Category: International EM
Keywords: Boarding, crowding, patient flow (PubMed Search)
Posted: 3/1/2017 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Emergency department crowding is an almost universal problem. Whether it is called "access block" (Austalia) or "boarding" (United States), it is seen everywhere.
The American College of Emergency Physicians (ACEP) states that "a “boarded patient” is defined as a patient who remains in the emergency department after the patient has been admitted to the facility, but has not been transferred to an inpatient unit."
It should be clear that the primary cause of overcrowding is boarding: the practice of holding patients in the emergency department after they have been admitted to the hospital, because no inpatient beds are available. This practice has been shown to have an adverse impact on patients, with longer delays causing greater morbidity and mortality.
ACEP has created resources to help address this issue, including an emergency medicine practice paper on high impact solutions. See: file:///Users/jhirshon/Downloads/EMPC_Crowding%20IP_092016%20(1).pdf
https://www.acep.org/Clinical---Practice-Management/Definition-of-Boarded-Patient-2147469010/
https://www.acep.org/content.aspx?id=32050
Category: Critical Care
Keywords: Ketamine, agitated delirium (PubMed Search)
Posted: 2/28/2017 by Rory Spiegel, MD
(Updated: 2/8/2026)
Click here to contact Rory Spiegel, MD
A recently published study adds to the growing body of literature supporting the use of IV//IM ketamine as a first line agent for the control of the acutely agitated patient. In this observational cohort Riddell et al found patients given ketamine more frequently achieved adequate sedation at both 5 and 10 minutes compared to benzodiazepines, Haloperidol, given alone or in combination. This rapid sedation was achieved without an increase in the need for additional sedation or the rate of adverse events.
Riddell J, Tran A, Bengiamin R, Hendey GW, Armenian P. Ketamine as a first-line treatment for severely agitated emergency department patients. Am J Emerg Med. 2017
Category: Orthopedics
Keywords: forearm trauma (PubMed Search)
Posted: 2/25/2017 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
The Essex-Lopresti injury pattern is the lesser known of the triad of forearm injuries (Monteggia & Galeazzi).
It follows the “rule of the ring” aka the life saver candy rule: You can’t break a life saver in just one place.
These injury patterns are frequently missed because our eyes are drawn to the fracture and miss the associated dislocation.
The Essex-Lopresti fracture pattern involves a fracture of the radial head with concomitant dislocation of the distal radio-ulnar joint (DRUG)
-With associated interosseous membrane disruption
Think of it as the Maisonneuve fracture of the forearm.
Mechanism: fall from height/high energy forearm trauma.
PE: Suspect if patient has significant tenderness at the DRUG with a radial head fx.
Patients have worse outcomes if injury is missed on initial presentation due to radial migration and instability.
Take home point: Remember the rule of the ring. Remember to exam the elbow with wrist injuries and the wrist with all elbow injuries
Category: Neurology
Keywords: stroke, alcohol, substance abuse, mimics (PubMed Search)
Posted: 2/22/2017 by Danya Khoujah, MBBS
(Updated: 2/8/2026)
Click here to contact Danya Khoujah, MBBS
Category: Orthopedics
Keywords: Back Pain, Treatment (PubMed Search)
Posted: 2/18/2017 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Treatment of Low Back Pain
A recent recommendation from the American College of Physicians (Internal Medicine) now recommends nonpharmacologic therapies as the first line treatment of acute or subacute lower back pain lasting 12 weeks or less. This might bring more people to our Emergency Departments so it is important that we know their current recommendations.
Some nonpharmacologic therapies recommended are:
For acute back pain they recommend:
For chronic back pain:
Category: Pediatrics
Keywords: unicameral bone cyst, fracture (PubMed Search)
Posted: 2/18/2017 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
A 12 year old with arm pain after doing push ups during gym class. What is the diagnosis?
Diagnosis: Pathologic fracture with a unicameral bone cyst
Unicameral bone cysts are benign lesions that mainly affect children and adolescents. On xray the cyst is noted to be a mildly expansile, lytic, thin walled lesion without periosteal reaction. The most common sites are the proximal humerus and femur. These lesions can resolve spontaneously, but there is a risk of pathologic fracture. If fracture is detected, then the fracture site should be treated as any other fracture in the area. These lesions can also be found incidentally in which case they should be referred to orthopedics for outpatient follow up.
Kadhim, M, Thacker M, Kadhim A and Holmes L. Treatment of unicameral bone cyst: systemic review and meta analysis. J Child Orthop. 2014 Mar; 8(2): 171-191.
Mascard E, Gomez-Brouchet A, Lambot K. Bone cysts: Unicameral and aneurysmal bone cyst. Orthop Traumatol Surg Res. 2015 Feb; 101.
Category: Toxicology
Keywords: Buprenorphine, Suboxone (PubMed Search)
Posted: 2/16/2017 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
The current opioid epidemic is considered the worst drug crisis in American history responsible for 50,000 deaths per year in the US from overdose of heroin and opioid prescription drugs. A 200% increase in the rate of overdose deaths involving opioids occurred between 2000 and 2014. The continued rise in opioid related deaths calls for an urgent need for treatment. Three types of medication-assisted therapies (MATs) are available for treating patients with opioid addiction:methadone, buprenorphine, and naltrexone. Suboxone a combination of buprenorphine and naloxone, is emerging as one of the best choices for the following reasons:
Rudd RA, Seth P, David F, Scholl L. Increase in Drug and Opioid-involved Overose Deaths -Unted States, 2010-2015. MMWR Morb Mortal Wkly Rep. ePub: 16 December 2016.
Jones HE. Practical Considerations for the Clinical Use of Buprenorphine. Science & Practice Perspectives. 2004;2(2):4-20.
Category: International EM
Keywords: Zika, arbovirus, pregnancy, congenital (PubMed Search)
Posted: 2/15/2017 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 2/8/2026)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Congenital infection with the Zika virus is associated with 5 types of birth defects
· These are rarely or never seen with other infections during pregnancy
· These defects are:
1. Severe microcephaly (small head size) resulting in a partially collapsed skull
2. Decreased brain tissue with brain damage
3. Damage to the back of the eye with a specific pattern of scarring and increased pigment
4. Limited range of joint motion, such as clubfoot
5. Too much muscle tone restricting body movement soon after birth
https://www.cdc.gov/zika/pregnancy/
Category: Critical Care
Posted: 2/14/2017 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Sepsis Mimics
Long B, Koyfman A. Clinical mimics: An emergency medicine-focused review of sepsis mimics. J Emerg Med. 2017; 52:34-42.
Category: Visual Diagnosis
Posted: 2/13/2017 by Tu Carol Nguyen, DO
Click here to contact Tu Carol Nguyen, DO
56 year-old male with history of hypertension presents with complaints of right scrotal swelling and pain. Denies any urinary symptoms, abdominal pain, nausea/vomiting or change in bowel habits or prior episodes. Temp was 99.0.
A scrotal ultrasound was done and an image of the right testis was seen (below). What's the diagnosis?
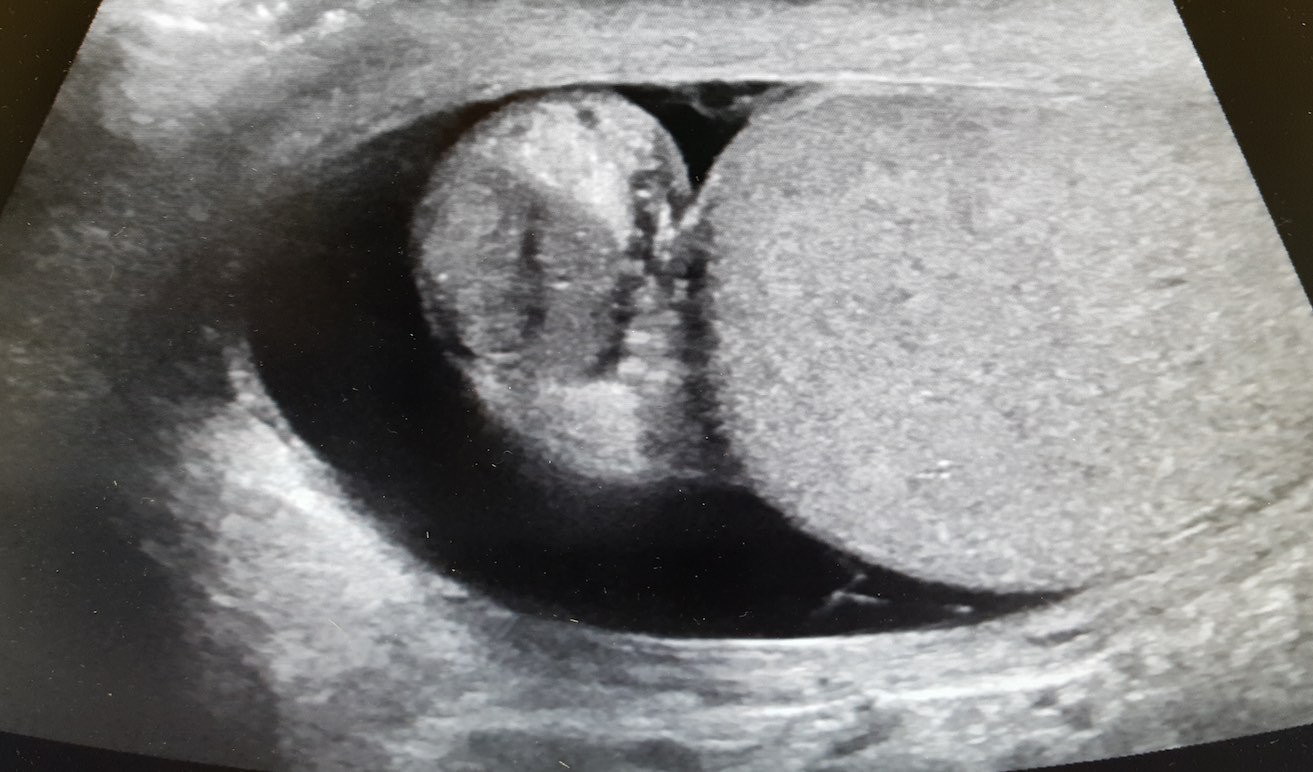
Answer: Right Epididymitis (and Hydrocele)
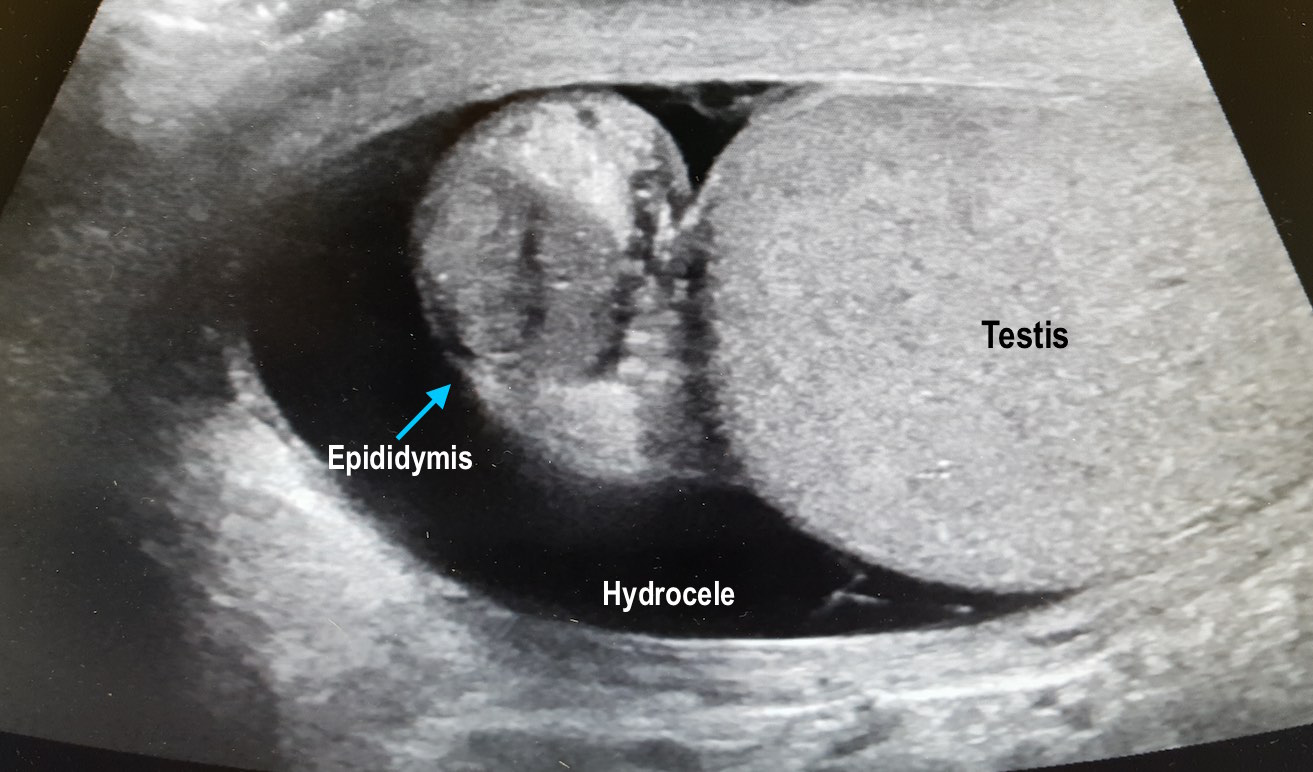
Take Home Points:
Kühn AL, Scortegagna E, Nowitzki KM, Kim YH. Ultrasonography of the scrotum in adults. Ultrasonography. 2016;35(3):180-97.
Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2015. MMWR Recomm Rep 2015;64(No. RR-3): 1-137.
Category: Airway Management
Keywords: Elbow, fracture, trauma (PubMed Search)
Posted: 2/11/2017 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Is that a fracture or a growth plate?
Pediatric elbow x-rays are complicated to interpret due to the large number of ossification centers.
Elbow trauma is common in pediatrics.
Ossification centers of the elbow appear in a reliable chronologic pattern which aids in distinguising fractures from growth plates.
Note the age ranges are an estimate with great variability. For example, girls can develop these up to 2 years earlier than boys.
The numbers 1/3/5/7/9/11 correspond to the average age of development of each ossification center
Years of fusion shown below in ()
Capitellum (12-14yo)
Radial head (14-16yo)
Medial epicondyle (16-18yo)
Trochlea (12-14yo)
Olecranon (15-17yo)
Lateral epicondyle (12-14yo)
Pneumonic: "Can't Resist My Team Of Lawyers"
Consider ordering films of both elbows to compare if in doubt.
How is this useful? If the trochlear center is present, but there is no medial epicondyle then you are most likely looking at a fx where the ossification center has been avulsed and displaced.
Category: Neurology
Keywords: aphasia, fluency, comprehension, repetition, Broca's aphasia, Wernicke's aphasia, conduction aphasia (PubMed Search)
Posted: 2/8/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Types of aphasia [Online image]. Retrieved February 8, 2017 from https://www.aphasia.org/
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: peri-Intubation hypotension, shock index (PubMed Search)
Posted: 2/7/2017 by Rory Spiegel, MD
(Updated: 2/8/2026)
Click here to contact Rory Spiegel, MD
Identifying patients at risk of hypotension during intubation is not always straight forward. The prevalence of peri-intubation hypotension in the Emergency Department has been demonstrated to be approximately 20%.1 And while certain variables increase the likelihood of peri-intubation hypotension (ex. Shock index> 0.80), no single factor predicts it accurately enough to be used at the bedside.2 In the majority of patients undergoing intubation, clinicians should be prepared for peri-intubation hypotension with either vasopressor infusions or push dose pressors.
1. Heffner AC, Swords D, Kline JA, Jones AE. The frequency and significance of postintubation hypotension during emergency airway management. J Crit Care. 2012;27(4):417.e9-13.
2. Heffner AC, Swords DS, Nussbaum ML, Kline JA, Jones AE. Predictors of the complication of postintubation hypotension during emergency airway management. J Crit Care. 2012;27(6):587-93.
Category: Visual Diagnosis
Keywords: Herpes Zoster Ophthalmicus; Hutchinson's sign (PubMed Search)
Posted: 2/6/2017 by Hussain Alhashem, MBBS
(Updated: 2/8/2026)
Click here to contact Hussain Alhashem, MBBS
24-year-old male with a history of Wagner's Granulomatosis, currently on Cellcept (Mycophenolate Mofetil) and high dose prednisolone, presented with two days of sore throat, malaise and the lesions shown in the picture. What is the diagnosis?


Answer: Herpes Zoster with Hutchinson's sign.
- This patient is presenting with a well demarcated eruptive skin lesion involving the tip of the nose and half of the lip and palate. This lesion is suggestive of Herpes Zoster with Hutchinson's sign.
- Hutchinson's sign is associated with a high rate of corneal denervation and ocular involvement. Some studies suggest that up to 100% of patients with Hutchinson's sign will present with a serious intraocular pathology.
- In addition to starting systemic antiviral therapy, all patients who present with Hutchinson's sign need an immediate and complete ophthalmologic evaluation including a complete slit lamp examination.
Adam, R. S., Vale, N., Bona, M. D., Hasanee, K., & Farrokhyar, F. (2010). Triaging herpes zoster ophthalmicus patients in the emergency department: do all patients require referral?. Academic Emergency Medicine, 17(11), 1183-1188.
Van Dyk, M., & Meyer, D. (2010). Hutchinson's sign as a marker of ocular involvement in HIV-positive patients with herpes zoster ophthalmicus. SAMJ: South African Medical Journal, 100(3), 172-174.
Category: Geriatrics
Keywords: physical abuse, neglect, identification (PubMed Search)
Posted: 2/5/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Evans CS, et al. Diagnosis of Elder Abuse in U.S. Emergency Departments. J Am Geriatr Soc 65:91–97, 2017
Category: Pharmacology & Therapeutics
Keywords: sepsis, antibiotics, vasopressors, shock (PubMed Search)
Posted: 2/4/2017 by Michelle Hines, PharmD
(Updated: 2/8/2026)
Click here to contact Michelle Hines, PharmD
Below is a list of pharmacy-related pearls from the 2016 Surviving Sepsis Guidelines:
Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016. Crit Care Med 2017; 3. [PMID 28098591]
Follow me on Twitter @mEDPharmD
Category: Critical Care
Keywords: Sepsis, Septic Shock, Fluid resuscitation (PubMed Search)
Posted: 1/31/2017 by Daniel Haase, MD
(Updated: 2/18/2017)
Click here to contact Daniel Haase, MD
At the Society of Critical Care Meeting (SCCM) this month, updates to the Surviving Sepsis Guidelines were released. Recommendations include:
--Initial 30mL/kg crystalloid resuscitation with frequent reassessment of fluid responsiveness using dynamic (not static) measures [goodbye CVP/ScvO2!]
--Initiation of broad-spectrum antibiotics within ONE hour of sepsis recognition [two agents from different classes]
--Further hemodynamic assessement (e.g. echo for cardiac function) if clinical assessment does not reveal the type of shock [get out the ultrasound!]
Rhodes A, Evans LE, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Crit Care Med. 2017 Jan 18.
Category: Visual Diagnosis
Posted: 1/30/2017 by Tu Carol Nguyen, DO
Click here to contact Tu Carol Nguyen, DO
25 year-old female with hx of cerebral palsy with significant developmental delay, s/p G-tube who presented with acute hypoxic respiratory failure, hypotension and a distended, tense abdomen. A CT was done with the scout film below. What's the diagnosis?
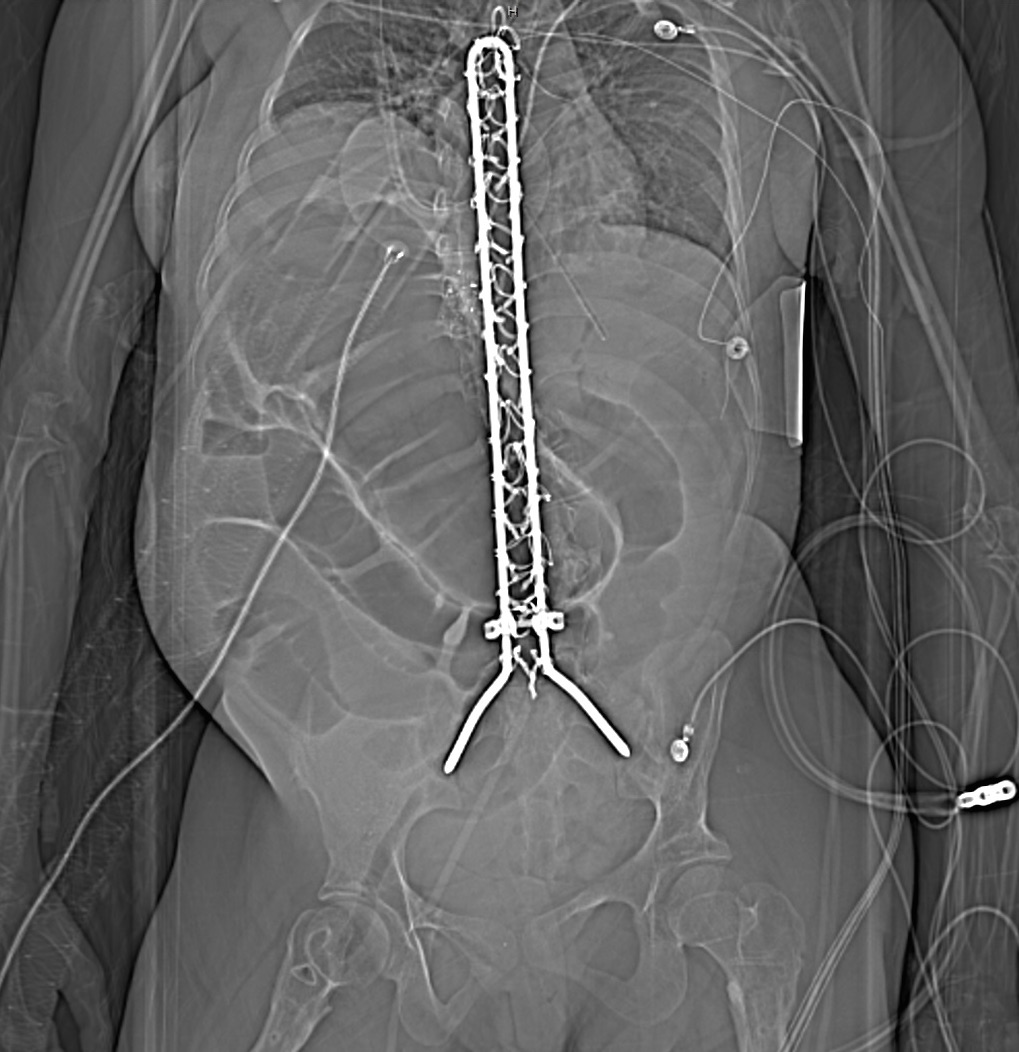
Answer: Cecal Volvulus
Patient was subsequently intubated, had an NG tube placed with over 500cc of fluid returned. Patient had multiorgan failure and received fluids, antibiotics, pressors, blood products and went to the OR, and had a partial bowel resection.
One way to differentiate cecal volvulus from sigmoid volvulus is that sigmoid volvulus generally do not have haustra.
Tonerini M, Pancrazi F, Lorenzi S, Pacciardi F, Ruschi F, et al. (2015) Cecal volvulus: what the radiologist needs to know. Glob Surg, 1: DOI: 10.15761/GOS.1000106.
Category: Orthopedics
Keywords: nerve, entrapment (PubMed Search)
Posted: 1/28/2017 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
During a busy ED shift, your 40yo charge nurse asked you to look at his hand. He is known avid mountain biker. He has pain in his right 4th and 5th digits. . He feels a lack of coordination and a feeling of “clumsiness” of the hand. Where is his possible nerve compression and what do you expect to find on exam?
Ulnar nerve entrapment is sometimes called “handlebar palsy.”
Compression location is Guyon’s canal.
The ulnar nerve supplies the intrinsic muscles of the hand AND the extrinsic muscles for flexion of the 4th and 5th digits. This is what aids in a “power grip” and why he may have diminished grip strength on exam.
Also innervates the ADDuctor pollicis and 1st dorsal interosseous muscles (pinch)
Note the ulnar nerve also passes through the radial tunnel at the elbow. Entrapment here is called Radial tunnel syndrome or Cubital tunnel syndrome and causes forearm pain and paresthesias in the 4th and 5th digits with grossly normal motor and sensory function.
Category: Pediatrics
Keywords: epinephrine, auto-injector (PubMed Search)
Posted: 1/27/2017 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
As a follow up to Dr. Winter’s Pearl on Anaphylaxis on 1/24/2017, here’s a handy pearl for pediatric anaphylaxis (part 1).
Anaphylaxis: rapid and potentially life-threatening involvement of at least 2 systems following exposure to an antigen.
Medications (max: adult doses)
Get it?!?! Easy right? Instead of fumbling through an app or reference card during your next case of pediatric anaphylaxis, be a rock star "EM DR" by remembering the “Rule of 2’s”.
(Can't help it...ya'll know I love my mnemonics!!)
