Category: Administration
Keywords: age, attrition, gender, workforce (PubMed Search)
Posted: 7/26/2023 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
In a recent study of emergency physicians (EPs) who left the workforce between 2013 and 2020, authors sought to investigate their age and number of years since residency graduation for males and females.
A total of 25,839 (70.2%) male and 10,954 (29.8%) female EPs were included.
Female gender (adjusted odds ratio 2.30) was significantly associated with attrition from the workforce.
Of those who left the workforce, the median number of years after residency that males left was 17.5, as compared with only 10.5 years for females.
Furthermore, among those who exhibited attrition, one in 13 males and one in 10 females exited clinical practice within 5 years of residency graduation.
As authors emphasize, these data identify widespread gender-based disparities regarding EM workforce attrition that are critical to address to ensure stability, longevity, and diversity in the EP workforce.
Gettel CJ, Courtney DM, Agrawal P, et al. Emergency medicine physician workforce attrition
differences by age and gender. Acad Emerg Med. 2023;00:1- 9. doi:10.1111/acem.14764
Category: Critical Care
Keywords: OHCA, ROSC, cardiac arrest, resuscitation, CT, pan-scan, computed tomography (PubMed Search)
Posted: 7/25/2023 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
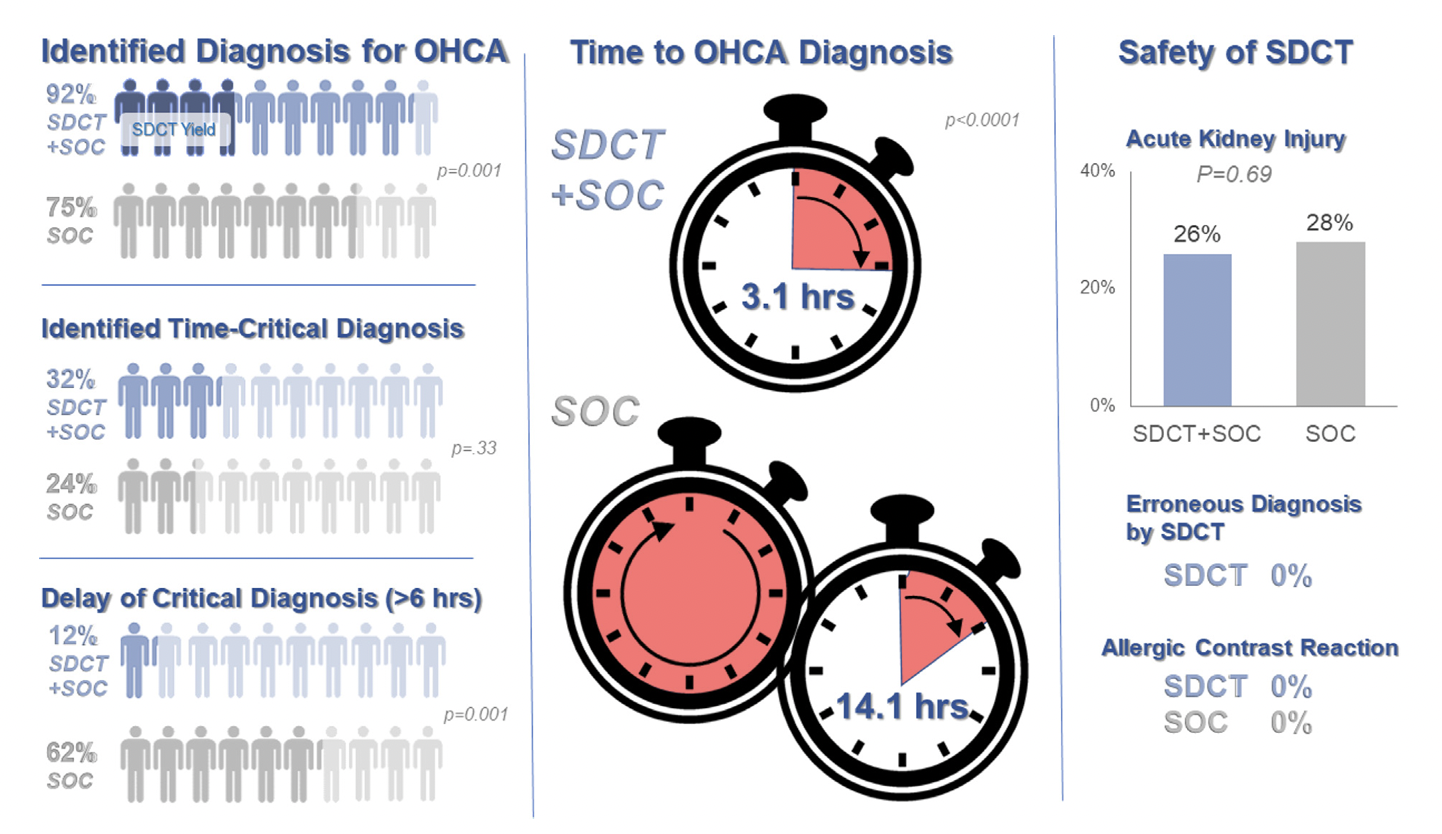
Background: Prior evidence1,2 has suggested that early “pan-scan” after ROSC provides clinically-relevant information that assists in the care of the patient in question, when the cause of OHCA is unclear.
The recent CT FIRST trial looked at patients pre- and post- implementation of a protocol for head-to-pelvis CT within 6 hours of ROSC for adult patients without known cause or evidence of possible cardiac etiology, stable enough for scan. *Patients with GFR <30 were excluded from assignment to CT, although were included in the post/CT cohort if their treating doctors ordered CT scans based on perceived clinical need. To balance this, a similar number of patients with GFR <30 were included in the pre/“standard of care” cohort.
Outcomes After Protocol (Pre- vs. Post-):
Bottom Line: Early pan-CT allows for earlier definitive diagnosis and stabilization without increase in adverse events. While this earlier diagnosis does not seem to yield better survival, earlier stabilization may provide some benefits in terms of resource allocation and disposition, a notable benefit during our current crisis of staffing shortages and ED boarding.
Category: Trauma
Keywords: radiology, transfer, trauma, imaging, rural (PubMed Search)
Posted: 7/23/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Evaluating trauma patients at Level 3 or 4 centers, rural hospitals, and non-trauma centers is difficult. Understanding the amount of work-up to perform prior to transfer is important. Summers, et al suggest less is more when it comes to imaging. The receiving facility often repeats imaging leading to time delays, additional radiation exposure, and increased costs. Chest X-ray and FAST exam may be all that is indicated in centers that do not have the resources to care for injures identified on CT imaging prior to transfer.
Summers LN, Harry ML, Colling KP. Evaluating our progress with trauma transfer imaging: repeat CT scans, incomplete imaging, and delayed definitive care. Emerg Radiol. 2021 Oct;28(5):939-948. doi: 10.1007/s10140-021-01938-x. Epub 2021 May 28. PMID: 34050410.
Category: Orthopedics
Keywords: shoulder pain, labrum tear (PubMed Search)
Posted: 7/22/2023 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
SLAP tear/lesion – Superior labral tear oriented anterior to posterior
Glenoid labrum – A rim of fibrocartilaginous tissue surrounding the glenoid rim, deepening the “socket” joint.
Integral to shoulder stability.
https://aosm.in/storage/2019/05/ch-shoulder-slap.jpg
O’Brien’s test aka active compression test for superior labral pathology.
2 parts – generally performed with the patient standing.
The patient’s shoulder is raised to 90 degrees with full elbow extension and approximately 30 degrees of adduction across the midline.
Resistance is applied, using an isometric hold.
Test in both full internal and external rotation
-This alters the position and rotation of the humerus against the glenoid
A positive test is when pain is elicited when the shoulder is in internal rotation with forearm pronation (thumb to floor) and much less or no pain when in external rotation (supination).
Note: AC joint pain may test similarly but will localize to different area of shoulder
The presence of similar, reproducible deep and diffuse glenohumeral joint pain is most indicative of a true positive test.
https://i0.wp.com/musculoskeletalkey.com/wp-content/uploads/2020/03/f50-02-9780323287845.jpg?w=960
Category: Administration
Keywords: racial disparity, substance use disorder (PubMed Search)
Posted: 7/22/2023 by Kevin Semelrath, MD
(Updated: 2/8/2026)
Click here to contact Kevin Semelrath, MD
Substance use disorder is now known to be a function of brain disease and not a moral failure. Patients with substance use disorder are highly complex and often use the ED at a higher frequency than those without the disorder. However, these patients are also frequently the target of implicit bias and stigmatizing behavior from the healthcare team that can lead to worsened outcomes. Add on top of that a racial disparity, and we can see how this group of patients can have really bad health outcomes.
This study looked at the length of time to treatment of patients with SUD, to see if there was a difference within this group based on racial or ethnic differences. It did find that black patients with SUD did wait on average 35% longer in the ED before being seen or treated. This difference was statistically significant.
While this study wasn't designed to identify the causes of such a disparity, it does raise concern for implicit bias being in effect among not only the healthcare workers, but ingrained into the healthcare systems themselves.
Patient's with SUD are a vulnerable group of patients, and black patients with SUD are experiencing a disparity in time to treatment. This should remind us all to seek out ways to remove these biases and disparities from the systems where we work.
Category: Pediatrics
Keywords: fever, limp, bacteremia, osteomyelitis, septic joint (PubMed Search)
Posted: 7/21/2023 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
El Helou R, Landschaft A, Harper MB, Kimia AA. Bacteremia in Children With Fever and Acute Lower Extremity Pain [published online ahead of print, 2023 Apr 4]. Pediatrics. 2023;e2022059504. doi:10.1542/peds.2022-059504
Category: Toxicology
Keywords: acetaminophen overdose, fomepizole, NAC (PubMed Search)
Posted: 7/19/2023 by Natasha Tobarran, DO
(Updated: 2/8/2026)
Click here to contact Natasha Tobarran, DO
Acetaminophen (APAP) is the leading cause of acute liver failure worldwide. Standard treatment for APAP overdose is with N-acetylcysteine (NAC), which is highly effective if given within 8 hours of ingestion. However, in delayed presenters or massive ingestions patients can still develop hepatotoxicity. Adjunctive therapies can be considered in these cases including augmented NAC dosing, renal replacement, and fomepizole.
A small amount of APAP is metabolized to N-acetyl-p-benzoquinone imine (NAPQI) by cytochrome 2E1. In therapeutic doses, the body is able to detoxify the NAPQI using glutathione. In overdose, glutathione stores get depleted and NAPQI can cause hepatotoxicity. Mitochondrial damage in APAP overdose is mediated by the c-Jun-N-terminal Kinase (JNK) pathway.
NAC works to replenish glutathione stores and detoxify NAPQI. In large overdoses, increased dosing of NAC may be necessary. Fomepizole is typically used for its alcohol dehydrogenase inhibitor property to treat methanol and ethylene glycol poisoning. Fomepizole is also a cytochrome 2E1 and JNK inhibitor and can be used in APAP overdose to block the formation of NAPQI and mitigate mitochondrial damage. Dialysis can be used to eliminate APAP from the body completely in massive overdoses or if significant acidosis or renal failure.
This study is a case series of 14 patients treated for APAP overdose between 2017 – 2021 at a tertiary hospital
Limitations of the study:
In summary:
Stephanie L. Link, Garrett Rampon, Stephen Osmon, Anthony J. Scalzo & Barry H. Rumack (2022) Fomepizole as an adjunct in acetylcysteine treated acetaminophen overdose patients: a case series, Clinical Toxicology, 60:4, 472-477, DOI: 10.1080/15563650.2021.1996591
Category: EMS
Keywords: handoff, communication, adverse outcomes (PubMed Search)
Posted: 7/19/2023 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Sumner BD, Grimsley EA, Cochrane NH, et al. Videographic Assessment of the Quality of EMS to ED Handoff Communication During Pediatric Resuscitations. Prehosp Emerg Care. 2019;23(1):15-21. doi:10.1080/10903127.2018.
Category: Critical Care
Keywords: Central Lines, Platelets, Bleeding (PubMed Search)
Posted: 7/18/2023 by Mark Sutherland, MD
(Updated: 2/8/2026)
Click here to contact Mark Sutherland, MD
Central Venous Catheter (CVC; aka central line) placement is a common procedure in both the ED and ICU, and while overall quite safe, does carry some risk. In particular, many of us regularly are confronted with the challenge of placing a line in a patient with profound thrombocytopenia, which can result in significant bleeding. In these cases, should we give platelets before we place the line?
Van Baarle et al published a randomized study in NEJM comparing an empiric 1u platelet transfusion vs no transfusion in patients with a platelet count of 10,000-50,000, prior to line placement. The study included both HD and non-HD (e.g. TLC) lines, from all three major access sites, in patients in their ICU or hematology ward. They found statistically fewer serious bleeding events in the transfusion group (4.8%) vs no transfusion group (11.9%). The study wasn't powered to look at more patient oriented outcomes like mortality, but I'm sure we can all agree less bleeding is probably a good thing. Also importantly, this study did not evaluate the risks/benefits of delaying line placement to obtain platelets when the line is urgently needed, so I would not recommend extending this to conclude platelets must be given before line placement if the line is needed for something highly time-sensitive (e.g. only available access to infuse pressors in a hypotensive patient).
Bottom Line: It is probably beneficial and appropriate to provide prophylactic platelet transfusion prior to CVC placement in patients with a platelet count less than 50,000, assuming circumstances allow.
van Baarle FLF, van de Weerdt EK, van der Velden WJFM, Ruiterkamp RA, Tuinman PR, Ypma PF, van den Bergh WM, Demandt AMP, Kerver ED, Jansen AJG, Westerweel PE, Arbous SM, Determann RM, van Mook WNKA, Koeman M, Mäkelburg ABU, van Lienden KP, Binnekade JM, Biemond BJ, Vlaar APJ. Platelet Transfusion before CVC Placement in Patients with Thrombocytopenia. N Engl J Med. 2023 May 25;388(21):1956-1965. doi: 10.1056/NEJMoa2214322. PMID: 37224197.
https://www.nejm.org/doi/10.1056/NEJMoa2214322
Category: Trauma
Keywords: access, IO, IV, resucitation (PubMed Search)
Posted: 7/9/2023 by Robert Flint, MD
Click here to contact Robert Flint, MD
This study found that time to intraosseous was faster than time to peripheral IV. This lead to quicker resuscitation time. This was particularly true in pateints that arrived without a pre-hospital IV.
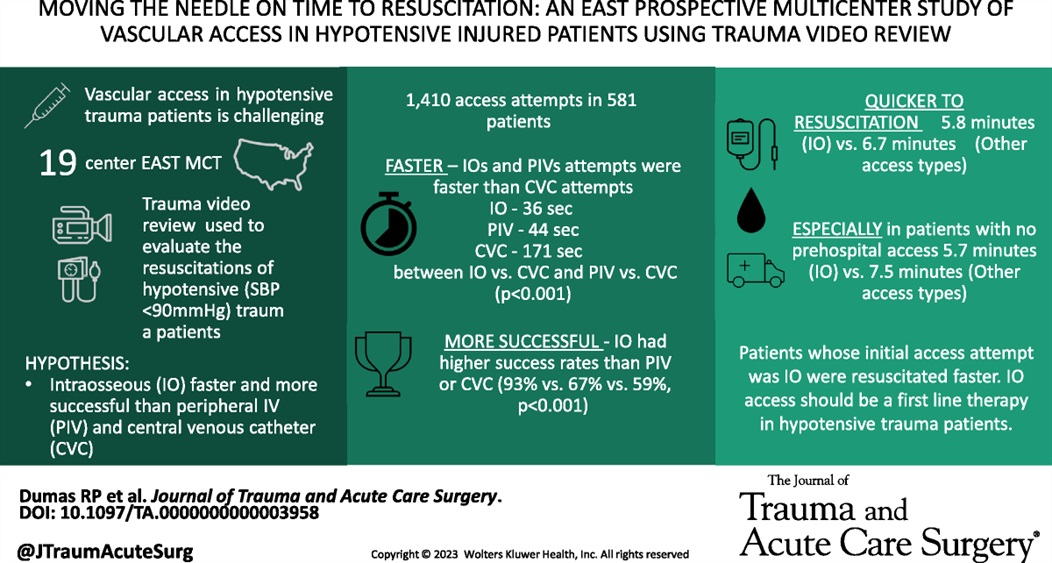
Dumas, Ryan P. MD; Vella, Michael A. MD; Maiga, Amelia W. MD; Erickson, Caroline R. MD; Dennis, Brad M. MD; da Luz, Luis T. MD, MSc; Pannell, Dylan MD; Quigley, Emily BSN; Velopulos, Catherine G. MD; Hendzlik, Peter; Marinica, Alexander DO; Bruce, Nolan MD; Margolick, Joseph MD; Butler, Dale F. MD; Estroff, Jordan MD; Zebley, James A. MD; Alexander, Ashley MD; Mitchell, Sarah MD; Grossman Verner, Heather M. MS; Truitt, Michael MD; Berry, Stepheny MD; Middlekauff, Jennifer BSN; Luce, Siobhan MD; Leshikar, David MD; Krowsoski, Leandra MD; Bukur, Marko MD; Polite, Nathan M. DO; McMann, Ashley H. MD; Staszak, Ryan MD; Armen, Scott B. MD; Horrigan, Tiffany MD; Moore, Forrest O. MD; Bjordahl, Paul MD; Guido, Jenny MD; Mathew, Sarah MD; Diaz, Bernardo F. MD; Mooney, Jennifer MD; Hebeler, Katherine MD; Holena, Daniel N. MD. Moving the needle on time to resuscitation: An EAST prospective multicenter study of vascular access in hypotensive injured patients using trauma video review. Journal of Trauma and Acute Care Surgery 95(1):p 87-93, July 2023. | DOI: 10.1097/TA.0000000000003958
Category: Pediatrics
Keywords: Pediatrics, infectious disease, fever, bacteremia (PubMed Search)
Posted: 7/14/2023 by Kathleen Stephanos, MD
(Updated: 2/8/2026)
Click here to contact Kathleen Stephanos, MD
This study attempts to answer the age old question: What is the importance of fever in pediatric illnesses?
The authors' goal was to assess if response to antipyretics was associated with bacteremia. This article retrospectively reviewed 6,319 febrile children in whom blood cultures were sent and found that 3.8% had bacteremia. They then looked at the fever curve in response to antipyretics for these two groups in the emergency department over 4 hours. The study concluded that patients with bacteremia have a higher rate of persistent fever despite antipyretics. It is important to note the limitations of this study. As this was retrospective, it is unclear what clinical findings resulted in blood cultures being sent - most febrile children did not have any drawn (23,999 were excluded for this reason). They did not assess other vital signs, and did not address other bacterial infections (UTI, cellulitis, meningitis, otitis media, etc). Additionally, while patients with bacteremia did have a higher likelihood of fever, the majority of patients in both groups had fever resolution within 4 hours, and both groups had some children with persistent fevers.
Overall, this does seem to support the decision to consider obtaining further testing in those children with a persistent fever, but also emphasizes the importance of not using fever resolution alone as support for discharge to home or exclusion of bacteremia from the differential.
Baker AH, Monuteaux MC, Michelson KA, Neuman MI. Resolution of Fever in the Pediatric Emergency Department and Bacteremia. Clin Pediatr (Phila). 2023;62(5):474-480.
Category: Pharmacology & Therapeutics
Keywords: Calcium, Massive transfusion protocol, Citrate, Blood products (PubMed Search)
Posted: 7/13/2023 by Wesley Oliver
(Updated: 2/8/2026)
Click here to contact Wesley Oliver
Citrate is an anticoagulant added to blood products to maintain stability for storage. With the administration of large volumes of blood products, citrate binds to ionized calcium, which can cause hypocalcemia. Evidence for specific calcium administration during massive transfusion protocols is limited; however, a proposed strategy has been to administer calcium gluconate 2 grams for every 2-4 units of red blood cells.
Robinson, et al. performed a retrospective analysis attempting to determine the optimal Citrate:Ca ratio (a novel ratio created for this study) to reduce 30-day mortality. They did not find any differences in mortality; however, they found a Citrate:Ca ratio of 2-3 produced a normalized ionized calcium level with 24 hours of a massive transfusion protocol.
Based on their calculations, this would equate to supplementing 1 g of calcium gluconate for every 3 units of red blood cells given.
***Reminder: Based on the amount of elemental calcium in each gram of calcium gluconate (4.7 mEq) and calcium chloride (13.6 mEq); 3 g calcium gluconate=1 g calcium chloride.***
Bottom Line: Supplementing with calcium gluconate 1 g for every 3 units of red blood cells should be sufficient to maintain normal ionized calcium levels after a massive transfusion protocol.
Robinson A, Rech MA, DeChristopher PJ, Vaughn A, Rubino J, Bannister E, Moore ME, Chang K. Defining the optimal calcium repletion dosing in patients requiring activation of massive transfusion protocol. Am J Emerg Med. 2023 May 13;70:96-100.
Category: Toxicology
Keywords: CO (PubMed Search)
Posted: 7/13/2023 by Mak Moayedi, MD
(Updated: 2/8/2026)
Click here to contact Mak Moayedi, MD
Age >36
LOC
Prolonged exposure (>24hrs)
COHgb level >25%
Weaver LK, Valentine KJ, Hopkins RO. Carbon monoxide poisoning: risk factors for cognitive sequelae and the role of hyperbaric oxygen. American journal of respiratory and critical care medicine. 2007;176(5):491-497. doi:10.1164/rccm.200701-026OC
Category: Trauma
Keywords: pelvic fracture, binder, hemorrhage (PubMed Search)
Posted: 7/9/2023 by Robert Flint, MD
Click here to contact Robert Flint, MD
Pelvic fractures can be a major source of life threatening hemorrhage. Suspect fracture with significant force/mechanism. Signs are pelvic tenderness (no need to “rock” the pelvis), bruising at perineum, and hypotension in the setting of major trauma. Major classifications of pelvic fractures are lateral compression, anterior posterior (wide public ramus, open book), and vertical sheer (fall from height). An appropriately applied pelvic binding device can be lifesaving. The biggest mistake in applying these devices is to apply them too high. Maximum pressure is achieved with application directly across the greater trochanters.
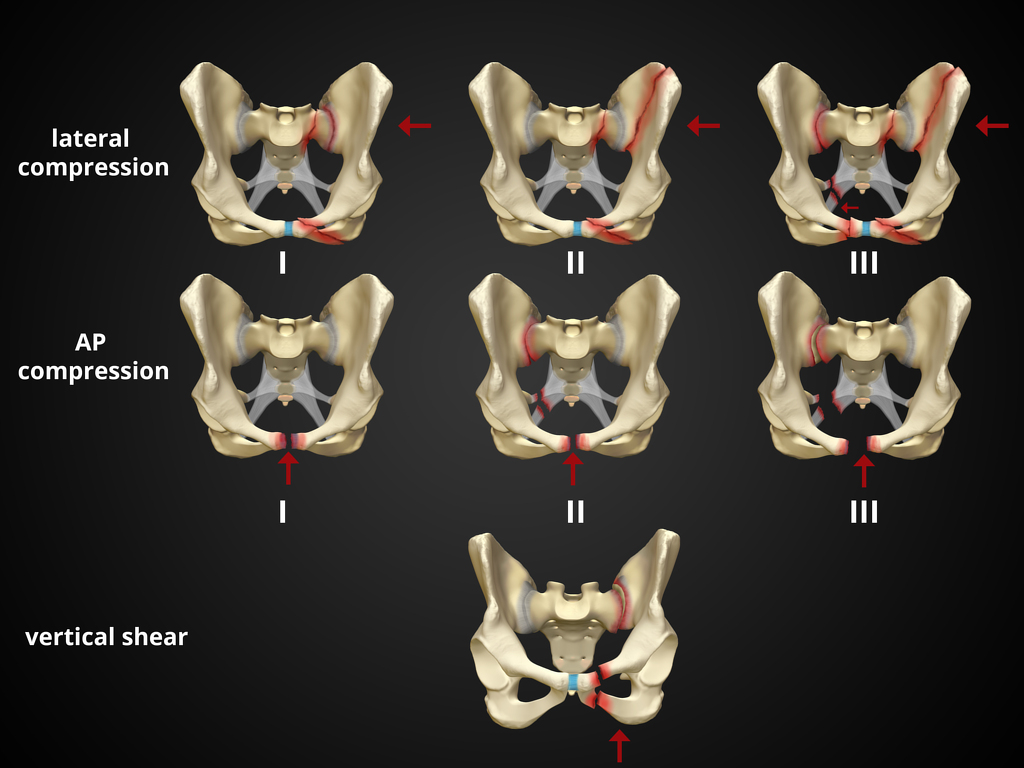
1. https://radiopaedia.org/cases/pelvic-fracture-diagrams
2. Bonner TJ, Eardley WGP, Newell N, et al. Accurate placement of a pelvic binder improves reduction of unstable fractures of the pelvic ring. J Bone Joint Surg Br. 2011;93-B(11):1524-1528. doi:10.1302/0301-620X.93B11.27023
Category: Orthopedics
Keywords: blurry vision, head trauma (PubMed Search)
Posted: 7/8/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Multiple vision disorders may occur after concussion including injury to the systems that control binocular vision including: Convergence insufficiency and Accommodation insufficiency
In order to obtain a single binocular vision, simultaneous movement of both eyes in opposite directions is required.
To look at an object close by such as when reading, the eyes must rotate towards each other (convergence).
Convergence insufficiency is the reduced ability to converge enough for near vision and is a common visual dysfunction seen after concussion.
One of both eyes may also turn outward.
May lead to complaints with reading such as diplopia, blurry vision, eyestrain, and skipping words or losing one's place.
Patient or parent may also report other difficulties such as becoming more easily fatigued when reading, needing to squint and/or having disinterest in reading.
Take home: consider testing convergence in patients with some of these complaints in setting of acute or subacute head trauma.
Master CL, Bacal D, Grady MF, Hertle R, Shah AS, Strominger M, Whitecross S, Bradford GE, Lum F, Donahue SP; AAP SECTION ON OPHTHALMOLOGY; AMERICAN ACADEMY OF OPHTHALMOLOGY; AMERICAN ASSOCIATION FOR PEDIATRIC OPHTHALMOLOGY AND STRABISMUS; and AMERICAN ASSOCIATION OF CERTIFIED ORTHOPTISTS. Vision and Concussion: Symptoms, Signs, Evaluation, and Treatment. Pediatrics. 2022 Aug 1;150(2):e2021056047.
Category: Pediatrics
Keywords: burns, pediatric (PubMed Search)
Posted: 7/7/2023 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Kliegman, R. M., MD, Stanton, B. F., MD, St Geme, J., MD, & Schor, N. F., MD PhD. (2015). Nelson Textbook of Pediatrics (20th ed.). Elsevier Health Sciences.
Category: Toxicology
Keywords: cannabis exposure, pediatric, toxicity, NPDS (PubMed Search)
Posted: 7/6/2023 by Hong Kim, MD
(Updated: 2/8/2026)
Click here to contact Hong Kim, MD
Medical Cannabis is permitted in 39 states and Washington DC while 18 sates and Washington DC has legalized recreational cannabis use. As cannabis products become more available, pediatric exposure has also increased.
A retrospective study of National Poison Data System involving children < 6 years from 2017 and 2021 showed: Pre-COVID (2017-2019) & COVID (2020-2021)
Common Clinical effects
Disposition
Conclusion
Tweet MS, Nemanich A, Wahl M. Pediatric Edible Cannabis Exposures and Acute Toxicity: 2017–2021. Pediatrics. 2023;151(2):e2022057761
Category: Gastrointestional
Keywords: POCUS, Appendicitis, Pregnancy (PubMed Search)
Posted: 7/3/2023 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
POCUS can be used to screen for appendicitis.
A recent study showed a sensitivity of 66.7% (CI 95% 47.1–82.7), and a specificity of 96.8% (CI 95% 83.3–99.9) during pregnancy, with the highest sensitivity in the first trimester.
2 methods to locate the appendix are:
1) have your patient point to the area where it hurts the most
2) perform a lawnmower technique over the right lower quadrant looking for the right psoas mucle and the iliac vessels. The appendix will usually be near these structures.
Sometimes it is easiest to use your curvilinear probe to identify an area of inflammation and then change to the linear probe for better visualization.
On ultrasound, appendicitis is defined as a non-compressible blind pouch with an outer diameter greater than 6 mm. On short axis the inflammed appendix will look like a target sign:
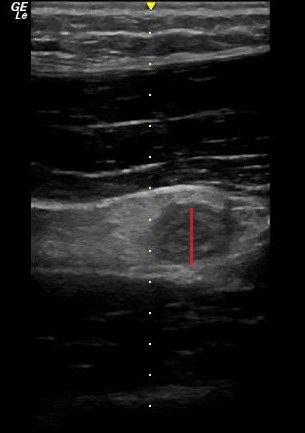
Abgottspon D, Putora K, Kinkel J, Süveg K, Widmann B, Hornung R, Minotti B. Accuracy of Point-of-care Ultrasound in Diagnosing Acute Appendicitis During Pregnancy. West J Emerg Med. 2022 Oct 23;23(6):913-918. doi: 10.5811/westjem.2022.8.56638
Category: Trauma
Keywords: shock index, trauma, pre-hospital (PubMed Search)
Posted: 7/2/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Shock index (heart rate/systolic blood pressure) has been used to predict trauma outcomes. This study from American Journal of Emergency Medicine looked at 89,000 pre-hospital patients who had a normal shock index on arrival at an emergency department. They then looked for those with abnormal pre-hospital shock index vs. those without an abnormal shock index and compared outcomes. Those with an abnormal pre-hospital shock index had worse outcomes than those with normal pre-hospital shock index.
Bottom line: A good handoff from pre-hospital to emergency department staff is critical because any abnormal shock index predicts a worse outcome than those with a normal shock index.
Yoshie Yamada Sayaka Shimizu, et al Prehospital shock index predicts 24-h mortality in trauma patients with a normal shock index upon emergency department arrival Am J Emerg Med 2023 May 10;70:101-108 doi: 10.1016/j.ajem.2023.05.008.
Category: Ophthamology
Keywords: Optho. (PubMed Search)
Posted: 6/16/2023 by Robert Flint, MD
(Updated: 6/29/2023)
Click here to contact Robert Flint, MD
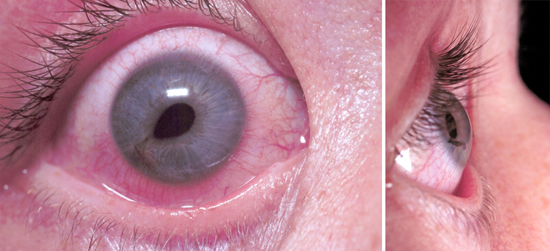
What is this called? What does it indicate? Treatment?
Tear Drop pupil. Globe rupture/corneal laceration. Protect the eye with a commercially available shield (Fox, etc) or if none is available use a paper/sytroform cup that can be cut to length to allow taping in place. Start IV antibiotics and emergency opthamology referal.
1. https://www.jems.com/patient-care/traumatic-eye-injury-management-principl-0/
2. https://eyesoneyecare.com/resources/ophthalmic-emergencies-open-globe-injuries/
