Category: Pharmacology & Therapeutics
Keywords: Necrotizing Fasciitis, Necrotizing Soft Tissue Infection, Skin and Soft Tissue Infection, clindamycin, linezolid, NSTI (PubMed Search)
Posted: 2/8/2024 by Matthew Poremba
Click here to contact Matthew Poremba
Empiric antimicrobial treatment for necrotizing soft tissue infections (NSTIs) should include coverage of a wide range of pathogens including Staphylococcus spp, Streptococcus spp, anaerobic bacteria and gram negative bacteria. Treatment should also include an agent that suppresses toxin production by group A Streptococcus (GAS), with the Infectious Diseases Society of America (IDSA) guidelines recommending clindamycin plus penicillin for treatment of GAS causing necrotizing fasciitis and toxic shock syndrome. A typical empiric NSTI regimen would be vancomycin plus clindamycin plus piperacillin-tazobactam.
Linezolid is an appealing alternative to clindamycin and vancomycin, as it has anti-toxin effects via inhibition of exotoxin expression, potent in vitro activity against Streptococcus spp, activity against methicillin-resistant Staphylococcus aureus (MRSA), and potential for less adverse effects than clindamycin plus vancomycin. Several recent studies have looked at using linezolid in lieu of clindamycin plus vancomycin when treating NSTIs.
Published Studies:
Dorazio and colleagues published a retrospective single center study compared 62 matched pairs of patients who received linezolid vs. clindamycin plus vancomycin as part of their NSTI treatment.
Heil and colleagues published a retrospective single center cohort study examined patients who received either linezolid (n = 29) or clindamycin (n = 26) for treatment invasive soft tissue infection or necrotizing fasciitis with GAS isolated from blood and/or tissue.
Lehman and colleagues published a retrospective single center study compared patients who received linezolid (n = 21) versus clindamycin plus vancomycin (n = 28) in addition to gram-negative and anaerobic coverage for empiric treatment of NSTIs.
Bottom Line:
When added to an agent with good gram negative and anaerobic coverage (i.e. piperacillin-tazobactam), linezolid may be a more viable option for coverage of MRSA and GAS toxin production during empiric NSTI treatment when compared to clindamycin plus vancomycin. This is largely due to a more favorable side effect profile.
Category: Critical Care
Posted: 2/6/2024 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
PEEP in the Ventilated COPD Patient?
Jubran A. Setting positive end-expiratory pressure in the severely obstructive patient. Curr Opin Crit Care. 2024; 30:89-96.
Category: Ultrasound
Keywords: POCUS; Renal Colic; Flank Pain; Hydronephrosis (PubMed Search)
Posted: 2/5/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
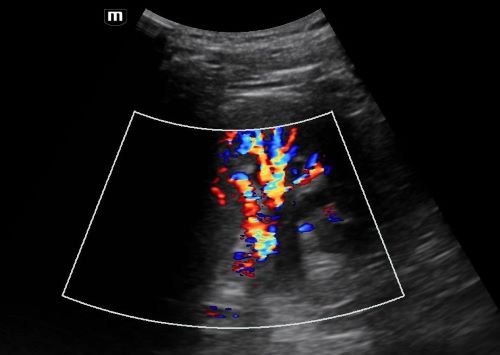
Ultrasound is the first line diagnostic tool to evaluate younger patients who present to the ED with flank pain.
Most of the time on ultrasound, you will not see the actual kidney stone. More often, you will see associated signs such as hydronephrosis.
In a patient with hydronephrosis, the normally hyperechoic renal pelvis will become anechoic. With increased severity of the hydronephrosis, you can have complete distortion of the kidney.

You can tell the difference between hydronephrosis and a renal vein by placing color doppler over the image. Hydronephrosis will not have flow.
Moore CL, Carpenter CR, Heilbrun ML, et al. Imaging in Suspected Renal Colic: Systematic Review of the Literature and Multispecialty Consensus. J Urol. 2019 Sep;202(3):475-483. doi: 10.1097/JU.0000000000000342.
Category: Trauma
Keywords: Ct, head injury, geriatric (PubMed Search)
Posted: 1/28/2024 by Robert Flint, MD
(Updated: 2/4/2024)
Click here to contact Robert Flint, MD
In this prospective study looking at geriatric patients with unknown head injury vs. known head injury, the unknown head injury group had an ICH 1.5%, neurosurgical intervention 0.3% and delayed ICH 0.1% when compared to known head injury (10.5%, 1.2% and 0.7% respectively). The authors concluded that the risk of ICH was high enough in uncertain head injury patients to warrant scanning.
Turchiaro ML Jr, Solano JJ, Clayton LM, Hughes PG, Shih RD, Alter SM. Computed Tomography Imaging of Geriatric Patients with Uncertain Head Trauma. J Emerg Med. 2023 Dec;65(6):e511-e516. doi: 10.1016/j.jemermed.2023.07.009. Epub 2023 Jul 26. PMID: 37838489.
Category: Quality Assurance/Quality Improvement
Keywords: Patient Mortality, Emergency Department Closure (PubMed Search)
Posted: 2/2/2024 by Brent King, MD
(Updated: 2/3/2024)
Click here to contact Brent King, MD
Takeaway Message: In this study from England, the closure or downgrading of selected emergency departments had no observable impact on patient mortality.
Due to staffing shortages in the UK, the NHS has closed or reduced the capacity of some emergency departments thus strategically concentrating emergency services. The authors of this observational study sought to determine the impact on patient mortality from the closure of five emergency departments between 2007 and 2014. While transport time to an emergency department did increase by up to 25 minutes (median change - 9 minutes, range 0-25 minutes), no change in mortality was identified in the population studied.
The Bottom Line: Closure of selected emergency departments had no impact on population mortality in this UK study but the affected patients had other EDs in relatively close proximity to the ones that had closed.
Comment: This article's findings contradict those of a previously posted Pearl which noted a decrease in mortality when newly opened EDs reduced the volume of existing EDs (Woodworth L. Swamped: Emergency department crowding and patient mortality. Journal of Health Economics, 2020; 70: 102279). The reasons for this discrepancy are unclear but may be due to differences in the healthcare systems of the US and UK.
Knowles E, Shephard N, Stone T_, et al_
The impact of closing emergency departments on mortality in emergencies: an observational study
Emergency Medicine Journal 2019;**36:**645-651.
Category: Critical Care
Keywords: sepsis, antibiotics, AKI, ACORN, zosyn, piperacillin-tazobactam, cefepime (PubMed Search)
Posted: 1/31/2024 by Kami Windsor, MD
(Updated: 2/8/2026)
Click here to contact Kami Windsor, MD
Background: For better or worse, the combination of “vanc-and-zosyn” has long been a go-to empiric regimen for the treatment of septic shock. Piperacillin-tazobactam is known to cause decreased creatinine secretion into the urine leading to an increased serum creatinine without any actual physiologic harm to the kidney, but the results of previous studies have led researchers to posit an increase in actual AKI with the vanc and zosyn combo. This concern has led to some physicians choosing cefepime for anti-pseudomonal gram-negative coverage instead, despite its known potential for neurotoxicity and cefepime-associated encephalopathy.
The ACORN trial: The recently published ACORN trial compared cefepime to piperacillin-tazobactam in adult patients presenting to the ED or medical ICU with sepsis or suspected serious infection. The primary outcome was a composite of highest stage of AKI or death at 14 days.
Results:
Bottom Line: Good antibiotic stewardship would probably decrease the frequency of vanc-and-zosyn administration, but concern for renal dysfunction alone shouldn’t guide the choice between cefepime or piperacillin-tazobactam, even in those with CKD, and even in those patients also receiving vancomycin.
Qian ET, Casey JD, Wright A, et al. Cefepime vs Piperacillin-Tazobactam in Adults Hospitalized With Acute Infection: The ACORN Randomized Clinical Trial. JAMA. 2023 Oct 24;330(16):1557-1567. doi: 10.1001/jama.2023.20583.
Category: Administration
Keywords: Medicare advantage, insurance, payor (PubMed Search)
Posted: 1/12/2024 by Steve Schenkel, MPP, MD
(Updated: 1/30/2024)
Click here to contact Steve Schenkel, MPP, MD
Approximately half of all Medicare beneficiaries are now enrolled in Medicare Advantage plans. Why does this matter?
Intrigued? Learn more at https://www.nejm.org/doi/full/10.1056/NEJMhpr2302315 or https://www.kff.org/medicare/issue-brief/medicare-advantage-2024-spotlight-first-look/.
Category: Ultrasound
Keywords: POCUS, musculoskeletal, ankle, arthrocentesis (PubMed Search)
Posted: 1/29/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
Many patients present to the emergency department for ankle swelling. On way to identify signs of intra-articular swelling is to use POCUS. To perform this, place the linear probe at the tibio-talar junction with the probe marker placed towards the patient’s head. An effusion is identified as anechoic fluid in-between the tibia and talus bone.
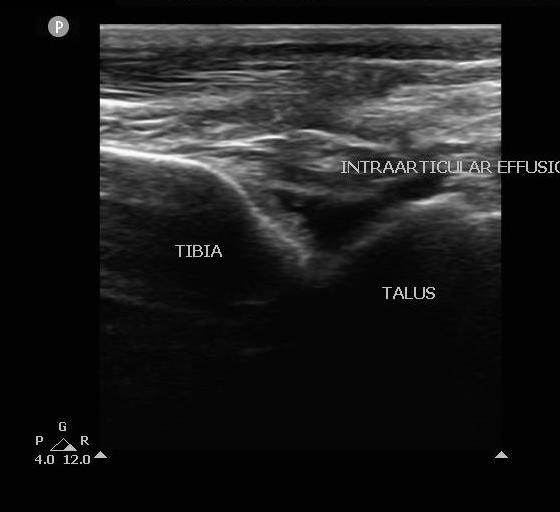
POCUS has been shown to improve first-pass success and overall success as compared to a landmark based approach for medium-sized joints. When performing an ankle arthrocentesis with POCUS, care should be taken to avoid blood vessels and tendons.
Gibbons RC, Zanaboni A, et al. Ultrasound-versus landmark-guided medium-sized joint arthrocentesis: A randomized clinical trial. Acad Emerg Med. 2022 Feb;29(2):159-163. doi: 10.1111/acem.14396.
Category: Trauma
Keywords: Prediction, surprise question, trauma, mortality (PubMed Search)
Posted: 1/28/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
The question “Would I be surprised if the patient died within the next year” has been validated as a tool to predict patients with a limited life expectancy. This study looked at trauma team members’ ability to use this question to predict one year mortality. Trauma team members over estimated mortality in this study.
Hoffman, Melissa Red MD, ND; Slivinski, Andrea DNP, APRN; Shen, Yan PhD; Watts, Dorraine D. PhD; Wyse, Ransom J. MPH; Garland, Jeneva M. PharmD; Fakhry, Samir M. MD, FACS; the Surprise Question in Trauma Research Group. Would you be surprised? Prospective multicenter study of the Surprise Question as a screening tool to predict mortality in trauma patients. Journal of Trauma and Acute Care Surgery 96(1):p 35-43, January 2024. | DOI: 10.1097/TA.0000000000004151
Category: Orthopedics
Posted: 1/27/2024 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Reducing musculoskeletal injury and concussion risk in schoolboy rugby players with a pre-activity movement control exercise programme: a cluster randomised controlled trial
Intro: Musculoskeletal injuries and concussion are prominent reasons for time loss from sport for adolescent rugby players.
Injury patterns in rugby differ from other team sports,
-Greater frequency of concussion, upper body and contact-related injuries
Increased concussion risk is associated with lower neck strength, highlighting this characteristic as a potentially modifiable risk factor.
Enhancing neck muscle strength may prevent concussion by improving the dissipation of impact forces transmitted to the brain.
The aim of study was to determine the efficacy of a movement control exercise program in reducing injuries in youth rugby players.
Methods: In a cluster-randomized controlled trial, 40 independent schools (118 teams, 3188 players aged 14-18 years) were allocated to receive either the intervention or a reference program, both of which were to be delivered by school coaches.
The intervention comprised balance training, whole-body resistance training, plyometric training, and controlled rehearsal of landing and cutting maneuvers. This also included a neck strengthening component.
Time-loss (>24 hours) injuries arising from school rugby matches were recorded by coaches and medical staff.
Results: When trial arm comparisons were limited to teams who had completed three or more weekly program sessions on average, clear reductions in overall match injury incidence (RR=0.28) and concussion incidence (RR=0.41) were noted in the intervention group.
Conclusion:
Hislop MD, et al. Reducing musculoskeletal injury and concussion risk in schoolboy rugby players with a pre-activity movement control exercise programme: a cluster randomised controlled trial. Br J Sports Med. 2017 Aug;51(15):1140-1146.
Category: Critical Care
Keywords: OHCA, elevated head and thorax, chest compression (PubMed Search)
Posted: 1/23/2024 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
Hot of the press from the Society of Critical Care Medicine (But most of us would know it already)
Settings: This is a prospective observational population-based study design with non-contemporaneous, nonrandomized clinical trial direct (unadjusted) head- to-head evaluations
Propensity score–matched comparisons of non-shockable cardiac arrest (NS-OHCA) patient survivor using conventional CPR (C-CPR) vs. C-CPR plus Automated Head/thorax up positioning-CPR (AHUP-CPR).
Participants: patients with non-traumatic, non-shockable out of hospital cardiac arrest (NS-OHCA).
Outcome measurement: primary outcome = survival, secondary outcome = survival with good neurologic outcome (Cerebral Performance Category score of 1–2 or modified Rankin Score less than or equal to 3).
Study Results:
• There was a total of 380 AHUP-CPR vs. 1852 C-CPR patients. After 1:1 matching, there were 353 AHUP-CPR patients and 353 C-CPR patients.
• In unadjusted analysis
o AHUP-CPR was associated with higher odds of survival (Odds ratio 2.46, 95% CI 1.55-3.92) and higher odds of survival with good neurologic function (Odds ratio 3.09 (95% CI 1.64-5.81)
• In matched groups
o AHUP-CPR was associated with higher odds of survival (Odds ratio 2.84, 95% CI 1.35-5.96) and higher odds of survival with good neurologic function [Odds ratio 3.87 (95% CI 11.27-11.78]
Discussion:
• There was no difference in rates of ROSC between groups. The authors argued that there was “neuroprotective effects” for the AHUP-CPR group.
• Although randomized controlled trials are usually required before clinical interventions are adopted, the aurthors argued that it would be difficult to randomize OHCA patients, and that the risk vs benefits may facilitate early adoption of this strategy.
• AHUP-CPR should be used first by well-trained clinicians to ensure its benefits.
Conclusion:
OHCA patients with NS presentations will have a much higher likelihood of surviving with good neurologic function when chest compressions are augmented by expedient application of the noninvasive tools to elevated head and thorax used in this study.
Bachista KM, Moore JC, Labarère J, Crowe RP, Emanuelson LD, Lick CJ, Debaty GP, Holley JE, Quinn RP, Scheppke KA, Pepe PE. Survival for Nonshockable Cardiac Arrests Treated With Noninvasive Circulatory Adjuncts and Head/Thorax Elevation. Crit Care Med. 2024 Feb 1;52(2):170-181. doi: 10.1097/CCM.0000000000006055. Epub 2024 Jan 19. PMID: 38240504.
Category: Hematology/Oncology
Keywords: CVC, Central Line Placement, Thrombocytopenia, Platelets, Transfusion (PubMed Search)
Posted: 1/22/2024 by Sarah Dubbs, MD
Click here to contact Sarah Dubbs, MD
The routine use of ultrasound guidance has decreased CVC-related complications, especially in patients at risk for bleeding. To this day, however, platelet transfusion threshold guidelines range widely from 20,000 - 50,000 platelets per cubic millimeter, and also lack good-quality evidence.
This multicenter, randomized, controlled, noninferiority trial randomly assigned patients with severe thrombocytopenia (platelet count 10,000 to 50,000 per cubic millimeter) to receive either one unit of prophylactic platelet transfusion or no platelet transfusion before ultrasound-guided CVC placement.
Author's Conclusions: Withholding prophylactic platelet transfusion before CVC placement in patients with a platelet count of 10,000 to 50,000 per cubic millimeter did NOT meet the predefined margin for noninferiority and resulted in more CVC-related bleeding events than prophylactic platelet transfusion.
BUT…taking a closer look at this study reveals many nuanced points. Many of the study patients were heme/onc patients possibly having bleeding issues outside of low platelets, bleeding complications trended with subclavian and femoral locations as well as lower initial platelet counts. All this suggests that additional studies need to be done to move towards more specific evidenced-based guidelines.
To read more details on the study, click the referenced link.
Category: Administration
Keywords: Risk, diagnostic error (PubMed Search)
Posted: 1/21/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
From the Canadian Medical Protective Association looking at 5 years of closed medical legal cases. This fits with previous risk management data and should give us pause when treating these conditions.
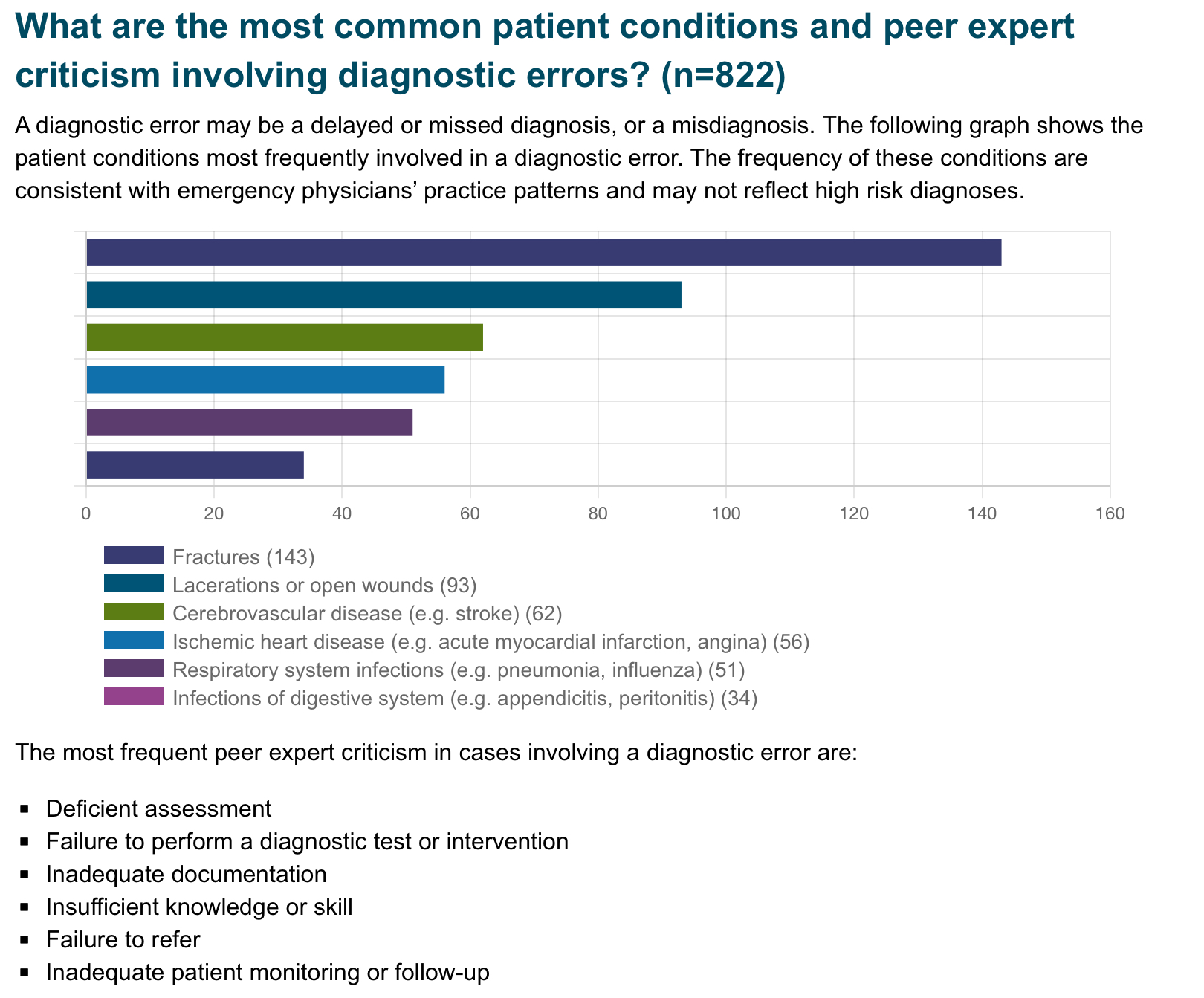
Published November 2023
Category: Administration
Keywords: restraint use (PubMed Search)
Posted: 1/21/2024 by Kevin Semelrath, MD
(Updated: 2/8/2026)
Click here to contact Kevin Semelrath, MD
This study was a retrospective review of restraint use at a level 1 trauma center in the Midwest.
It found the following were factors in a patient encounter associated with an increased risk of restraint usage:
This study found a decreased OR of restraint use with Black or Hispanic race, which was in contrast to other studies
This was a single center, retrospective study, so it was already limited in what it could tell us. In addition, they didn't see the reason for the restraints being ordered in the first place. Nonetheless, it does show that people in certain marginalized groups have a higher likelihood of ending up in restraints. Please think twice when ordering restraints in the ED, especially for behavioral reasons
Published:September 19, 2023DOI:https://doi.org/10.1016/j.annemergmed.2023.08.009
Category: Pediatrics
Keywords: Bouncebacks, high risk discharges, gastroenteritis, death (PubMed Search)
Posted: 1/19/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Revisits back to the ED within 3 days of the initial visit represent a standard quality measure. A critical ED revisit was defined as an ICU admission or death within 3 days of ED discharge. This study looked at 16.3 million children who were discharged from various EDs over a 4 year period and found that 0.1% (18,704 patients) had a critical revisit and 0.00001% (180 patients) died.
The most common diagnosis at the initial visit of those patients coming back with a critical revisit included: Upper respiratory infections, gastroenteritis/nausea/vomiting and asthma.
The most common critical revisit diagnosis were: asthma, pneumonia, cellulitis, bronchiolitis, upper respiratory infections, respiratory failure, seizure, gastroenteritis/nausea/vomiting, appendectomy and sickle cell crisis. Among the patients who died, 48.9% were younger than 4 years. Patients with complex medical problems and patients seen at a high volume center were more likely to have a critical ED visit.
Bottom line: These ED revisits may not have been related to missed diagnosis (with the exception of appendicitis), but rather due to the natural progression of certain disease processes. Patients with these diagnoses may benefit from careful reassessment, targeted patient education, more specific return precautions and closer outpatient follow up.
Cavallaro et al. Critical Revisits Among Children After Emergency Department Discharge. Annals of Emergency Medicine. 2023. epub ahead of print.
Category: Critical Care
Keywords: IVC, POCUS (PubMed Search)
Posted: 1/17/2024 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
IVC POCUS is often misapplied in attempts to assess volume status and/or volume “responsiveness.” Here are some important concepts to understand when using IVC POCUS to guide management:
Rola P, Haycock K, Spiegel R. What every intensivist should know about the IVC. Journal of Critical Care. Published online November 2023:154455.
Category: EMS
Keywords: ACS, PE, risk stratification (PubMed Search)
Posted: 1/17/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
The 2nd most common reason for EMS activation is chest pain. In this study, paramedics were asked to complete the HEAR (history, EKG, age, risk factor) score, EDACS (ED Assessment of chest pain score), the Revised Geneva Score and the PERC (Pulmonary embolism rule-out criteria) for all patients older than 21 who presented with chest pain. The positive and negative likelihood ratios (LR) of the risk scores in relation to 30 day MACE and PE risk were calculated.
837 patients were included in this study with 687 patients having all 4 scores completed. The combination of HEAR/PERC had the best negative LR (0.25) for ruling our MACE and PE at 30 days. However, these scores, alone or in combination, were not sufficient to exclusively guide treatment or destination decisions. Adding biomarkers (ie troponin or Ddimer to the prehospital setting) could improve the usefulness of these scores.
Stopyra JP, Snavely AC, Ashburn NP, et al. Performance of Prehospital Use of Chest Pain Risk Stratification Tools: The RESCUE Study. Prehosp Emerg Care. 2023;27(4):482-487. doi:10.1080/10903127.2022.2036883
Category: Ultrasound
Keywords: POCUS; Cardiac Tamponade; Cardiology; Critical Care (PubMed Search)
Posted: 1/15/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
What are the signs of Cardiac Tamponade on ultrasound?
Think of them as a pyramid with clinical importance decreasing as you rise to the top of the pyramid.
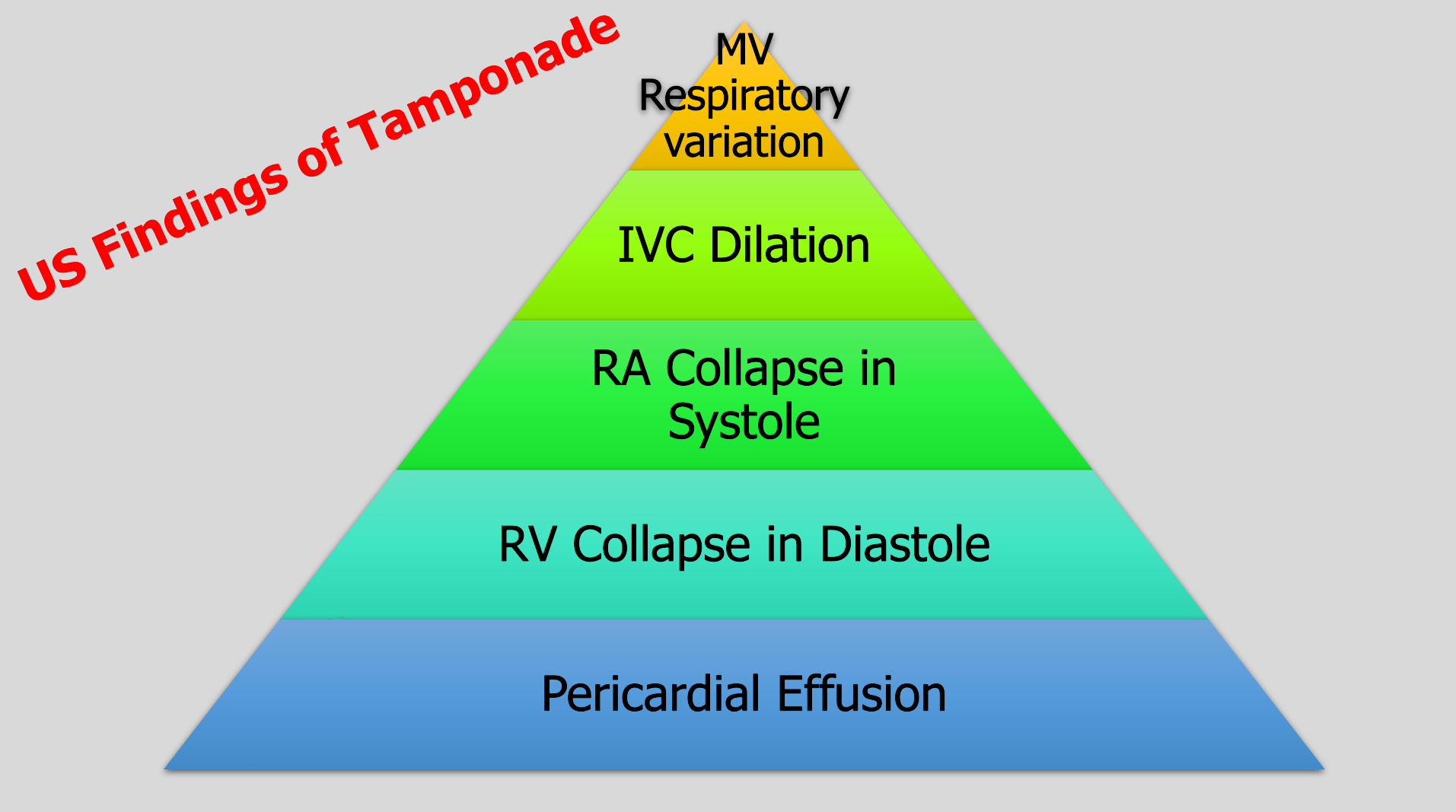
To have tamponade you need a pericardial effusion.
The most specific sign of tamponade is RV collapse in diastole.
The earliest and most sensitive sign is RA collapse over 1/3 of the cardiac cycle from late diastole into systole, which is why we say RA collapse during systole.
IVC dilation also occurs but is not sensitive.
Placing the pulse wave Doppler over the mitral valve and evaluating the change with respirations is an advanced technique. It’s positive if you have 25% change.
Don’t know if you are in systole or diastole? Connect your telemetry leads to the ultrasound machine. Don't have leads? Then you can also cine scroll on a subxiphoid view or parasternal view to look at when the valves are open and closed, then compare to the cardiac wall positioning.
Alerhand S, Adrian RJ, Long B, Avila J. Pericardial tamponade: A comprehensive emergency medicine and echocardiography review. Am J Emerg Med. 2022 Aug;58:159-174. doi: 10.1016/j.ajem.2022.05.001. Epub 2022 May 6. PMID: 35696801.
Category: Trauma
Keywords: elder, Trauma, delirium, confusion (PubMed Search)
Posted: 1/14/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Imagine lying in a bed staring at the ceiling and these fuzzy faces looking down on you clearly saying something to you but you can't hear them while your hip and pelvis are hurting worse than anything you have ever felt. That's what many of our fall from standing elderly patients experience in emergency departments on a regular basis. Do not remove glasses or hearing aides from your elderly patients. Work with our EMS colleagues to make it a practice to bring glasses and hearing aides along from the scene. Speak slowly and get close to their ear to help if necessary. That confusion, delirium or dementia you assume this patient has is actually just hearing impairment and poor vision.
Category: Orthopedics
Posted: 1/13/2024 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Wrist pain in golfers
70% of amateur golfers will experience a sport related injury in their lifetime.
The hand/wrist is the third most common body area injured by golfers after the back and elbow.
Studies fail to include multi trauma from golf cart accidents:)
Wrist injuries are 3x more frequent than hand injuries.
Wrist injury affects 13 to 20 percent of amateur golfers.
Injury is most likely to occur at the point of ball impact.
Injury most commonly affects the lead wrist rather than the trail wrist.
The lead wrist is left sided for right-handed players and right sided for lefties
Due to many differences in grip and wrist position there are several injury patterns.
Most causes of wrist pain in golfers are tendinopathies.
Due to impact stress and repetitive swinging movements
If pain is primarily radial, consider DeQuervain's tenosynovitis
Poor swing mechanics such as premature wrist uncocking in the early downswing places the wrist in ulnar deviation thereby stressing the first dorsal compartment.
Significant ulnar deviation of the lead wrist at time of ball impact may also stress the tendons of the first dorsal compartment.
If pain is primarily ulnar consider Extensor Carpi Ulnaris tendonitis & subluxation
A strong golf grip (more knuckle’s visible) is associated with greater ECU stress during the swing
The height of hand position can also stress the ECU tendon
Differential diagnosis:
TFCC injury
Hook of hamate fracture
Carpal Tunnel Syndrome
Ulnar Tunnel Syndrome
