Category: Vascular
Keywords: aortic aneurysm; point-of-care ultrasound; pocus; aortic dissection (PubMed Search)
Posted: 12/4/2023 by Alexis Salerno Rubeling, MD
(Updated: 2/7/2026)
Click here to contact Alexis Salerno Rubeling, MD
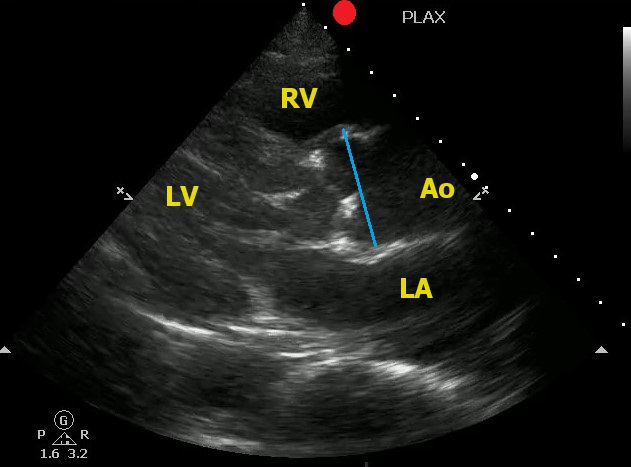
Point-of-Care Ultrasound can help to identify signs of thoracic aortic dissection.
One view to help in your assessment is the Parasternal Long Axis View.
To correctly measure the aortic root:
Here is an example of an aortic root aneurysm:
Kennedy Hall M, Coffey EC, Herbst M, Liu R, Pare JR, Andrew Taylor R, Thomas S, Moore CL. The "5Es" of emergency physician-performed focused cardiac ultrasound: a protocol for rapid identification of effusion, ejection, equality, exit, and entrance. Acad Emerg Med. 2015 May;22(5):583-93. doi: 10.1111/acem.12652.
Category: Vascular
Keywords: POCUS, AAA, (PubMed Search)
Posted: 6/19/2023 by Alexis Salerno Rubeling, MD
(Updated: 2/7/2026)
Click here to contact Alexis Salerno Rubeling, MD
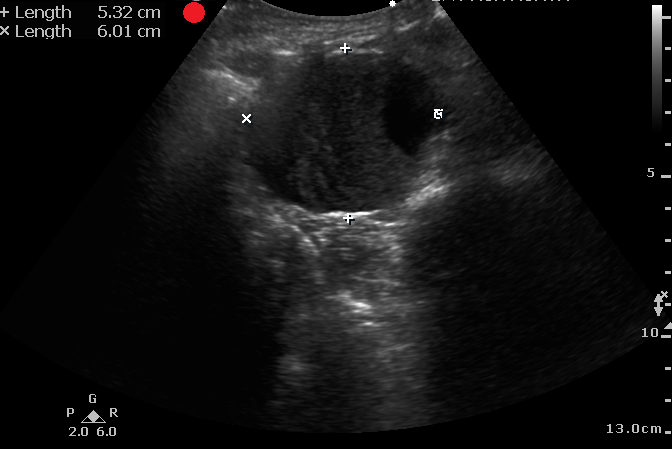
It is difficult to diagnosis a ruptured AAA with POCUS. However, based on one systematic review and meta-analysis, POCUS has a sensitivity of 97.8% and a specificity of 97% for diagnosing AAA in patients supsected of having a ruptured AAA.
Remeber:
Laslty, make sure you are measuring the aortic wall and not a mural thrombus.
Fernando SM, Tran A, Cheng W, Rochwerg B, Strauss SA, Mutter E, McIsaac DI, Kyeremanteng K, Kubelik D, Jetty P, Nagpal SK, Thiruganasambandamoorthy V, Roberts DJ, Perry JJ. Accuracy of presenting symptoms, physical examination, and imaging for diagnosis of ruptured abdominal aortic aneurysm: Systematic review and meta-analysis. Acad Emerg Med. 2022 Apr;29(4):486-496. doi: 10.1111/acem.14475.
Category: Vascular
Keywords: Aortic Dissection (PubMed Search)
Posted: 6/20/2011 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
There are several complications of acute aortic dissection that emergency physicians must be familiar with.
These include:
*Key Pearl: If a patient with suspected or confirmed acute aortic dissection suddenly arrests consider cardiac tamponade.
Category: Vascular
Posted: 1/3/2011 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
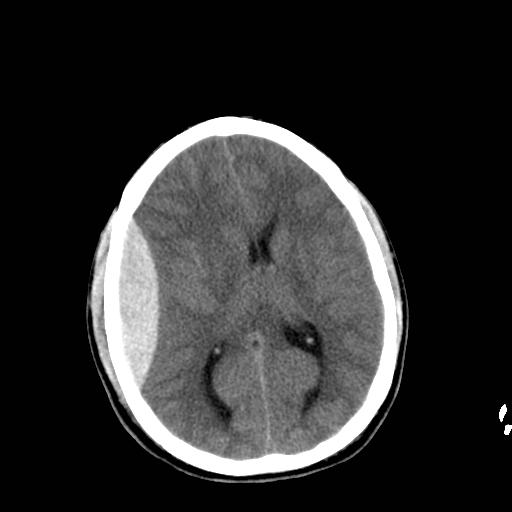
60 year-old male s/p assault. + LOC. Awake and normal neuro examination on arrival. Deteriorates in the ED after about an hour....
Diagnosis: Epidural Hematoma
Category: Vascular
Keywords: subarachnoid hemorrhage (PubMed Search)
Posted: 12/13/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Diagnosing Subarachnoid Hemorrhage-6 Pitfalls
1. Subarachnoid hemorrhage (SAH) doesn't always present as the "worst ever" headache. Don't most of our patients say their headache is the worst headache anyway? Be suspicious of the diagnosis if your patient has acute onset of an unusual or atypical headache. Diagnoses starts with the history.
2. The neuro exam may be completely normal in some cases, especially early on.
3. The headache due to SAH may get better with analgesics. This is a huge pitfall. Don't rule this diagnosis out if analgesics help.
4. The CT scan may be negative. Enough said.
5. Be careful with interpretation of the CSF. We all want the number of red cells in tube 4 to be zero. Be careful with this. Although the rbcs may have dropped by 50% from tubes 1 to 4, the diagnosis hasn't been excluded unless the cells clear completely. Although there have been some case reports of SAH with rbcs < 100, this is pretty uncommon.
6. CT Angiography and/or MRI with FLAIR is not a substitute for the lumbar puncture.
Stuart Swadron, Emergency Physicians Monthly
Category: Vascular
Keywords: hypertension (PubMed Search)
Posted: 12/6/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Got Symptomatic Hypertension? Why not try Fenoldopam?
Fenoldopam is a rapid-acting vasodilator.
Dosing (Adult): After a starting dose of 0.1 to 0.3 mcg/kg/minute, the dose is titrated at 15 minute intervals, depending on the BP response. May be increased in increments of 0.05 to 0.1 mcg/kg/minute every 15 minutes until target blood pressure is reached. Maximal infusion rate reported in clinical studies: 1.6 mcg/kg/minute.
Onset/duration: 5-10 minutes/~ 1 hour.
The Clinician's Ultimate Reference
Category: Vascular
Keywords: Pulmonary Embolism, IVC Filter (PubMed Search)
Posted: 9/20/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Pulmonary Embolism and IVC Filters
Inferior vena cava filters are placed in patients with massive DVT and /or in patients who cannot receive systemic anticoagulation.
The question is, can patients develop pulmonary embolism if a filter is already in place? The answer: yes
How does this happen?:
Category: Vascular
Keywords: Hypertension (PubMed Search)
Posted: 8/30/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Hypertensive Encephalopathy (HE) is a clinical diagnosis and can look like many other disease entities.
HE refers to a relatively rapidly evolving syndrome of severe hypertension in association with severe headache, nausea, and vomiting, visual disturbances, convulsions, altered mental status and, in advanced cases, stupor and coma.
The key is the presence of severe hypertension. Remember, though, that 160/105 mm Hg may be high for an individual patient. Most patients with the syndrome will have diastolic pressures well in excess of 120-130 mm Hg. The only way you will know if the diagnosis is correct is to treat the BP (carefully control), work up other etiologies, and see of symptoms improve with BP control.
Beware the patient with severe HTN and seizure. Seizure may be the first, and only, symptom of hypertensive encephalopathy.
Category: Vascular
Keywords: Aortic Dissection (PubMed Search)
Posted: 8/23/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Beta Blockade in Treating Acute Aortic Dissection
Medical therapy for acute aortic dissection is aimed at decreasing shear stress within the aorta. Although there are many agents to choose from when treating hypertension in patients with acute aortic disease, all regimens should include a beta blocker (like esmolol) unless contraindicated. Initiation of a beta blocker before another antihypertensive agent is added is crucial as this will prevent reflex tachycardia associated with vasodilators and other afterload reducers. Reflex tachycardia may worsen the dissection.
Category: Vascular
Posted: 8/16/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Treatment of Cerebral Venous and Sinus Thrombosis
Thrombosis of the cerebral venous system, also known as cerebral venous and sinus thrombosis and dural sinus thrombosis, is an uncommon condition encountered in the emergency department. The diagnosis may be stumbled upon by various CT findings or by MRI and/or a high opening pressure on lumbar puncture.
The treatment of choice is full dose anticoagulation with heparin. Available studies looked at unfractionated heparin, but many experts now consider LMWH (like Lovenox) an acceptable alternative. Despite the risk of hemorrhagic transformation of a venous infarct, heparin therapy is considered the standard treatment for this condition.
Couthino JM, et al. How to treat cerebral venous and sinus thrombosis. J Thromb Haemost 2010;8:877-83
Category: Vascular
Keywords: Pulmonary Embolism (PubMed Search)
Posted: 8/2/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Pulmonary Embolism and Blood Pressure
Patients with massive PE will often develop worsening hypotension after a fluid bolus due to increased right ventricular distension and deviation of the interventricular septum towards the left side of the heart. This septal deviation decreases left heart cardiac output.
In addition, patients with massive PE will sometimes develop higher blood pressures after intubation as positive pressure ventilation reduces preload, decreases deviation of the septum, and increases left sided cardiac output.
Category: Vascular
Keywords: Pulmonary Embolism (PubMed Search)
Posted: 6/28/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Silent Pulmonary Embolism?
As many as 50% of patients with isolated DVT will be found to have silent pulmonary embolism (i.e. no chest pain or shortness of breath) on VQ scanning. Studies performed in the last year or so with CT scanning show that this percentage is much higher.
The clinical take-home point is NOT to get a pulmonary CTA on suspected DVT patients but to remember that many patients can and do have PE in the absence of cardiopulmonary symptoms. Pretty frightening....
Stein. Silent Pulmonary Embolism. Arch Intern Med.2000;
Category: Vascular
Keywords: Pulmonary Embolism (PubMed Search)
Posted: 6/7/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Thrombolytic Therapy for Pulmonary Embolism
Current, FDA-approved thrombolytic therapy for PE:
Category: Vascular
Keywords: Pulmonary Embolism (PubMed Search)
Posted: 5/24/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Massive Pulmonary Embolism and Response to Fluids and Mechanical Ventilation
Massive pulmonary embolism leads to acute pulmonary hypertension and right ventricular overload. This leads to release of troponin and a "bowing" of the interventricular septum on echocardiography. Deviation of the septum then leads to a decrease in left-sided cardiac output.
A few interesting clinical pearls:
Category: Vascular
Keywords: PERC, pulmonary embolism (PubMed Search)
Posted: 4/26/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
A review of the PERC rule...
The "PERC Rule" is used to assess a patient's risk for probability of PE in the emergency department. It involves evaluating the presence or absence of 8 clinical criteria to arrive at a pretest probability. And remember, this rule is supposed to be used for patients with really low pretest probability where you weren't concerned about PE to begin with. Some experts claim that "PERC negative" on the chart proves you considered PE in the differential diagnosis. But the test isn't designed to be used on EVERY patient as a means to rule out PE. Only use if you thought about the disease in a low risk patient and didn't plan on getting a d-dimer or further testing.
The criteria are (all must be YES):
age < 50 years
heart rate less than 100 beats per minute
room air oxygen saturations 95% or greater
no prior deep venous thrombosis [DVT] or PE
no recent trauma or surgery (4 weeks)
no hemoptysis
no exogenous estrogen
no clinical signs suggestive of DVT (Unilateral leg swelling on visual inspection
Jeff, "Dr. PE," Kline
Category: Vascular
Keywords: Hypertension (PubMed Search)
Posted: 4/19/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Secondary Hypertension...say what?
We obviously see tons of patients in the ED with hypertension, and we are very comfortable with both symptomatic and asymptomatic presentations. Most of these patients have essential or primary hypertension. Some patients, however, may have secondary hypertension (i.e. something is causing it). Although we will refer patients to a primary care physician for further management and workup it is worth discussing when to suspect other diagnoses as the cause of the hypertension. Is it out job necessarily to diagnose these conditions in the ED? No.
Causes of secondary hypertension to consider:
Consider the ABCDE mnemonic:
A-Accuracy (is it really htn?), Apnea, Aldosteronism
B-Bruits, Bad Kidneys
C-Catecholamines, Coarctation, Cushing's
D-Drugs, Diet
E-Endocrine
Aren't you glad you didn't do a Medicine residency???
Onusko E. Diagnosing secondary hypertension. Am Fam Physician. 2003 Jan 1;67(1):67-74.
Category: Vascular
Keywords: aortic dissection (PubMed Search)
Posted: 4/5/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Some not too uncommon complications of Type B (distal) aortic dissection:
Category: Vascular
Posted: 3/29/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Acute Mesenteric Ischemia
Although we all know the classic presentation of acute mesenteric ischemia (AMI), it can be tough to diagnose.
Some pearls about AMI:
Category: Vascular
Keywords: Aneurysm (PubMed Search)
Posted: 3/8/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Splenic Artery Aneurysm (SAA)
Ever scanned someone and the report says "incidental note of a splenic artery aneurysm"? Well, if it hasn't happened yet, it will sooner or later. This type of aneurysm isn't that rare and with the number of abdominal CTs we order we are bound to see this in clinical practice.
Some important points to remember about SAA:
Category: Vascular
Keywords: Aortic Dissection (PubMed Search)
Posted: 2/22/2010 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Suspect your patient has an aortic dissection? Don't wait to lower the blood pressure.
A few considerations for the patient with suspected aortic dissection:
