Category: Trauma
Keywords: trauma, hyperopia, oxygen, length of stay (PubMed Search)
Posted: 8/29/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This retrospective study of Swiss trauma patients looked at blood gas oxygen levels within 3 hours of arrival to the trauma bay in severely injured patients over age 16. When comparing hypoxic, hyperoxic and normo-oxic patients there was no difference in 28 day mortality. Those with above normal oxygen levels tended toward longer hospital stays. The above normal oxygen cohort also were more likely to be intubated in the field.
This study fits with others showing around 20% of trauma patients arrive to our trauma bays over oxygenated. More research is needed to see the impact this has on care. Be mindful of over oxygenation especially in intubated trauma patients.
Iten, M., Pietsch, U., Knapp, J. et al. Hyperoxaemia in acute trauma is common and associated with a longer hospital stay: a multicentre retrospective cohort study. Scand J Trauma Resusc Emerg Med 32, 75 (2024). https://doi.org/10.1186/s13049-024-01247-5
Category: Administration
Keywords: Medicare advantage, insurance, payor, fee-for-service (PubMed Search)
Posted: 8/28/2024 by Steve Schenkel, MPP, MD
(Updated: 2/8/2026)
Click here to contact Steve Schenkel, MPP, MD
Traditional Medicare now covers < 50% of Medicare beneficiaries. It reimburses on a fee-for-service basis. For beneficiaries, it includes deductibles and coinsurance requirements that yield average annual out-of-pocket expenses measured in the thousands of dollars.
Medicare Advantage, the new alternative, has grown quickly. Plans typically promise beneficiaries fewer co-pays and more services. It relies on private insurers (think United, Blue Cross, Kaiser Permanente) to coordinate care and rein in costs. Subsidies to Medicare Advantage have helped spur growth, subsidies that mean costs per beneficiary for Medicare Advantage exceed those for traditional Medicare.
Which means Medicare still needs to figure out how to save money and remain viable while the US population over 65 grows.
When listening to a lecture about Medicare or reading a study that uses Medicare data, take a moment to ask “Which Medicare? Fee-for-service? Or Advantage?”
For a take on the future of Medicare, see McWilliams JM, The Future of Medicare and the Role of Traditional Medicare as Competitor, NEJM, August 22/29, 763-769.
To understand why Medicare Advantage plans are popular, see https://www.kff.org/medicare/issue-brief/10-reasons-why-medicare-advantage-enrollment-is-growing-and-why-it-matters/.
Category: Critical Care
Posted: 8/27/2024 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Hepatorenal Syndrome
Nadim M, et al. Hepatorenal syndrome in the intensive care unit. Intensive Care Med. 2024; 50:978-981.
Category: Hematology/Oncology
Keywords: Oncology, Endocrine, Hypercalcemia, Electrolyte (PubMed Search)
Posted: 8/26/2024 by Sarah Dubbs, MD
(Updated: 2/8/2026)
Click here to contact Sarah Dubbs, MD
We see patients with nausea, fatigue, altered mental status, and other vague symptoms all day, every day in the ED. Let's not forget about hypercalcemia in the differential, especially in patients with a known malignancy! Many tumor types secrete a Parathyroid hormone (PTH)- related protein that mimics PTH and leads to high calcium levels.
Here are some clinical pearls on hypercalcemia of malignancy:
Category: Infectious Disease
Keywords: Mpox, monkeypox, outbreak, democratic republic of congo (PubMed Search)
Posted: 8/25/2024 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
Background:
What’s new?
Who is at risk?
Patients with epidemiologic characteristics and lesions or other signs and symptoms consistent with mpox. This includes anyone with travel to DRC or any of its neighboring countries (ROC, CAR, Rwanda, Burundi, Uganda, Zambia, Angola, Tanzania, and South Sudan) in the previous 21 days.
What to look for?
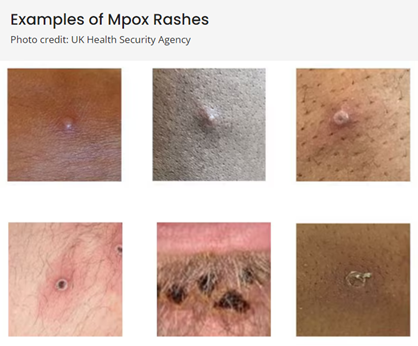
(Above photos from https://www.cdc.gov/poxvirus/mpox/clinicians/clinical-recognition.html)
What to do?
If mpox is suspected in a patient:
Duwell M. Mpox Clinician Letter. Maryland Department of Health. August 19, 2024.
Mpox Caused by Human-to-Human Transmission of Monkeypox Virus in the Democratic Republic of the Congo with Spread to Neighboring Countries. US Centers for Disease Control and Prevention. CDC Health Alert Network, August 7, 2024, 3:15 PM ET, Accessed at https://emergency.cdc.gov/han/2024/han00513.asp# on August 25, 2024.
Mpox. US Centers for Disease Control and Prevention. https://www.cdc.gov/poxvirus/mpox/index.html, Accessed on August 25, 2024.
Category: Orthopedics
Posted: 8/24/2024 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
When it comes to walking, recent research and public health strategies have focused on how much you do that helps. This idea frequently comes up in the form of the 10,000 step goal.
A recent study in the British Journal of Sports Medicine found that walking between 9,000 and 10,000 steps/day could reduce the risk of death by 39% and cardiovascular disease by 21%.
For both outcomes (all-cause mortality and incident CVD), approximately 50% of the benefit was achieved between 4,000-4,500 steps per day.
Study accessed data on greater than 72,000 individuals (avg age 61, 58% female) using accelerometer data over an average of 6.9 years.
Instead of volume, a recent study in the same journal looked at the benefits of walking speed.
The study looked at pooled data from 10 studies involving more than 500,000 people from the U.S., Japan and the U.K.
Walking speed definitions:
Easy or casual walking - less than 2 mph.
Average or normal pace was defined as 2-3mph.
A “fairly brisk” pace was 3-4 mph
A “brisk/striding walking pace” was greater than 4mph
Compared with people who walked at a casual/easy speed, those who walked at a normal/avg speed (2–3 mph) had a 15% lower risk of Type 2 diabetes.
Walking at a fairly brisk pace (3–4 mph) was associated with a 24% lower risk of Type 2 diabetes.
Walking at a brisk or striding pace (over 4 mph) was associated with a 39% reduced risk of Type 2 diabetes.
Globally, 537 million adults have type 2 diabetes, a figure that is expected to reach 783 million by 2045.
Take home: Consider recommending tips on walking pace and distance for our sedentary patient population to optimize health.
Jayedi A, Zargar MS, Emadi A, Aune D. Walking speed and the risk of type 2 diabetes: a systematic review and meta-analysis. Br J Sports Med. 2024 Mar 13;58(6):334-342.
Category: Administration
Keywords: confounding factors, epidemiologic (PubMed Search)
Posted: 8/21/2024 by Mike Witting, MS, MD
Click here to contact Mike Witting, MS, MD
“I’m not going to the hospital, my father died in a hospital.”
In planning a study it’s a good practice to consider what confounding variables you may need to look out for.
Confounding variables are associated with the predictor (independent) and outcome (dependent) variables, but they are not in the causal chain. In the above example, disease is likely the predictor variable, death is the outcome variable, and going to the hospital is a confounder. Of course, this assumes the death was not iatrogenic; then the hospital would be in the causal chain.
Patients may be selected for interventions based on severity of disease, functional status, education level, and other factors, and these may be confounders.
Confounding can be addressed at the design stage, by:
It can be addressed in the analysis stage by:
Adapted from Hulley SB, Cummings SR. Designing clinical research, 4th edition, Lippincott, Williams and Wilkins, 2013.
Category: Critical Care
Keywords: Euglycemic DKA (PubMed Search)
Posted: 8/20/2024 by Cody Couperus-Mashewske, MD
Click here to contact Cody Couperus-Mashewske, MD
Euglycemic DKA (eDKA) is a medical emergency requiring prompt attention. It is caused by an imbalance of insulin and glucagon leading to ketone accumulation (1-3). In addition to typical risk factors for DKA, those for eDKA include SGLT-2 inhibitor use and pregnancy, with 30% of DKA cases in pregnancy presenting euglycemic (4, 5).
eDKA presents with an anion gap metabolic acidosis, ketosis/ketonuria, & blood glucose less than 250 mg/dL.
Diagnosis requires ruling out other causes of anion gap metabolic acidosis, including toxic ingestions.
The cornerstone of eDKA management is ensuring enough dextrose to allow needed insulin administration to reverse ketone accumulation.
1. McCabe, D. E., Strollo, B. P. & Fuhrman, G. M. Euglycemic Diabetic Ketoacidosis in the Surgical Patient. Am. Surg. 89, 1083–1086 (2023).
2. Chaudhry, A., Roels, C. & Lee, J. Sodium–Glucose Cotransporter-2 Inhibitor–associated Euglycemic Diabetic Ketoacidosis: Lessons From a Case Series of 4 Patients Undergoing Coronary Artery Bypass Grafting Surgery. Can. J. Diabetes 46, 843–850 (2022).
3. Wan Azman, S. S., Sukor, N., Abu Shamsi, M. Y., Ismail, I. & Kamaruddin, N. A. Case Report: High-Calorie Glucose Infusion and Tight Glycemic Control in Ameliorating Refractory Acidosis of Empagliflozin-Induced Euglycemic Diabetic Ketoacidosis. Front. Endocrinol. 13, 867647 (2022).
4. Jaber, J. F., Standley, M. & Reddy, R. Euglycemic Diabetic Ketoacidosis in Pregnancy: A Case Report and Review of Current Literature. Case Rep. Crit. Care 2019, 1–5 (2019).
5. Algaly, G., Abdelrahman, A. & Ahmed, S. M. I. Euglycemic diabetic ketoacidosis in a pregnant woman. J. Am. Coll. Emerg. Physicians Open 4, e13089 (2023).
6. Dutta, S. et al. Euglycemic diabetic ketoacidosis associated with SGLT2 inhibitors: A systematic review and quantitative analysis. J. Fam. Med. Prim. Care 11, 927 (2022).
7. Koceva, A. & Kravos Tramšek, N. A. From Sweet to Sour: SGLT-2-Inhibitor-Induced Euglycemic Diabetic Ketoacidosis. J. Pers. Med. 14, 665 (2024).
8. Juneja, D., Nasa, P., Jain, R. & Singh, O. Sodium-glucose Cotransporter-2 Inhibitors induced euglycemic diabetic ketoacidosis: A meta summary of case reports. World J. Diabetes 14, 1314–1322 (2023).
9. Albert, S. G., Shrestha, E. & Wood, E. M. Euglycemic diabetic ketoacidosis: The paradox of delayed correction of acidosis. Diabetes Metab. Syndr. Clin. Res. Rev. 17, 102848 (2023).
Category: Ultrasound
Keywords: musculoskeletal, POCUS, joint arthrocentesis, shoulder dislocation, joint injection (PubMed Search)
Posted: 8/19/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
To obtain a posterior shoulder view: Have the patient sit up with the back of the bed down. Position the curvilinear probe in the posterior aspect of the shoulder with the probe parallel to the patient bed, at the level just below the scapular spine and the marker towards the patient's left. You can have the patient rotate their arm to help you visualize the movement of the humeral head.
In the normal anatomy, the humeral head should be at the level of the glenoid (this is a patient's left shoulder):
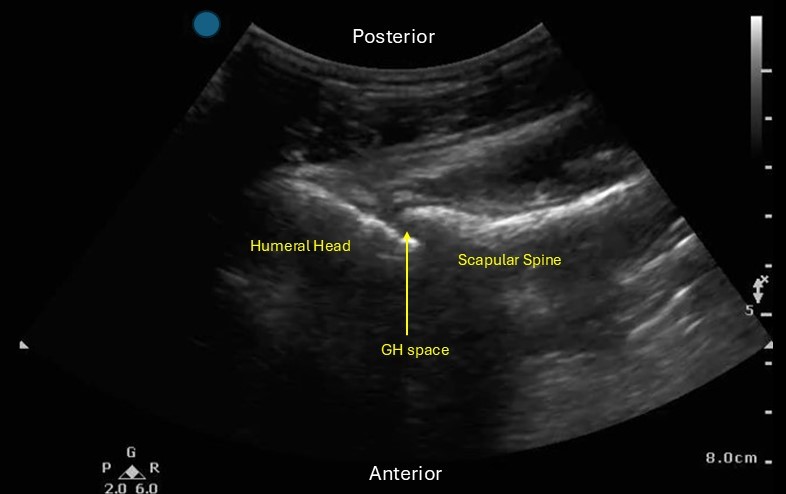
Locate the glenohumeral joint space. You can evaluate the GH joint for effusion, perform joint arthrocentesis/injection and look for signs of shoulder dislocation.
If you are evaluating for signs of a dislocation:
Posterior dislocation: the humeral head will be more SUPERFICIAL in the image than the scapular spine
Anterior dislocation: the humeral head will be DEEPER in the image than the scapular spine.
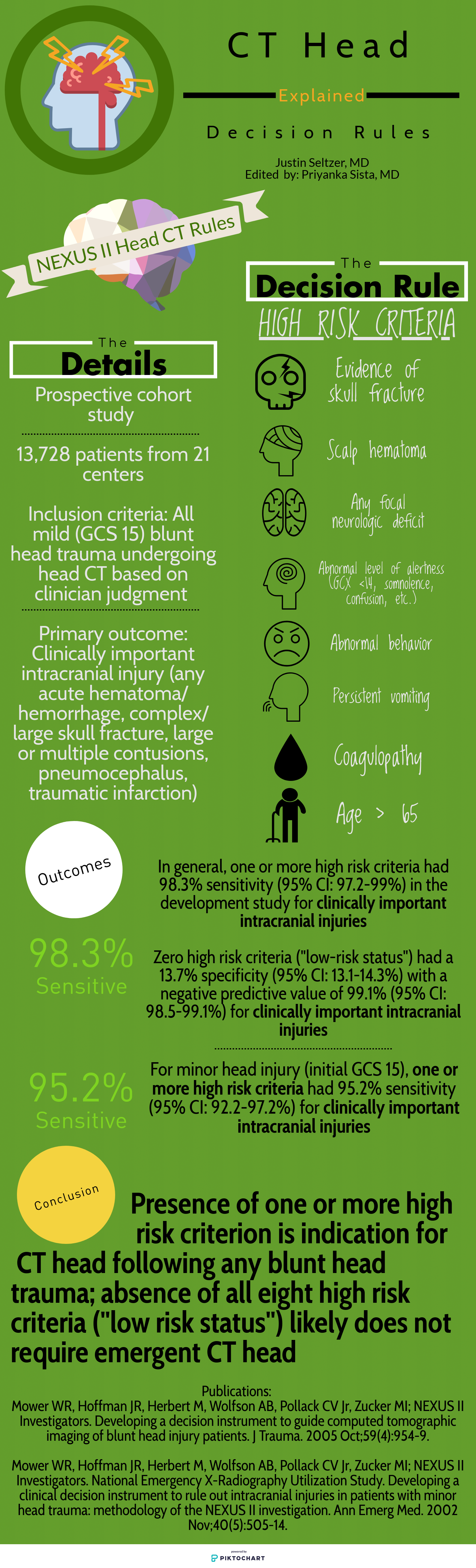
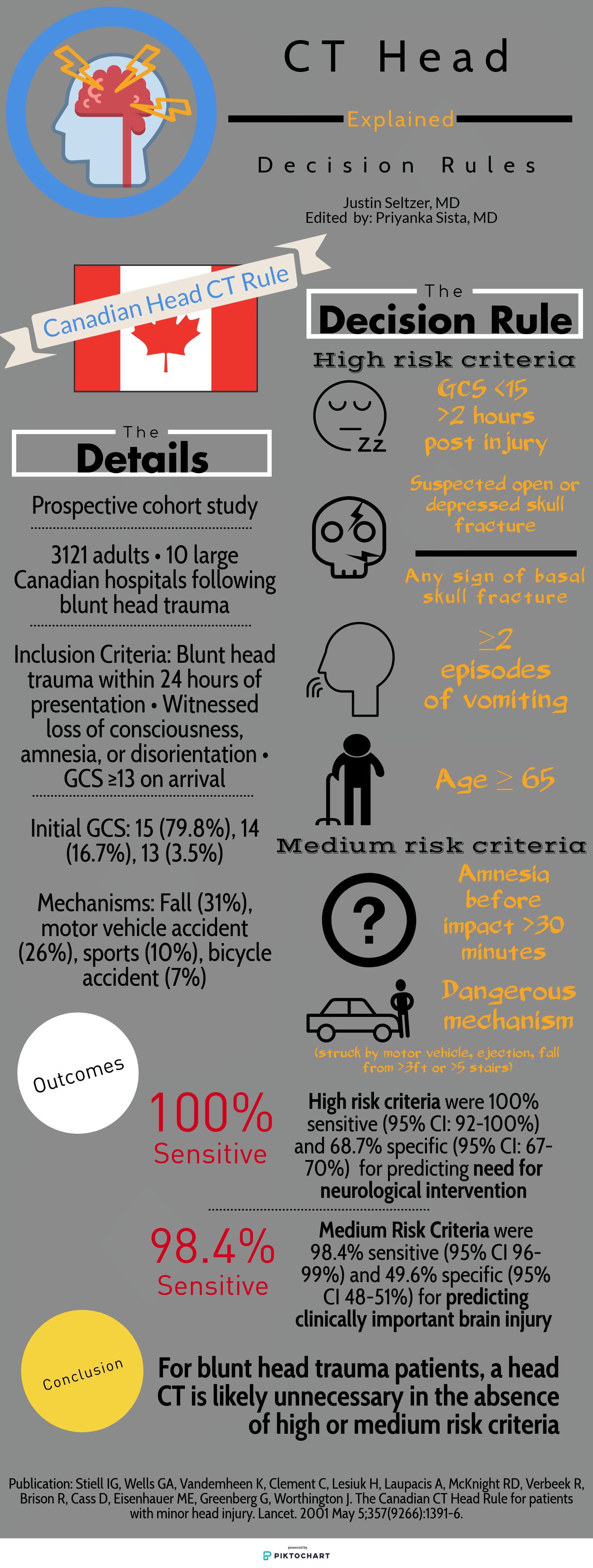
Category: Trauma
Keywords: Head injury, decision tools (PubMed Search)
Posted: 8/18/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
Deciding who needs exposure to radiation after blunt head injury has been looked at by both the Canadian Head Injury Guidelines as well as NEXUS. This website has excellent graphics outlining the rules. Note age over 65 alone is predictive of significant intracranial injury. All recent studies indicate age over 65 even with a low suspicion mechanism such as fall from standing is still a significant risk for intracranial pathology.
Category: Administration
Keywords: racial disparities, antibiotic prescribing (PubMed Search)
Posted: 8/14/2024 by Kevin Semelrath, MD
(Updated: 8/17/2024)
Click here to contact Kevin Semelrath, MD
This retrospective study found that while overall rates of antibiotic prescriptions for viral URIs were low (that's good!), patients identified as non Hispanic white were prescribed antibiotics, despite guidelines advising against them, at a higher rate than non white patients (that's bad). It also found that in areas of socioeconomic deprivation, the prescribing rates were lower across all races than in more affluent areas (that's good and bad!)
Open AccessPublished:January 23, 2024DOI:https://doi.org/10.1016/j.annemergmed.2023.12.003
Category: Pediatrics
Keywords: chest tube landmarks, PTX, placement (PubMed Search)
Posted: 8/16/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
This was an observational study where ultrasound was used to evaluate if the diaphragm came into view at the 5th intercoastal space (ICS) at the midaxillary line in pediatric patients during maximal respiration. A convenience sample of pediatric patients who presented to the an academic pediatric emergency department was used.
In 10.3% of patients, the diaphragm crossed the 5th ICS during normal respirations and 27.2% crossed during maximal respirations. This was a more common occurrence on the right compared to the left. An increase in body mass index was also associated with an increased risk of the diaphragm crossing the during both tidal respiration and maximal respirations.
Bottom line: Using a blind insertion of a chest tube at the 5th ICS, midaxillary line in the pediatric patient poses a not insignificant risk of piercing the diaphragm. this study recommends using ultrasound prior to chest tube placement.
Ruthford MR, Shah A, Wolf BJ, Kane ID, Borg K, Moake MM. Ultrasound Investigation of the Fifth Intercostal Space Landmark for Chest Tube Thoracostomy Site Selection in Pediatric Patients. Pediatr Emerg Care. Published online April 23, 2024. doi:10.1097/PEC.0000000000003207
Category: Trauma
Keywords: Fall, alcohol, geriatric, head injury (PubMed Search)
Posted: 8/9/2024 by Robert Flint, MD
(Updated: 8/15/2024)
Click here to contact Robert Flint, MD
A study looking at patients over age 65 with head injuries from falls assessed the association of alcohol use with severity of injury. The alcohol use was self-reported which does limit the findings. The study found “Of 3128 study participants, 18.2% (n = 567) reported alcohol use: 10.3% with occasional use, 1.9% with weekly use, and 6.0% with daily use.” Those daily drinkers had a higher incidence of intercranial injuries.
The authors concluded: “Alcohol use in older adult emergency department patients with head trauma is relatively common. Self-reported alcohol use appears to be associated with a higher risk of ICH in a dose-dependent fashion. Fall prevention strategies may need to consider alcohol mitigation as a modifiable risk factor.”
Zirulnik A, Liu S, Wells M, et al. Alcohol use is associated with intracranial hemorrhage in older emergency department head trauma patients. JACEP Open. 2024; 5:e13245. https://doi.org/10.1002/emp2.13245
Category: Gastrointestional
Posted: 8/13/2024 by Neeraja Murali, DO, MPH
(Updated: 8/14/2024)
Click here to contact Neeraja Murali, DO, MPH
This study, done out of Australia, examined the association between abdominal pain and severity of liver injury in patients presenting after acute acetaminophen overdose.
539 cases were identified where N-acetylcysteine was administered to patients with acetaminophen overdose. The investigators explored parameters including presence of abdominal pain, time post-ingestion, and peak ALT.
Patients less than 8 hours post overdose WITH abdominal pain were as likely to develop hepatotoxicity as those presenting WITHOUT abdominal pain. (OR=1.18 [0.07 to 19.4])
Patients presenting 8 or more hours post overdose WITH abdominal pain were as likely to develop hepatotoxicity as those WITHOUT abdominal pain (OR=1.28 [0.39 to 4.21])
Don't let lack of pain fool you! Just as we all learned in medical school - let your history be your guide!
Wang C, Wong A. The presence of abdominal pain associated with acetaminophen overdose does not predict severity of liver injury. Am J Emerg Med. 2024;79:52-57. doi:10.1016/j.ajem.2024.02.011
Category: Critical Care
Keywords: DKA (PubMed Search)
Posted: 8/13/2024 by Jordan Parker, MD
Click here to contact Jordan Parker, MD
Diabetic ketoacidosis (DKA) is a serious condition that carries the risk of significant morbidity and mortality if not managed appropriately. Typically managed with an infusion of regular insulin, IV fluids, and electrolytes, there is evidence to support treatment of mild to moderate DKA with a subcutaneous (SQ) regimen using a combo of fast-acting and long-acting insulin instead, decreasing the need for ICU admission without increasing adverse events [1].
What patients?
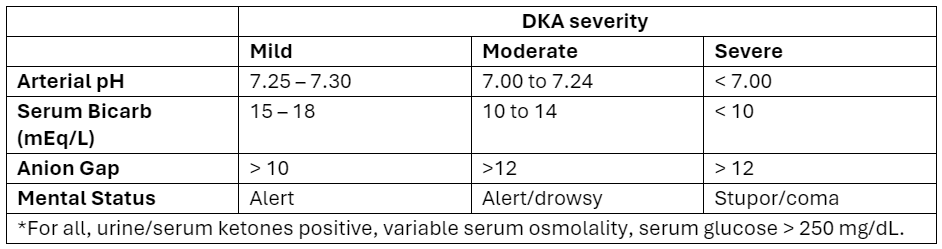
Adapted from Abbas et al.
How to manage?
Initial dose
Subsequent dosing:
If serum glucose is > 250 mg/dL
If serum glucose is < 250 mg/dL
Bottom Line
DKA management with a SQ insulin protocol is a reasonable approach for patients with mild to moderate DKA, is supported by the American Diabetes Association [5], and can be particularly helpful in this era of ED boarding and bed shortages. Give a long-acting insulin dose every 24 hours (or restart the patient’s home long-acting regimen) and short-acting insulin every 2 to 4 hours. Aggressive IV fluid resuscitation, electrolyte repletion, and treatment of underlying precipitating cause remain additional cornerstones of DKA management.
Category: Trauma
Keywords: Cspine, nexus, Canadian, rule (PubMed Search)
Posted: 8/9/2024 by Robert Flint, MD
(Updated: 8/12/2024)
Click here to contact Robert Flint, MD
A reminder of two validated tools used to determine the need for cervical spine imaging in adult blunt trauma patients. A recent meta analysis concluded:
“Based on studies, both CCR and NEXUS were sensitive rules that have the potential to reduce unnecessary imaging in cervical spine trauma patients. However, the low specificity and false-positive results of both of these tools indicate that many people will continue to undergo unnecessary imaging after screening of cervical SCI using these tools. In this meta-analysis, CCR appeared to have better screening accuracy.”
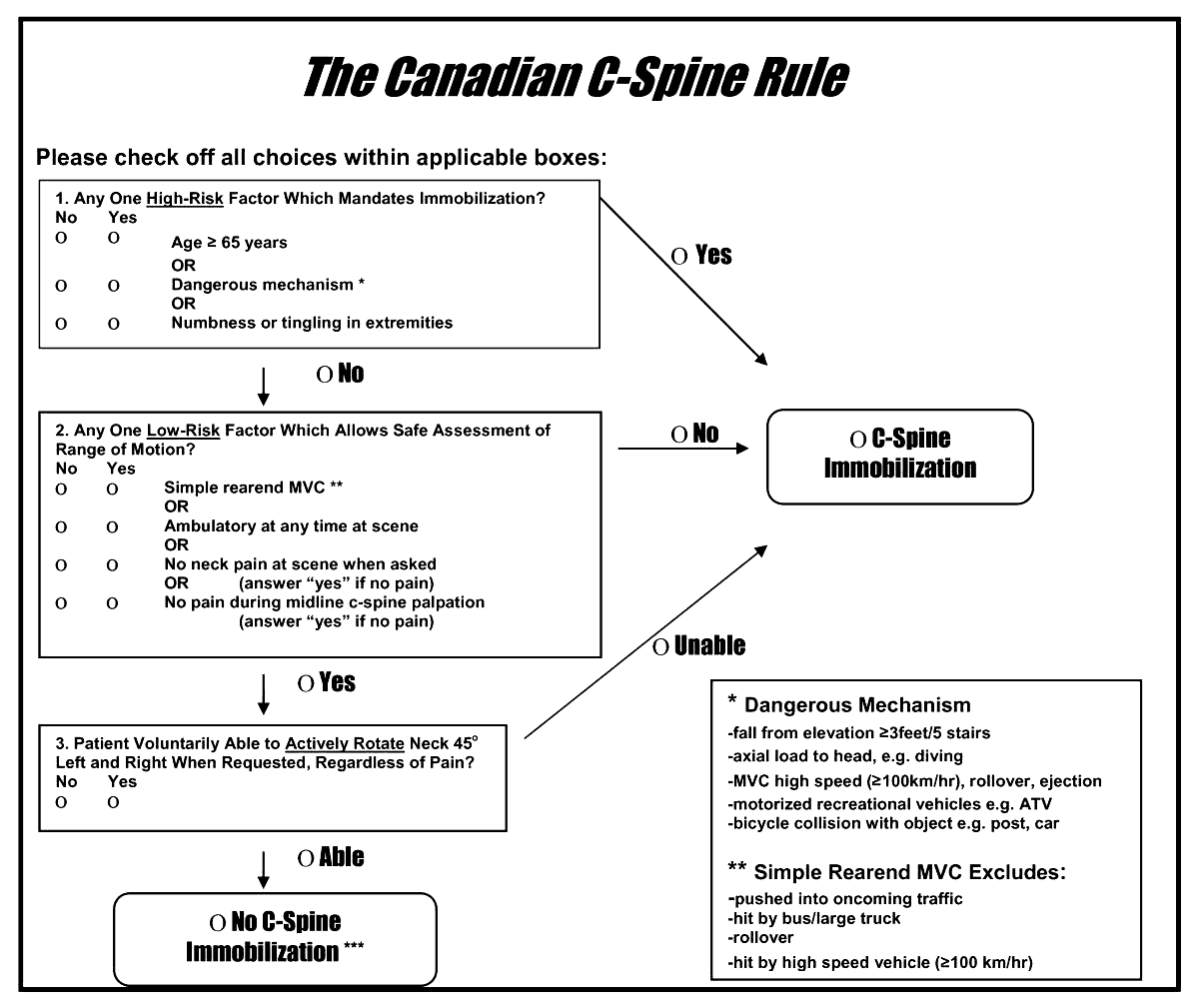
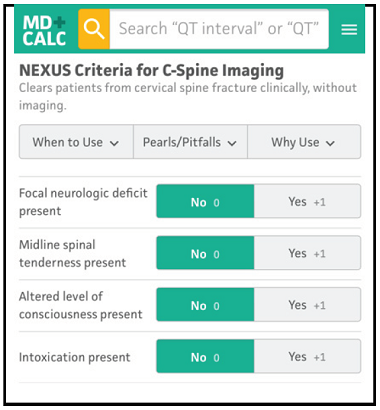
Arch Acad Emerg Med. 2023; 11(1): e5.
Published online 2023 Jan 1. doi: 10.22037/aaem.v11i1.1833
PMCID: PMC9807951
PMID: 36620739
Canadian C-spine Rule versus NEXUS in Screening of Clinically Important Traumatic Cervical Spine Injuries; a systematic review and meta-analysis
Category: Trauma
Keywords: Cspine, pecarn, rule, injury (PubMed Search)
Posted: 8/9/2024 by Robert Flint, MD
(Updated: 8/11/2024)
Click here to contact Robert Flint, MD
A just released study published in the Lancet gives us guidance on which pediatric blunt trauma patients need cervical spine imaging. Age range was 0-17 years.
“Out of 22,430 children included in the study, 433 (1.9%) were found to have Cervical spine injury (CSI). The study identified 4 high risk factors for CSI to be used to triage children to CT (12% risk for a cervical spine injury):
In children without high-risk findings, 5 additional findings identified children with intermediate, non-negligible risk of CSI (3.6% risk of a cervical spine injury):
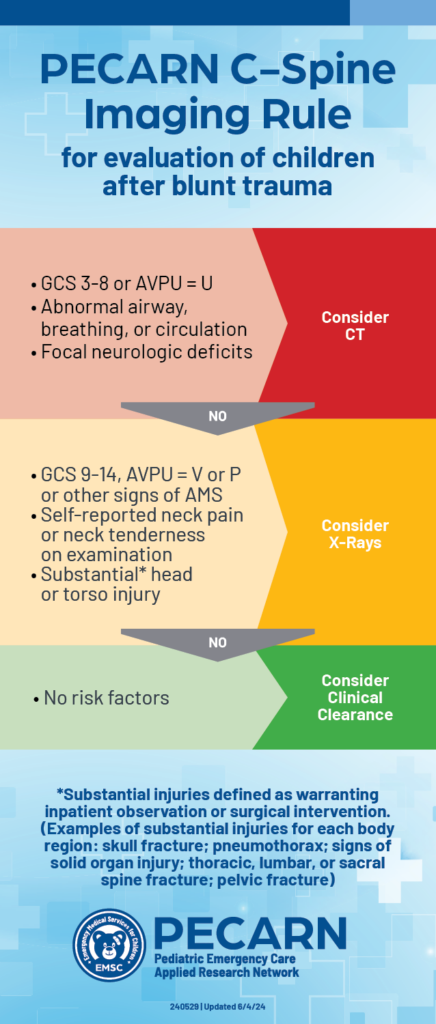
PECARN prediction rule for cervical spine imaging of children presenting to the emergency department with blunt trauma: a multicentre prospective observational study
Prof Julie C Leonard, MD Monica Harding, MS Prof Lawrence J Cook, PhD Prof Jeffrey R Leonard, MD
Prof Kathleen M Adelgais, MD Fahd A Ahmad, MD et al.
Published:June 03, 2024DOI:https://doi.org/10.1016/S2352-4642(24)00104-4
2. https://pecarn.org/pecarn_news/clinical-decision-rule-cervical-spine/
Category: Orthopedics
Posted: 8/10/2024 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
The Lever test can be used to examine for a torn ACL
May be helpful when examining larger patients
Place patient supine with both knees extended. Examiner places fist below the proximal third of patient’s calf.
With the other hand, the examiner presses down on the distal third of the patient’s quadriceps.
Positive test: A torn ACL disrupts the lever arm of the lower leg. The heel will not rise.
Negative test: An intact ACL allows the lever arm of the lower leg to lift the heel. The heel will rise.
More study is needed but reported sensitivities are similar to classic tests such as the anterior drawer or Lachman.
Category: Obstetrics & Gynecology
Keywords: breastfeeding, lactation (PubMed Search)
Posted: 8/7/2024 by Ashley Martinelli
(Updated: 8/8/2024)
Click here to contact Ashley Martinelli
Breastfeeding provides a great nutrition source for infants, but early cessation is common for a wide variety of reasons. Notably, being asked to withhold breastmilk (“pump and dump”) due to safety concerns or illness increases rates of termination.
A recent paper is an invaluable reference on commonly used medications in the care of emergency department women of childbearing age and the lactation risk. It breaks down medications into clinical categories and then further highlights those that are safe, likely safe, and safe-but may reduce milk supply, and those to avoid.
The majority of commonly used medications in the ED are safe to use in breastfeeding. Only 3% of the medication analyzed should be avoided (aspirin [at doses > 325mg/day], dicyclomine, prochlorperazine, and benzonatate) and in most cases a safe alternative could be used.
Using these recommendations can help prescribe safe medications, prevent the recommendations to pump and dump, and relieve stress for the patient breastfeeding.
Consider adding the LactMed(R) app to your phone as well - This is a free database through the NIH to search individual medications to assess risk in lactation.
Premer C, Caruso K. Safety profile of the most ordered medications for breastfeeding patients in the emergency department. Am J Emerg Med. 2024;80:1-7.
Category: EMS
Keywords: EMS, cardiopulmonary resuscitation, CPR, emergency medical services (PubMed Search)
Posted: 8/8/2024 by Ben Lawner, MS, DO
Click here to contact Ben Lawner, MS, DO
BACKGROUND:
Cardiac arrest is time sensitive disease. Despite significant advances in resuscitation technology such as eCPR and mechanical compression devices, early basic life support interventions (specifically bystander CPR) are strongly associated with survival. EMS systems must advocate for early initiation of bystander CPR. Dispatch Assisted CPR (DA-CPR) is one of several strategies designed to improve outcomes and encourage early compressions. To optimize survival, EMS systems should achieve a comprehensive understanding about barriers to succesful initiation of DA-CPR.
METHODS AND OUTCOMES:
49,165 patients with out of hospital cardiac arrest were eligible for inclusion the study, and over 36,000 underwent successful DA-CPR. The study's primary outcome was good neurological recovery at hospital discharge. Secondary outcomes included: prehospital return of spontaneous circulation (ROSC)and survival to hospital discharge. The authors defined successful DA-CPR when bystanders initiated compressions and continued resuscitation until the arrival of EMS.
RESULTS:
Quite a few results were consistent with prior studies. Unsuccessful DA-CPR was associated with:
Successful DA-CPR was more likely associated with the presence of family members at the scene and improved neurological recovery. Witnessed arrests were also more likely to receive successful DA-CPR. Not surpringly, patients in the successful DA-CPR group also exhibited improved survival to discharge and prehospital ROSC.
BOTTOM LINE:
Though the study is retrospective and involves a host of confounding variables, EMS systems continue to identify modifiable factors linked to the delivery of DA-CPR. Improved community CPR education and dispatcher training may contribute to higher DA-CPR rates.
BALTIMORE, MD, SPECIFIC PEARL:
Baltimore metropolitan jurisdictions are collaborating with the CPR LifeLinks program to address DA-CPR. The CPR LifeLinks program a national initiative “to help communities save more lives through implementation of telecommunicator and high performance CPR programs." https://www.911.gov/projects/cpr-lifelinks/
Park DH, Park GJ, Kim YM, Chai HS, Kim SC, Kim H, Lee SW. Barriers to successful dispatcher-assisted cardiopulmonary resuscitation in out-of-hospital cardiac arrest in Korea. Resusc Plus. 2024 Jul 19;19:100725. doi: 10.1016/j.resplu.2024.100725. PMID: 39091585; PMCID: PMC1129358
