Category: Vascular
Keywords: aortic aneurysm; point-of-care ultrasound; pocus; aortic dissection (PubMed Search)
Posted: 12/4/2023 by Alexis Salerno Rubeling, MD
(Updated: 2/7/2026)
Click here to contact Alexis Salerno Rubeling, MD
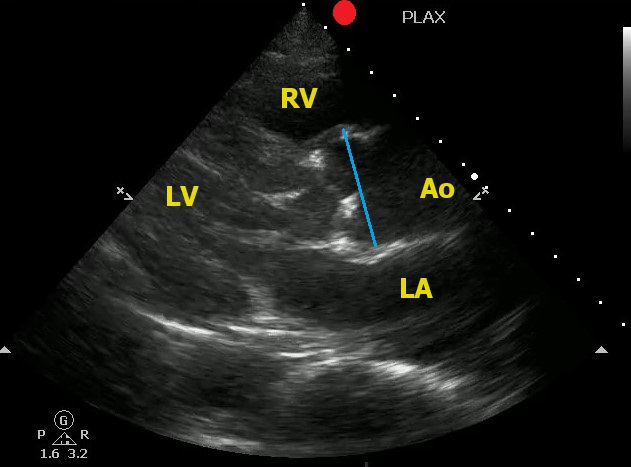
Point-of-Care Ultrasound can help to identify signs of thoracic aortic dissection.
One view to help in your assessment is the Parasternal Long Axis View.
To correctly measure the aortic root:
Here is an example of an aortic root aneurysm:
Kennedy Hall M, Coffey EC, Herbst M, Liu R, Pare JR, Andrew Taylor R, Thomas S, Moore CL. The "5Es" of emergency physician-performed focused cardiac ultrasound: a protocol for rapid identification of effusion, ejection, equality, exit, and entrance. Acad Emerg Med. 2015 May;22(5):583-93. doi: 10.1111/acem.12652.
Category: Trauma
Keywords: prehospital, EDTCO2, mortality (PubMed Search)
Posted: 12/3/2023 by Robert Flint, MD
Click here to contact Robert Flint, MD
A retrospective study of 2 years of data from 24 trauma centers looking at end tidal CO2 as a predictor of mortality in trauma patients found:
"A total of 1,324 patients were enrolled. ETCO2 was better in predicting mortality than shock index (SI) and systolic blood pressure (SBP). Prehospital lowest ETCO2 , SBP , and SI were all predictive of Mass Transfusion."
Another data point to consider when setting up trauma triage protocols and looking for patients who will require intensive interventions early.
Campion EM, Cralley A, Sauaia A, Buchheit RC, Brown AT, Spalding MC, LaRiccia A, Moore S, Tann K, Leskovan J, Camazine M, Barnes SL, Otaibi B, Hazelton JP, Jacobson LE, Williams J, Castillo R, Stewart NJ, Elterman JB, Zier L, Goodman M, Elson N, Miner J, Hardman C, Kapoen C, Mendoza AE, Schellenberg M, Benjamin E, Wakam GK, Alam HB, Kornblith LZ, Callcut RA, Coleman LE, Shatz DV, Burruss S, Linn AC, Perea L, Morgan M, Schroeppel TJ, Stillman Z, Carrick MM, Gomez MF, Berne JD, McIntyre RC, Urban S, Nahmias J, Tay E, Cohen M, Moore EE, McVaney K, Burlew CC. Prehospital end-tidal carbon dioxide is predictive of death and massive transfusion in injured patients: An Eastern Association for Surgery of Trauma multicenter trial. J Trauma Acute Care Surg. 2022 Feb 1;92(2):355-361. doi: 10.1097/TA.0000000000003447. PMID: 34686640.
Category: Quality Assurance/Quality Improvement
Keywords: Checklists, Patient Safety, Quality (PubMed Search)
Posted: 12/2/2023 by Brent King, MD
Click here to contact Brent King, MD
The Bottom Line: Investigators studying the use of a pre-intubation checklist versus "usual care" found no differences in important outcomes such as oxygen saturation and first pass success. However, the study was conducted as a part of a larger study, was unblinded, and not well controlled.
The investigators who conducted the multicenter CHECK UP trial, a study of head up intubation in ICU patients, reviewed the care of 262 ICU patients who were intubated. Some intubation attempts were guided by a pre-intubation checklist and some were not. The authors found no difference between the groups in lowest SPO2, number of intubation attempts, etc. However, the study was unblinded and largely observational. In many cases, the elements of a checklist had been incorporated into routine practice.
Take Home Point: While the authors found no differences in outcomes, this study does little to prove or disprove the value of pre-intubation checklists. Not only was the study essentially uncontrolled, the untoward events being studied are unusual in the hands of experienced clinicians.
Comment: Pre-procedural checklists make intuitive sense to me. They help us to avoid cultural drift. I am certainly not ready to abandon the use of a pre-intubation checklist based upon this study
Janz DR, Semler MW, Joffe AM, et al. A multicenter, randomized trial of a checklist for endotracheal intubation of critically ill adults. Chest 2018;153:816-824.
Category: Pediatrics
Posted: 12/1/2023 by To-Lam Nguyen, MD
Click here to contact To-Lam Nguyen, MD
Since Christmas is coming up, let's talk about Hemophilia A (factor VIII deficiency) and Hemophilia B (factor IX deficiency, also known as Christmas disease)
Deficiencies in Factors VIII and IX are the most common severe inherited bleeding disorders.
Pathophysiology:
Clinical Manifestations:
Lab findings and diagnosis
Genetics
Classification
trauma to induce bleeding
Treatment
Summary:
Kliegman R, Stanton B, St. Geme JW, Schor NF, Behrman RE. Nelson Textbook of Pediatrics. Edition 20. Elsevier; 2016. Accessed December 1, 2023. https://search.ebscohost.com/login.aspx?direct=true&db=cat01362a&AN=hshs.004567758&site=eds-live
Category: Pediatrics
Posted: 12/1/2023 by To-Lam Nguyen, MD
Click here to contact To-Lam Nguyen, MD
Since Christmas is coming up, let's talk about Hemophilia A (factor VIII deficiency) and Hemophilia B (factor IX deficiency, also known as Christmas disease)
Deficiencies in Factors VIII and IX are the most common severe inherited bleeding disorders.
Pathophysiology:
Clinical Manifestations:
Lab findings and diagnosis
Genetics
Classification
trauma to induce bleeding
Treatment
Summary:
Kliegman R, Stanton B, St. Geme JW, Schor NF, Behrman RE. Nelson Textbook of Pediatrics. Edition 20. Elsevier; 2016. Accessed December 2, 2023. https://search.ebscohost.com/login.aspx?direct=true&db=cat01362a&AN=hshs.004567758&site=eds-live
Kliegman R, Stanton B, St. Geme JW, Schor NF, Behrman RE. Nelson Textbook of Pediatrics. Edition 20. Elsevier; 2016. Accessed December 2, 2023. https://search.ebscohost.com/login.aspx?direct=true&db=cat01362a&AN=hshs.004567758&site=eds-live
Category: Critical Care
Posted: 11/28/2023 by Caleb Chan, MD
(Updated: 2/7/2026)
Click here to contact Caleb Chan, MD
McCallister R, Nuppnau M, Sjoding MW, Dickson RP, Chanderraj R. In patients with sepsis, initial lactate clearance is confounded highly by comorbidities and poorly predicts subsequent lactate trajectory. CHEST. 2023;164(3):667-669.
Category: Hematology/Oncology
Keywords: Transfusion, Anemia, MI, ACS, hematology (PubMed Search)
Posted: 11/27/2023 by Sarah Dubbs, MD
Click here to contact Sarah Dubbs, MD
Hot off the NEJM press, published November 11, 2023:
Restrictive or Liberal Transfusion Strategy in Myocardial Infarction and Anemia (Carson, Brooks, Hebert, et al Myocardial Ischemia and Transfusion (MINT) Investigators)
3504 pateints were included in this study. A primary-outcome event occurred in 295 of 1749 patients (16.9%) in the restrictive-strategy group and in 255 of 1755 patients (14.5%) in the liberal-strategy group. More specifically, death occurred in 9.9% of the patients with the restrictive strategy and in 8.3% of the patients with the liberal strategy; myocardial infarction occurred in 8.5% and 7.2% of the patients, respectively.
Conclusions from the study: Liberal transfusion strategy did NOT significantly reduce the risk of recurrent MI or death at 30 days.
N Engl J MedCarson JL, Brooks MM, Hébert PC, et al. Restrictive or Liberal Transfusion Strategy in Myocardial Infarction and Anemia. . Published online November 11, 2023. doi:10.1056/NEJMoa2307983
Category: Trauma
Keywords: Geriatric, trauma, mortality, risk factors (PubMed Search)
Posted: 11/26/2023 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
A chart review of 1300 patients over age 65 admitted to the trauma service, arrived as a trauma activation, or had an injury severity score over 12 over a 6 year period looking at 30 day mortality found:
"five factors associated with increased 30-day mortality in older trauma patients: GCS < 15, ISS > 15, age ≥ 85 years, anticoagulation, and multimorbidity."
Fall from standing was the leading cause of trauma
Again, fragility is the index we should be using, not age alone. This study is limited in its retrospective chart review nature. Prospective research in the area of geriatric trauma is needed. Until then, assess those over age 65 for risk factors associated with fragility and treat accordingly.
Yadav, K., Lampron, J., Nadj, R. et al.Predictors of mortality among older major trauma patients. Can J Emerg Med 25, 865–872 (2023). https://doi.org/10.1007/s43678-023-00597-w
Category: Orthopedics
Keywords: foot injury (PubMed Search)
Posted: 11/25/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
The fleck sign of the foot is a small bony fragment seen in the Lisfranc joint space.
The space between the bases of the first and second metatarsal
This finding is associated with an avulsion of the Lisfranc ligament
Lisfranc Injuries
Category: Critical Care
Posted: 11/23/2023 by William Teeter, MD
Click here to contact William Teeter, MD
https://pubmed.ncbi.nlm.nih.gov/37142091/
Category: Trauma
Keywords: Geriatric, older person, trauma, super-geriatric (PubMed Search)
Posted: 11/23/2023 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This retrospective study looked at trauma patients over age 65 and divided them into age ranges 65-80 (geriatric) and 80 plus (super-geriatric). They then looked at mechanusm of injury, mortality, interventions,etc. What they found was ages 65-80 were more likely to be injured in motor vehicle crashes vs. falls for those over 80. Those over 80 received less interventions including hemmorhage control surgery and had much higher levels of withdrawal of care.
This study highlights that the geriatric population is not as a monolithic group over age 65, but more nuanced by various age ranges over 65. Research going forward should be adjusted to these nuanced age ranges. Out treatment approaches should be adjusted in geriatric vs. super-geriatric patients as well.
El-Qawaqzeh K, Anand T, Alizai Q, Colosimo C, Hosseinpour H, Spencer A, Ditillo M, Magnotti LJ, Stewart C, Joseph B. Trauma in the Geriatric and the Super-Geriatric: Should They Be Treated the Same? J Surg Res. 2024 Jan;293:316-326. doi: 10.1016/j.jss.2023.09.015. Epub 2023 Oct 6. PMID: 37806217.
Category: Administration
Keywords: boarding, administration, crowding (PubMed Search)
Posted: 11/22/2023 by Mercedes Torres, MD
(Updated: 2/7/2026)
Click here to contact Mercedes Torres, MD
A recently published study of ED APPs, residents, attendings, and nurses attempted to assess clinician's perspectives on how ED boarding impacts ED staff and patients. Authors performed a survey followed by focus group sessions to obtain qualitative insignts from participants.
All respondents associated boarding with feelings of burnout and self-reported poor satisfaction with communication and the process of boarding care.
Several key themes emerged which are outlined below:
This publication highlights the negative workforce and patient safety effects of ED boarding. It amplifies the voices of our colleagues who work towards change to improve both the health of our wrokforce as well as that of our patients and the communities that we serve.
Loke D, et al. Clinicians’ Insights on Emergency Department Boarding: An Explanatory Mixed Methods Study Evaluating Patient Care and Clinician Well-Being. The Joint Commission Journal on Quality and Patient Safety 2023; 000:1-8.
Category: Pediatrics
Keywords: POCUS, Pediatrics, Lung Ultrasound, Bronchiolitis (PubMed Search)
Posted: 11/20/2023 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Acute bronchiolitis (AB) is a common cause of respiratory tract infections in infants. A recent study looked at the application of Point-of-Care Lung Ultrasound (LUS) in infants <12 months who presented with symptoms of AB.
They scored infant lungs using a cumulative 12-zone system. With the below scale:
0 - A lines with <3 B lines per lung segment.
1 - ≥3 B lines per lung segment, but not consolidated.
2 - consolidated B lines, but no subpleural consolidation.
3 - subpleural consolidation with any findings scoring 1 or 2.
They found that infants with higher LUS scores had increased rates of hospitalization and length of stay.
Here are some tips for ultrasounding a pediatric patient:
Smith JA, Stone BS, Shin J, Yen K, Reisch J, Fernandes N, Cooper MC. Association of outcomes in point-of-care lung ultrasound for bronchiolitis in the pediatric emergency department. Am J Emerg Med. 2023 Oct 21;75:22-28. doi: 10.1016/j.ajem.2023.10.019. Epub ahead of print. PMID: 37897916.
Category: Trauma
Keywords: Reverse shock index, Peds trauma, prediction (PubMed Search)
Posted: 11/18/2023 by Robert Flint, MD
Click here to contact Robert Flint, MD
This small study suggests using reverse shock index times the Glasgow Comma Scake score may give a prognostication on pediatric trauma severity and resource utilization.
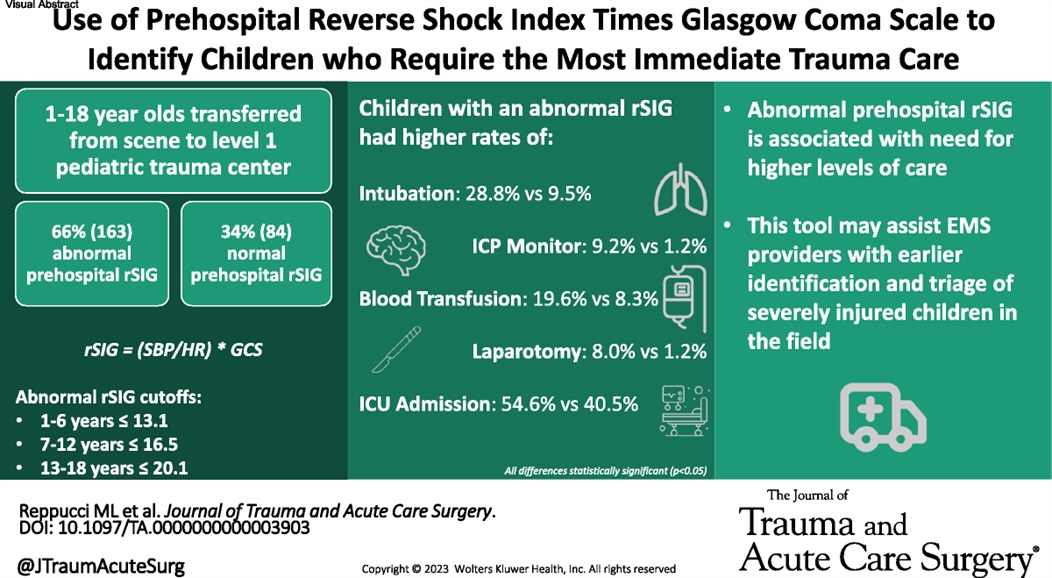
Reppucci, Marina L. MD; et al.
Journal of Trauma and Acute Care Surgery 95(3):p 347-353, September 2023. | DOI:
Category: Pediatrics
Keywords: pediatric trauma, transport, time to destination (PubMed Search)
Posted: 11/17/2023 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
Hosseinpour H. Interfacility Transfer of Pediatric Trauma to Higher Levels of Care: The Effect of Transfer Time and Level of Receiving Trauma Care. Journal of Trauma and Acute Care Surgery. Epub ahead of print.
Category: EMS
Keywords: mental health, excited delirium, agitation, sedation, ketamine (PubMed Search)
Posted: 11/15/2023 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
Bourke et al. Acute Severe Behavioral Disturbance Requiring Parenteral Sedation in Pediatric Mental Health Presentations to Emergency Medical Services: A Retrospective Chart Review. Annals of Emergency Medicine. 2023; 1-13. epub ahead of print.
Category: Trauma
Keywords: Brain injury, ketamine ICP (PubMed Search)
Posted: 11/12/2023 by Robert Flint, MD
Click here to contact Robert Flint, MD
This pediatric ICU study measured ICP during and after ketamine infusion. There was no increase in ICP associated with the ketamine infusion. This small study adds to the data that ketamine is safe in pediatric brain injured patients.
Laws, Jennifer C. MD1; Vance, E. Haley DNP2; Betters, Kristina A. MD1; Anderson, Jessica J. PharmD3; Fleishman, Sydney BA4; Bonfield, Christopher M. MD2; Wellons, John C. III MD, MSPH2,5; Xu, Meng MS6; Slaughter, James C. DrPH6; Giuse, Dario A. Dr.Ing7; Patel, Neal MD, MPH5,7; Jordan, Lori C. MD, PhD8; Wolf, Michael S. MD1,2
Category: Orthopedics
Posted: 11/11/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
https://prod-images-static.radiopaedia.org/images/626179/d58f35a8aa4a0a6750a6adce4087a4_gallery.jpg
"I was kicked in the inside of my knee while it was straight (extended). Look at the x-ray and tell me if its bad"
The arcuate sign
Avulsion fracture of the styloid of the proximal fibula. The fragment is usually small (less than 1 cm) and displaced superiorly and medially. This fracture pattern is pathognomonic for posterolateral corner (PLC) injury.
Treatment in ED is knee immobilization in full extension. Refer to orthopedics for PCL reconstruction.
Category: Critical Care
Keywords: Pneumonia, Corticosteroids, Steroids, Respiratory Failure, Infection (PubMed Search)
Posted: 11/9/2023 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
For the folks who have been in practice for a while, you may be aware of the roller-coaster evidence base looking at steroids for pneumonia. Once thought to be beneficial and clearly indicated, of late steroids for pneumonia have fallen out of favor. Hamad et al have published an excellent (and brief) review in Clinical Infectious Diseases which suggests the pendulum might be swinging back in favor of giving steroids to patients with pneumonia. It's a ~5 minute read, so I recommend glancing through it yourself, but below are my two cents (solely my opinion) on where we are with steroids for pneumonia.
Take Home Points (OPINION ALERT):
1) When you have a condition present that you consider an indication for steroids (e.g. severe COVID-19 for sure; septic shock, s. pneumo infection, and ARDS depending on how you feel about the existing literature) --> strongly consider giving steroids unless there's a contraindication
2) When you have an undifferentiated patient who MAY have one of these conditions (e.g. pneumonia with COVID pending, patient potentially in ARDS or high risk of going into ARDS, etc) who is very sick --> it is reasonable to give steroids (if no contraindication) or not give steroids. My tendency is to lean towards giving steroids in these cases, but do be aware that society guidelines recommend against steroids here (although debatable if they just haven't caught up to more recent literature)
3) When you have an undifferentiated patient who may have one of these conditions, but is NOT very sick --> I do not think there is significant enough evidence to support empiric steroids
4) Factors that might push you one way or another:
Category: Gastrointestional
Keywords: NG Tube (PubMed Search)
Posted: 11/9/2023 by Neeraja Murali, DO, MPH
Click here to contact Neeraja Murali, DO, MPH
Think before placing a nasogastric tube!
Multiple articles which discussed complications of NGT placement were included in this integrative review, with the majority (n=67) publishing results in English. The authors categorized adverse events into two broad categories:
1) Mechanical adverse events - including respiratory, esophageal, and pharyngeal complications, obstructed tube, intestinal and intracranial (!) perforation, and tube withdrawal
-The largest cohort (n=44) was respiratory, with displacement or placement of tube to the respiratory tract
2) Others - pressure injury and misconnection
-One study showed pressure related injury in 25%, and 5 articles discussed complications of misconnection (including extravasation of gastric fluids and inadvertent connection to central venous catheters)
16 of the 69 studies reported death as a consequence of improper placement.
One big takeaway: there is no universally accepted standard for verificaiton of tube placement. Xray is considered to be *most* accurate. Tubes should also be checked periodically and depth should be marked. Evidence-based guidelines need to be developed to improve patient safety, outcomes, and quality of care.
Motta APG, Rigobello MCG, Silveira RCCP, Gimenes FRE. Nasogastric/nasoenteric tube-related adverse events: an integrative review. Rev Lat Am Enfermagem. 2021 Jan 8;29:e3400. doi: 10.1590/1518-8345.3355.3400. PMID: 33439952; PMCID: PMC7798396.
