Category: Geriatrics
Keywords: Geriatrics, frailty, screening (PubMed Search)
Posted: 5/27/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
This Delphi study and companion editorial highlight current thought on frailty screen in emergency department patients. Key takeaways are:
Emergency departments should be instituting procedures that incorporate screening older patients for frailty. These references are a good starting point.
Category: Trauma
Keywords: Lefort, facial, trauma, fracture (PubMed Search)
Posted: 5/26/2024 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
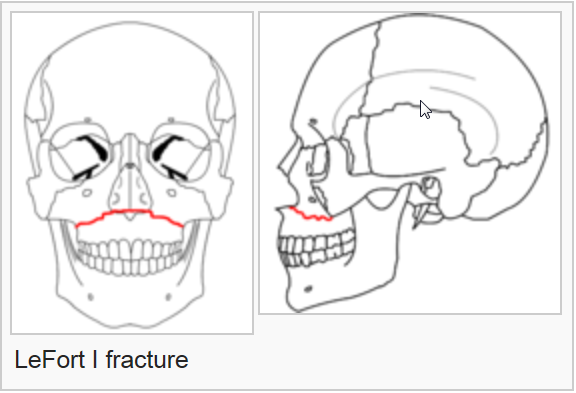
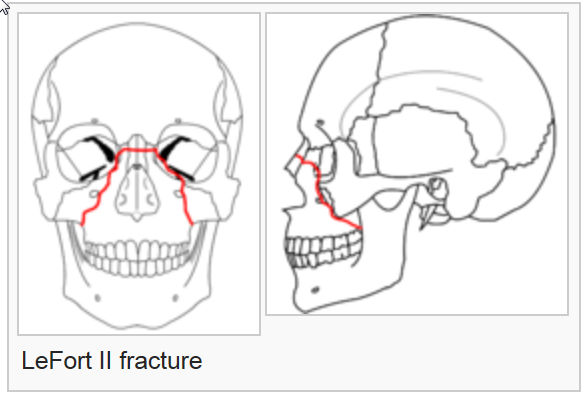
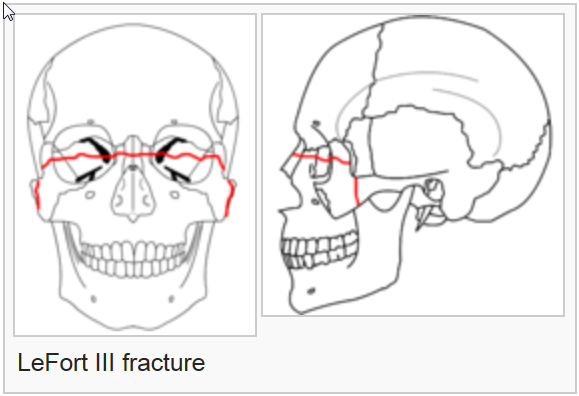
On exam, assess for facial instability and airway patency. CT scan is the imaging of choice. The higher the number, the more complex the fracture, the more unstable and the more difficult the airway managment will be. Look for open lacerations or blood in the sinuses and treat with antibiotics if these are found. Consult ENT or plastics urgently for further management.
The reference is a nice review of these fractures
Category: Orthopedics
Posted: 5/25/2024 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
A recent study in Annals of EM investigated the use of topical Diclofenac in the treatment of lower back pain.
Small studies have shown topical NSAIDs to be effective for single joint OA and tendinopathies.
Currently, NSAIDs are first-line treatment for ED patients with acute low back pain.
Theoretically, topical NSAIDs deliver medications directly to the injured tissue while minimizing systemic side effects.
-Topical NSAIDs provide similar concentrations of the drugs in muscle tissue but much lower plasma concentrations than oral formulations
Design: Randomized, double-blind, placebo-controlled trial.
ED patients aged 18 to 69 years with non-radicular, non-traumatic acute lower back pain.
Screened 3,281 and enrolled 198.
Study groups:
Patients received 2 days of meds. Follow up by phone at 2 and 7 days.
Investigators used the RMDQ score to measures pain and functional impairment.
Results: At the 2 day follow-up, all 3 groups showed an improvement in the mean RMDQ score compared to baseline as expected.
Participants had a mean RMDQ improvement of 10.1 in the ibuprofen group, 6.4 in the diclofenac gel group, and 8.7 in the ibuprofen + diclofenac gel group.
At the 7-day follow-up, participants had a mean RMDQ change compared to baseline of 12.2 in the ibuprofen group, 9.5 in the diclofenac group, and 10.7 in the ibuprofen + diclofenac gel group.
Conclusion: This study does not support the use of topical diclofenac among patients who can otherwise tolerate oral ibuprofen.
Because the study did not compare placebo gel to topical Diclofenac, we cannot infer whether topical medication is helpful for treatment in acute lower back pain in those patients who may not be able to take NSAIDs.
Khankhel N, et al. Topical Diclofenac Versus Oral Ibuprofen Versus Diclofenac + Ibuprofen for Emergency Department Patients With Acute Low Back Pain: A Randomized Study. Ann Emerg Med. 2024 Jun;83(6):542-551.
Category: Cardiology
Posted: 5/24/2024 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
Category: Ultrasound
Keywords: Abdomen, ultrasound, trauma, contrast (PubMed Search)
Posted: 5/23/2024 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This very small study looked at the utility of using IV contrast media to enhance abdominal sonography in identifying injuries in blunt abdominal trauma patients. The comparison was CT scanning of the abdomen to identify injuries. The study concluded:
“With the addition of contrast and careful inspection of solid organs, abdominal sonography with contrast performed by the emergency physician improves the ability to rule out traumatic findings on abdominal CT. CEUS performed by emergency physicians may miss injuries, especially in the absence of free fluid, in cases of low-grade injuries, simultaneous injuries, or poor-quality examinations.”
To me, this is a limited study and the technique is not ready for wide spread use but further study is warranted.
Viviane Donner MD, Julian Thaler MD, Wolf E Hautz Prof. Dr.Med, MME, Thomas Christian Sauter Prof. Dr.Med, MME, Daniel Ott MD, Karsten Klingberg MD, Aristomenis K Exadaktylos Prof.Dr.Med, Beat Lehmann MD
First published: 19 April 2024
Journal of the American College of Emergency Physicians OpenVolume 5, Issue 2
Category: Administration
Keywords: Specialty ED, Geriatric ED, Oncologic ED (PubMed Search)
Posted: 5/21/2024 by Mercedes Torres, MD
(Updated: 5/22/2024)
Click here to contact Mercedes Torres, MD
There is a growing trend toward the development of specialty-specific emergency services, such as Geriatric or Oncologic EDs.
Will this trend continue? Is the segmentation of emergency care in our future? The author of this article opines that the answer depends on future outcomes research in this area.
Brouillette M. Are Specialty Emergency Departments the Future of Emergency Care? Oncology- and Geriatric-Focused Emergency Departments Hope to Improve Care, Lower Costs. Annals of Emergency Medicine. May 2024, 83(5):9A-12A. https://doi.org/10.1016/j.annemergmed.2024.03.015
Category: Critical Care
Posted: 5/21/2024 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Historically, guideline recommendations have been to use a transfusion threshold of hemoglobin < 7 g/dL for patients unless they are a) undergoing orthopedic surgery or b) have cardiovascular disease (CVD).
Applefeld et al conducted a meta-analysis in 2018 which suggested that restrictive (i.e. lower hemoglobin trigger, typically 7-8) transfusion targets lead to worse outcomes in CVD patients than liberal (i.e. higher hemoglobin trigger, typically 9-10) targets, and those authors have updated this analysis to include data from newer trials. Interestingly, the conclusion remains similar: that when you look at the larger studies on restrictive vs liberal transfusion targets, CVD plays an important role, as patients with CVD tend to do better with liberal targets, and patients without CVD tend to do better with restrictive targets. Of note, CVD is variably defined in these studies, and sometimes limited only to active Acute Coronary Syndromes, and other times refers to all patients with acute or chronic CVD. However, according to their analysis, the aggregated data suggests that we should continue having higher transfusion targets in patients with CVD, and perhaps even more in the 9-10 range, as opposed to the goals of 7 or 8 which are common.
Bottom Line: We will likely continue to see different transfusion targets recommended for patients with cardiovascular disease (CVD), and may even see guideline and blood bank recommendations raise the target for these patients more into the 9-10 range, or expand this group to include chronic CVD. This would mean a substantial increase in recommended RBC transfusions, and as emergency physicians it is important for us to monitor these recommendations, especially since transfusions are not harmless and raising hemoglobin thresholds could lead to complications that are difficult to measure in the literature.
Category: Misc
Keywords: Research Question (PubMed Search)
Posted: 5/20/2024 by Mike Witting, MS, MD
Click here to contact Mike Witting, MS, MD
Starting a study? Frame your research question in the PICO format:
Patients (consider severity of presentation, setting, demographics)
Intervention (either something you propose or something in use)
Comparison (another group, the same group without intervention, or a benchmark)
Outcome (a measurement)
This classic format has been used to evaluate studies, as in Journal Club (by our esteemed Dr. Wilkerson), as a literature search tool, or by the Cochrane review.
Starting with a PICO research question can help you narrow your focus and maintain it.
Category: Trauma
Keywords: vasopressor, hemorrhage, shock, trauma (PubMed Search)
Posted: 5/19/2024 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
In this podcast, the concept of vasopressor use in hemorrhagic shock is discussed. Key take away points:
Category: Pediatrics
Keywords: psych, pediatric mental health, suicide (PubMed Search)
Posted: 5/17/2024 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
This was a cross sectional study examining insurance data to determine if there is seasonality related to ED visits and psychiatric hospitalizations related to suicidality.
Suicidality includes both suicidal ideation and suicide attempts (but not suicide). One survey showed that up to 12% of US adolescents reported serious thoughts of suicide. This study included 73,123 patients where 19.4% were direct inpatient admissions and 80.6% were ED visits, 44% of whom were subsequently admitted.
Metrics for suicidality in 10-18 year olds peaked in April and October with a nadir in June. Incidentally, in the Spring of 2020 when US schools closed due to COVID, there was a decrease in both ED visits and hospitalizations with April and May having the lowest rates across the study period.
School is believed to increase stress with risk factors such as bullying and peer pressure, academic and extracurricular stressors and poor sleep hygiene.
Bottom line: There has been an increase in adolescent suicidality over the recent years, many of whom present to the ED for evaluation. More mental health resources are needed, especially during the school year.
Bottom line: There has been an increase in adolescent suicidality over the recent years, many of whom present to the ED for evaluation. More mental health resources are needed, especially during the school year.
Category: EMS
Keywords: delivery, neonatal, OB, contractions (PubMed Search)
Posted: 5/15/2024 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
Maternal morbidity continues to increase in the US with a mortality rate in 2021 of 39.2 deaths/100,000 live births. There has been an intense focus on training and quality improvement within hospitals, but not much has changed in the prehospital education arena. This study aimed to quantify the complications encountered by EMS clinicians.
In the 2018-2019 EMS dataset used, there were a total of 56,735,977 EMS activations which included 8641 out of hospital deliveries, 1712 documented delivery complications and 5749 records of newborns.
1% of the out of hospital deliveries had a documented complication for the mother. Of these complications, 94% were for hemorrhage, 6% for abnormal presentation, 0.2% for shoulder dystocia, and 0.4% for nuchal cord.
Few patients had medications given, including 0.4% receiving oxytocin. no patients received prehospital blood transfusion or TXA. Of note, in the years since this data was obtained, TXA and whole blood have started to appear on more medic units, but it is still not necessarily commonplace.
Bottom line: While still rare, prehospital delivery does occur and EMS should be prepared for any possible complications. Medical directors should look at their jurisdictional/state protocols to see if oxytocin/TXA or whole blood should be included (if not already available). EMS clinicians should be educated on up to date management of OB emergencies.
Rebecca E. Cash, Anjali J. Kaimal, Margaret E. Samuels-Kalow, Krislyn M. Boggs, Maeve F. Swanton & Carlos A. Camargo Jr (2023) Epidemiology of Emergency Medical Services-Attended out-of-Hospital Deliveries and Complications in the United States, Prehospital Emergency Care, DOI: 10.1080/10903127.2023.2283892
Category: Administration
Posted: 5/13/2024 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This retrospective study looked at patients diagnosed with urinary tract infections receiving an IV dose of antibiotics prior to discharge and compared ED length of stay and return visit rate. They found:
“Parenteral antibiotic administration in the ED was associated with a 60-minute increase in ED LOS compared with those who received an oral antibiotic (P < 0.001) and a 30-minute increase in ED LOS compared with no antibiotic (P < 0.001). No differences were observed in revisits to the ED at 72 hours”
Appears no benefit to the practice of IV antibiotics prior to discharge in UTI patients.
Mohammed A. Alrashed Stephen J. Perona Mark C. Borgstrom Elias Ramirez-Moreno
JAPhA VOLUME 64, ISSUE 3, 102020, MAY 2024
Published:January 29, 2024DOI:https://doi.org/10.1016/j.japh.2024.01.016
Category: Trauma
Posted: 5/12/2024 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
Hemodynamic instability in trauma patients is most often associated with hemorrhagic shock, however, there is an entity known as brain injury associated shock (BIAS). BIAS is thought to be associated with catecholamine surges secondary to brain injury. BIAS is found in both isolated head injury pts as well as multi-trauma patients. Studies have identified BIAS in 13% of adult trauma patients and up to 40% of pediatric major trauma patients.
We know hypotension in brain injury worsens outcome. We should assume hemorrhagic etiology until we prove otherwise. Once we suspect BIAS and have excluded hemorrhagic etiology our strategy should switch to blood pressure support using non-blood product management.
Partyka C, Alexiou A, Williams J, Bliss J, Miller M, Ferguson I. Brain Injury Associated Shock: An Under-Recognized and Challenging Prehospital Phenomenon. Prehospital and Disaster Medicine. Published online 2024:1-6. doi:10.1017/S1049023X24000359
Category: Orthopedics
Posted: 5/11/2024 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Concussion Visits to the Emergency Department
In a study looking at concussion discharge instructions in the ED:
A 2020 study looked at patients aged 6-18 years diagnosed with concussion on either first or subsequent ED visit.
Those patients with delayed diagnosis required more medical visits during recovery, had a significantly longer time to symptom resolution (21 vs. 11 days), and had a higher likelihood of having persistent concussion symptoms.
Take home: Consider printed concussion discharge instructions in the appropriate ED patients as this has downstream benefits for health and recovery.
Lane et al., 2017. Retrospective Chart Analysis of Concussion Discharge Instructions in the Emergency Department.
Upchurch et al., 2015. Discharge instructions for youth sports-related concussions in the emergency department, 2004 to 2012.
Corwin DJ et al. Characteristics and Outcomes for Delayed Diagnosis of Concussion in Pediatric Patients Presenting to the Emergency Department. 2020.
Category: Pediatrics
Posted: 4/5/2024 by Kathleen Stephanos, MD
(Updated: 5/10/2024)
Click here to contact Kathleen Stephanos, MD
Intranasal medications are an increasingly popular option for pediatric patients, particularly for analgesia and anxiolysis, with an increasing number of medications being used via the intranasal route of administration.
Fentanyl has been shown in prior studies to be a safe and effective pain management strategy for children, but is likely under utilized. In sickle cell patients, studies have shown that time to analgesia may improve outcomes including hospitalization.
In 2023, Rees et al. showed that in the sickle cell patient population IN fentanyl can be a very effective tool for patient's experiencing a Vaso-occlusive episode (VOE). This study looked at 400 children with a mean age of 14.6 years. Of these 19% received IN fentanyl.
Ultimately, the IN fentanyl patient population had a shorter time to initial administration of analgesia and a lower chance of admission to the hospital.
Notably, this was not a randomized study, so there is limitations in assessment of the causality of the lower discharge rates. However this is a tool that could likely be used more regularly in the pediatric sickle cell patient population to allow for more rapid pain management in the emergency department.
1. Payne J, Aban I, Hilliard LM, Madison J, Bemrich-Stolz C, Howard TH, Brandow A, Waite E, Lebensburger JD. Impact of early analgesia on hospitalization outcomes for sickle cell pain crisis. Pediatr Blood Cancer. 2018 Dec;65(12):e27420. doi: 10.1002/pbc.27420. Epub 2018 Aug 27. PMID: 30151977; PMCID: PMC6192851.
2. Rees CA, Brousseau DC, Ahmad FA, Bennett J, Bhatt S, Bogie A, Brown KM, Casper TC, Chapman LL, Chumpitazi CE, Cohen DM, Dampier C, Ellison AM, Grasemann H, Hatabah D, Hickey RW, Hsu LL, Bakshi N, Leibovich S, Patil P, Powell EC, Richards R, Sarnaik S, Weiner DL, Morris CR; SCD Arginine Study Group and PECARN. Intranasal fentanyl and discharge from the emergency department among children with sickle cell disease and vaso-occlusive pain: A multicenter pediatric emergency medicine perspective. Am J Hematol. 2023 Apr;98(4):620-627. doi: 10.1002/ajh.26837. Epub 2023 Feb 6. PMID: 36606705; PMCID: PMC10023395.
Category: Pharmacology & Therapeutics
Keywords: myasthenia gravis, myasthenic crisis, exacerbation, drugs to avoid (PubMed Search)
Posted: 5/9/2024 by Alicia Pycraft
Click here to contact Alicia Pycraft
Myasthenia gravis (MG) is an autoimmune neuromuscular disorder that affects an estimated 14 to 20 patients per 100,000 in the United States. Most patients with MG have autoantibodies against acetylcholine receptors (AChRs), which disrupt neuromuscular transmission through downregulation, destruction, blocking of AChRs or disrupting receptors in the postsynaptic membrane.
Several medications may worsen MG or precipitate myasthenic crisis, however, incidence is difficult to describe as literature is largely limited to case reports and there is often presence of other confounding factors. There are two proposed mechanisms for medications to cause or exacerbate MG:
Several medications commonly used in the emergency department are known to impair neuromuscular transmission and may induce or worsen MG. The following medications should be avoided, or used with extreme caution in patients with MG*:

*This list contains several common medications utilized in the emergency department, but is not an all-inclusive list of medications that may exacerbate MG. Please refer to the reference section for additional information.
Category: Gastrointestional
Keywords: CT, contrast (PubMed Search)
Posted: 5/8/2024 by Neeraja Murali, DO, MPH
(Updated: 2/7/2026)
Click here to contact Neeraja Murali, DO, MPH
Oftentimes, CT imaging is used in diagnosis of emergent abdominal pathology. However, there may be instances where there is hesitancy to use IV contrast, whether due to patient factors or extrinsic factors (remember the contrast shortage during covid?)
This study examines the diagnostic accuracy of dry CT. 3 quaternary centers with residency training programs participated, and contrasted images underwent further processing to remove any IV or oral contrast. Both residents and faculty reviewed the images, and findings were compared to both the initial read by radiologist as well as independent reads by a panel of experts. They looked for both primary findings (those that explained the abdominal pain) as well as actionable secondary findings (ie incidental findings requiring additional imaging or further management).
When compared to contasted imaging, the accuracy of dry CT was 70% (faculty, 68% to 74%; residents, 69% to 70%). Faculty had higher accuracy than residents for primary diagnoses but lower accuracy for actionable secondary diagnoses.
Thus when considering the necessity of contrast, please consider the potential for missed diagnosis.
Shaish H, Ream J, Huang C, et al. Diagnostic Accuracy of Unenhanced Computed Tomography for Evaluation of Acute Abdominal Pain in the Emergency Department. JAMA Surg. 2023;158(7):e231112. doi:10.1001/jamasurg.2023.1112
Category: Trauma
Keywords: trauma, blunt, cardiac injury, shock, thoracic (PubMed Search)
Posted: 5/5/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
Blunt Cardiac Injury is a continuum from asymptomatic, not clinically relevant to catastrophic, life ending disease . Consider blunt cardiac injury in patients with significant force to the chest wall or sudden deceleration injuries (motor vehicle crashes, motorcycle crashes, falls from height etc.). This algorithm is helpful when working up patients suspected of having significant blunt cardiac injury.
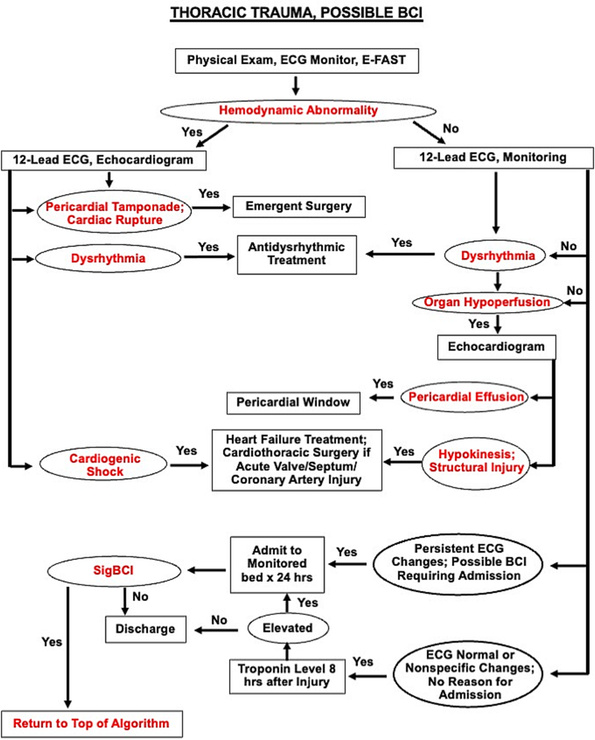
Biffl, Walter L. MD; Fawley, Jason A. MD; Mohan, Rajeev C. MD. Diagnosis and management of blunt cardiac injury: What you need to know. Journal of Trauma and Acute Care Surgery 96(5):p 685-693, May 2024. | DOI: 10.1097/TA.0000000000004216
Category: Administration
Keywords: trauma, EMS, hemorrhagic shock (PubMed Search)
Posted: 5/3/2024 by Ben Lawner, MS, DO
Click here to contact Ben Lawner, MS, DO
BACKGROUND:
Prehospital administration of whole blood involves some areas of controversy. Though theoretical benefits are clear, concerns about logistics and timing of blood often dominates the discussion. This study was a retrospective analysis of prehospital blood administration within an urban EMS system from 2021-2023. Primary endpoints included: time to administration and in hospital mortality.
PATIENTS/METHODS:
The study population included patients presenting to the EMS system with signs and symptoms of hemorrhagic shock (SBP<70 or SBP<90 + HR> 100, n=61) and who received at least 1 unit of prehospital blood (PHB). The EMS system administered blood in conjunction with an advanced resuscitative bundle (calcium, TXA, blood). Isolated head injuries and blunt trauma patients were excluded from the analysis. The control group (n=82) was comprised of patients in the system's trauma registry presenting to EMS PRIOR to the initiation of whole blood and who exhibited similar clinical crtieria.
RESULTS:
BOTTOM LINE:
In this prospective study conducted within an urban EMS system, patients receiving prehospital whole blood demonstrated improved vital signs and reduced mortality when compared to a control group. Slightly extended prehospital time intervals for patients receiving PHB may be offset by the measured benefits of whole blood therapy.
Duchesne, J. , McLafferty, B. , Broome, J. , Caputo, S. , Ritondale, J. , Tatum, D. , Taghavi, S. , Jackson-Weaver, O. , Tran, S. , McGrew, P. , Harrell, K. , Smith, A. , Nichols, E. , Dransfield, T. , Marino, M. & Piehl, M. (9900). Every minute matters: Improving outcomes for penetrating trauma through prehospital advanced resuscitative care. Journal of Trauma and Acute Care Surgery, Publish Ahead of Print , doi: 10.1097/TA.0000000000004363.
Category: Obstetrics & Gynecology
Keywords: postpartum depression (PubMed Search)
Posted: 5/2/2024 by Michele Callahan, MD
(Updated: 2/7/2026)
Click here to contact Michele Callahan, MD
Perinatal mental health problems are unfortunately quite common: according to the World Health Organization, approximately 10% of women in high-income countries and approximately 30% in low- or middle-income countries are affected.
It's important to be able to distinguish “baby blues” from more significant mental health issues. Typical symptoms of the “baby blues” include mild and short-lived changes in mood, as well as feelings of exhaustion, worry, and unhappiness in the weeks that follow giving birth.
Symptoms that are more severe or lasting >2 weeks post-partum should prompt further investigation and discussion with a mental health professional. Symptoms of perinatal depression may include: feeling persistently sad, feelings of hopelessness, loss of interest or pleasure in hobbies/activities, trouble bonding with the infant, appetite changes, and can even become as severe as wanting to harm onself or one's child. There are specific DSM-5 Criteria used to diagnose postpartum depression.
Universal screening for all pregnant and postpartum patients is highly recommended, and can be life-saving.
Bauman BL, Ko JY, Cox S, et al. Vital Signs: Postpartum Depressive Symptoms and Provider Discussions About Perinatal Depression — United States, 2018. MMWR Morb Mortal Wkly Rep 2020;69:575–581. DOI: http://dx.doi.org/10.15585/mmwr.mm6919a2
