Category: Toxicology
Keywords: Ketamine, Benzodiazepines (PubMed Search)
Posted: 4/7/2016 by Kathy Prybys, MD
(Updated: 4/8/2016)
Click here to contact Kathy Prybys, MD
[CORRECTION]: Versed dose is 2-2.5 mg total not mg/kg
Patients with severe agitation present a unique challenge to the emergency department. Acute delirium is often due to psychostimulants such as cocaine, amphetamines, PCP, or synthetic cannabinoids, alcohol, or psychiatric illness. These patients require urgent evaluation necesssitating the use of physical and chemical restraints, not only for their own safety but also the hospital staff's. Fingerstick glucose, pulse oximetry, and vital signs must be expeditiously obtained. Severely agitated combative patients who are physically restrained are at high risk for morbidity from asphyxiation, hypermetabolic consequences (acidosis, hyperthermia, rhabdomyolysis), and death can occur.
Ketamine is phencyclidine derivative that causes dissociative state between the cortical and limbic systems which prevents the higher centers from preceiving visual, auditory, or painful stimuli. Ketamine has a wide safety profile and has been used worldwide for many years with few complications. It possesses ideal characteristics for rapid sedation of agitated patients:
Experience with Ketamine in patients with excited delirium has shown good initial control of agitation however, patients often require additional medications for deeper or longer duration of sedation. Benzodiazepines are recommmended as second line agents particularly intravenous or intramuscular Midazolam 2-2.5 mg /kg.
Scheppke KA, Braghiroli J, Shalaby M, Chait R. Prehospital Use of IM Ketamine for Sedation of Violent and Agitated Patients. Western Journal of Emergency Medicine. 2014;15(7):736-741.
Isbister GK, Calver LA, et al. Ketamineas RescueTreatment for Difficult-to-Sedate Severe Acute Behavioral Disturbance in the Emergency Department. Ann Emerg Med 2016 Feb 10 [Epub ahead of print].
Category: International EM
Keywords: Mortality, injuries (PubMed Search)
Posted: 4/6/2016 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
As noted previously, injuries cause substantial morbidity and mortality globally. How does it vary by age group?
The following table shows that unintentional injuries are the leading cause of death for individuals 1-44 years of age. Even when they are not the leading cause of death, injuries cause substantial mortality in all age groups.
http://www.cdc.gov/injury/images/lc-charts/leading_causes_of_death_age_group_2014_1050w760h.gif
Category: Critical Care
Posted: 4/5/2016 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Follow me on Twitter (@criticalcarenow)
Category: Pharmacology & Therapeutics
Keywords: vancomycin, loading dose, nephrotoxicity (PubMed Search)
Posted: 3/24/2016 by Bryan Hayes, PharmD
(Updated: 4/2/2016)
Click here to contact Bryan Hayes, PharmD
Guidelines recommend loading doses of vancomycin (15-20 mg/kg, up to 30 mg/kg in critically ill patients), but the risk of nephrotoxicity is unknown. A new retrospective cohort study aimed to compare nephrotoxicity in ED sepsis patients who received vancomycin at high doses (>20 mg/kg) versus lower doses (20 mg/kg).
What They Found
1,330 patients had three SCr values assessed for the primary outcome
High-dose initial vancomycin was actually associated with a lower rate of nephrotoxicity (5.8% vs 11.1%)
After adjusting for age, gender, and initial SCr, the risk of high dose vancomycin compared to low dose was decreased for the development of nephrotoxicity (RR=0.60; 95% CI: 0.44, 0.82)
Application to Clinical Practice
It appears initial loading doses of vancomcyin > 20 mg/kg do not cause increased risk of nephrotoxicity.
Rosini JM, et al. High single-dose vancomycin loading is not associated with increased nephrotoxicity in emergency department sepsis patients. Acad Emerg Med. 2016 Feb 6. Epub ahead of print. [PMID 26850378]
Follow me on Twitter (@PharmERToxGuy)
Category: International EM
Keywords: Match, training, emergency medicine, residency (PubMed Search)
Posted: 3/26/2016 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 4/6/2016)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Emergency medicine remains a relatively young and developing specialty in most parts of the world. However, it is growing in popularity, especially in the U.S. How competitive is it currently?
For the recent 2016 Match, there were 2476 applicants for 1895 categorical emergency medicine positions from 174 programs.
Bottom Line: Emergency medicine remains a highly desired and competitive specialty in the U.S.
Congratulations to all the incoming interns for the 2016-2017 year!
Category: Critical Care
Keywords: cardiorenal syndrome, heart failure, kidney failure (PubMed Search)
Posted: 3/29/2016 by Feras Khan, MD
Click here to contact Feras Khan, MD
What is cardio-renal syndrome CRS?
There are 5 types
1. Acute CRS: abrupt worsening of heart function leading to kidney injury
2. Chronic CRS: chronic heart failure leads to progressive kidney disease
3. Acute renocardiac syndrome: abrupt kidney dysfunction leading to acute cardiac disorder
4. Chronic renocardiac syndrome: chronic kidney disease leading to decreased cardiac function
5. Systemic CRS: Systemic condition leading to both heart and kidney disease
Category: Orthopedics
Keywords: Metacarpal Fractures (PubMed Search)
Posted: 3/26/2016 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Metacarpal Fractures
* Localize fracture to head, neck or shaft (neck most common)
5th metacarpal most commonly fractured
* Note amount of angulation, shortening and the presence of malrotation
*Treatment is based on which metacarpal is fractured and the location of the fracture
*The amount of acceptable angulation varies by the digit involved
For example for index and long finger - acceptable angulation of the shaft is 10-20 degrees and neck is 10 to 15 degrees
Whereas for the 5th digit - acceptable angulation for the shaft is 40 degrees and neck is 50 degrees
Pearls
No degree of malrotation is acceptable (document the absence of this!)
Strongly suspect fight bite injury with abrasions/lacerations overlying metacarpal heads
Highly prone to infection given the proximity to the joint capsule
Consider lacerations over metacarpal fractures as open fractures (do not close/discuss management with hand surgery re timing of washout. Many prefer delayed fixation for suspected infections )
Document integrity of the extensor tendon (can be lacerated and retracted)
Category: Neurology
Keywords: geriatrics, seizures, mimics, TIA, syncope (PubMed Search)
Posted: 3/23/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Carlson C, Anderson CT. Special Issues in Epilepsy: The Elderly, the Immunocompromised, and Bone Health. Continuum 2016;22(1):246 261
Category: Critical Care
Posted: 3/22/2016 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Cerebral Venous Thrombosis
Fam D, Saposnik G. Critical care management of cerebral venous thrombosis. Curr Opin Crit Care 2016; 22:113-9.
Category: Orthopedics
Keywords: osteoarthritis, nsaids (PubMed Search)
Posted: 3/20/2016 by Michael Bond, MD
(Updated: 2/7/2026)
Click here to contact Michael Bond, MD
A meta-analysis of 74 randomized trials with a total of 58,556 patients was recently published in the Lancet that looked at the effectiveness of NSAIDs in the treatment of osteoarthritis (OA) pain.
Briefly, their conclusion was that:
You can find the article here http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2816%2930002-2/abstract
Category: Pediatrics
Keywords: End tidal capnography, diabetic ketoacidosis (PubMed Search)
Posted: 3/19/2016 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
A previous pearl has looked at serum HCO3 as a predictor of DKA (see pearl from 8/21/15). The article by Gilhotra looks at using end tidal CO2 (ETCO2) to exclude DKA. 58 pediatric patients were enrolled with 15 being in DKA. No patient with ETCO2 > 30 mmHg had DKA. Six patients with ETCO2 < 30 mmHg did not have DKA. Other studies done in children have shown similar results.
An article recently published by Chebl and colleagues examined patients older than 17 years with hyperglycemia. In this study, 71 patients were included with 32 having DKA. A ETCO2 >35 excluded DKA in this group while a level <22 was 100% specific for DKA.
Bottom line: ETCO2 >35 mmHg is a quick bedside test that can aid in the evaluation of hyperglycemic patients.
Gilhotra Y and Porter P. Predicting diabetic ketoacidosis in children by measuring end-tidal CO2 by non-invasive nasal capnography. J Paediatr Child Health 2007; 43 (10): 677-80.
Chebl BR, Madden B, Belsky J, Harmouche E, Yessayan L. Diagnostic value of end tidal capnography in patients with hyperglycemia in the emergency department. BCM Emerg Med 2016: 16 (1).
Category: Infectious Disease
Keywords: Rash, Cutaneous larva migrans, nematode, tropics (PubMed Search)
Posted: 3/16/2016 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Cutaneous larva migrans (CLM) is an acquired dermatosis
Clinical manifestations:
Treatment:
Bottom Line:
http://emedicine.medscape.com/article/1108784-clinical
http://www.cdc.gov/parasites/zoonotichookworm/gen_info/faqs.html
https://cid.oxfordjournals.org/content/30/5/811.full
Category: Critical Care
Keywords: Pharmacology, Hypertension, Vasoactive (PubMed Search)
Posted: 3/15/2016 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
There are multiple vasoactive infusions available for acute hypertensive emergencies, many having serious side effect profiles or therapeutic disadvantages.
Clevidipine (Cleviprex) is rapidly-titratable, lipid-soluable dihydropyridine calcium channel blocker which has become increasingly used in the ICU in recent years [1]:
ECLIPSE trial compares clevidipine, nicardipine, nitroglycerin and nitroprusside in cardiac surgery patients. .
Clevidipine was as effective as nicardipine at maintaining a pre-specified BP range, but superior when that BP range was narrowed (also studied in ESCAPE-1 and ESCAPE2 with similar results) [2-3]
TAKE-HOME: Clevidipine is an ultra short-acting, rapidly-titratable vasoactive with favorable cost, pharmacokinetics, and side-effect profile. Consider its use in hypertensive emergencies.
1. Lexicomp (accessed via UpToDate on 3/15/2016)
2. Aronson S, Dyke CM, Stierer KA, et al, "The ECLIPSE Trials: Comparative Studies of Clevidipine to Nitroglycerin, Sodium Nitroprusside, and Nicardipine for Acute Hypertension Treatment in Cardiac Surgery Patients," Anesth Analg, 2008, 107(4):1110-21.
3. ESCAPE-2 Study Group.Treatment of acute postoperative hypertension in cardiac surgery patients: an efficacy study of clevidipine assessing its postoperative antihypertensive effect in cardiac surgery-2 (ESCAPE-2), a randomized, double-blind, placebo-controlled trial.Anesth Analg. 2008 Jul;107(1):59-67.
Category: Orthopedics
Keywords: X-ray, Hip pain (PubMed Search)
Posted: 3/12/2016 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Femoral neck fracture
We typically think of the presentation of the displaced fracture severe pain, writhing in the bed, unable to ambulate, limited ROM
* However, patients with nondisplaced fractures (15 20%) may walk with a limp
* Occurs primarily in the elderly & osteoporotic population after a fall directly onto the hip
* Look for a cortical step-off in the femoral neck (w/ foreshortening)
* A patient with a minimally displaced fracture may only complain of hip, knee, or groin pain and may be able to walk (albeit with a limp)
* Almost 9% of hip fractures are radiographically normal (Nondisplaced or impacted fractures)
* Fractures which were initially nondisplaced, may become displaced upon re-presentation
* Remember the limitations of plain x-ray in the evaluation of femoral neck fractures!
* Because of the significant complication of overlooking a femoral neck fracture, MRI has become the recommended imaging modality of choice for a patient with a high suspicion for a femoral neck fracture, despite normal plain radiographs of the hip
Category: Toxicology
Keywords: cocaine, toxicity, cardiovascular (PubMed Search)
Posted: 3/9/2016 by Bryan Hayes, PharmD
(Updated: 3/12/2016)
Click here to contact Bryan Hayes, PharmD
Acute cocaine toxicity can manifest with several cardiovascular issues such as tachycardia, dysrhythmia, hypertension, and coronary vasospasm. A new systematic review collated all of the available evidence for potential treatment options. Here is what the review found (there is also an 'other agents' section for medications with less published reports):
Benzodiazepines and other GABA-active agents: Benzodiazepines may not always effectively mitigate tachycardia, hypertension, and vasospasm from cocaine toxicity.
Calcium channel blockers: Calcium channel blockers may decrease hypertension and coronary vasospasm, but not necessarily tachycardia.
Nitric oxide-mediated vasodilators: Nitroglycerin may lead to severe hypotension and reflex tachycardia.
Alpha-adrenoceptor blocking drugs: Alpha-1 blockers may improve hypertension and vasospasm, but not tachycardia, although evidence is limited.
Alpha-2-adrenoceptor agonists: There were two high-quality studies and one case report detailing the successful use of dexmedetomidine.
Beta-blockers and alpha/beta-blockers: No adverse events were reported for use of combined alpha/beta-blockers such as labetalol and carvedilol, which were effective in attenuating both hypertension and tachycardia.
Antipsychotics: Antipsychotics may improve agitation and psychosis, but with inconsistent reduction in tachycardia and hypertension and risk of extrapyramidal adverse effects.
Sodium bicarbonate: Twelve case reports documented treatment of dysrhythmia with IV sodium bicarbonate, with seven reporting successful termination.
The authors note that "publication bias is a concern, and it is possible that successful treatment and/or adverse events have not been reported in some of the publications, and in general."
Richard JR, et al. Treatment of cocaine cardiovascular toxicity: a systematic review. Clin Toxicol. 2016 Feb 26:1-20. [Epub ahead of print] [PMID 26919414]
Follow me on Twitter (@PharmERToxGuy)
Category: Neurology
Keywords: Up-gaze paresis, ophthalmoparesis, hydrocephalus, shunt malfunction (PubMed Search)
Posted: 3/9/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Sunset Eye Sign
Category: Critical Care
Posted: 3/8/2016 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Follow me on Twitter (@criticalcarenow)
Category: Pharmacology & Therapeutics
Keywords: status epilepticus (PubMed Search)
Posted: 3/3/2016 by Bryan Hayes, PharmD
(Updated: 3/5/2016)
Click here to contact Bryan Hayes, PharmD
A new guideline for convulsive status epilepticus in adults AND children was recently published. [1] An insightful commentary was published alongside it (both are open access). [2] The proposed algorithm is below. Here are a few additional points to note:
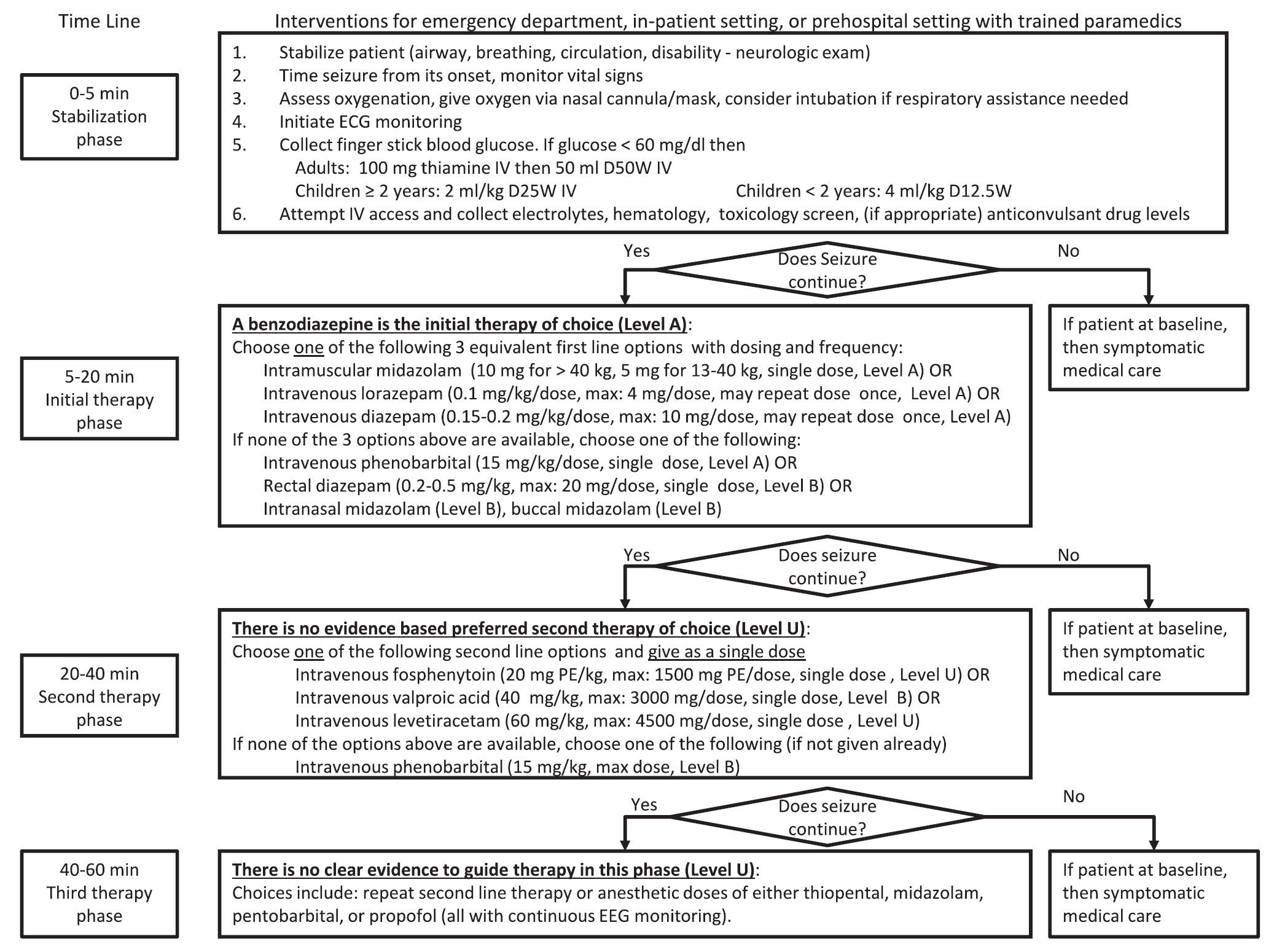
Follow me on Twitter (@PharmERToxGuy)
Category: Toxicology
Keywords: Fentanyl, W-18, Clandestine (PubMed Search)
Posted: 3/4/2016 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
Pure opioid agonists such as Morphine, Hydromorphone, and Fentanyl stimulate opioid receptors and are the most potent analgesics. Fentanyl and fentanyl analogues are up to 100 times more powerful than morphine and 30-50 times more powerful than heroin.
W-18 is a highly potent opioid agonist with a distinctive chemical structure which is not closely related to older established families of opioid drugs. While Fentanyl is approximately 100 times more powerful than Morphine, W-18 is about 100 times more powerful than Fentanyl.
Increases in Drug and OpioidOerdose Deaths-United States. 2000-2014. Rudd RA, et al. MMWR Morb Mortal Wkly Rep. 2016 Jan 1;64(50-51):1378-82.
Increases in fentanyl drug confiscations and fentanyl-related overdose fatalities. CDC. HAN Health Advisory. Atlanta, GA: US Department of Health and Human Services, CDC; 2015.
W-18, a synthetic opiate 100 times more potent than fentanyl. The Poison Review February 2016
Category: International EM
Keywords: Infectious diseases, influenza (PubMed Search)
Posted: 3/2/2016 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
While the flu season this year has been mild, it is still important to recognize which patients are at high risk for flu-related complications:
During the influenza season, when admitting a patient who 1) has respiratory symptoms and 2) is at high risk for influenza complications, consider testing them for influenza.
http://www.cdc.gov/flu/about/disease/high_risk.htm
