Category: Pediatrics
Keywords: Apparent life threatening event, ALTE, apnea, low risk infants, brief unexplained resolved events (PubMed Search)
Posted: 5/20/2016 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
The American Academy of Pediatrics has developed a new set of clinical practice guidelines to help better manage and think about patients who have experienced an ALTE (Apparent Life Threatening Event). The term BRUE (Brief Resolved Unexplained Event) will replace ALTE.
BRUE is defined as an event in a child younger than 1 year where the observer reports a sudden, brief and now resolved episode of one or more of: cyanosis or pallor; absent, decreased or irregular breathing, marked change in tone or altered level of responsiveness. A BRUE can be diagnosed after a history and physical exam that reveal no explanation.
BRUE can be classified as low risk or high risk. Those that can be categorized as low risk do not require the extensive inpatient evaluation that has often occurred with ALTE.
LOW risk BRUE:
Age > 60 days
Gestational age at least 32 weeks and postconceptual age of at least 45 weeks
First BRUE
Duration < 1 minute
No CPR required by a trained medical provider
No concerning historical features (outlined in the article)
No concerning physical exam findings (outlined in the article)
Recommendations for low risk BRUE:
-SHOULD: Educate, shared decision making, ensure follow up and offer resources for CPR training
-May: Obtain pertussis and 12 lead; briefly monitor patients with continuous pulse oximetry and serial observations
-SHOULD NOT: Obtain WBC, blood culture, CSF studies, BMP, ammonia, blood gas, amino acids, acylcarnitine, CXR, echocardiogram, EEG, initiate home cardiorespiratory monitoring, prescribe acid suppression or anti-epileptic drugs
-NEED NOT: obtain viral respiratory tests, urinalysis, glucose, serum bicarbonate, hemoglobin or neuroimaging, admit to the hospital solely for cardiorespiratory monitoring
*When looking at the evidence strength behind these recommendations, the only one that had a strong level was that you should not obtain WBC, blood culture or CSF
Tieder JS, Bonkowsky JL, Etzel RA, et al. Brief Resolved Unexplained Events (Formerly Apparent Life-Threatening Events) and Evaluation of Lower-Risk Infants. Clinical Practice Guideline. Pediatrics. 2016; 137 (5):e20160590.
Category: International EM
Keywords: Blast, Bombings, Explosions, Terrorism (PubMed Search)
Posted: 5/4/2016 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 5/18/2016)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
The classification of blast injuries was first described by Zuckerman in 1941 and is still widely used today. This system organizes injuries by the mechanism through which they are sustained and classifies them as primary, secondary, tertiary and quaternary. These injuries may occur in isolation or in combination with each other.
| Category | Mechanism | Typical Injuries |
| Primary | Caused by blast wave of overpressure | Tympanic membrane rupture, blast lung, intestinal hemorrhage and rupture |
| Secondary | Caused by flying debris and shrapnel | Blunt and penetrating traumatic injuries
|
| Tertiary | Due to individual being thrown by blast | Blunt and penetrating traumatic injuries
|
| Quaternary | Thermal, toxic, and asphyxiant effects | Thermal burns, chemical burns, exposure to toxins, asphyxiation
|
The term quinary blast injury has also been used to describe delayed effects of explosions, such as infections, radiation exposure, and other toxic exposures.
Author: R. Gentry Wilkerson
Category: Critical Care
Posted: 5/17/2016 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Situations Where ECMO Will Likely Fail
Schmidt M, et al. Ten situations in which ECMO is unlikely to be successful. Intensive Care Med 2016; 42:750-752.
Category: Orthopedics
Keywords: MI, Sport (PubMed Search)
Posted: 5/14/2016 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
https://www.youtube.com/watch?v=sCFOObsx_W4
What is their risk of MI???
Anger outbursts are bad for your heart. Out of 300 patients with an acute MI, just over 2% reported losing their temper within 2 hours of the event. A review of nine studies of rage and cardiovascular events all found an increase in cardiovascular events in the 2 hours preceding an anger outburst. Examples included arguments at home, at work or by road rage. Compared with their usual anger levels, the relative risk of heart attack from a fit of rage was 8.5.
What about those of us who are just fanatics, I mean fans....A recent study of World Cup soccer found that the intense strain and excitement of viewing a dramatic soccer match more than doubles the risk of acute heart attack, particularly in men with known coronary heart disease. This was regardless of the outcome of the match!
Eichner, E. Randy. Current Sports Medicine Reports: March/April 2016
Category: Toxicology
Keywords: digoxin, chronic, poisoning, immune Fab (PubMed Search)
Posted: 5/9/2016 by Bryan Hayes, PharmD
(Updated: 5/12/2016)
Click here to contact Bryan Hayes, PharmD
Patients with chronic digoxin toxicity generally have multiple co-morbidities such as renal failure, dehydration, and cardiac failure. Sick patients with chronically high digoxin levels may have more than just digoxin toxicity as the cause of illness.
A New Study
Prospective observational study with the primary objective to investigate changes in free digoxin concentrations and clinical effects on heart rate and potassium concentrations in chronic digoxin poisoning when digoxin immune Fab are given.
What They Found
One to two vials of digoxin immune Fab initially bound all free digoxin confirming Fab efficacy. However, this was associated with only a moderate improvement in HR (49 to 57 bpm) and potassium (5.3 to 5.0 mmol/L).
Application to Clinical Practice
Chan BS, et al. Efficacy and effectiveness of anti-digoxin antibodies in chronic digoxin poisonings from the DORA study (ATOM-1). Clin Toxicol. 2016 Apr 27. Epub ahead of print. [PMID 27118413]
Follow me on Twitter (@PharmERToxGuy)
Category: Neurology
Keywords: magnetic resonance imaging, MRI, T1, T2, FLAIR, DWI, ADC (PubMed Search)
Posted: 5/11/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Want to learn more about how to read a brain MRI? Here are the basics:
Stay tuned for more pearls in this series on brain MRI!
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: Zika, Guillain-Barre, GBS, ITP, Critical Care (PubMed Search)
Posted: 5/10/2016 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
Zika virus has received significant media attention in the US due to its recent link with teratogenicity. But Zika is also associated with critical and life-threatening complications, including death. Differentiating it from other Flavivirus diseases such as Dengue or Chikungunya can be challenging.
Diagnosis
Complications
1. Petersen LR, Jamieson DJ, Powers AM, Honein MA. Zika Virus. N Engl J Med. 2016 Apr 21;374(16):1552-63. doi: 10.1056/NEJMra1602113. Epub 2016 Mar 30. Review. PubMed PMID: 27028561.
2. LaBeaud, AD. Zika virus infection: An overview. uptodate.com. Accessed 5/10/2016.
3. Cao-Lormeau VM, et al. Guillain-Barr Syndrome outbreak associated with Zika virus infection in French Polynesia: a case-control study. Lancet. 2016 Apr 9;387(10027):1531-9. doi: 10.1016/S0140-6736(16)00562-6. Epub 2016 Mar 2. PubMed PMID: 26948433.
4. Centers for Disease Control and Prevention. Zika virus - What clinicians need to know? Clinician Outreach and Communication Activity (COCA) Call, January 26, 2016. Available at: http://emergency.cdc.gov/coca/ppt/2016/01_26_16_zika.pdf. Accessed May 10, 2016.
Category: Pharmacology & Therapeutics
Keywords: ketamine, shock index, hemodynamic, prehospital, RSI (PubMed Search)
Posted: 5/3/2016 by Bryan Hayes, PharmD
(Updated: 5/7/2016)
Click here to contact Bryan Hayes, PharmD
Ketamine is often thought to be the induction agent least associated with hypotension in the peri-intubation period. However, reports of hypotension following ketamine do exist, including 2 cases of cardiac arrest. [1] There are limited objective means to predict which patients may have an adverse hemodynamic response.
New Study
A new prospective observational study followed 112 patients in the prehospital setting who received ketamine for rapid sequence intubation. 81 had a low shock index [< 0.9], 31 had a high shock index. [2]
Shock index = HR / SBP
What They Found
Patients with a high shock index were more likely to experience hypotension (SBP < 90 mm Hg) in the peri-intubation period compared to those with a low shock index (26% vs 2%).
Application to Clinical Practice
Follow me on Twitter (@PharmERToxGuy)
Category: International EM
Keywords: Selfie; injury; mobile phone; smartphone; social media; travel (PubMed Search)
Posted: 5/2/2016 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 5/4/2016)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Why are selfie deaths on the rise?
People travel everywhere now with their camera equipped smart phones. Capturing a selfie while travelling is very common. This leads to more distracted people and lack of situational-awareness.
Where and how do these deaths occur?
Selfies taken from a height, on a bridge, near motorized traffic, during thunderstorms, at sporting events and near wild animals
Other information:
Submitted by Dr. Laura Diegelmann
Flaherty GT, Choi J; The 'selfie' phenomenon: reducing the risk of harm while using smartphones during international travel. J Travel Med. 2016 Feb 8;23(2).
-Other info sources;
"Mumbai sets no-selfie zones as deaths linked to selfies rise". The Big Story. Retrieved 25 February 2016.
Annie Gowen (14 January 2016). "More people died taking selfies in India last year than anywhere else in the world — The Washington Post". The Washington Post. Retrieved 6 March 2016.
Horton, Helena (22 September 2015). "More people have died by taking selfies this year than by shark attacks". The Daily Telegraph. Retrieved 26 September 2015.
Category: Pediatrics
Posted: 4/29/2016 by Mimi Lu, MD
(Updated: 4/30/2016)
Click here to contact Mimi Lu, MD
Neonatal jaundice- Incidence ~85% of term newborns
Bili levels are EXPECTED to rise during first 5 days of life
Be aware of CONJUGATED hyperbilirubinemias (biliary atresia, infection)
Majority of cases due to increase in unconjugated (indirect) bilirubin 2/2 residual fHgb breakdown and insufficient capacity of hepatic conjugation
Severe hyperbilirubinemia (Tbili >20mg/dL) <2% of term infants
⇒
Acute bilirubin encephalopathy(ABE)- Hypertonia, arching, opisthotonos, fever, high pitched cry
⇒
Kernicterus (5% of ABE)-CP, MR, auditory dysfunction, upward gaze palsy
When to refer for phototherapy/exchange transfusion
“Evaluation and Treatment of Neonatal Hyperbilirubinemia” Muchowski MD, Naval Hospital Camp Pendleton Family Medicine Residency Program, Camp Pendleton, California; Am Fam Physician. 2014 Jun 1;89(11):873-878.
Management of Hyperbilirubinemia in the Newborn Infant35 ore More Weeks of Gestatiion, Pediatrics 2004 July; 114(1)
Category: Neurology
Keywords: seizure, epilepsy, antiepileptic (PubMed Search)
Posted: 4/28/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
A 25 year old patient presents to the emergency department (ED) with a first unprovoked seizure. His ED workup is normal and he is back to his baseline, and you plan to discharge the patient with outpatient follow up within 1 week. The patient is requesting to be discharged on an anti-epileptic drug (AED). What do you do?
Educate the patient about the risk of recurrence, and the possible side effects of AEDs!
The American Academy of Neurology (AAN) specifically addressed this in their 2015 guidelines. A few points to remember:
- The risk of recurrence is greatest within the first 2 years, and occurs in 21-45% of patients.
- The risk of recurrence increases with a remote brain lesion or injury, abnormal EEG, significant brain imaging abnormality or nocturnal seizures.
- AED therapy is likely to reduce the risk of a 2nd unprovoked seizure by about 35% over the next 2 years, but the delay in initiating therapy does not increase the long-term remission risk.
Is it different if the patient had multiple seizures within 24 hours?
Patients presenting with multiple seizures in a 24-hour period were as likely to have seizure recurrence as those presenting with a single seizure, irrespective of etiology or treatment.
Bergey GK. Management of a First Seizure. Continuum 2016;22(1):38 50.
Category: Critical Care
Keywords: in hospital cardiac arrest, cardiac arrest (PubMed Search)
Posted: 4/26/2016 by Feras Khan, MD
Click here to contact Feras Khan, MD
A recent survey looked at resuscitation practices that could help improve survival during in-hospital cardiac arrest
Category: Orthopedics
Keywords: Sudden cardiac death, physical activity (PubMed Search)
Posted: 4/23/2016 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Exercise and the heart
Exercise increases the risk of sudden cardiac death (SCD) acutely.
Exercise decreases the risk of SCD in the long term.
Regular physical activity (even as little as 15 mins/day) reduces the risk of cardiovascular disease (CVD).
Up to 15% of MIs occur during or soon after vigorous physical exercise. This is typically in sedentary men with coronary risk factors.
In a 1993 study, in the first hour after heavy exertion, risk of heart attack rose more than 100-fold from baseline for habitually inactive persons. However, for frequent exercisers, this risk rose less than three-fold. Think of snow shoveling after a winter storm.
Both the Physicians’ Health Study and the Nurses’ Health Study show that the risk of SCD during exertion is reduced by habitual exercise.
If you are physically active, stay active. If you are not active, you should be because exercise has innumerable personal benefits. However, it is important to start gradually Some individuals at higher risk need to start under the guidance of a physician.
Category: International EM
Keywords: Research, ethics, informed consent (PubMed Search)
Posted: 4/21/2016 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
The terms and concepts of “waiver of informed consent’ versus “exception from informed consent” are often confused. Within the U.S., these concepts are not the same.
Bottom line:
Waiver of Informed Consent ≠ EFIC
These are the rules and regulations for the U.S. The regulations for emergency research in other countries may or may not be similar to these.
45 CFR 46.116(d)
21 CFR 50.24 and 45 CFR 46.101
Category: Critical Care
Posted: 4/19/2016 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Can NIV be Used in ARDS?
Demoule A, et al. Can we prevent intubation in patients with ARDS? Intensive Care Med 2016; 42:768-771.
Category: Pediatrics
Keywords: Intracranial hemorrhage, ultrasound, non accidental trauma (PubMed Search)
Posted: 4/15/2016 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Typically, if an infant or young child presents to the ED with concern for intracranial hemorrhage (ICH), CT is performed as a rapid diagnostic tool. Now that clinicians are more aware of the radiation associated with head CT, the possible use of ultrasound was studied. Ultrasound is commonly used in the neonatal population for detecting ICH. A study by Elkhunovich et al looked at children younger than 2 years who had cranial ultrasounds preformed. Over a 5 year period, 283 ultrasounds were done on patients between 0 to 485 days old (median 33 days). There were 39 bleeds detected. Ultrasound specificity and sensitivity was calculated by comparing the results with CT, MRI and/or clinical outcome. For significant bleeds, the sensitivity for ultrasound was 81%. The specificity for detecting ICH was 97%.
Only 2 patients in the study were older than 1 year. The proper windows are easiest to visualize in children younger than 6 months.
Bottom Line: The sensitivity of cranial ultrasound is inadequate to justify its use as a screening tool for detection of ICH in an infant with acute trauma, but it could be considered in situations when obtaining advanced imaging is not an option because of availability or patient condition.
Elkhunovich M, Sirody J, McCormick T, Goodarzian F and Claudius I. The Utility of Cranial Ultrasound for Detection of Intracranial Hemorrhage in Infants. Ped Emerg Care 2016 [epub ahead of print].
Category: Toxicology
Keywords: Extracorporeal Membrane Oxygenation, ECMO, toxicology, poison (PubMed Search)
Posted: 4/13/2016 by Bryan Hayes, PharmD
(Updated: 4/14/2016)
Click here to contact Bryan Hayes, PharmD
The American College of Medical Toxicology's ToxIC Registry is a self-reporting database completed by medical toxicologists across 69 insitutions in the US.
Application to Clinical Practice
In settings where ECMO is available, it may be a potential treatment option in severely poisoned patients. From the limited data, ECMO was generally administered prior to cardiovascular failure and might be of benefit particularly during the time the drug is being metabolized.
Table from the Case Series
Wang GS, et al. Extracorporeal Membrane Oxygenation (ECMO) for Severe Toxicological Exposures: Review of the Toxicology Investigators Consortium (ToxIC). J Med Toxicol 2016;12(1):95-9. [PMID 26013746]
Follow me on Twitter (@PharmERToxGuy)
Category: Neurology
Keywords: dizzy, dizzinesss, acute vestibular syndrome, triggered episodic vestibular syndrome, spontaneous episodic vestibular syndrome, HINTS, Dix-Hallpike (PubMed Search)
Posted: 4/13/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
What Do You Mean By Dizzy?
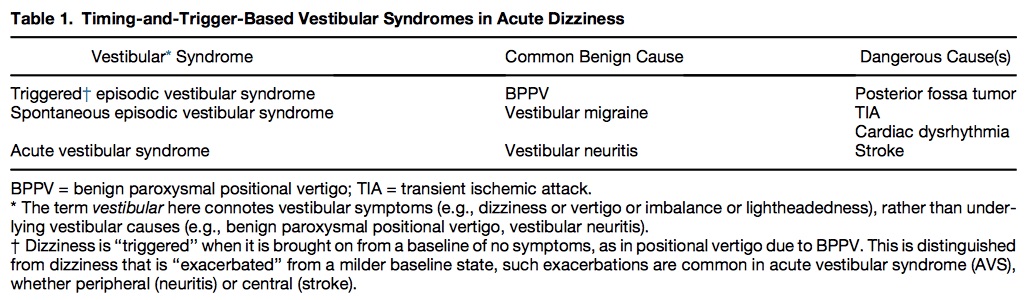
Table 1 shows common benign and serious causes of these vestibular syndromes.
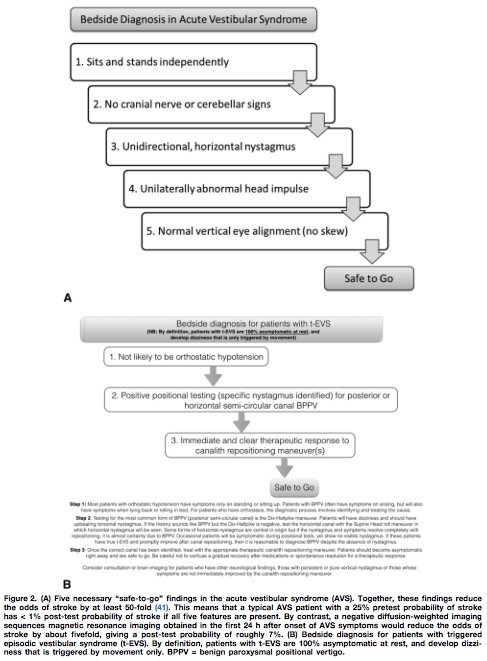
Utilizing the HINTS battery or the Dix-Hallpike maneuver, a “safe to go” algorithm for acute vestibular syndrome and triggered episodic vestibular syndrome is outlined in Figure 2.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: seizure, status epilepticus, pregnancy (PubMed Search)
Posted: 4/13/2016 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
Disclaimer: Talking about seizures/status that is NOT due to eclampsia
TAKE HOME: While no AEDs are completely safe in pregnancy, treatment and stabilization of maternal status epilepticus is paramount for fetal health. Involve neurology/epileptology and OB/maternal-fetal medicine.
1. Hern ndez-D az S, et al; North American AED Pregnancy Registry; North American AED Pregnancy Registry. Comparative safety of antiepileptic drugs during pregnancy. Neurology. 2012 May 22;78(21):1692-9.
2. McElhatton PR. The effects of benzodiazepine use during pregnancy and lactation. Reprod Toxicol. 1994 Nov-Dec;8(6):461-75.
3. Lexicomp online accessed via uptodate.com.
Category: Orthopedics
Posted: 4/10/2016 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Orthopedic documentation
1) Document location with specificity and laterality.
2) Document the location with as much specificity as possible
-Name of specific bone and specific site on bone (Shaft, head, neck, distal, proximal, styloid)
3) Document fractures as open/closed, displaced vs. non-displaced, routine or delayed healing,
-Orientation of fractures, such as transverse, oblique, spiral
- Document intra-articular or extra-articular involvement
4) For a particular injury, a complete note will include mention of the following
The joint above (e.g. for shoulder injuries this would be the neck, for hip injuries - the back)
The joint below
Motor (e.g. for arm injuries document the distal median, radial and ulnar motor innervation)
Sensory
Vascular
Skin (for all fractures document intact overlying skin esp. when covering with a splint)
Compartments (a simple mention of compartments are grossly soft/not tense will suffice)
*Especially relevant for forearm and tib/fib injuries
