Category: Pulmonary
Keywords: pulmonary embolism, intervention, scoring, out come (PubMed Search)
Posted: 7/18/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
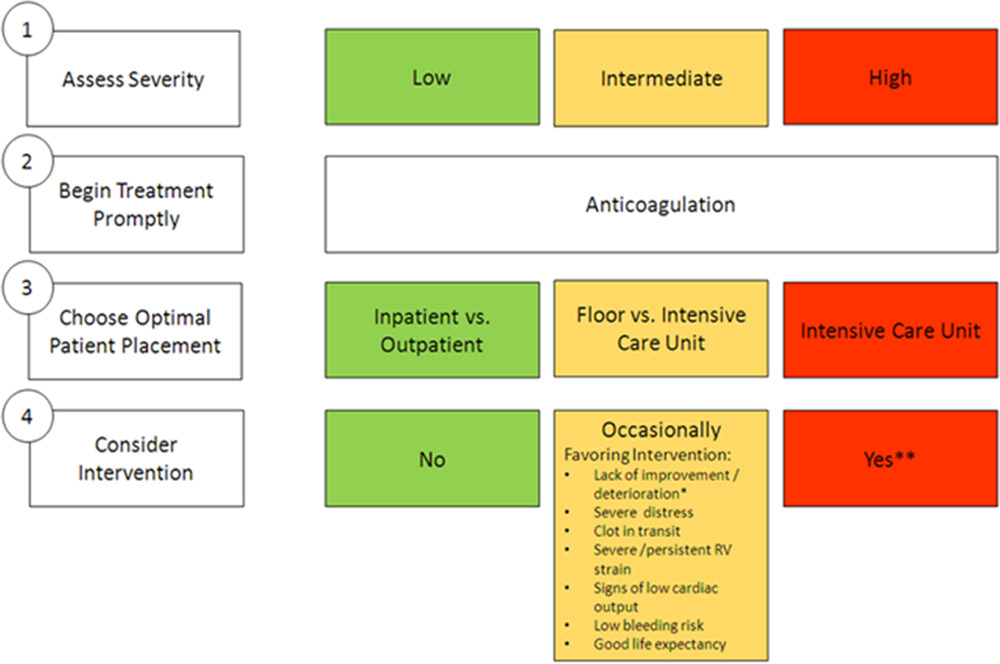
Deciding which pulmonary embolism patient needs thrombolytics/catheter based intervention is a shared decision among emergency physicians, intensivists, interventionalists, hospitalists, and the patient/family. This article provides evidence to help guide this decision. Keep in mind “The use of either CDL or catheter-based embolectomy in patients with intermediate-risk PE has, thus far, been correlated only with more rapid improvement of RV dysfunction than anticoagulation alone, not short- or long-term clinical or functional outcomes.”
"1. Massive (AHA) or high risk (ESC): Hypotension, defined as a systolic blood pressure <90 mm?Hg, a drop of >40 mm?Hg for at least 15 minutes (this latter criterion may be difficult to ascertain in some clinical circumstances), or need for vasopressor support, identifies these patients. They account for ?5% of hospitalized patients with PE and have an average mortality of ?30% within 1 month.
2.Submassive (AHA) or intermediate risk (ESC): RV strain without hypotension (see above) primarily identifies these patients. RV strain includes RV dysfunction on computed tomography pulmonary angiography or echocardiography (RV/left ventricular [LV] ratio >0.9)6,7 or RV injury and pressure overload detected by an increase in cardiac biomarkers such as troponins or brain natriuretic hormone.
3.Low risk (ESC and AHA): These patients do not meet criteria for submassive (AHA) or intermediate-risk (ESC) PE"
Interventional Therapies for Acute Pulmonary Embolism: Current Status and Principles for the Development of Novel Evidence: A Scientific Statement From the American Heart Association
Jay Giri, MD, MPH, FAHA, Chair, Akhilesh K. Sista, MD, FAHA, Vice Chair, Ido Weinberg, MD, MSc, Clive Kearon, MB, PhD, Dharam J. Kumbhani, MD, FAHA, Nimesh D. Desai, MD, PhD, Gregory Piazza, MD, MS, FAHA, Mark T. Gladwin, MD, FAHA, Saurav Chatterjee, MD, Taisei Kobayashi, MD, Christopher Kabrhel, MD, MPH, and Geoffrey D. Barnes, MD, MSc, FAHAAUTHOR INFO & AFFILIATIONS
Circulation
Category: Pulmonary
Keywords: pulmonary embolism, BOVA Sscore, intervention (PubMed Search)
Posted: 7/11/2024 by Robert Flint, MD
(Updated: 7/14/2024)
Click here to contact Robert Flint, MD
The Bova score has been validated to predict mortality and complications in hemodynamically stable patients with intermediate to high-risk pulmonary embolisms. There is some literature on using the Bova score to decide on thrombolytics/interventional therapy as well.
Scoring Criteria:
Interpretation:
Category: Pulmonary
Keywords: CAP, Pneumonia (PubMed Search)
Posted: 2/1/2020 by Ashley Martinelli
(Updated: 2/8/2026)
Click here to contact Ashley Martinelli
The new IDSA and American Thoracic Society guidelines for community acquired pneumonia were recently released. Major updates to the guidelines include but are not limited to:
1. It is not recommended to obtain sputum cultures in routine care. Consider only in patients who are intubated or empirically being treated for hospital associated pathogens such as MRSA or P. aeruginosa.
2. Blood cultures are only recommended for severe CAP managed in the hospital or those empirically being treated for MRSA or P. aeruginosa, or prior infection with those pathogens, or hospitalized and received parenteral antibiotics in the last 90 days.
3. Test for influenza during time periods when influenza is prominent (as in our current 2020 influenza outbreak).
4. Healthy patients can receive either amoxicillin 1g TID, doxycycline 100mg BID, or azithromycin 500mg followed by 250mg daily x 4 doses.
5. Patients with comorbidities such as chronic heart, lung, liver, or renal disease, diabetes, alcoholism, malignancy, or asplenia should receive combination therapy with a beta-lactam (amoxicillin/clavulanate, cefdinir, or cefpodoxime) + azithromycin or doxycycline. If allergies preclude the use of a beta-lactam, a fluoroquinolone (levofloxacin or moxifloxacin) can be used.
6. Patient admitted for non-severe CAP can receive combination beta-lactam (ampicillin/sulbactam, or ceftriaxone) and azithromycin therapy. Patients with severe beta-lactam allergies can receive either levofloxacin or moxifloxacin).
7. It is no longer recommended to add anaerobic coverage for suspected aspiration pneumonia unless the patient is suspected to have a lung abscess or empyema. It is most likely a chemical pneumonitis and should resolve within 24-48 hours with supportive therapy.
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Resp Crit Care. 2019;200(7):e45-e67.
