Category: Critical Care
Keywords: OHCA, Critical Care, Whole Body CT, Post Cardiac Arrest Care (PubMed Search)
Posted: 5/9/2023 by Lucas Sjeklocha, MD
Click here to contact Lucas Sjeklocha, MD
Just scan ‘em? Should everyone with unexplained out-of-hospital cardiac arrest get whole-body CT/CTA?
Background: Determination of the cause and subsequent management of out-of-hospital cardiac arrest is clinically challenging in those patients who survive to hospital admission without a clear diagnosis. CT imaging is often used to ascertain the cause of an arrest, find potentially intervenable etiologies, and assess for neurological injury but this practice and diagnostic yield are inconsistent and not well studied.
Study and Methods: The CT FIRST study is a single center cohort study using head-to-pelvis contrasted triple phase CT within 6 hours for cardiac arrest without obvious cause (sudden death CT or SDCT) studied in a before and after manner compared to usual care to determine the influence of early pan CT on diagnostic yield and outcomes. The primary outcome was diagnostic yield following SDCT and secondary outcomes include time to diagnosis of “time critical” findings and survival to discharge. 104 patients undergoing SDCT were compared to 143 historical controls after study implementation. Patients deemed to have a clear cause or are too unstable for CT were among exclusions.
Results: For the primary outcome of diagnostic yield: 92% of SDCT cohort received a separately adjudicated diagnosis for the arrest compared to 75% of the control cohort (p = 0.001). With time to such diagnosis of 3.1hrs in SDCT versus 14.1hrs of controls, with 39% versus 17% being made by CT. Time critical diagnoses including MI, PE, aortic dissection, pneumonia, embolic or hemorrhagic CVA and abdominal catastrophe were identified in 32% versus 24% (non significant) of the cohorts with delay greater than 6hrs to diagnosis reported in 12% in SDCT versus 62% in usual care (p=0.001).
There was no difference in survival to hospital discharge and no difference in safety measures and no evaluation reporting changes to and timing of patient managements.
The SDCT cohort had 100% scan rate compared to usual care where 81% received early head CT with chest CT and abdominal CT done in 36% and 18%, respectively. Notably there were no CT reported diagnoses that were later reversed on adjudication in either cohort. The planned economic and resource analysis was not reported in this study.
Discussion: There was a notable increase in diagnostic yield based on the study design with faster time to potentially time sensitive diagnoses. There were, however, no differences in mortality and it was not clear the degree to which these diagnoses influenced patient management given the limited numbers in this study and diverse set of diagnoses associated with cardiac arrest. Like previous studies of selective versus whole body CT in trauma populations, the increased diagnostic yield was not associated with reduced mortality or reported changes in management. The yield numbers suggest increased confidence by exclusion as much as positive findings of the cause. As always, the caveats of a relatively small single center before-and-after cohort study apply.
An interesting twist is that no CT diagnosis pointing to the cause of the arrest was reversed on subsequent review, this may speak to the accuracy of modern CT and radiology interpretation, but I sometimes worry that this can also be reflective of diagnostic fixation, especially with “objective” tests, as well as nihilism about the utility of clinical diagnosis.
That said, non-selective CT has many potential benefits for many critically ill and unexaminable populations with diagnostic uncertainty, as demonstrated here, which must be balanced against risks of intrahospital transport and of resource utilization as we do not yet have clear data that patients benefit from the practice despite increased diagnostic yield.
Kelley R.H. Branch, M.O. Gatewood, P.J. Kudenchuk et al., Diagnostic yield, safety, and outcomes of Head-to-pelvis sudden death CT imaging in post arrest care: The CT FIRST cohort study, Resuscitation, https://doi.org/10.1016/j. resuscitation.2023.109785
Category: Cardiology
Keywords: Posterior MI, ECG (PubMed Search)
Posted: 5/8/2023 by Leen Alblaihed, MBBS, MHA
Click here to contact Leen Alblaihed, MBBS, MHA
52 yo M with chest pain and shortness of breath, ECG as shown, do you activate cath lab?
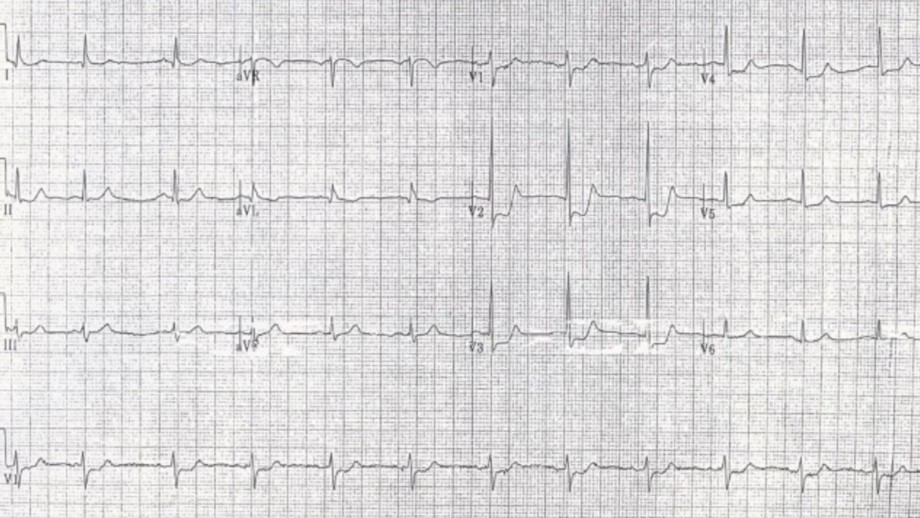
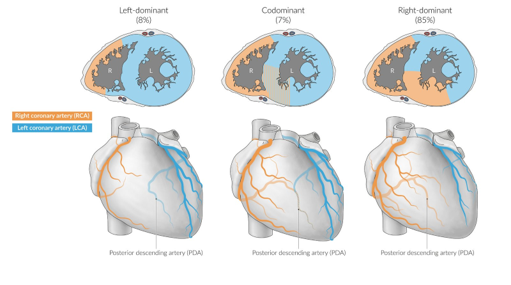
The posterior descending artery (PDA) supplies the posterior third of the interventricular septum, including the posterior and inferior walls of the left ventricle. The vessel most commonly originates from either the right coronary artery (right dominant), left circumflex artery (left dominant), or both (codominant).
Posterior MI frequently occurs as an extension of an inferior or lateral infarct. Isolated posterior MI occurs in 3 - 5% of cases (1), and is frequently missed on ECGs.
The posterior myocardium is not directly visualized on a standard 12 lead ECG, but reciprocal changes of STEMI in the anteroseptal leads (V1- V3) are seen (the posterior electrical activity is recorded from the anterior side of the heart)
If in V1- V3 you see
* ST segment depression
* Tall R wave
* Upright T waves
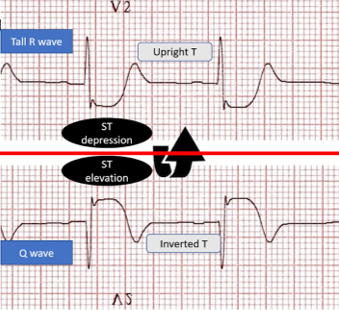
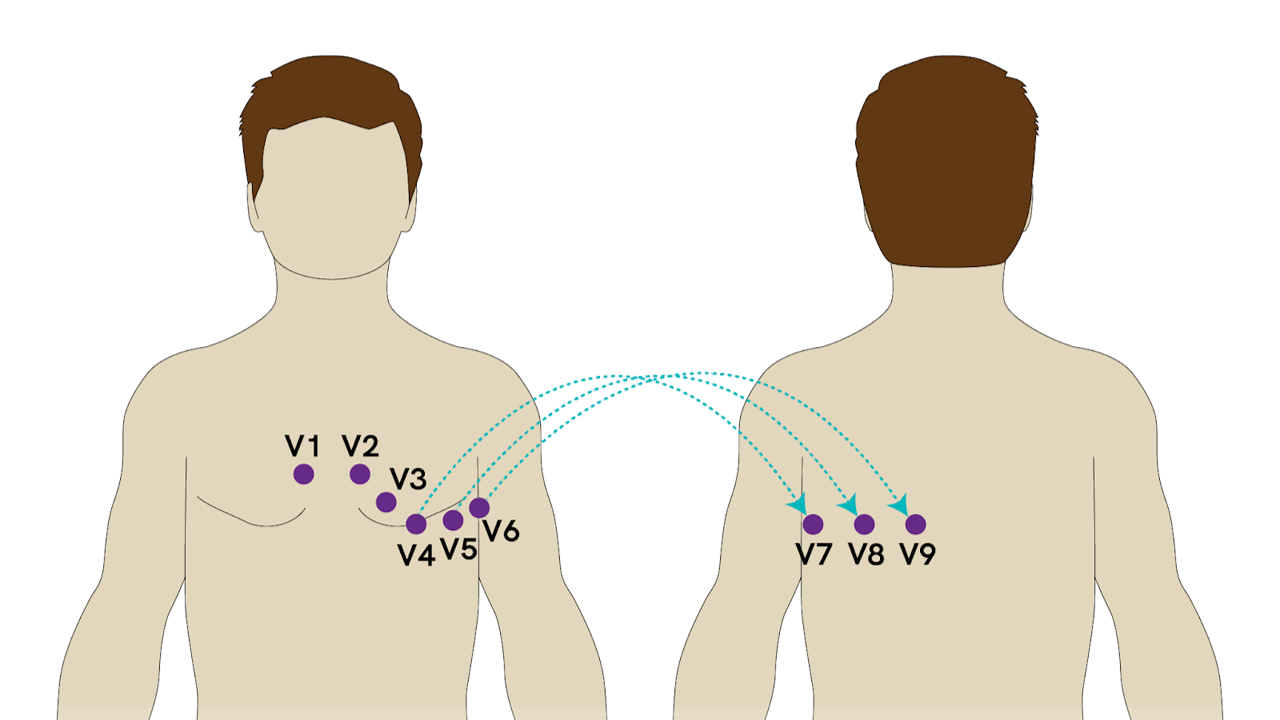
Consider posterior MI as a cause. You need to then obtain an ECG with posterior leads. If there is 0.5 mm elevation in any posterior lead this is diagnostic of posterior MI.
van Gorselen EO, Verheugt FW, Meursing BT, Oude Ophuis AJ. Posterior myocardial infarction: the dark side of the moon. Neth Heart J. 2007 Jan;15(1):16-21
Category: Trauma
Keywords: trauma, vasopressors, mass transfusion, uncertainty (PubMed Search)
Posted: 5/7/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This extensive review looks at the literature surrounding vasopressors in trauma. Take away points are:
1. Most of the studies were done when the use of crystalloid was still being used as initial resuscitation fluid instead of blood.
2. Use of whole blood and mass hemorrhage protocols are not reflected in the literature regarding vasopressor use.
3. There are physiologic reasons vasopressors could be useful, particularly in head injured patients where we want increased mean arterial pressures.
4. European guidelines include vasopressor use whereas American ones do not.
5. Vasopressin and norepinephrine appear to be the vasopressors of choice if using a vasopressor in a trauma patient.
6. We need better studies looking at this topic
7. We need better studies looking at permissive hypotension in trauma now that our resuscitative strategy emphasizes mass hemorrhage protocol of blood, blood products, TXA and hemorrhage control.
8. As with all things in medicine, never say never.
Richards, Justin E. MD*; Harris, Tim MD†,‡; Dünser, Martin W. MD§; Bouzat, Pierre MD, PhD?; Gauss, Tobias MD¶. Vasopressors in Trauma: A Never Event?. Anesthesia & Analgesia 133(1):p 68-79, July 2021. | DOI: 10.1213/ANE.0000000000005552
Category: Pediatrics
Keywords: Pediatrics, infections, neonatal (PubMed Search)
Posted: 5/5/2023 by Rachel Wiltjer, DO
(Updated: 2/8/2026)
Click here to contact Rachel Wiltjer, DO
Neonatal rashes are common and, usually, benign. There are some skin findings, however, that require early recognition and treatment for best outcomes. One of these concerning etiologies is omphalitis, infection of the umbilical stump and surrounding tissues.
Features of omphalitis may include erythema and induration around the umbilicus, purulent drainage, and potentially systemic illness.
Risk factors include poor cord hygiene, premature or prolonged rupture of membranes, maternal infection, low birth weight, umbilical catheterization, and home birth.
Evaluation includes surface cultures from the site of infection as well as age-appropriate fever workup if patient is febrile. Consider ultrasound to evaluate for urachal anomalies as these can co-exist.
Management is IV antibiotics to cover S. aureus and gram negatives with surgical consultation if there are signs of necrotizing fasciitis or abscess. Some newer literature suggests that patients with omphalitis seen and treated in high-income countries may not be as sick as previously thought (as most data has been obtained in lower income countries where incidence is higher) and there has been a suggestion that there may be a role for oral antibiotics in well appearing, lower risk infants. This deserves further exploration but cannot yet be considered standard of care.
Other umbilical cord findings to consider (when it isn’t omphalitis): patent urachus, granuloma, local irritation, or partial cord separation
Kaplan RL. Omphalitis: Clinical Presentation and Approach to Evaluation and Management. Pediatr Emerg Care. 2023;39(3):188-189.
Category: Critical Care
Keywords: etomidate, intubation, critically ill, mortality (PubMed Search)
Posted: 5/2/2023 by Quincy Tran, MD, PhD
(Updated: 2/8/2026)
Click here to contact Quincy Tran, MD, PhD
As emergency physicians, we use etomidate to intubate patients most of the time, although there was controversy whether etomidate would suppress critically ill patients’ cortisol production. Whether etomidate was associated with mortality was controversial. A recent meta-analysis investigated the issue again.
Methods: meta-analysis of randomized trials using etomidate for intubation versus other agents. Outcome = mortality as defined by the authors. Mortality was defined from 24 hours to 30 days by study’s authors.
Results: 11 RCTs, including one new RCT in 2022
319 (1359, 23%) patients received etomidate died vs. 267 (1345, 20%) receiving other agents died; Risk Ratio 1.16, 95% CI 1.01-1.33, P = 0.03.
Etomidate was also associated with higher risk ratio for adrenal insufficiency, when compared with other control agents (147/695, 21% vs. 69/686, 10%, RR 2.01, 95% CI (1.59-2.56), P < 0.01.
Etomidate was also associated with higher risk ratio of mortality, when compared with ketamine, for mortality, as defined by each study’s author (273/1201, 23% vs. 226/1198. 19%. RR 1.18, 95% CI 1.02-1.37, P = 0.03).
Discussion:
The authors used fixed effects model, as they claimed that their meta-analysis had low heterogeneity (I2 =0%). However, fixed effects model should only be used when there is no difference among patient population. In this study, the outcome definitions were different, the patient populations were different (trauma, pre-hospital, ED, ICU). Therefore, random effects model should be used. Random effects models tend to yield larger 95% CI, thus, more likely yield non-statistically significant results.
The authors claimed a Number Needed To Treat (NNT) for etomidate of 31, so basically many ED patients would die, while most of patients being intubated by Anesthesiology, regarding settings, would not die, as anesthesiologists mostly use propofol.
Category: Cardiology
Keywords: POCUS, ACS, Regional Wal Motion Abnormality, Ultrasound (PubMed Search)
Posted: 5/1/2023 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
In this study the researchers looked at patients presenting to the emergency department with high suspicion for ACS and explored if Regional Wall Motion Abnormality (RWMA) evaluation by EPs was associated with occlusion myocardial ischemia (OMI).
FOCUS identified RWMA in 87% of patients with coronary angiography proven OMI. With a sensitivity of 94%, specificity 35%, and overall accuracy of 78%.
The authors concluded that using FOCUS can have good utility when a patient is high risk for OMI and has an equivocal ekg. However, if RWMA is not present, physicians should still continue with work up such as cardiac catheterization.
To evaluate RWMA it is easiest to:
For more information check out this ACEPnow article: https://www.acepnow.com/article/detect-cardiac-regional-wall-motion-abnormalities-point-care-echocardiography/?singlepage=1
Bracey A, Massey L, Pellet AC, Thode HC, Holman TR, Singer AJ, McClure M, Secko MA. FOCUS amay detect wall motion abnormalities in patients with ACS, A retrospective study. Am J Emerg Med. 2023 Apr 2;69:17-22. doi: 10.1016/j.ajem.2023.03.056. Epub ahead of print. PMID: 37037160.
Category: Trauma
Keywords: CXR, blunt aortic injury (PubMed Search)
Posted: 4/30/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
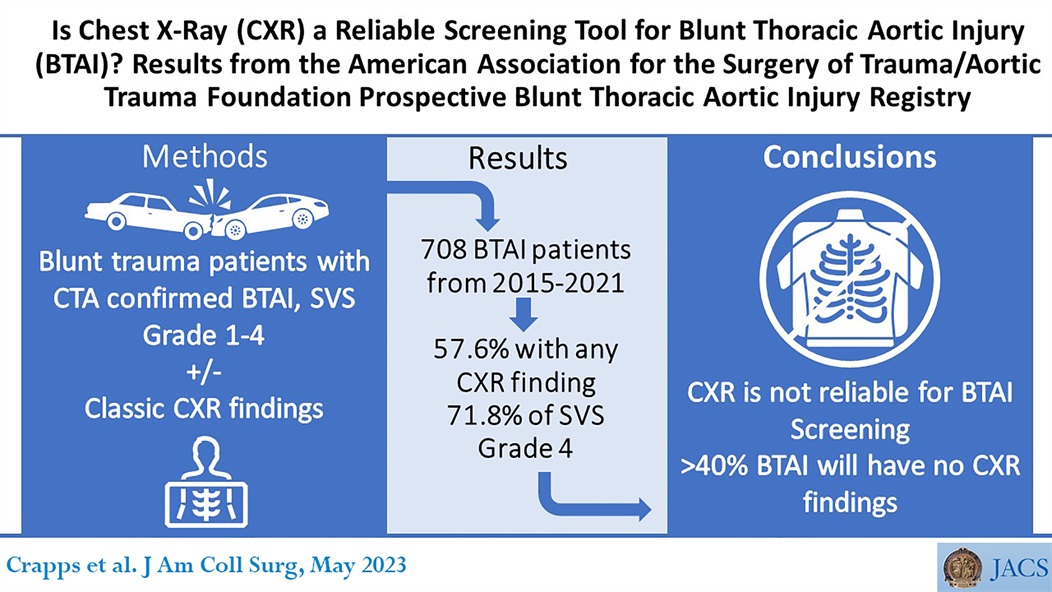
Crapps, Joshua L md; Efird, Jessica md; DuBose, Joseph J md, facs; Teixeira, Pedro G md, facs; Shrestha, Binod md, mba; Brown, Carlos VR md, facs. Is Chest X-Ray a Reliable Screening Tool for Blunt Thoracic Aortic Injury? Results from the American Association for the Surgery of Trauma/Aortic Trauma Foundation Prospective Blunt Thoracic Aortic Injury Registry. Journal of the American College of Surgeons 236(5):p 1031-1036, May 2023. | DOI: 10.1097/XCS.0000000000000607
Category: Critical Care
Posted: 4/25/2023 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
Hypoxemic respiratory failure is a common presentation of critically ill patients. If the degree of hypoxemia is severe and disproportionate to the patient's radiographic findings and not responding to increasing FiO2, a right-to-left shunt should be considered. To evaluate for an anatomic shunt, an intravenous agitated saline contrast (ASC) echocardiographic evaluation can be conducted by an ED provider at the bedside.
Technique:
Interpretation:
Millington SJ, Mayo-Malasky H, Koenig S. Agitated saline contrast injection in patients with severe hypoxemia. J Intensive Care Med. 2023;38(5):479-486.
Category: Procedures
Keywords: inhospital cardiac arrest, manual compression devices (PubMed Search)
Posted: 3/28/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This is a review of the literature surrounding using mechanical compression devices for in-hospital cardiac arrest. The bottom line is there isn’t much evidence to support the use of these devices and there is scant literature in general on this topic. This is an area in need of further research
Mechanical Cardiopulmonary Resuscitation During In?Hospital Cardiac Arrest
Oscar J. L. Mitchell,Xinyi Shi, Benjamin S. Abella and Saket Girotra
Originally published21 Mar 2023https://doi.org/10.1161/JAHA.122.027726 Journal of the American Heart Association. 2023;0:e027726
Category: Pediatrics
Keywords: Ketamine, morphine, fentanyl, pediatrics, EMS, pain control (PubMed Search)
Posted: 4/21/2023 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Frawley J, Goyal A, Gappy R, et al. A Comparison of Prehospital Pediatric Analgesic Use of Ketamine and Opioids [published online ahead of print, 2023 Mar 8]. Prehosp Emerg Care. 2023;1-5. doi:10.1080/10903127.2023.
Category: Critical Care
Posted: 4/20/2023 by William Teeter, MD
Click here to contact William Teeter, MD
CCM recently published Stanford's experience with their Emergency Critical Care Program (ECCP), an ED based intensivist consultation/management model staffed by EM/CC during peak hours with the "goals of improving care of the critically ill in the ED, offloading the ED team, and optimizing ICU bed utilization without the need for a dedicated physical space."
Conclusions:
This is the third group to document decrease in overall mortality utilizing an early or dedicated critical care consult model. EC3 and the CCRU here at UMMC have also both shown improvements in patient transfer and resource utilization metrics. As with all studies in this space, there are many limitations to these studies in both design and generalizability, even amongst each other. However, the literature is replete with data that increased boarding time in the ED for critically ill patients is associated with worse outcomes and these studies are now a body of complementary and growing evidence that teams such as this can perhaps bridge that gap. Hopefully come to an ED near you soon...
Study Details:
Objectives: To determine whether implementation of an Emergency Critical Care Program (ECCP) is associated with improved survival and early downgrade of critically ill medical patients in the emergency department (ED).
Design: Single-center, retrospective cohort study from a tertiary academic medical center using ED-visit data between 2015 and 2019 for adult medical patients presenting to the ED with a critical care admission order within 12 hours of arrival.
Pre and post intervention (2017) cohort analysis of patients when facility implemented dedicated bedside critical care by an ED-based intensivist "following initial resuscitation by the ED team". A difference-in-differences (DiD) analysis compared the change in outcomes for patients arriving during ECCP hours (2 pm to midnight, weekdays) between the preintervention period (2015–2017) and the intervention period (2017–2019) to the change in outcomes for patients arriving during non-ECCP hours (all other hours).
Primary outcomes: In-hospital mortality and proportion of patients downgraded to non-ICU status while in the ED within 6 hours
Results:
Mitarai, Tsuyoshi; Gordon, Alexandra June; Nudelman, Matthew J et al. Association of an Emergency Critical Care Program With Survival and Early Downgrade Among Critically Ill Medical Patients in the Emergency Department. Critical Care Medicine ():10.1097/CCM.0000000000005835.
Gunnerson KJ, Bassin BS, Havey RA, et al.: Association of an emergency department–based intensive care unit with survival and inpatient intensive care unit admissions. JAMA Netw Open 2019; 2:e197584
Tran QK, O’Connor J, Vesselinov R, et al.: The critical care resuscitation unit transfers more patients from emergency departments faster and is associated with improved outcomes. J Emerg Med 2020; 58:280–289
Category: Trauma
Keywords: elderly, cervical spine, trauma, systematic review (PubMed Search)
Posted: 3/28/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In a systematic review looking at patients over age 65 who sustained a cervical spine injury from a low-level fall, there was a 3.8% prevalence of injury identified. The paper could not correlate injury with GCS level or altered level of consciousness due to the quality of the data available.
Bottom line again is patients over age 65 with low-level falls should be considered to have significant injury until proven otherwise.
Cervical spine injuries in adults ≥ 65 years after low-level falls - A systematic review and meta-analysis.
Jessica McCallum, Debra Eagles, Yongdong Ouyang, Jamie Vander Ende, Christian Vaillancourt, Christophe Fehlmann, Risa Shorr, Monica Taljaard, Ian Stiell
American Journal of Emergency Medicine 2023 Februrary 11
Category: Critical Care
Keywords: Glucagon, Beta Blocker, Calcium Channel Blocker, Overdose (PubMed Search)
Posted: 4/11/2023 by Zach Rogers, MD
Click here to contact Zach Rogers, MD
Glucagon therapy in beta blocker and calcium channel blocker overdose is controversial and no high level evidence is available to support or refute its use in overdose treatment.
Glucagon has the ability to bypass adrenergic blockade from beta and calcium channel blocking agents and theoretically increase myocardial contraction, increase heart rate, and increase AV conduction through cyclic AMP production.
However, practically, the use of glucagon is limited due to high risk of vomiting and subsequent risk of aspiration with administration as well as the high cost and limited hospital stock available for continued use.
Given these limitations, glucagon therapy is no longer recommended for calcium channel blocker overdose in the 2017 Critical Care Medicine Expert Consensus*. The use in beta blocker therapy is still recommended. However, caution must be taken to ensure that more advanced (and possibly more efficacious) therapies such as vasopressors and high dose insulin are administered without delay.
The dose of glucagon therapy for this indication is 3-10 mg IV. You can repeat this dose a second time if no response is seen with the first dose. If clinical response is seen with bolus dosing, transition to continuous infusion at the dose of clinical response (eg. if two 5 mg boluses produced the desired response; start 10 mg/hr infusion). Antiemetic administration prior to initial bolus dose is highly recommended to avoid vomiting.
Peterson CD, Leeder JS, Sterner S. Glucagon therapy for beta-blocker overdose. Drug Intell Clin Pharm. 1984 May;18(5):394-8. doi: 10.1177/106002808401800507. PMID: 6144498.
*St-Onge M, Anseeuw K, Cantrell FL, Gilchrist IC, Hantson P, Bailey B, Lavergne V, Gosselin S, Kerns W 2nd, Laliberté M, Lavonas EJ, Juurlink DN, Muscedere J, Yang CC, Sinuff T, Rieder M, Mégarbane B. Experts Consensus Recommendations for the Management of Calcium Channel Blocker Poisoning in Adults. Crit Care Med. 2017 Mar;45(3):e306-e315. doi: 10.1097/CCM.0000000000002087. PMID: 27749343; PMCID: PMC5312725.
Khalid MM, Galuska MA, Hamilton RJ. Beta-Blocker Toxicity. [Updated 2023 Feb 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448097/
Category: Trauma
Keywords: TXA, intramuscular, pre-hospital (PubMed Search)
Posted: 3/28/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This paper looks at the possibility of intramuscular tranexamic acid (TXA) administration. Pharmacologic studies support this route as giving correct drug bioavailability to control hemorrhage. Several London, England pre-hospital services have begun using intramuscular TXA for trauma patients when intravenous access cannot be quickly obtained. This paper suggests 500 mg intramuscular injection dosing.
Journal of Intensive Care volume 11, Article number: 12 (2023)
Category: Orthopedics
Keywords: lower back pain, analgesia, NSAIDs (PubMed Search)
Posted: 4/8/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Acute lower back pain is a very common emergency department presenting complaint. Over the last several years there has been impetus to move away from opioids in the management of lower back pain.
A recent systematic review investigated the pharmacologic management of acute low back pain. This review looked at RCTs investigating the efficacy of muscle relaxants, NSAIDs, and acetaminophen for the treatment of acute nonspecific lower back pain of fewer than 12 weeks duration in patients > 18 years of age. Studies that investigated the use of opioids were not considered.
18 RCTs, totaling 3478 patients were included. 54% were women. The mean patient age was 42.5 ± 7.3 years. The mean length of follow-up was 8.0 ± 5.6 days. The mean duration of symptoms before treatment was 15.1 ± 10.3 days.
Results: Muscle relaxants and NSAIDs were effective in reducing pain and disability in acute LBP at approximately 1 week.
The combination of NSAIDs and acetaminophen was associated with a greater improvement than the sole administration of NSAIDs.
However, acetaminophen alone did not promote any significant improvement. Placebo administration was not effective.
Limitations: Most patients with acute LBP experience spontaneous recovery or at least reduction of symptoms, therefore, the real impact of most medications is uncertain. The present study wasn't able to distinguish among different classes of NSAIDs. A best practice treatment protocol cannot be extrapolated from this study.
Take home: In my practice, patients are treated with NSAIDs and Acetaminophen first line. I also include Licocaine patches for all patients. If there is a contraindication to NSAIDs, I treat with muscle relaxants alone.
This study highlights the lack of benefit of acetaminophen as mono therapy (which has been noted in other studies).
Baroncini A, et al. Nonopioid pharmacological management of acute low back pain: A level I of evidence systematic review. J Orthop Res. 2023 Feb 22. doi: 10.1002/jor.25508.
Category: Pediatrics
Keywords: sedation, anxiolysis, procedure (PubMed Search)
Posted: 4/7/2023 by Rachel Wiltjer, DO
Click here to contact Rachel Wiltjer, DO
Background: Intranasal dexmedetomidine has seen usage in the anesthesia and sedation realms over the past few years, with an increasing interest in usage in the ED setting given its generally favorable safety profile and ease of administration. There has been specific interest and consideration in children with autism and neurodevelopmental disorders.
Study: Single center prospective provider study (compared to a retrospective group of patients under 18 who received oral midazolam for indications of agitation or anxiety via chart review) looking at patients 6 months to 18 years of age with an order for intranasal dexmedetomidine. Following use, a provider survey was completed to evaluate indication/rationale for use, satisfaction, comfort with use, and perceived time to onset as well as duration of effect.
Results: 29% of patients receiving IN dexmedetomidine experienced treatment failure compared with 20.7% of patients receiving oral midazolam (not statistically significant). In subgroup analysis, rates of treatment failure were lower for patients diagnosed with autism spectrum disorder receiving IN dexmedetomidine versus oral versed (21.2% versus 66.7%). Length of stay was longer in the IN dexmedetomidine group (6.0 hours versus 4.4 hours). Indication for use had variability between the two groups.
Bottom Line: IN dexmedetomidine may be a reasonable agent to utilize for anxiolysis in pediatric patients, especially those who have previously had paradoxical reactions or poor efficacy of benzodiazepines. It may be specifically useful when effects are desired for a slightly longer time and for non-painful/minimally painful interventions.
Kenneally A, Cummins M, Bailey A, Yackey K, Jones L, Carter C, Dugan A, Baum RA. Intranasal Dexmedetomidine Use in Pediatric Patients for Anxiolysis in the Emergency Department. Pediatr Emerg Care. 2023 Jan 5. Epub ahead of print.
Category: Critical Care
Keywords: pneumonia, acute hypoxic respiratory failure, steroids (PubMed Search)
Posted: 4/5/2023 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Background: The use of steroids in pneumonia has long been controversial with conflicting data, and the recent ESCAPe randomized controlled trial by Meduri et al. showing no mortality benefit with their use, but likely underpowered due to recruitment issues. The recently published CAPE COD study by Dequin et al. may change the game.
Design: Double-blind, placebo-controlled, multicenter, RCT
Intervention: Early hydrocortisone within 24 hrs, 200mg/day x 4-8 days depending on improvement, then preset taper
Primary outcome: Death at 28 days
Secondary outcomes:
Bottom Line: The addition of hydrocortisone to antibiotics in severe CAP may decrease need for intubation and development of shock, and in this well-done study, decreased 28 and 90-day mortality.
Meduri GU, Shih MC, Bridges L, et al; ESCAPe Study Group. Low-dose methylprednisolone treatment in critically ill patients with severe community-acquired pneumonia. Intensive Care Med. 2022 Aug;48(8):1009-1023. doi: 10.1007/s00134-022-06684-3. Epub 2022 May 13. PMID: 35723686.
doi: 10.1056/NEJMoa2215145. Epub ahead of print. PMID: 36942789.
Category: Trauma
Keywords: sexual assault, injury, trauma, intimate partner violence (PubMed Search)
Posted: 3/28/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
A retrospective review of patients over age 13 presenting to one urban level one trauma center and one urban community hospital looked at traumatic injuries in patients presenting for sexual assault. They looked at 157 patients and found 61% of assailants were acquaintances, 22% strangers, and 15% intimate partners. One third of all patients had some traumatic injury however only 12 patients has serious injuries such as non-fatal strangulation or a fracture. Assault by an intimate partner was more likely to lead to injury/trauma including non-fatal strangulation. Drug and alcohol use was not associated with presence of injury.
Traumatic Injuries in Sexual Assault Patients in the Emergency Department
Denise McCormack, et al. Western Journal of Emergency Medicine Volume 23, no5; September 2022
Category: Pharmacology & Therapeutics
Keywords: Myasthenia gravis, Myasthenic crisis, neuromuscular blocker, paralytic, rocuronium, vecuronium, succinylcholine (PubMed Search)
Posted: 4/1/2023 by Matthew Poremba
Click here to contact Matthew Poremba
Myasthenia gravis is an autoimmune disease of the neuromuscular junction, most commonly due to antibodies attacking acetylcholine receptors in the postsynaptic membrane. Up to 30% of patients with myasthenia gravis will experience a myasthenic crisis during their disease course. If rapid sequence intubation is indicated, the unique characteristics of this patient population must be considered in the event use of a paralytic is necessary. All paralytic agents can be expected to last significantly longer, and an unpredictable response may be seen with depolarizing agents - therefore non-depolarizing agents are preferred in this population.
Non-Depolarizing Agents (Rocuronium, Vecuronium)
Depolarizing Agents (Succinylcholine)
Roper J, Fleming ME, Long B, Koyfman A. Myasthenia Gravis and Crisis: Evaluation and Management in the Emergency Department. J Emerg Med. 2017;53(6):843-853.
Abel, Mark, and James B Eisenkraft. “Anesthetic implications of myasthenia gravis.” The Mount Sinai journal of medicine, New York vol. 69,1-2 (2002): 31-7.
Category: Critical Care
Keywords: Pancreatitis, IV Fluids, Hydration (PubMed Search)
Posted: 3/28/2023 by Mark Sutherland, MD
(Updated: 2/8/2026)
Click here to contact Mark Sutherland, MD
The classic teaching is that patients with acute pancreatitis should be aggressively hydrated with IV fluids. But as we increasingly question heavy handed fluid strategies in other areas such as sepsis, should we look at pancreatitis management too?
Li et al did a systematic review of the literature on aggressive fluid resuscitation (the exact protocol/definition varied per study, but we're mostly talking 15-20 mL/kg boluses followed by 3-5 mL/kg/hr infusion) vs less aggressive fluid resuscitation (mostly 10 mL/kg boluses followed by 1.5 mL/kg/hr infusion). They found that aggressive resuscitation worsened mortality in severe pancreatitis (RR 2.45) and trended towards worse mortality in non-severe pancreatitis (RR 2.26, but CI crossed 1). Aggressive was associated with more complications in both severe and non-severe pancreatitis pancreatitis.
Multiple society guidelines still call for aggressive IVF resuscitation for acute pancreatitis, but probably need to be updated given mounting evidence that this is harmful. More recent guidelines suggest "goal-directed therapy", but no one is completely sure what that means.
Bottom Line: In acute pancreatitis, a more conservative empiric IVF resuscitation is probably better than the clasically taught aggressive approach. Whether even less fluids would be better or worse is not known, but for now it's probably best to stick to a 10 mL/kg bolus and 1-2 mL/kg/hr infusion when ordering fluids for these patients unless you have another indication.
Li, XW., Wang, CH., Dai, JW. Comparison of clinical outcomes between aggressive and non-aggressive intravenous hydration for acute pancreatitis: a systematic review and meta-analysis. Crit Care 27, 122 (2023). https://doi.org/10.1186/s13054-023-04401-0
de-Madaria E, Buxbaum JL, Maisonneuve P, García García de Paredes A, Zapater P, Guilabert L, Vaillo-Rocamora A, Rodríguez-Gandía MÁ, Donate-Ortega J, Lozada-Hernández EE, Collazo Moreno AJR, Lira-Aguilar A, Llovet LP, Mehta R, Tandel R, Navarro P, Sánchez-Pardo AM, Sánchez-Marin C, Cobreros M, Fernández-Cabrera I, Casals-Seoane F, Casas Deza D, Lauret-Braña E, Martí-Marqués E, Camacho-Montaño LM, Ubieto V, Ganuza M, Bolado F; ERICA Consortium. Aggressive or Moderate Fluid Resuscitation in Acute Pancreatitis. N Engl J Med. 2022 Sep 15;387(11):989-1000. doi: 10.1056/NEJMoa2202884. PMID: 36103415.
