Category: Misc
Keywords: prescribing, racial, disparity (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/28/2025)
Click here to contact Robert Flint, MD
Comparing prescribing patterns from early 2000s to late 2010s in the National Hospital Ambulatory Medical Care Survey, these authors found we continue to under prescribe pain medications to non-white patients for traumatic injuries.
Day, Jessica et al.
Journal of Emergency Medicine, Volume 78, 184 - 191
Category: Misc
Keywords: Neck pain, crowned dens syndrome (PubMed Search)
Posted: 12/22/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
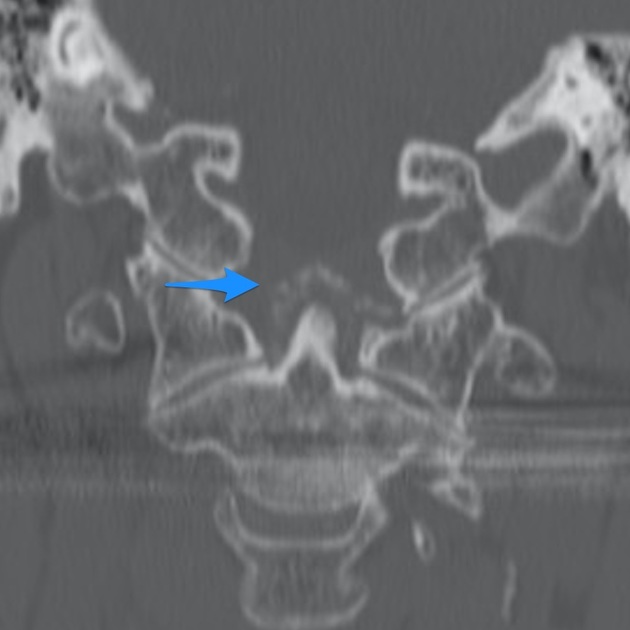
Crowned dens syndrome is an acute inflammatory disease caused by deposition of calcium pyrophosphate dihydrate crystals or hydroxyapatite crystals in the soft tissue and ligaments surrounding the dense. Patient presentation is severe pain in the neck and base of the skull, low grade fever, and elevated inflammatory markers. It is most commonly seen in elderly females. Ct scan is the gold standard for diagnosis. Once meningitis and other significant infectious process has been excluded, treatment is anti inflammatory medications including steroids.
Category: Misc
Keywords: sample size calculation, biostatistics (PubMed Search)
Posted: 7/25/2024 by Mike Witting, MS, MD
(Updated: 2/8/2026)
Click here to contact Mike Witting, MS, MD
Free Biostatistics Software Options
EpiCalc 2000 – available for Windows. Capabilities include sample size calculation, inferential statistics (p values, 95% CI), simple stratified analysis, paired and independent analyses. Right clicking allows you to do many things. (http://www.brixtonhealth.com/epicalc.html). I've had the most experience with this one.
Epi Info – supported by CDC. Available for Windows and for hand-held. (https://www.cdc.gov/epiinfo/index.html)
P/S – Power and Sample Size Calculation – available for Mac and Window. Supported by Vanderbilt biostatistics. (https://biostat.app.vumc.org/wiki/Main/PowerSampleSize)
Epicalc: http://www.brixtonhealth.com/epicalc.html
Epi Info: https://www.cdc.gov/epiinfo/index.html
Category: Misc
Posted: 6/29/2024 by Mike Witting, MS, MD
(Updated: 2/8/2026)
Click here to contact Mike Witting, MS, MD
Needed for sample size determination
Power – (1-beta), where beta is the risk of a type 2 error – rejecting the accepting the null hypothesis when it is true – this is usually selected to be 0.8 or 0.9.
Significance (alpha), the chance of making a type 1 error – accepting the alternate hypothesis when the null hypothesis is true. This is usually selected to be 0.05.
One-tailed or two-tailed – is the null hypothesis one of no difference (experimental arm not better or worse) or one-sided (experimental arm not better)?
Effect Size. This is the challenging part. This is the size of the difference in outcomes you’re looking for.
For continuous outcomes (example – difference in pain scores). You’ll need an estimate for the variation in the scores between presentations, or the standard deviation. You can get this from a literature estimate or a from small local measurement, say of 10 patients or so.
For a dichotomous outcome (example – percentage of successes), you can usually estimate the percentage in one group and choose the difference you are looking for.
The effect size has a big effect on the sample size. Generally, cutting the effect size in half increases the sample size by fourfold.
Statistical software - next pearl.
Category: Misc
Keywords: sleep (PubMed Search)
Posted: 5/29/2024 by Visiting Speaker
(Updated: 2/8/2026)
Click here to contact Visiting Speaker
Title: Basics of Sleep Physiology and Architecture
By: Youssef Annous, MD
Sleep is integral for physical and mental health and performance. Sleep is extremely well conserved among species. All mammals need sleep to survive.1 A single sleep cycle typically lasts anywhere between 90 and 120 minutes and is broken down into two phases2:
Non-Rapid Eye Movement sleep
Stage 1 (Light Sleep)
This is the lightest form of sleep and the easiest to wake up from. During this stage, it is normal to experience muscle twitching and the sensation of drifting in and out of consciousness. This stage lasts approximately 5 minutes in the beginning of sleep and comprises around 5% of total sleep duration.2
Stage 2 (Light Sleep)
During this stage, you are likely to begin experiencing decrease in body temperature, heart rate (HR), blood pressure (BP) and respiratory rate (RR). Electroencephalography (EEG) during this phase of sleep would show sleep spindles and K complexes.2 These findings have been linked to memory consolidation.3
Stage 3 (Deep Sleep)
This is the deepest stage of sleep. During this phase, body temperature, HR, BP, and RR are at their lowest. This is the most restorative stage of sleep. It is essential for immune health, cardiovascular health, tissue repair, bone growth, and muscle recovery.2 It is also when growth hormone (GH) is at its highest. Physiological (e.g. illness) or psychological (e.g. anxiety) stressors can negatively impact this stage. We experience less deep sleep as we age.4
Rapid Eye Movement (REM) sleep
This stage of sleep is characterized by rapid eye movement, abundance of dreaming and heightened brain activity. During REM, there is total body paralysis with exception of ocular and respiratory muscles. It is theorized that your body is paralyzed during this stage to protect you from dream enactment. You experience more REM the longer you sleep. REM has been shown to be essential for memory consolidation, cognitive function, mood regulation and for coping with stress. This stage is particularly compromised by sedatives including but not limited to alcohol, benzodiazepines, and tetrahydro-cannabinoid (THC). Several studies in animals and humans showed that even modest REM sleep deprivation can result in increased mortality. 2,5,6
All sleep stages are extremely essential. Be careful of self-medicating with sleep aids such benzodiazepines or alcohol as this can be detrimental for your health. In later UMEM pearls, we will discuss protocols, supplements and behavioral ways to improve each stage of sleep for better mental and physical health.
References:
1 Miyazaki S, Liu C-Y, Hayashi Y. Sleep in vertebrate and invertebrate animals, and insights into the function and evolution of sleep. Neuroscience Research. 2017;118:3-12. doi:10.1016/j.neures.2017.04.017
2 JF; PAVK. Physiology, sleep stages. National Center for Biotechnology Information. Accessed May 26, 2024. https://pubmed.ncbi.nlm.nih.gov/30252388/.
3 Antony JW, Schönauer M, Staresina BP, Cairney SA. Sleep spindles and memory reprocessing. Trends in Neurosciences. 2019;42(1):1-3. doi:10.1016/j.tins.2018.09.012
4 El Shakankiry H. Sleep physiology and sleep disorders in childhood. Nature and Science of Sleep. Published online September 2011:101. doi:10.2147/nss.s22839
5 Della Monica C, Johnsen S, Atzori G, Groeger JA, Dijk D-J. Rapid eye movement sleep, sleep continuity and slow wave sleep as predictors of cognition, mood, and subjective sleep quality in healthy men and women, aged 20–84 years. Frontiers in Psychiatry. 2018;9. doi:10.3389/fpsyt.2018.00255
6 Leary EB, Watson KT, Ancoli-Israel S, et al. Association of Rapid Eye Movement Sleep with mortality in middle-aged and older adults. JAMA Neurology. 2020;77(10):1241. doi:10.1001/jamaneurol.2020.2108
Category: Misc
Keywords: Research Question (PubMed Search)
Posted: 5/20/2024 by Mike Witting, MS, MD
Click here to contact Mike Witting, MS, MD
Starting a study? Frame your research question in the PICO format:
Patients (consider severity of presentation, setting, demographics)
Intervention (either something you propose or something in use)
Comparison (another group, the same group without intervention, or a benchmark)
Outcome (a measurement)
This classic format has been used to evaluate studies, as in Journal Club (by our esteemed Dr. Wilkerson), as a literature search tool, or by the Cochrane review.
Starting with a PICO research question can help you narrow your focus and maintain it.
Category: Misc
Posted: 3/26/2024 by Heidi Teague, MD
(Updated: 3/30/2024)
Click here to contact Heidi Teague, MD
Advancements in complex illness management have led to an increasing number of patients surviving longer, with subsequent development of end-stage organ disease, cancer, and dementia. EDs are encountering patients with more complex medical needs who present with challenging complaints such as functional loss, bounce-back visits for uncontrolled symptoms, and caregiver fatigue. ACEP underscored the importance of advancing access to palliative care in 2013 and is one of its top five measures in the Choosing Wisely campaign, aimed at minimizing unwarranted and excessive medical interventions. Proactive symptom management, including promptly addressing pain, dyspnea, nausea, and other distressing symptoms, as well as goals of care conversations, and early referral to hospital and outpatient palliative services can enhance patient and caregiver comfort and quality of life.
Wang DH. Beyond Code Status: Palliative Care Begins in the Emergency Department. Annals of emergency medicine. 2017;69(4):437-443. doi:10.1016/j.annemergmed.2016.10.027
Category: Misc
Posted: 3/12/2024 by Mike Witting, MS, MD
(Updated: 3/28/2024)
Click here to contact Mike Witting, MS, MD
Considering starting a research project? Apply the FINER criteria:
Feasible
Do you have the resources to study this? Enough patients? Support?
Interesting
Does it interest you enough to devote your time to it? Does it interest colleagues?
Novel
Would it provide new findings, or confirm, refute, or extend prior findings?
Ethical
Can you think of a way to ethically study it?
Relevant
Consider possible outcomes of your research. Could the study advance care or policy?
Adapted from Hulley SB, Cummings SR. Designing clinical research, 4th edition, Lippincott, Williams and Wilkins, 2013.
Category: Misc
Posted: 2/10/2024 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Ever see a commercial showing active fit people drinking sugar beverages?
Ever wonder if exercise is protective from the effects of added sugar?
What are the health risks of added sugar?
How much is too much?
C. elegans, a roundworm, shares 40% of its genes with humans
-Frequently used as a model for health and longevity research
In a 2021 study, researchers altered the diet of the roundworms and found that added sugar was linked to increased glycation end products, high levels of which are associated with an increased risk of CV disease, diabetes and Alzheimer’s disease.
Foods such as fruits are high in natural sugars. Added sugars however are “added” by manufactures to increase flavor.
In our diet, added sugars are everywhere from white bread to ketchup to your favorite Starbucks beverage.
-Sugar- sweetened beverages are the largest source of added sugars in the American diet.
In 2016 the FDA added a section on nutritional labels for added sugars.
The CDC advises limitation of added sugars to 10% of total daily caloric intake.
Added sugars (vs. natural sugars) are more likely to cause spikes in blood sugar and create an inflammatory state thereby increasing the risk of numerous medical problems.
A recent study from the Harvard school of public health investigated whether the benefits of physical activity outweigh the risks of CV disease associated with consumption of sugar-sweetened beverages.
Using 2 cohorts (100,000 people) over a 30-year period, those who consumed sugar-sweetened beverages more than twice a week had a higher risk of CV disease.
Those with daily consumption were at higher risk.
Even those that hit the recommended 150 minutes of weekly exercise were not protected.
Physical activity only reduced the risk of CV disease by approximately 50%.
Though the study did not specifically look at sports and energy drinks, these beverages are large sources of added sugars.
For example, A 20-ounce Gatorade's Thirst Quencher contains 36g of sugar.
Take home: Added sugar, even in moderation, may have negative health consequences even in individuals who exercise regularly.
Category: Misc
Keywords: POCUS (PubMed Search)
Posted: 9/18/2023 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Point of Care Ultrasound has been shown to change medical management and decrease time to diagnosis.
However, sometimes on a busy shift we may get an xray or radiological study prior to performing a POCUS exam due to time constraints.
A recent study looked at the time it takes to perform a bedside ultrasound.
The authors measured the duration of time from starting the exam through the ultrasound worklist to the timestamp on the last recorded image.
They reviewed 2144 studies and found a median time of 6 minutes to perform a study.
Of course the study is limited by the time it takes to find a machine, make sure it is functioning and other supplies such as gel.
Conclusion: You can take 6 minutes to assist in your patient's clinical care.
Patrick DP, Bradley XG, Wolek C, Anderson B, Grady J, Herbst MK. Minutes matter: Time it takes to perform point-of-care ultrasound. AEM Educ Train. 2023 Aug 18;7(4):e10901. doi: 10.1002/aet2.10901. PMID: 37600853; PMCID: PMC10436032.
Category: Misc
Keywords: EMS, Alternate destinations, pediatric, EMS, reduce transport times (PubMed Search)
Posted: 5/17/2023 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Ward CE, Singletary J, Campanella V, Page C, Simpson JN. Caregiver Perspectives on Including Children in Alternative Emergency Medical Services Disposition Programs: A Qualitative Study [published online ahead of print, 2023 May 5]. Prehosp Emerg Care. 2023;1-9. doi:10.1080/10903127.2023.
Category: Misc
Keywords: hydration, mortality (PubMed Search)
Posted: 1/28/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
In a recent study in The Lancet, researchers at NIH attempted to test the hypothesis that optimal hydration may slow down the aging process.
A large proportion of people do not consume the recommended fluid amounts. This has likely become worse with our masking during the pandemic.
Previous studies in a mouse model showed that water restriction, increasing serum sodium by 5 mmol/l, shortened the mouse lifespan by 6 months which corresponds to about 15 years of human life.
Population: Data from Atherosclerosis Risk in Communities (ARIC) study: an ongoing population-based prospective cohort study in which 15,792 45-66 year-old black (African American) and white men and women were enrolled from four US communities in 1987–1989 and followed up for more than 25 years.
Variables: 15 biomarkers and serum sodium (as a proxy for the hydration habits of study participants).
They attempted to exclude people whose serum sodium could be affected by factors other than the amount of liquids they consume. After these exclusions, 11,255 participants remained in the datase.
Authors also calculated ones biologic age by sampling 15 biomarkers characterizing performance of multiple organ systems and processes: cardiovascular (systolic blood pressure), renal (eGFR, cystatin-C, urea nitrogen, creatinine, uric acid), respiratory (FEV), metabolic (glucose, cholesterol, HbA1c, glycated albumin, fructosamine), immune/inflammatory (CRP, albumin, beta 2-microglobulin).
Conclusions: The analysis showed that middle age serum sodium >142 mmol/l is associated with a 39% increased risk to develop chronic diseases (hazard ratio [HR] = 1.39, 95% confidence interval [CI]:1.18–1.63) and >144 mmol/l with 21% elevated risk of premature mortality (HR = 1.21, 95% CI:1.02–1.45). People with serum sodium >142 mmol/l had up to 50% higher odds to be older than their chronological age (OR = 1.50, 95% CI:1.14–1.96).
Limitations: Observational study. No firm conclusions without intervention studies.
Summary: Serum sodium concentration exceeding 142 mmol/l is associated with increased risk to be biologically older, develop chronic diseases and die at younger age.
Take home: Drink more water
Dmitrieva NI, Gagarin A, Liu D, Wu CO, Boehm M. Middle-age high normal serum sodium as a risk factor for accelerated biological aging, chronic diseases, and premature mortality. EBioMedicine. 2023 Jan;87:104404.
Category: Misc
Keywords: Aging, mortality, physical activity (PubMed Search)
Posted: 1/14/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Humor me and imagine that your birth certificate vanished, and your age was based on the way you feel inside. How old would you say you are (subjective age) versus your actual age?
In a few studies, those individuals reporting a younger subjective age had a lower risk of depression, greater mental well-being, better physical health, and a lower risk of dementia. These individuals also had improved episodic memory and executive functioning. Subjective age also predicts incident hospitalization.
Three longitudinal studies tracked more than 17,000 middle aged and elderly individuals.
Over a 20-year period, researchers tracked: Subjective age, demographic factors, disease burden, functional limitations, depressive symptoms, and physical inactivity.
Researchers found that those who felt approximately 8, 11, and 13 years older than their actual age had an 18%, 29%, and 25% higher risk of mortality, respectively. They also had a greater disease burden even after controlling for demographic factors such as education, race and marital status. Multivariable analyses showed that disease burden, physical inactivity, functional limitations, and cognitive problems, but not depressive symptoms, accounted for the associations between subjective age and mortality.
This study provides evidence for an association between an older subjective age and a higher risk of mortality across adulthood. These findings support the role of subjective age as a biopsychosocial marker of aging. This may allow for early intervention for select individuals who may have a higher association with poor health outcomes.
Your subjective age can better predict your overall health than the date on your birth certificate.
Stephan Y, Sutin AR, Terracciano A. Subjective Age and Mortality in Three Longitudinal Samples. Psychosom Med. 2018 Sep;80(7):659-664.
Category: Misc
Keywords: Health policy, healthcare (PubMed Search)
Posted: 1/7/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
These two pieces from Becker’s Hospital Review demonstrate significant areas of weakness within the American healthcare system. Hospitals that care for underserved as well as medically and socially complicated patients should be afforded protection and financial security. Not only do they care for the most complex patients, they often educate the next generation of health care providers.
The loss of small community or rural hospitals also has a major negative impact on the US health care system. For time sensitive conditions such as trauma, myocardial infarction or stroke these facilities are often the first, closest facility to initiate care or stabilization. The loss of these critical smaller hospitals also adds to the burden at already overwhelmed larger facilities.
As medical providers, we are in a unique position to advocate for our patients, our co-workers and our communities. Join your professional societies (ACEP, AAEM, SAEM etc.), write your local and national representatives, find like minded colleagues, please get involved with the process any way you can. As a nation we can not afford to lose large essential hospitals or small critical access, rural hospitals.
Category: Misc
Keywords: human rights (PubMed Search)
Posted: 12/26/2022 by Rachel Wiltjer, DO
Click here to contact Rachel Wiltjer, DO
Universal Human Rights
Human rights are rights inherent to all human beings, whether our nationality, place of residency, sex, national or ethnic origin, color, religion, language defines , or any other status
The United Nations Human Rights Council (UNHRC) defines seven substantive rights: the right to life, freedom from torture, freedom from slavery, right to a fair trial, freedom of speech, freedom of thought, conscience and religion, and freedom of movement
The right to life is the essential right that a human being has a right not to be killed by another human being. This has been central in debates on issues of abortion and euthanasia.
Emergency care is an often overlooked, but essential component of the right to life in the highest attainable standard of health and universal health coverage (UHC - a WHO description used to describe access to care). Particularly for vulnerable and disadvantaged populations, emergency care is often the last chance for the health system to save a life.
The focus on vulnerable populations with little access to care and subsequent poor health outcomes has many similarities to the delivery of emergency care. Emergency conditions, such as traumatic injuries, disproportionately affect people in low- and middle-income countries. About 90% of the burden of death and disability from injuries occurs in low- and middle-income countries
COVID-19 emphatically highlighted how far countries (and differences in regulations between states in the US) are from meeting the supreme human rights command of non-discrimination, from achieving the highest attainable standard of health that is equally the right of all people everywhere, and from taking the human rights obligation of international assistance and cooperation seriously.
Implementation of a rights-based framework for emergency care requires countries to enact legislation that ensures access to non-discriminatory emergency care and establish a regulatory body with appropriate oversight and authority to enforce these laws.
Category: Misc
Keywords: Intimate Partner Violence (PubMed Search)
Posted: 11/7/2022 by Rachel Wiltjer, DO
Click here to contact Rachel Wiltjer, DO
IPV can occur once or over years by a current or former romantic partner. Types of IPV include: Physical and/or Sexual violence, Stalking, and Psychological/Financial aggression (the use of verbal and non-verbal communication to harm mentally or emotionally and to exert control over another partner).
IPV is more prevalent that Aortic Dissection and Pulmonary Embolism combined. Think about how risky it is to NOT recognize IPV.
1:4 women and 1:10 men have been victims of IPV during their lifetime.
1:5 homicide victims are killed by an intimate partner.
Over 50% of female homicide victims are killed by a current or former intimate partner. Patients who have been strangled are 4 times more likely to be killed within a year.
Your Spidey Sense should go off when:
Once patient is identified as a victim:
Category: Misc
Keywords: Migrant Health (PubMed Search)
Posted: 8/28/2022 by Rachel Wiltjer, DO
Click here to contact Rachel Wiltjer, DO
Approximately 284,000 immigrants reside in Baltimore (10% of the total population). In April 2022, Governor Abbott of Texas began sending migrants from the US southern border to Washington, DC, with Arizona joining soon after. It is important for emergency providers to be aware of these changes and how new disparities may arise.
2. Assess acute vs non-acute needs: A study done in pediatric migrant populations suggests that the severity of the reasons for visiting the ED and the hospitalization rates were not higher in the pediatric migrant population than in the general pediatric population. Some common non-urgent diagnoses include scabies, anemia, oral and dental disorders.
3. Create a safe environment: In a study done in 2013, up to 12% of undocumented immigrants that presented to the ED expressed fear of discovery and consequent deportation. On further assessment there was the belief that medical staff are required to report these patients to immigration. It is important to proactively address inaccurate beliefs to promote a safe trusting environment.
Resources in Baltimore/Maryland:
-CASA
-Esperanza Center
-International Rescue Committee
- John's Hopkins Centro Sol
- National Immigration Law Center
National Resources (US):
-Rural Health Information Hub
-National Resource Center for Refugees, Immigrants, and Migrants
Mahmoud I, Eley R, Hou XY. Subjective reasons why immigrant patients attend the emergency department. BMC Emerg Med. 2015 Mar 28;15:4.
Maldonado CZ, Rodriguez RM, Torres JR, Flores YS, Lovato LM. Fear of discovery among Latino immigrants presenting to the emergency department. Acad Emerg Med. 2013 Feb;20(2):155-61.
Tarraf W, Vega W, González HM. Emergency department services use among immigrant and non-immigrant groups in the United States. J Immigr Minor Health. 2014 Aug;16(4):595-606.
Category: Misc
Posted: 1/20/2021 by Michael Bond, MD
Click here to contact Michael Bond, MD
Title: Mammalian meat allergy (alpha-gal syndrome) following tick bites
Author: Dan Gingold, MD, MPH
Development of IgE antibodies to the oligosaccharide galactose-alpha-1-3-galactose (alpha-gal) appears to be responsible for an acquired allergy to non-primate mammalian meat (i.e., beef and pork) and derived products. Antigen in the salivary apparatus of certain ticks (gross!!) can sensitize an IgE-mediated response to alpha-gal which is present in mammalian meat.
Symptoms are similar to other IgE-mediated hypersensitivity reactions, and can cause a delayed-onset reaction with hives, GI upset, or anaphylaxis after ingestion of red meat. Treatment with standard anti-histamines and epinephrine is effective. Individuals with no prior history of meat sensitivity can develop the syndrome at any age, often after exposure to the outdoors in tick-endemic areas. Skin and blood allergy testing can confirm the diagnosis. Symptoms can persist for years, but can recede over time if not exposed to further tick bites.
In the US, the primary tick responsible is Lone Star Tick (Amblyomma americanum), found primarily in the Eastern, Southeastern, and Midwestern US. Other tick species in Europe, Australia, and Asia have been found to induce the syndrome as well. Interestingly, there is a cross-reactivity with the monoclonal antibody Cetuximab (used to treat colorectal and head and neck cancers), an allergic reaction to which can also induce similar alpha-gal meat sensitivity.
Having first been described in 2009, the syndrome often goes unrecognized; increased physician awareness can inform the evaluation, diagnosis, and education of patients presenting to the ED with undifferentiated allergic reaction.
Further Reading:
Khoury JK, Khoury NC, Schaefer D, Chitnis A, Hassen GW. A tick-acquired red meat allergy. Am J Emerg Med. 2018 Feb;36(2):341.e1-341.e3. doi: 10.1016/j.ajem.2017.10.044. Epub 2017 Oct 16. PMID: 29074067.
Crispell G, Commins SP, Archer-Hartman SA, Choudhary S, Dharmarajan G, Azadi P, Karim S. Discovery of Alpha-Gal-Containing Antigens in North American Tick Species Believed to Induce Red Meat Allergy. Front Immunol. 2019 May 17;10:1056. doi: 10.3389/fimmu.2019.01056. PMID: 31156631; PMCID: PMC6533943.
Category: Misc
Keywords: CT, head, radiation (PubMed Search)
Posted: 4/13/2019 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Most (65%) scans were performed at nonacademic adult centers
Strauss et al., 2019. Radiation Dose for Pediatric CTT: Comparison of Pediatric versus Adult Imaging Facilities
Category: Misc
Keywords: dental pain, ibuprofen, acetaminophen (PubMed Search)
Posted: 4/6/2018 by Michael Bond, MD
Click here to contact Michael Bond, MD
