Category: Critical Care
Keywords: Zika Virus, Guillain-Barre (PubMed Search)
Posted: 8/9/2016 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Zika Virus-associated GBS
Thiery G, et al. Zika virus-associated Guillain-Barre syndrome: a warning for critical care physicians. Intensive Care Med 2016; epub ahead of print.
Category: Pharmacology & Therapeutics
Keywords: amiodarone, procainamide, ventricular tachycardia (PubMed Search)
Posted: 8/6/2016 by Michelle Hines, PharmD
Click here to contact Michelle Hines, PharmD
Amiodarone 150 mg IV over 10 minutes and procainamide IV 20-50 mg/min (up to 17 mg/kg) are two antiarrhythmic medications recommended in the American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care for stable wide QRS complex tachycardia. [1]
What they did:
Multi-center, prospective, randomized, open-label trial comparing the incidence of major cardiac events in the acute treatment of hemodynamically stable patients with wide QRS monomorphic tachycardia (presumed to be VT) using amiodarone 5 mg/kg IV infused over 20 minutes versus procainamide 10 mg/kg IV infused over 20 minutes. [2] The study period was 40 minutes, starting from the beginning of the infusion.
What they found:
Application to clinical practice:
Follow me on Twitter (@mEDPharmD)
Category: Toxicology
Keywords: Hypoglycemia, Sulfonylureas (PubMed Search)
Posted: 8/4/2016 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
Drug-induced hypoglycemia is an often severe and symptomatic. It is a potentially preventable cause of significant morbidity. In one large study, it accounted for 23% for hospital admissions due to adverse drug events and 4.4% of overall admissions. The majority of hypoglycemic events occur with insulin and sulfonylureas. However, multiple drugs can affect glucose homeostasis and have been cited to cause hypoglycemia in therapeutic dose alone or in combination with other medications or illness. Factors that predispose to low blood sugar include reduced food intake, age, hepatic and renal disease, and severe infection. Beware of the possibility of inducing hypoglycemia in patients taking the following:
Agents with lesser quality evidence as predisposing medications or illnesses were present:
Drugs induced hypoglycemia should always be considered in the differential diagnosis of every patient presenting with low blood glucose. Octreotide antagonizes pancreatic insulin secretion and should be considered for first-line therapy in the treatment of sulfonylurea-induced hypoglycemia particularly when glucose levels cannot be maintained by dextrose infusions. Octreotide is administered 50 mcg subcutaneously (1-10 mcg in children) every 12 hours.
Category: Toxicology
Keywords: novel synthetic opioid, U-47700 (PubMed Search)
Posted: 8/1/2016 by Hong Kim, MD
(Updated: 2/7/2026)
Click here to contact Hong Kim, MD
Recently, there have been several news reports regarding the emergence of synthetic opioids in the U.S. and Canada. There are multiple synthetic opioids that have been identified as potential agents of abuse including W-18, U-47700, fentanyl derivatives, AH-7921 and MT-45. These compounds share a similar story with synthetic cannabinoid where they were synthesized for research purpose or by pharmaceutical companies but were not marketed. They are often sold as “research chemicals” over the internet.
In July 2016, three case reports have been published regarding several cases of U-47700 intoxication in San Diego, CA and Dallas, TX.
It is unknown if currently available heroin is cut with above mentioned synthetic opioids. Like other opioid receptor agonists, administration of naloxone will likely reverse the opioid toxidrome. But clinical experience in reversing synthetic opioids intoxication with naloxone is limited.
Bottom line:
Irrespective of whether an ED patient is exposed to synthetic opioids or "traditional" opioids of abuse (prescription opioid pain medication or heroin), the management of opioid intoxication management remains unchanged for respiratory depression.
Category: International EM
Keywords: Arbovirus, mosquitos (PubMed Search)
Posted: 8/3/2016 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 2/7/2026)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
An Arbovirus is a virus transmitted primarily by an arthropod
There are a number of major arbovirus families:
The main viral family that causes substantial human disease is the Flaviviridae family.
Category: Critical Care
Keywords: ROSC, Cardiac Arrest, ETCO2 (PubMed Search)
Posted: 8/2/2016 by Rory Spiegel, MD
Click here to contact Rory Spiegel, MD
Despite a lack of prospective data, end-tidal CO2 (ETCO2) is often proposed as a viable replacement for the traditional pulse check to identify return of spontaneous circulation (ROSC) in patients presenting to the Emergency Department in Cardiac Arrest. A recent study by Tat et al examined this very question. The authors prospectively enrolled 178 patients suffering out-of-hospital cardiac arrest (OHCA) and examined the accuracy of a rise in ETCO2 at predicting ROSC. The authors examined both a rise of 10 and 20 mm Hg in ETCO2. Of the 178 patients included in this cohort, 60 (34%) experienced ROSC. The sensitivity and specificity of ETCO2 to predict ROSC at a threshold of 10 mm Hg was 33% and 97% respectively. At a threshold of 20 mm Hg ETCO2 performed no better with a sensitivity and specificity of 20% and 99% respectively.
What this data suggests is while a rise of ETCO2 of greater than 10 is highly suggestive of ROSC, the contrary cannot be said. The absence of a spike in ETCO2 does not rule out ROSC, as the large majority of patients experiencing ROSC in this cohort did so without demonstrating a significant rise in ETCO2. This evidence suggests that ETCO2 is a poor surrogate for a pulse check.
Tat LC, Ming PK, Leung TK, Abrupt rise of end tidal carbon dioxide level was a specific but non sensitive marker of return of spontaneous circulation in patient with out-of-hospital cardiac arrest, Resuscitation (2016), http://dx.doi.org/10.1016/j.resuscitation.2016.04.018
Category: Pediatrics
Keywords: airway. mac (PubMed Search)
Posted: 7/29/2016 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
The pediatric epiglottis is more "U" shaped, often overlies the glottic opening, and is "less in line with the trachea."1 Because of this, it has traditionally been taught that a Miller blade is the ideal laryngoscope.
Varghese et al compared the efficacy of the Macintosh blade and the Miller blade when placed in the vallecula of children between the ages of 1 and 24 months. The blades provided similar views and suffered similar failure rates. When the opposite blade was used as a backup, it had a similar success rate as the opposing blade.2 Passi et al also compared these two blades, this time placing the Miller blade over the epiglottis. Again, similar views were achieved.3
1. Harless J, Ramaiah R, Bhananker S. Pediatric airway management. Int J. Crit Illn Inj Sci. 2014;4(1):65-70.
2. Varghese E, Kundu R. Does the Miller blade truly provide a better laryngoscopic view and intubating conditions than the Macintosh blade in small children? Paediatr Anaesth. 2014;24:825-829.
3. Passi Y, Sathyamoorthy M, Lerman J, et al. Comparison of the laryngoscopy views with the size 1 Miller and Macintosh laryngoscope blades lifting the epiglottis or the base of the tongue in infants and children <2 yr. of age. Br J Anaesth. 2014;113(5):869-874.
Category: Neurology
Keywords: SAH, headache, LP, CTA (PubMed Search)
Posted: 7/27/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Clinical Guidelines for the Emergency Department Evaluation of Subarachnoid Hemorrhage. Meurer WJ, Walsh B, Vilke GM and Coyne CJ. JEM 2016; 50(4) 696-701
Category: Critical Care
Posted: 7/26/2016 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Predicting Fluid Responsiveness with ETCO2
Category: Orthopedics
Keywords: Chest, muscle injury (PubMed Search)
Posted: 7/24/2016 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
30yo male weight lifter who 10 days ago had a painful left shoulder injury after bench press. The next morning his left anterior chest wall and left upper arm were bruised and swollen. He went to see his PCP who diagnosed him with a muscle strain. 8 days later the bruising and swelling have resolved but he still cant move his shoulder and comes to the ED.
http://321gomd.com/wp-content/uploads/2015/01/pec-major-tears.jpg
The pec major attaches to the humerus and originates from the sternum and clavicle
Injury is usually due to tendon rupture off the humerus but can also occur at the muscle tendon junction or within the muscle belly itself.
Injury is becoming increasingly common due to the popularity in power lifting sports.
Mechanism: excessive tension on a maximally eccentrically contracted muscle.
Patients will complain of pain and weakness of the shoulder.
PE: Swelling and bruising to anterior medial arm. Palpable defect and deformity or anterior axially fold (may be hidden by swelling).
Weakness and pain with adduction and internal rotation and forward flexion
Chronic presentations can be challenging to diagnose. Consider ultrasound
Non operative treatment may be indicated for partial tears (sling, ice, NSAIDs)
Operative repair of tendon avulsions is very successful. Patients age, occupation/activity level and location of injury and condition of tear are considered.
Category: Critical Care
Posted: 7/20/2016 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Bucher J, Koyfman A. Intubation of the neurologically injured patient. J Emerg Med 2016; 49:920-7.
Category: International EM
Keywords: World Health Organization, blood donation (PubMed Search)
Posted: 7/9/2016 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 7/20/2016)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Just the Facts:
112.5-million blood donations globally and half of these come from High-income countries
High-income countries more often use blood for supportive care during surgery, in traumas or therapy for malignancies
Low and middle-income countries more often use blood to manage pregnancy-related complications or in severe childhood anemia
General availability of blood is based on the donation rate
High-income countries have 33.1 donations/1000 people
Middle-income countries have 11.7 donations/1000 people
Low-income countries have 4.6 donations/1000 people
70 countries reported collecting fewer than 10 donations per 1000 people and half of these countries were in the African region
Disease prevalence in the region is reflected in the transmission rate of transfusion-transmissible infections (TTI)
Table 1. Prevalence of TTIs in blood donations (Median, Interquartile range (IQR)), by income groups
|
| HIV | HBV | HCV |
|
|---|---|---|---|---|
| High-income countries | 0.003% (0.001% – 0.040%) | 0.030% (0.008% – 0.180%) | 0.020% (0.003% – 0.160%) | |
| Middle-income countries | 0.120% (0.020% – 0.340%) | 0.910% (0.280% – 2.460%) | 0.320% (0.090% – 0.690%) | |
| Low-income countries | 1.080% (0.560% – 2.690%) | 3.700% (3.340% – 8.470%) | 1.030% (0.670% – 1.800%) |
Submitted by: Dr. Laura Diegelmann
Category: Misc
Keywords: Neck pain (PubMed Search)
Posted: 7/16/2016 by Michael Bond, MD
(Updated: 2/7/2026)
Click here to contact Michael Bond, MD
Non-Musculoskeletal Causes of Neck Pain
Neck pain is a common complaint of people presenting to the ED. Most of the cases will be musculoskeleteal in origin and will respond to conservative therapy with NSAIDs or acetominophen. However, other non-musculoskeletal causes of pain could be lurky behind this benign complaint.
Don't forget to consider:
Category: Pediatrics
Keywords: Intranasal vaccine, immunizations (PubMed Search)
Posted: 7/15/2016 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Although it is summer, preparations are being made for the 2016-2017 influenza season. The Center for Disease Control (CDC) no longer recommends the live attenuated influenza vaccine (LAIV4). The American Academy of Pediatrics has supported this statement.
The LAIV4 (the only intranasal vaccine available) was offered to patients over the age of 2 years without respiratory problems. Observational studies during the 2013-2015 seasons have shown that the LAIV4 has an adjusted vaccine efficacy of 3% compared to 63% for the inactivated vaccine (intramuscular). Children who received the intranasal vaccine were almost 4 times more likely to get the flu compared to children who received the injection.
Bottom line: Only the intramuscular shot is recommended for this upcoming season. This is causing many primary care practices to scramble to obtain enough vaccine.
Bernstein HH and Kimberlin DW. Intranasal FluMISSED its target. AAP News. July 2016.
Chung J et al. Seasonal Effectiveness of Live Attenuated and Inactivated Influenza Virus. Pediatrics 2016: 137 (2).
Category: Neurology
Keywords: Large vessel occlusion stroke, endovascular intervention, Field Assessment Stroke Triage for Emergency Destination, FAST-ED, NIHSS, Rapid Arterial Occlusion Evaluation, RACE, Cincinnati Prehospital Stroke Severity scale, CPSS (PubMed Search)
Posted: 7/13/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
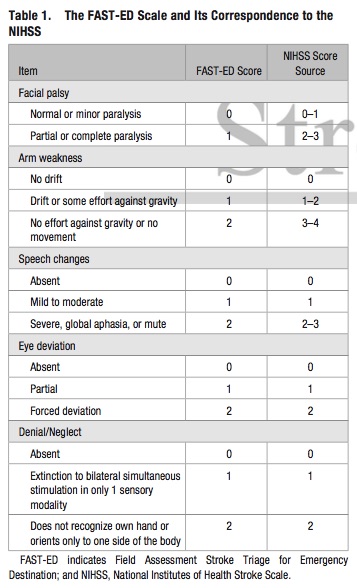
Bottom Line: Additional assessment of gaze deviation, aphasia and neglect, as included in the FAST-ED scale, increases the accuracy of predicting LVOS.
Follow me on Twitter @EM_NCC
Category: Critical Care
Posted: 7/12/2016 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
LVADs and RV Failure
Sen A, et al. Mechanical circulatory assist devices: a primer for critical care and emergency physicians. Crit Care 2016; 20:153.
Category: Orthopedics
Keywords: Foot injury, bipartate (PubMed Search)
Posted: 7/10/2016 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Sesamoid Injuries
Unlike other bones in the human body that are connected to each other at joints, sesamoid bones are only connected via tendons (or are imbedded in muscle).
The largest sesamoid bone is the patella.
2 small sesamoid bones lie on the plantar foot near the great toe
Sesamoid bones can fracture and the surrounding tendons can become inflamed (sesamoiditis)
Traumatic injury is usually due to hyperextension and axial loading
Sx: Pain located under the great toe on the ball of the foot (Gradual with sesamoiditis and acutely with a fracture).
There may be associated swelling and bruising. Pain with palpation, flexion and extension.
The medial/tibial sesamoid is larger, has great weight bearing status and is more commonly injured that its lateral counterpart.
In many people (10 - 25%) the medial sesamoid of the foot has two parts (bipartite). This finding is bilateral in 25% of people.
This may confuse some providers as it may appear to be a fracture
Look for a smooth contour to the bones and clinically correlate (bruising, soft tissue swelling, etc.) if it is an incidental finding.
Other radiographic clues include
1) The fractured sesamoid is usually slightly larger than the lateral sesamoid while the bipartite sesamoid has a much larger medial sesamoid than lateral sesamoid
2) The fractured sesamoid shows a sharp, radiolucent, uncorticated line between the two fragments while the bipartite sesamoid has two corticated components
3) The fractured sesamoid fragments often fit together like pieces of a puzzle while the bipartite sesamoid has two components that do not fit together snugly
4) Other means to differentiate the two involve MRI and bone scanning
Treatment involves a stiff-soled shoe or applying a cushioning pad or J-shaped pad around the area to relieve pressure.
It may take months for the pain to subside.
http://www.apfmj-archive.com/afm5_3/afm50.htm#F1
Chu and Resnick, MRI Web Clinic June 2014.
Category: International EM
Keywords: Disaster, mass casuality (PubMed Search)
Posted: 7/6/2016 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
There are many definitions for a disaster. Per the International Federation of Red Cross and Red Crescent Societies (IFRC), they define a disaster as:“…a sudden, calamitous event that seriously disrupts the functioning of a community or society and causes human, material, and economic or environmental losses that exceed the community’s or society’s ability to cope using its own resources. Though often caused by nature, disasters can have human origins.”
However, in the heat of the moment, a shorter definition is easier to remember. The IFRC also define a disaster as:
A shorter, more practical definition is:
http://www.ifrc.org/en/what-we-do/disaster-management/about-disasters/what-is-a-disaster/
Category: Pharmacology & Therapeutics
Keywords: fluoroquinolone, tendon rupture (PubMed Search)
Posted: 7/1/2016 by Michelle Hines, PharmD
(Updated: 7/2/2016)
Click here to contact Michelle Hines, PharmD
Fluoroquinolone antibiotics are used to treat a wide range of infections and as prophylaxis against infection in certain immune compromised patients. In 2008 the FDA issued a boxed warning for tendonitis and tendon rupture for the fluoroquinolone antibiotic class, and in May 2016 a statement recommending the use of alternate therapies for uncomplicated UTIs and upper respiratory infections was issued. The mechanism by which fluoroquinolones causes tendon injury has not been elucidated, but may be related to oxidative stress caused by the overproduction of reactive oxygen species in tenocytes.
Adverse event reporting to the FDA is performed voluntarily by healthcare professionals and consumers through MedWatch. An analysis of tendon rupture events associated with fluoroquinolone use reported to the FDA’s Adverse Event Reporting System (FAERS) database was recently published.
What they found:
Application to clinical practice:
Arabyat RM, et al. Fluoroquinolone-associated tendon-rupture: a summary of reports in the Food and Drug Administration’s adverse event reporting system. Expert Opin Drug Saf 2015; 14:1653-60. (PMID 26393387)
FDA Drug Safety Communication from 5/12/2016: http://www.fda.gov/Drugs/DrugSafety/ucm500143.htm
Follow me on Twitter (@mEDPharmD)
Category: Orthopedics
Keywords: Trauma, pelvis, plain films (PubMed Search)
Posted: 6/26/2016 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Plain films are commonly used to screen children for pelvic fractures or dislocations following blunt torso trauma
The sensitivity of this common screening practice is unknown
A recent study looked at this question.
Of 451 patients with pelvic fractures or dislocations, 382 had AP radiographs. Injury was correctly identified in 297 patients (sensitivity 78%).
The sensitivity was greater in the sicker subgroups :92% for those requiring operative intervention and 82% for those with hypotension
Plain AP pelvic radiographs should have a limited role in the sole evaluation of children with blunt torso trauma.
They should be incorporated in the assessment of hemodynamically unstable children and those in whom the clinician is not planning on otherwise obtaining an abdominal/pelvis CT.
Kwok et al., 2015 Annals of Emergency Medicine
