Category: Visual Diagnosis
Keywords: C Spine, osteomyelitis, (PubMed Search)
Posted: 5/25/2023 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD


Neck pain and trouble swalowing. No trauma.
Osteomyelitis of the cervical spine is the least common location to find spinal infection. “Osteomyelitis of the cervical spine is a rare disease, representing only 3% – 6% of all cases of vertebral osteomyelitis. In contrast with other locations of spinal infections, osteomyelitis of the cervical spine can be a much more dramatic and rapidly deteriorating process, leading to early neurologic deficit”.
Note the bony destruction as well as the abscess labeled on the lateral view.
Category: Visual Diagnosis
Posted: 5/11/2022 by Michael Bond, MD
Click here to contact Michael Bond, MD
Small Bowel Obstruction
For more information on how to perform these exams and research data take a look at coreultrasound.com, thepocusatlas.com and ultrasoundgel.org.
Category: Visual Diagnosis
Posted: 5/11/2022 by Michael Bond, MD
Click here to contact Michael Bond, MD
Aortic Dissection
Ultrasound has a great specificity for aortic dissection. Remember to take a look at your aorta on all cardiac views.
Let’s give a shout out to Nikki Cali for diagnosing aortic dissection in a patient with a recent PE. Can you find the dissection flap in this image?
For more information on how to perform these exams and research data take a look at coreultrasound.com, thepocusatlas.com and ultrasoundgel.org.
Category: Visual Diagnosis
Posted: 5/11/2022 by Michael Bond, MD
Click here to contact Michael Bond, MD
Peritonsillar Abscess
For more information on how to perform these exams and research data take a look at coreultrasound.com, thepocusatlas.com and ultrasoundgel.org.
Category: Visual Diagnosis
Posted: 5/11/2022 by Michael Bond, MD
(Updated: 2/7/2026)
Click here to contact Michael Bond, MD
Appendicitis
Ultrasound has a reported high specificity (97.9) for acute appendicitis in moderate to high pre-test probability of patients.
Let’s give a shout out to Reed Macy, who diagnosed appendicitis in a male with vomiting and abdominal pain!
Category: Visual Diagnosis
Posted: 2/12/2022 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
23 y/o otherwise healthy Male presents for approx. 3 month history of Right leg mass. It is painful with activity (deep and sharp) but not enlarging. Patient remembers a fall from a bicycle 6 months ago, with negative imaging for fracture.
What is the diagnosis?
https://plinthsandplatforms.files.wordpress.com/2016/06/screen-shot-2016-06-20-at-10-58-18-am.png
https://radsource.us/wp-content/uploads/2019/02/1E.jpg
Myositis Ossificans
Category: Visual Diagnosis
Posted: 11/26/2019 by Tu Carol Nguyen, DO
Click here to contact Tu Carol Nguyen, DO
A ~55 year-old female with a history of ESRD and diabetes who presented to the ED with progressively worsening foot odor. An x-ray was performed. The picture below shows the right foot.
What is the diagnosis?

Necrotizing infection of the foot
https://radiopaedia.org/articles/necrotising-fasciitis
Yaghoubian et al. Use of admission serum lactate and sodium levels to predict mortality in necrotizing soft-tissue infections. Archives of surgery. 2007.
Anaya DA and Dellinger EP. Necrotizing soft-tissue infection: diagnosis and management. Clinical infectious diseases. 2007.
Category: Visual Diagnosis
Keywords: Green urine, diuretic (PubMed Search)
Posted: 2/17/2018 by Michael Bond, MD
(Updated: 2/7/2026)
Click here to contact Michael Bond, MD
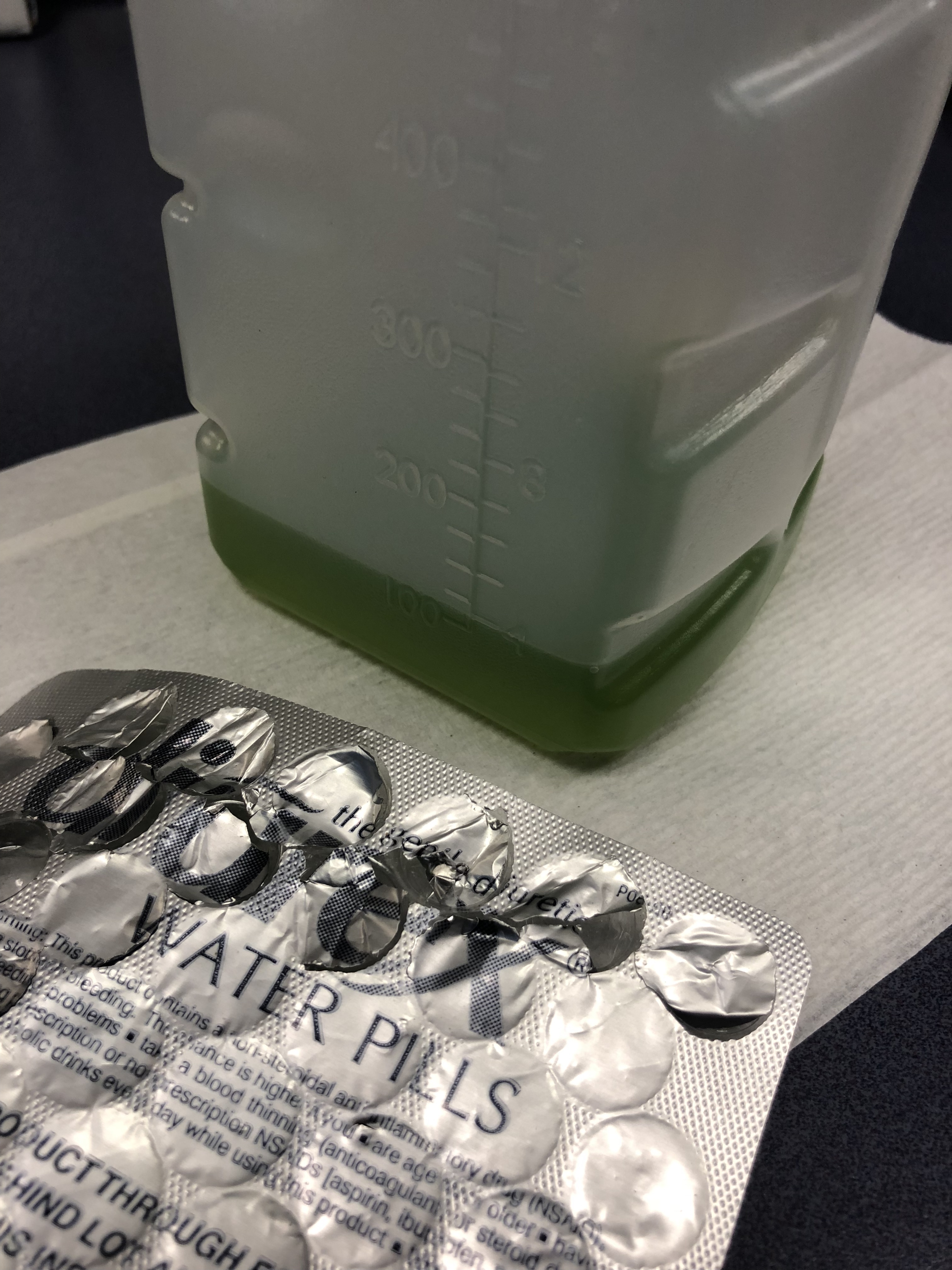
75 y/o M is brought in by EMS after he fell off the light rail and hit his head. In the ED he is A&Ox3, and is asking for a urinal. Two minutes later the tech comes running to show you the following:
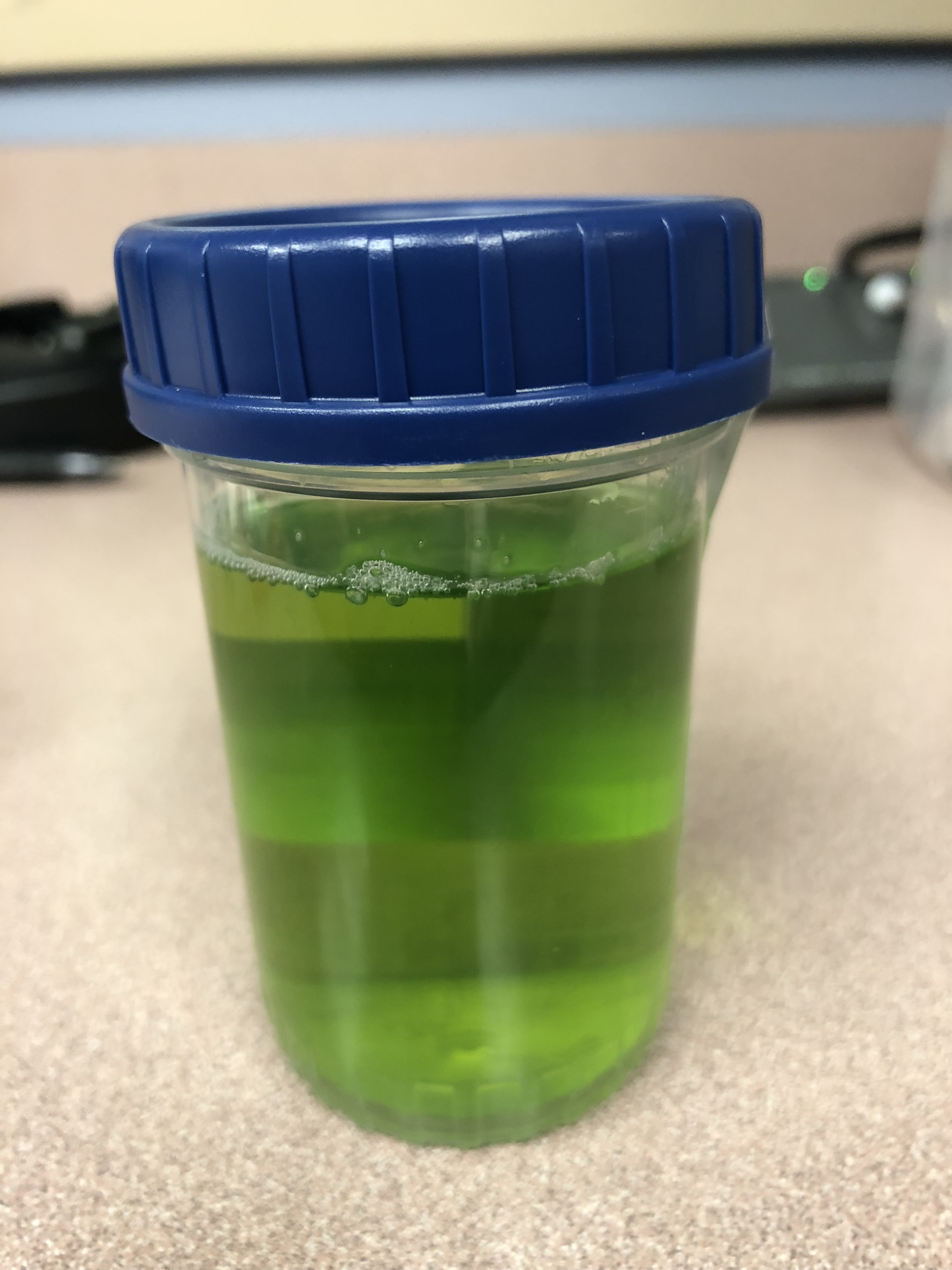
What is the cause of this patients Jolly Rancher Green Apple looking urine sample?
Answer:
Pamabrom side effect. Patient admitted to taking an “over the counter diuretic” called Diurex. The generic name is pamabrom. Pamabrom is a xanthine diuretic with only modest diuretic effect. It is marked mostly for weight loss to lose “water weight” and for relief of bloating during menstruation. A common side effect of the pills is a blue, green or golden discoloration of the urine. The capsules do not have the same side effect. The side effect is otherwise harmless and will disappear after stopping the diurex.
Category: Visual Diagnosis
Keywords: Pleural effusion; POCUS (PubMed Search)
Posted: 4/17/2017 by Tu Carol Nguyen, DO
Click here to contact Tu Carol Nguyen, DO
A 50 years old male with a history of CHF, presenting to the ED with progressively worsening shortness of breath. POCUS was performed. The picture shows the left lower part of the chest. What is the diagnosis?
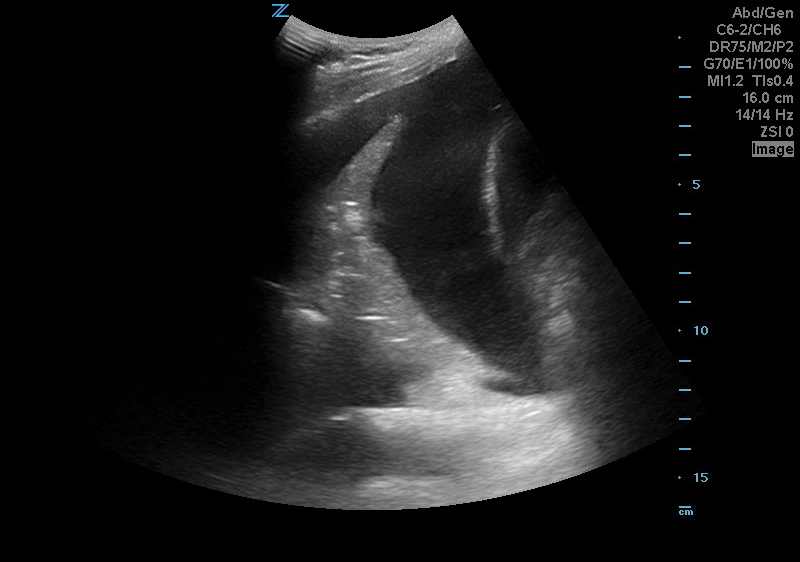
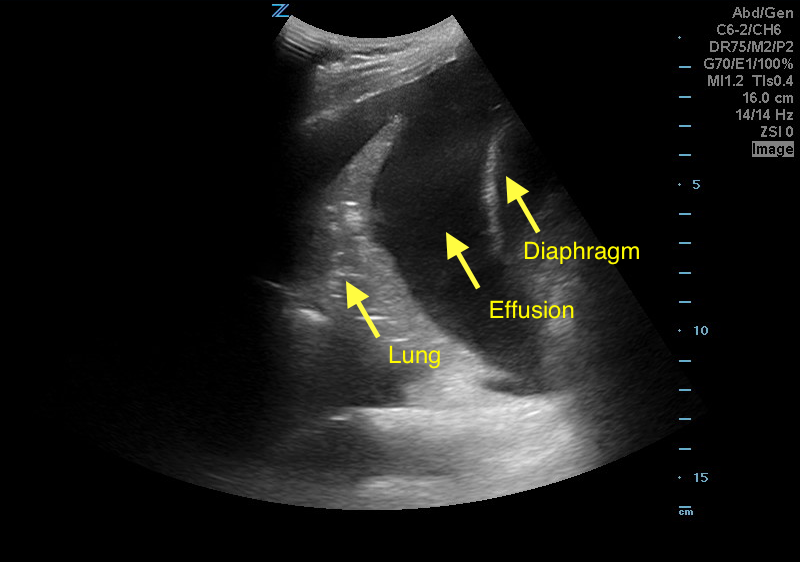
Answer: Pleural effusion
Eibenberger, K. L., Dock, W. I., Ammann, M. E., Dorffner, R., Hörmann, M. F., & Grabenwöger, F. (1994). Quantification of pleural effusions: sonography versus radiography. Radiology, 191(3), 681-684.
Atkinson, P., Milne, J., Loubani, O., & Verheul, G. (2012). The V-line: a sonographic aid for the confirmation of pleural fluid. Critical ultrasound journal, 4(1), 19.
Category: Visual Diagnosis
Posted: 2/13/2017 by Tu Carol Nguyen, DO
Click here to contact Tu Carol Nguyen, DO
56 year-old male with history of hypertension presents with complaints of right scrotal swelling and pain. Denies any urinary symptoms, abdominal pain, nausea/vomiting or change in bowel habits or prior episodes. Temp was 99.0.
A scrotal ultrasound was done and an image of the right testis was seen (below). What's the diagnosis?
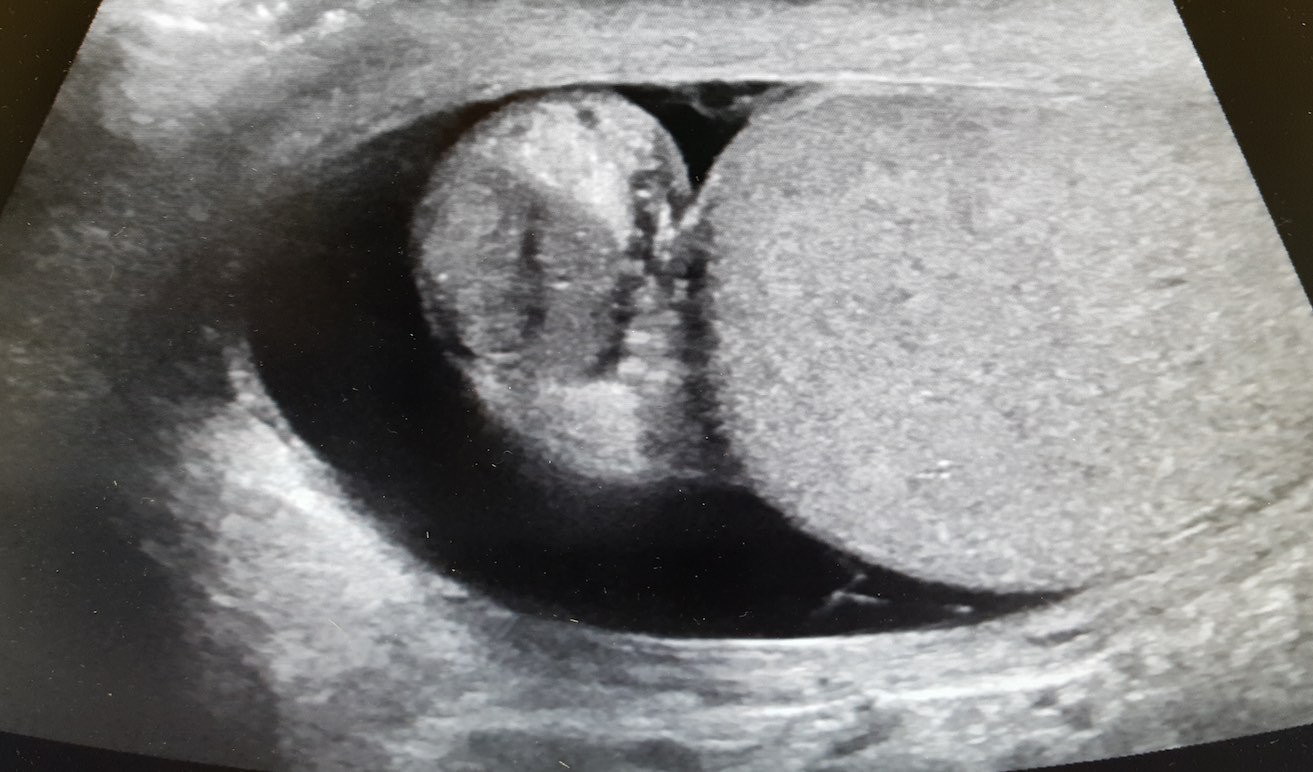
Answer: Right Epididymitis (and Hydrocele)
Take Home Points:
Kühn AL, Scortegagna E, Nowitzki KM, Kim YH. Ultrasonography of the scrotum in adults. Ultrasonography. 2016;35(3):180-97.
Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2015. MMWR Recomm Rep 2015;64(No. RR-3): 1-137.
Category: Visual Diagnosis
Keywords: Herpes Zoster Ophthalmicus; Hutchinson's sign (PubMed Search)
Posted: 2/6/2017 by Hussain Alhashem, MBBS
(Updated: 2/7/2026)
Click here to contact Hussain Alhashem, MBBS
24-year-old male with a history of Wagner's Granulomatosis, currently on Cellcept (Mycophenolate Mofetil) and high dose prednisolone, presented with two days of sore throat, malaise and the lesions shown in the picture. What is the diagnosis?


Answer: Herpes Zoster with Hutchinson's sign.
- This patient is presenting with a well demarcated eruptive skin lesion involving the tip of the nose and half of the lip and palate. This lesion is suggestive of Herpes Zoster with Hutchinson's sign.
- Hutchinson's sign is associated with a high rate of corneal denervation and ocular involvement. Some studies suggest that up to 100% of patients with Hutchinson's sign will present with a serious intraocular pathology.
- In addition to starting systemic antiviral therapy, all patients who present with Hutchinson's sign need an immediate and complete ophthalmologic evaluation including a complete slit lamp examination.
Adam, R. S., Vale, N., Bona, M. D., Hasanee, K., & Farrokhyar, F. (2010). Triaging herpes zoster ophthalmicus patients in the emergency department: do all patients require referral?. Academic Emergency Medicine, 17(11), 1183-1188.
Van Dyk, M., & Meyer, D. (2010). Hutchinson's sign as a marker of ocular involvement in HIV-positive patients with herpes zoster ophthalmicus. SAMJ: South African Medical Journal, 100(3), 172-174.
Category: Visual Diagnosis
Posted: 1/30/2017 by Tu Carol Nguyen, DO
Click here to contact Tu Carol Nguyen, DO
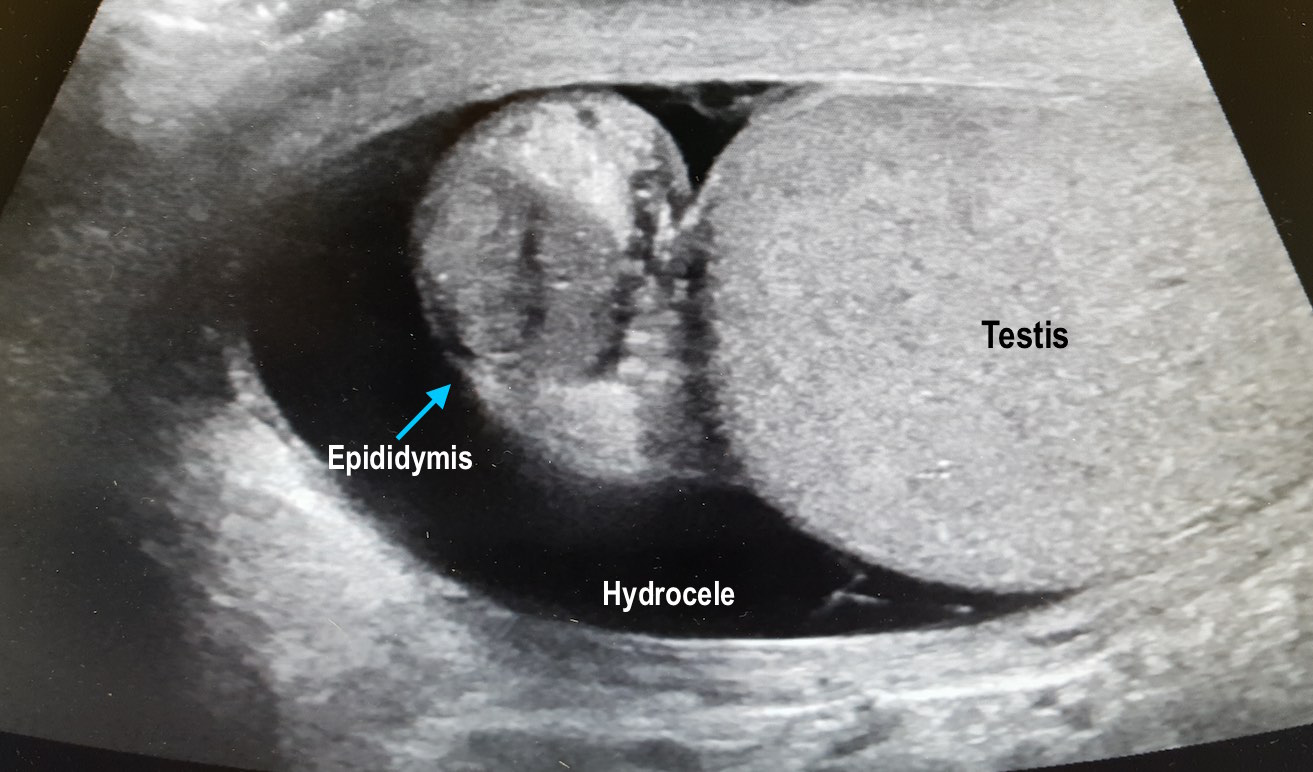
25 year-old female with hx of cerebral palsy with significant developmental delay, s/p G-tube who presented with acute hypoxic respiratory failure, hypotension and a distended, tense abdomen. A CT was done with the scout film below. What's the diagnosis?
Answer: Cecal Volvulus
Patient was subsequently intubated, had an NG tube placed with over 500cc of fluid returned. Patient had multiorgan failure and received fluids, antibiotics, pressors, blood products and went to the OR, and had a partial bowel resection.
One way to differentiate cecal volvulus from sigmoid volvulus is that sigmoid volvulus generally do not have haustra.
Tonerini M, Pancrazi F, Lorenzi S, Pacciardi F, Ruschi F, et al. (2015) Cecal volvulus: what the radiologist needs to know. Glob Surg, 1: DOI: 10.15761/GOS.1000106.
Category: Visual Diagnosis
Posted: 1/9/2017 by Tu Carol Nguyen, DO
Click here to contact Tu Carol Nguyen, DO
A 60 year-old man with history of atrial fibrillation, CAD presents with left lower leg/foot pain for a few days. His foot is seen below. What's the diagnosis?


Mottling with concerns for Acute Limb Ischemia
Key Points:
Creager MA, Kaufman JA, Conte MS. Clinical practice. Acute limb ischemia. N Engl J Med. 2012;366(23):2198-206.
http://www.emdocs.net/acute-limb-ischemia-pearls-pitfalls/
Category: Visual Diagnosis
Posted: 1/2/2017 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
A 36-year-old male, who recently immigrated from Africa, presented to the ED with fever, rash, cough and shortness of breath. He was noted to be febrile to 39.0 C. The rash is disseminated but present mainly in his trunk as shown in the picture.

Disseminated Varicella Zoster Virus (VZV) Infection
- The patient is presenting with a rash in different stages, associated with fever and signs of systematic involvement, indicating a disseminated varicella infection.
- Definitive diagnosis of disseminated VZV infection is made by detecting its DNA in multiple anatomic sites.
- The most common complication of VZV infection in immunocompetent adults is VZV pneumonia. Early detection of VZV pneumonia can be done with bronchoalveolar lavage and PCR testing.
- Treatment is with IV acyclovir and is more effective if started within 24 hours of the beginning of symptoms. In cases that require prolonged treatment, gene sequencing should be done to detect resistant strains.
Beby?Defaux, Agnès, et al. "Disseminated varicella with multiorgan failure in an immunocompetent adult." Journal of medical virology 81.4 (2009): 747-749.
Category: Visual Diagnosis
Posted: 12/27/2016 by Tu Carol Nguyen, DO
Click here to contact Tu Carol Nguyen, DO
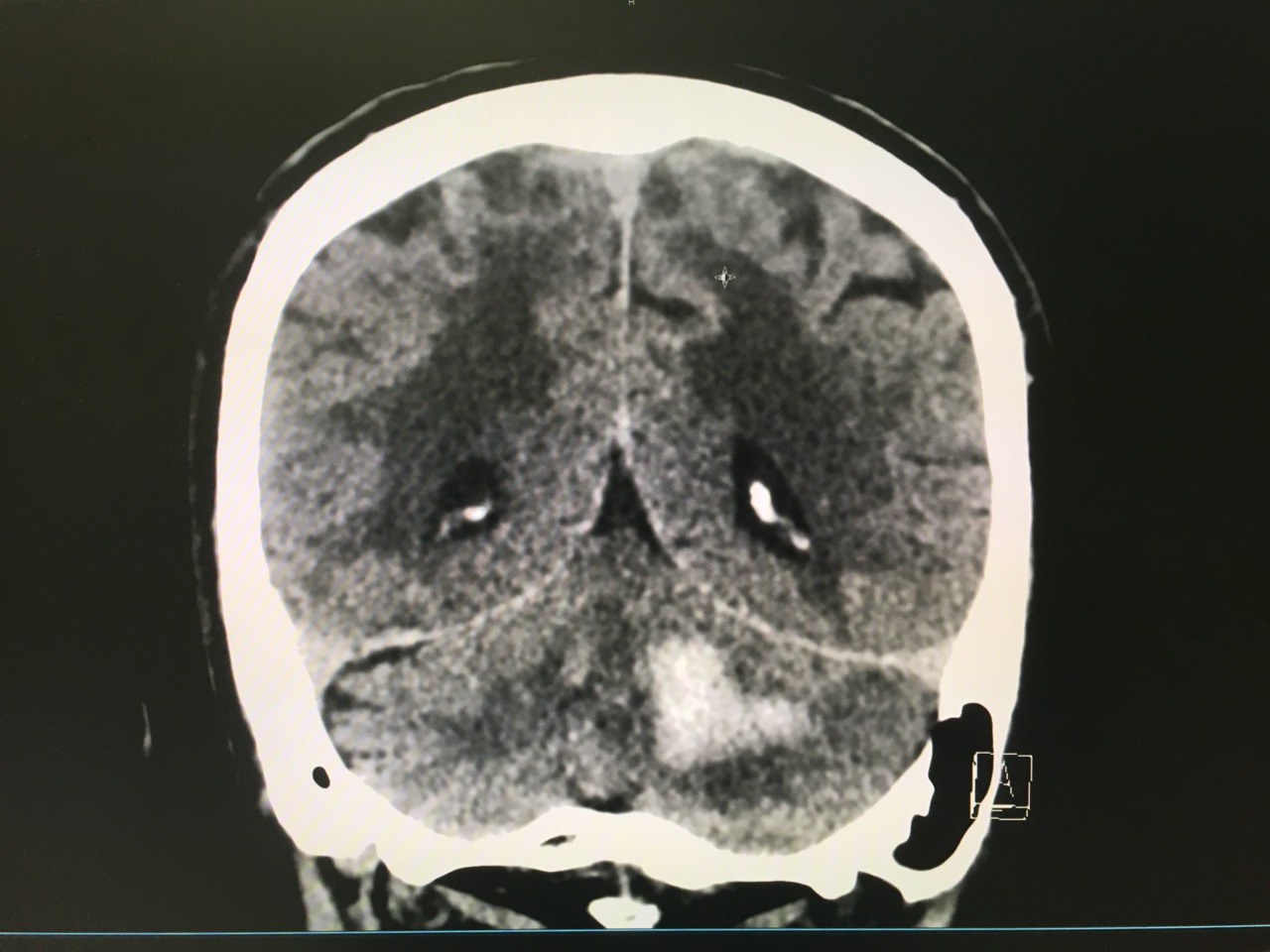
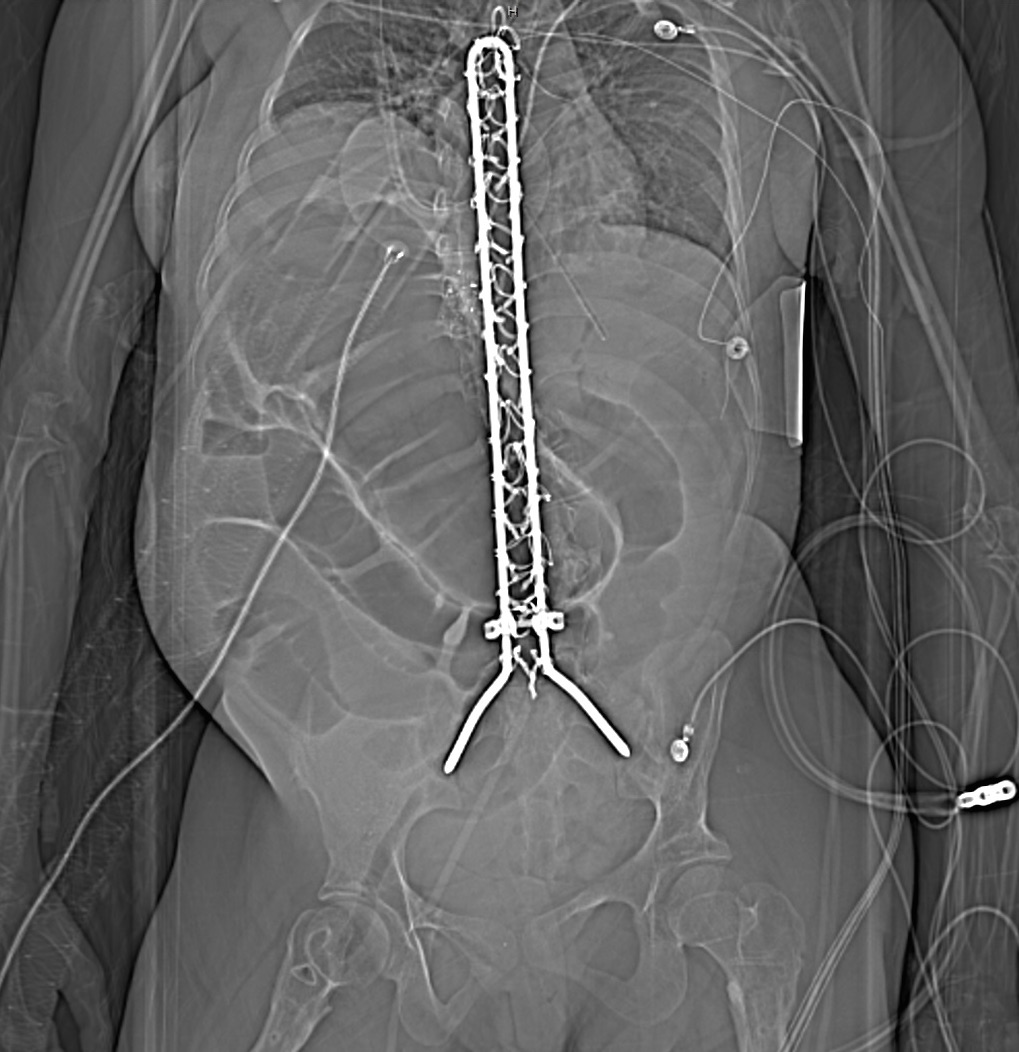
Answer: Large left cerebellar intraparenchymal hemorrhage with surrounding vasogenic edema with mild infratentorial midline shift of ~4mm
Take Home Points:
Hemphill JC, Greenberg SM, Anderson CS, et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015;46(7):2032-60.
Category: Visual Diagnosis
Posted: 12/12/2016 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
30 Year-old female presents to the ED for a rash. The rash started suddenly, mainly in her extremities and it is painful. The patient denied having fever or chills. Her past medical history is unremarkable. She admits to using cocaine frequently. The rash is shown in the picture.

Levamisole-Induced Vasculitis
- Levamisole is an antihelmintic drug that was banned by the US Food and Drug Administration in 2000 because of its adverse effects.
- It is added to cocaine to increase its weight and potentiate its effect.
- Patients usually present with painful purpuric rash without central necrosis.
- Laboratory values might include agranulocytosis and elevated ESR.
- Treatment is by cessation of cocaine use.
- Because Levamisole is strongly associated with agranulocytosis, corticosteroids should be avoided to prevent immunosuppression.
Roberts, Jordan A., and Patricia Chévez-Barrios. "Levamisole-induced vasculitis: a characteristic cutaneous vasculitis associated with levamisole-adulterated cocaine." Archives of pathology & laboratory medicine 139.8 (2015): 1058-1061.
Category: Visual Diagnosis
Posted: 12/5/2016 by Tu Carol Nguyen, DO
Click here to contact Tu Carol Nguyen, DO
27 year-old G2P1 presents with 3 days of abdominal pain that is mostly suprapubic. Denies any urinary symptoms and vaginal bleeding. Physical examination reveals slight rebound in the right lower quadrant.
An ultrasound revealed the following. What's the diagnosis?

Pregnancy with Appendicitis
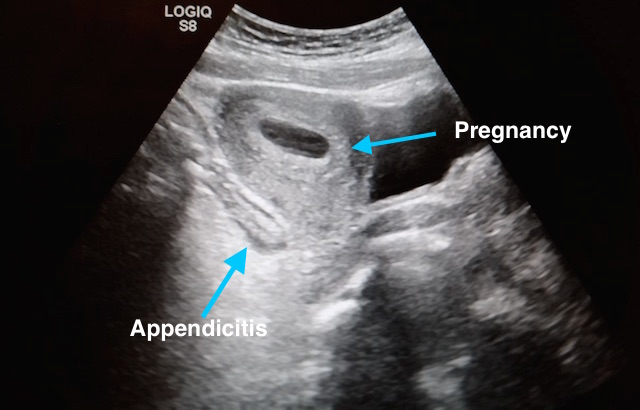
Take Home Points:
See previous pearl for how to conduct an ultrasound to evaluate for appendicitis.
Dewhurst C, Beddy P, Pedrosa I. MRI evaluation of acute appendicitis in pregnancy. J Magn Reson Imaging. 2013;37(3):566-75.
Israel GM, Malguria N, Mccarthy S, Copel J, Weinreb J. MRI vs. ultrasound for suspected appendicitis during pregnancy. J Magn Reson Imaging. 2008;28(2):428-33.
Segev L, Segev Y, Rayman S, Nissan A, Sadot E. The diagnostic performance of ultrasound for acute appendicitis in pregnant and young nonpregnant women: A case-control study. Int J Surg. 2016;34:81-85.
Segev L, Segev Y, Rayman S, Nissan A, Sadot E. Acute Appendicitis During Pregnancy: Different from the Nonpregnant State?. World J Surg. 2016.
Theilen LH, Mellnick VM, Longman RE, et al. Utility of magnetic resonance imaging for suspected appendicitis in pregnant women. Am J Obstet Gynecol. 2015;212(3):345.e1-6.
Category: Visual Diagnosis
Keywords: Intussusception, pediatric, ultrasound (PubMed Search)
Posted: 11/21/2016 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
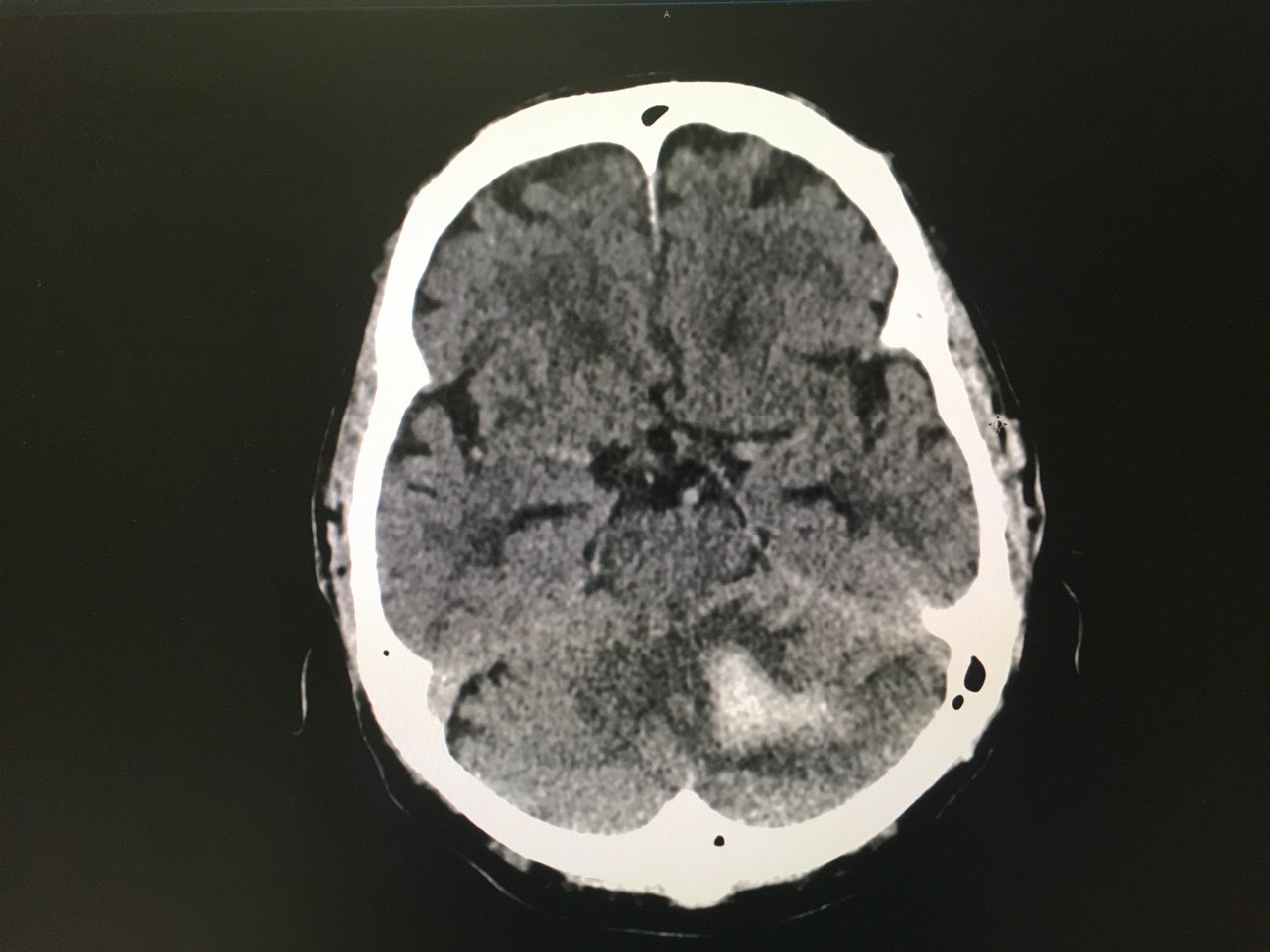
A 15 months old male with no past medical history, presenting with two days of decreased oral intake and decreased urine output. The exam was notable for minimal tenderness of abdomen. During an oral fluid challenge in the ED, the patient had a single episode of bilious vomiting. The ED physician ordered an ultrasound study and the results are shown below. What is the diagnosis?

Diagnosis: Intussusception.
- The use of point of care ultrasound in the ED shortens the time to diagnosis and to definitive treatment. It has a sensitivity of 98-100% even if done by an inexperienced sonographer.
- To diagnose intussusception in the pediatric population, use the High-frequency linear probe for a better image quality. Start with scanning the right upper quadrant, and then move down to scan all four quadrants.
- Classic ultrasound findings include either a Donut-shaped or a Pseudo-kidney appearance, seen as a hypoechoic outer ring and a hyperechoic center. Other variants include; Mesenteric Crescent, where the inner loop will have a crescent hyperechoic appearance with few hypoechoic areas representing lymph nodes, or Central Limb of the Intussusceptum, where a fluid collection is present in the central limb of the intussusceptum instead of a collapsed limb.
- Utilize the US doppler to check for blood flow to the intestinal loops. Diminished blood flow correlates with irreducibility.
Del-Pozo, Gloria, et al. "Intussusception in children: current concepts in diagnosis and enema reduction." Radiographics 19.2 (1999): 299-319.
Category: Visual Diagnosis
Posted: 11/7/2016 by Tu Carol Nguyen, DO
Click here to contact Tu Carol Nguyen, DO
8 year-old female with no PMH who presents with concerns for "purple patches" popping up on her arm for 2-3 days. Stated that one appeared and then, the other one appeared 12 hours later. She denied any trauma whatsoever, history of easy bleeding/bruising and did feel safe at home. The rest of the review of systems was negative.
Patient said there was mild pain when the area was touched. The rest of the physical examination was normal.
What's the diagnosis? (Image below)

Superficial Thermal Burn
Upon further questioning, patient stated that she had been making s'mores by roasting marshmallows over an electric stove 3 days prior. The burns showed up the subsequent morning.
Take Home Points:
Previous pearls about burns:
Pediatric Burns:
Monseau AJ, Reed ZM, Langley KJ, Onks C. Sunburn, Thermal, and Chemical Injuries to the Skin. Prim Care. 2015;42(4):591-605.
"Pathophysiology of Thermal Injury." Civic Plus. 2007.
Category: Visual Diagnosis
Posted: 10/31/2016 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
30 year old female presents with a painful finger for 1 week. Finger exam showed the following. What is the diagnosis ?

Herpetic whitlow
- It is caused by either HSV 1 or 2.
- Infection is usually transmitted by direct unprotected contact.
- Healthcare workers are at risk of contracting the infection if appropriate preventative measures were not taken when dealing with patients who have the infection.
- Diagnosis is mainly clinical. Tzank smears can be done to confirm the diagnosis if in doubt.
- Treatment with Acyclovir is thought to shorten the duration of the infection and prevent recurrence if started within 72 hours of beginning of symptoms.
- Incision of the vesicular lesion is contraindicated and can cause severe bacterial superinfection.
McDonald, Lucas S., et al. "Hand infections." The Journal of hand surgery36.8 (2011): 1403-1412.
