medicine looking at reducing PICS-F through a “caregiver pathway” got me wondering if there's any literature out there about reducing PICS-F via interventions in the emergency department. Patients' treatment course in the ED is a highly stressful and uncertain time for both the patient and family members, so it stands to reason this is an impactful period where intervention may help, and even in patients where their condition is too advanced for us to make a medical difference, our actions could have a positive impact on long term outcomes for the family members.
The short answer is no, to this author's knowledge and based on my review of the literature, there is no good evidence for reducing PICS-F by ED interventions (hint, hint: if anyone's looking for a good area to study…) Based on evidence from the critical care realm, the following are probably reasonable approaches that would translate well to the ED:
Watland, Solbjørg RN, MS1,,2,3; Solberg Nes, Lise LP, PhD1,,3,,4; Ekeberg, Øivind MD, PhD5; Rostrup, Morten MD, PhD2,,6; Hanson, Elizabeth RN; PhD7,,8; Ekstedt, Mirjam RN, PhD7,,9; Stenberg, Una PhD10,,11; Hagen, Milada PhD12; Børøsund, Elin RN, PhD1,,13. The Caregiver Pathway Intervention Can Contribute to Reduced Post-Intensive Care Syndrome Among Family Caregivers of ICU Survivors: A Randomized Controlled Trial. Critical Care Medicine ():10.1097/CCM.0000000000006546, December 24, 2024. | DOI: 10.1097/CCM.0000000000006546
Shirasaki K, Hifumi T, Nakanishi N, Nosaka N, Miyamoto K, Komachi MH, Haruna J, Inoue S, Otani N. Postintensive care syndrome family: A comprehensive review. Acute Med Surg. 2024 Mar 11;11(1):e939. doi: 10.1002/ams2.939. PMID: 38476451; PMCID: PMC10928249.
Category: Trauma
Keywords: chest injury, exercise, chronic pain, (PubMed Search)
Posted: 12/30/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This study suggests no. The control arm was given standard physical therapy and the intervention arm was instructed in four basic exercises to do on their own daily for a week. Patents were then surveyed to assess for long term pain. There was no difference in pain between the two groups. Meaning, at least in this study reliant on patient journaling and follow up, that these four simple exercises did not impact long term pain in chest wall injured patients. More work needs to be done in this important area.
Cheri Battle, Timothy Driscoll, Deborah Fitzsimmons, Shaun Harris, Fiona Lecky, Claire O'Neill, Alan Watkins, Jane Barnett, Susan Davies, Hayley Anne Hutchings, Kate Jones, Andrew Eglington, Sophie Place, Hannah Toghill, Katie Foster, Bethan Uzzell, Elizabeth Ford, Mark Baker, Sophie Lewis, Sara Davies, Sarah Nicholls, Amy Charnock, Claire Watkins, Sarah-Jane Garside, Jeannie Bishop, Thomas Dawson, Jessica Pendlebury, Reece Doonan,
EarLy Exercise in blunt Chest wall Trauma: A multi-centre, parallel randomised controlled trial (ELECT2 Trial),
Injury,
2024,
112075,
ISSN 0020-1383,
https://doi.org/10.1016/j.injury.2024.112075.C
Category: Critical Care
Keywords: agitation, choking, hypoxia, acidosis, breathing (PubMed Search)
Posted: 12/29/2024 by Steve Schenkel, MPP, MD
(Updated: 2/8/2026)
Click here to contact Steve Schenkel, MPP, MD
In a fascinating perspective piece, Matt Bivens and colleagues explain that the combination of struggle and restraint leads to death not because of hypoxia, but because of acidosis.
The sequence is something like this: exertion or struggle results in an acidotic state -> restraint reduces respiratory ability, especially when held prone or weight is applied to back or chest -> acidosis worsens with the potential for cardiac arrhythmia and arrest.
In this setting, “I can’t breathe” does not mean that there is no air movement over the vocal cords but that respiration is impaired, much as it is in asthma or obstructive lung disease.
Use of sedation in this setting reduces respiration even further, worsening acidosis and risking death. It’s not hypoxia that kills; it’s acidosis.
See the complete perspective here: https://www.nejm.org/doi/full/10.1056/NEJMp2407162.
Bivens M, Jaeger E, Weedn V. Handcuffs and Unexpected Deaths — “I Can’t Breathe” as a Medical Emergency. NEJM 2024; 391:2068-9. DOI: 10.1056/NEJMp2407162
Category: Orthopedics
Posted: 12/28/2024 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
A stinger is a short lived neuropraxia to the upper brachial plexus
Named for the temporary sensation that radiates from the shoulder to the hand
Can occur though 3 common mechanisms
Most commonly from direct traumatic or tractional injury
https://www.physio-network.com/wp-content/uploads/2021/11/unnamed-1.png
Common in American Football
Occurs in almost 50% of players over a 4-year college career
Most commonly to running backs and linebackers in one NFL study
Symptoms: Unilateral burning pain and tingling in the arm with transient weakness
Symptoms NOT confined to a single dermatome.
Usually in C5, C6 innervated muscles (deltoid and biceps).
Symptoms are transient usually resolving in approximately 2 minutes
If asked to examine someone for this at a sporting event
Evaluate patient for:
C spine tenderness
Full cervical range of motion
UNILATERAL weakness in shoulder Abductors and external rotators
UNILATERAL weakness in biceps
UNILATERAL weakness in forearm pronation
UNILATERAL weakness in triceps extension
Consider evaluation for concussion symptoms if appropriate
Majority of patients in college and profession sports return to play in game when exam returns to normal
Category: Administration
Keywords: push notification, EMR, ED flow, results, radiology (PubMed Search)
Posted: 12/26/2024 by Steve Schenkel, MPP, MD
(Updated: 2/8/2026)
Click here to contact Steve Schenkel, MPP, MD
Clinical practice in the world of the Electronic Medical Record has made many a clinician question the value of electronic reminders.
Banners warn of sepsis, the need for repeat evaluation, vital signs outside expected limits, wait times, and risks for readmission.
Can they instead help ED flow?
Sayan Dutta and colleagues suggest that they can. When clinicians chose to receive notice of a lab or imaging result, push notification reduced time between final result and ED disposition by 18 minutes (95% CI: 15-21 minutes).
The likely key here? Clinicians actively chose when and about what to be notified.
See: Result Push Notifications Improve Time to Emergency Department Disposition: A Pragmatic Observational Study, Annals of Emergency Medicine, 85(1), 53-62. https://www.annemergmed.com/article/S0196-0644(24)00404-9/abstract.
Result Push Notifications Improve Time to Emergency Department Disposition: A Pragmatic Observational Study
Dutta, Sayon et al.
Annals of Emergency Medicine, Volume 85, Issue 1, 53 - 62
Category: Misc
Keywords: Neck pain, crowned dens syndrome (PubMed Search)
Posted: 12/22/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Crowned dens syndrome is an acute inflammatory disease caused by deposition of calcium pyrophosphate dihydrate crystals or hydroxyapatite crystals in the soft tissue and ligaments surrounding the dense. Patient presentation is severe pain in the neck and base of the skull, low grade fever, and elevated inflammatory markers. It is most commonly seen in elderly females. Ct scan is the gold standard for diagnosis. Once meningitis and other significant infectious process has been excluded, treatment is anti inflammatory medications including steroids.
Category: Pediatrics
Keywords: nasal suctioning, rsv, bronchiolitis (PubMed Search)
Posted: 12/18/2024 by Jenny Guyther, MD
(Updated: 12/20/2024)
Click here to contact Jenny Guyther, MD
Infants are typically obligate nasal breathers and the increased mucus production associated with bronchiolitis can impair both breathing and feeding. AAP bronchiolitis guidelines state that the routine use of deep suctioning may not be beneficial.
This was an observational study of 121 infants aged 2-23 months with bronchiolitis who received either nasal suction (31), deep suction (68) or a combination (52). Groups were based on clinician discretion. Respiratory scores and pulse ox were obtained pre-suction and at 30 and 60 minutes post suction.
There was no difference between suction type and respiratory score. However, there was an improvement in respiratory score between the 0-30 and 0-60 time point with any suctioning. Suction type had no effect on pulse ox, airway adjunct escalation, length of stay or outpatient outcomes.
The study also showed no association between albuterol use and respiratory scores (albuterol is not recommended by the AAP in the management of bronchiolitis).
Bottom line: In this small study, nasal aspiration and deep suction appear to be equal in improving respiratory scores up to 1 hour post suction suggesting that deep suctioning may not be needed.
Hedland JL, Chang TP, Schmidt AR, Festekjian A. Suctioning in the management of bronchiolitis: A prospective observational study. Am J Emerg Med. 2024;82:57-62. doi:10.1016/j.ajem.2024.05.013
Category: Airway Management
Keywords: Ketamine, etomidate, RSI, induction (PubMed Search)
Posted: 12/19/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Another large database evaluation of the use of etomidate vs. ketamine as an induction agent for intubation found a trend toward higher mortality in the etomidate group. Even when trying to control for steroid use (to control for etomidate’s possible adrenal suppression), etomidate had a higher mortality rate.
A well done study that adds to the chorus advocating for choosing ketamine when looking for a hemodynamically neutral induction agent.
Wunsch H, Bosch NA, Law AC, Vail EA, Hua M, Shen BH, Lindenauer PK, Juurlink DN, Walkey AJ, Gershengorn HB. Evaluation of Etomidate Use and Association with Mortality Compared with Ketamine among Critically Ill Patients. Am J Respir Crit Care Med. 2024 Nov 15;210(10):1243-1251. doi: 10.1164/rccm.202404-0813OC. PMID: 39173173.
