Category: Neurology
Keywords: seizure, status epilepticus, benzodiazepine, RAMPART, pediatric (PubMed Search)
Posted: 9/13/2017 by WanTsu Wendy Chang, MD
(Updated: 9/14/2017)
Click here to contact WanTsu Wendy Chang, MD
IV vs. Non-IV Benzodiazepines for Cessation of Seizures
Follow me on Twitter @ EM_NCC
Category: Critical Care
Keywords: respiratory failure, pulmonary edema, airway obstruction (PubMed Search)
Posted: 9/12/2017 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Negative-pressure pulmonary edema (NPPE) is a well-documented entity that occurs after a patient makes strong inspiratory effort against a blocked airway. The negative pressure causes hydrostatic edema that can be life-threatening if not recognized, but if treated quickly and appropriately, usually resolves after 24-48 hours. These patients may have any type of airway obstruction, whether due to edema secondary to infection or allergy, laryngospasm, or traumatic disruption of the airway, such as in attempted hangings.
Management:
1. Alleviate or bypass the airway obstruction.
· Usually via intubation; may require a surgical airway
· If obstruction in an intubated patient is due to biting on tube or dyssynchrony, add bite-block (if not already in place), sedation, and even paralysis if needed.
2. Provide positive pressure ventilation and oxygen supplementation.
3. Use low tidal volume ventilation.
4. In severe hypoxemia without shock, add a diuretic agent and consider additional measures such as proning and even ECMO if the hypoxemia is refractory to standard therapy.
Negative-pressure pulmonary edema (NPPE), also called post-obstructive pulmonary edema, can occur after any event in which a patient exerts strong inspiratory effort against an obstructed airway. This obstruction can be essentially due to any cause; in adults it is most well-documented secondary to post-extubation laryngospasm, in children the etiology is usually infectious, such as in epiglottitis. It has also been documented secondary to laryngeal edema, tumor, trauma, biting on an endotracheal tube, vent dyssynchrony, as well as disruptions to breathing mechanics during generalized seizures, among other causes.
It is noted that many of the documented cases involve patients who are relatively young and otherwise healthy, and thus capable of creating a strong negative intrathoracic pressure. The pathophysiology is thought to be related to hydrostatic mechanisms rather than a “leaky-capillary” permeability edema, and it usually resolves quickly if managed appropriately, within 24-48 hours. Diffuse alveolar hemorrhage, related to capillary rupture from the negative pressure, has been documented to occur in severe cases but is rare.
Consider the diagnosis in patients with an appropriate clinical picture or witnessed event leading to abrupt respiratory distress and/or failure. The diagnosis is even more strongly supported if they had absence of respiratory symptoms, or a clear chest x-ray prior to the event, with a chest x-ray demonstrating pulmonary edema afterwards.
Appropriate management of these patients includes:
1. Alleviation or bypass of the upper airway obstruction, which usually requires intubation.
· Depending on the etiology of obstruction (e.g. epiglottitis), endo/nasotracheal intubation may be difficult and a surgical airway may be necessary. Be prepared for this possibility.
· Ventilated patients who develop NPPE may require sedation to prevent biting on the ETT or to promote vent synchrony
2. Provide with positive-pressure ventilation to counteract the negative airway pressures, and oxygen supplementation to decrease pulmonary vascular resistance.
3. Lung-protective ventilation with low tidal volumes is generally accepted as the preferred ventilation strategy in these patients, extrapolated from data regarding its use in acute lung injury.
4. In cases of moderate to severe hypoxemia without the presence of shock, add a diuretic agent.
5. For refractory hypoxemia, consider early utilization of additional therapies, including neuromuscular blockade, proning, and ECMO.
Bhattacharya M, Kallet RJ, Ware LB, Matthay MA. Negative-pressure pulmonary edema. Chest. 2016;150(4):927-33.
Contou D, Voiriot G, Djibre et al. Clinical features of patients with diffuse alveolar hemorrhage due to negative-pressure pulmonary edema. Lung. 2017;195(4):477-487.
Category: Orthopedics
Keywords: Knee OA, injection (PubMed Search)
Posted: 9/9/2017 by Brian Corwell, MD
(Updated: 2/9/2026)
Click here to contact Brian Corwell, MD
Viscosupplementation
Hyaluronic acid (HA) is a high-molecular weight polysaccharide
A major component of synovial fluid and of cartilage
Major role of HA is as a lubricant, shock absorption, antinociceptive effect
Used in veterinary medicine for decades
Multiple brands exist with differences based on the molecular weight and how they are produced
Use supported by the Cochrane database (2007, 2014) for knee OA
Post injection strength gains are due to pain relief
May have a role for those who cannot receive steroid injections
Inject in similar manner to intra articular steroids
Caution in those with known allergy to poultry /eggs
Risks: Local reaction (likely from preservative), injection site pain, infection, bleeding.
Category: Toxicology
Keywords: Radiographs, poisoning (PubMed Search)
Posted: 9/7/2017 by Kathy Prybys, MD
(Updated: 9/8/2017)
Click here to contact Kathy Prybys, MD
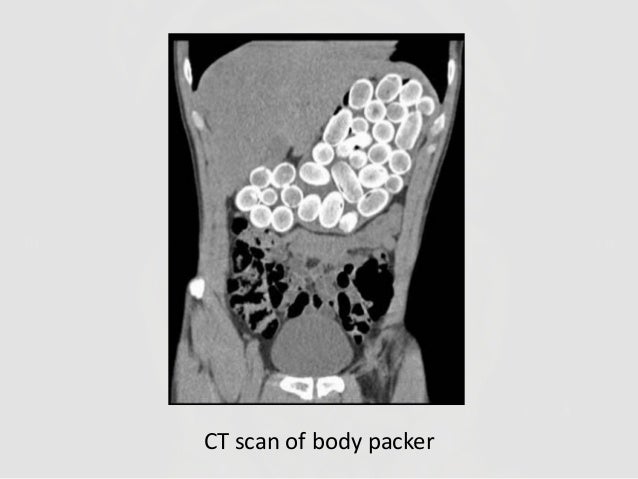
Radiographs studies can be valuable in poisoning diagnosis, management, and prognosis. Radiographic imaging should be utilized for the following toxins:
Container toxins - Body packers
Sustained Released preparations
Plain adominal radiography: a powerful tool to prognosticate outcome in patients with zinc phosphide. Hassanian-Moghaddam H, Shahnazi M, et al. Clin Radiolol. 2014. Oct;69 (10);1062-5.
Systemic Plumbism following remote ballistic injury, Reinboldt M, Franics K, Emerg Radio. 2014 Aug:21 (4): 423-6.
Lead arthropathy: radiographic, CT, and MRI findings, Fernandes JL, Rocha AA, et al. Skeletal Radiol. 2007 Jul;36(7):647-57.
Intentional Intravenous Mercury injection. Yudelowitz G. S Afr Med J. 2017 Jan 30;107(2):112-114.
The role of radiology in diagnosis and management of drug mules: an update with new challenges and new diagnostic tools. Schulz B. Grossbach A, et al. Clin Radiol. 2014 Dec;69(12)
Category: Toxicology
Keywords: fentanyl, first responder exposure (PubMed Search)
Posted: 9/7/2017 by Hong Kim, MD
Click here to contact Hong Kim, MD
There have been reports of “intoxication” or adverse effects among first responders and law enforcement due to exposure to a “powder” suspected to be fentanyl or its analog.
This has led to a significant concern among first responders and law enforcement when investigating or handling “powder” at the scene of overdose or drug enforcement related raids. (http://www.foxnews.com/health/2017/08/15/police-department-gets-hazmat-like-protective-gear-for-overdose-calls.html)
American College of Medical Toxicology and American Association of Clinical Toxicology recently published a position statement to help clarify the potential health risk associated with exposure to fentanyl and its analogs.
Category: International EM
Keywords: Floods, earthquakes, hurricanes, natural disasters (PubMed Search)
Posted: 9/6/2017 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 2/9/2026)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
With the recent destruction by Hurricane Harvey and the impending impact of Hurricane Irma, it is important to recognize the historical death toll from natural disasters. While the list can vary, here is a top ten list from the library of the National Oceanic and Atmospheric Administration:
| Rank | Event | Location | Date | Death Toll (Estimate) |
| 1 | 1931 Yellow River flood | Yellow River, China | Summer 1931 | 850,000-4,000,000 |
| 2 | 1887 Yellow River flood | Yellow River, China | September-October 1887 | 900,000-2,000,000 |
| 3 | 1970 Bhola cyclone | Ganges Delta, East Pakistan | November 13, 1970 | 500,000- 1,000,000 |
| 4 | 1201 Earthquake | Eastern Mediterranean | 1201 | 1,000,000 |
| 5 | 1938 Yellow River flood | Yellow River, China | June 9th, 1938 | 500,000 - 900,000 |
| 6 | Shaanxi Earthquake | Shaanxi Province, China | January 23, 1556 | 830,000 |
| 7 | 2004 Indian Ocean earthquake/tsunami | Indian Ocean | December 26, 2004 | 225,000-275,000 |
| 8 | 1881 Haiphong Cyclone | Haiphong, Vietnam | 1881 | 300,000 |
| 9 | 1642 Kaifeng Flood | Kaifeng, Henan Province, China | 1642 | 300,000 |
| 10 | Tangshan Earthquake | Tangshan, China | July 28, 1976 | 242,000* |
* Official Government figure. Estimated death toll as high as 655,000.
https://docs.lib.noaa.gov/noaa_documents/NOAA_related_docs/death_toll_natural_disasters.pdf
Category: Geriatrics
Keywords: arrhythmia, syncope, fall (PubMed Search)
Posted: 9/4/2017 by Danya Khoujah, MBBS
(Updated: 2/9/2026)
Click here to contact Danya Khoujah, MBBS
20% of unexplained falls in the elderly can be attributed to an arrhythmia.
Bhangu J, McMahon CG, Hall P, et al. Long-term cardiac monitoring in older adults with unexplained falls and syncope. Heart 2016;102:681-686.
Category: Pharmacology & Therapeutics
Keywords: Ureteral stones, Alpha-blockers (PubMed Search)
Posted: 9/2/2017 by Wesley Oliver
(Updated: 2/9/2026)
Click here to contact Wesley Oliver
Alpha-blockers (tamsulosin, alfuzosin, doxazosin, and terazosin) are antagonists of alpha1A-adrenoreceptors, which results in the relaxation of ureteral smooth muscle. Current evidence suggests alpha-blockers may be useful when ureteral stones are 5-10 mm; however, there is no evidence to support the use of alpha-blockers with stones <5 mm. Patients with ureteral stones >10 mm were excluded from studies utilizing these medications.
The size of most ureteral stones will be unknown due to the lack of need for imaging able to measure stone size. Given that the median ureteral stone size is <5 mm, most patients will not benefit from the use of an alpha-blocker.
Also, keep in mind that the data for adverse events with alpha-blockers used for ureteral stones is limited and that these medications have a risk of hypotension.
Ferre RM et al. Tamsulosin for ureteral stones in the emergency department: a randomized, controlled trial. Ann Emerg Med 2009.
77 patients
Ibuprofen + oxycodone + tamsulosin vs. ibuprofen + oxycodone
Stone expulsion at 14 days: Tamsulosin group=77.1% vs. Standard therapy=64.9%
-Difference=12% (95% CI: -8.4-32.8%)
No clinically/statistically significant differences
Pickard R et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet 2015.
1,136 patients
Tamsulosin vs. nifedipine vs. placebo
No further intervention at 4 weeks: Tamsulosin=81% vs. Nifedipine=80% vs. Placebo=80%
No clinically/statistically significant differences
Furyk JS et al. Distal ureteric stones and tamsulosin: a double-blind, placebo-controlled, randomized, multicenter trial. Ann Emerg Med 2016.
403 patients
Tamsulosin vs. placebo
Stone passage at 28 days: Tamsulosin=87% vs. Placebo=81.9%
-Difference=5% (95% CI: -3-13%)
Found difference in subgroup analysis of large stones (5-10 mm)
-Tamsulosin=83.3% vs. Placebo=61%
-Difference=22.4% (95% CI: 3.1-41.6%)
No other clinically/statistically significant differences
Hollingsworth JM et al. Alpha blockers for treatment of ureteric stones: systematic review and meta-analysis. BMJ 2016.
Meta-analysis of 55 trials
No benefit in patients with smaller stones (<5 mm): RR=1.19 (95% CI: 1.00-1.98)
Benefit in patients with larger stones (5-10 mm): RR=1.57 (95% CI: 1.39-1.61)
1.) Ferre RM, Wasielewski JN, Strout TD, Perron AD. Tamsulosin for ureteral stones in the emergency department: a randomized, controlled trial. Ann Emerg Med 2009;54:432-9.
2.) Furyk JS, Chu K, Banks C, et al. Distal ureteric stones and tamsulosin: a double-blind, placebo-controlled, randomized, multicenter trial. Ann Emerg Med 2016;67:86-95.
3.) Hollingsworth JM, Canales BK, Rogers MAM, et al. Alpha blockers for treatment of ureteric stones: systematic review and meta-analysis. BMJ 2016;355:i6112.
4.) Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet 2015;386:341-9.
Category: Pediatrics
Keywords: VTE, Thrombophilia, Enoxaparin, Children, Thromboembolism (PubMed Search)
Posted: 9/1/2017 by Megan Cobb, MD
Click here to contact Megan Cobb, MD
Background:
There is an increased incidence of venous thromboembolic events (VTE) in pediatrics due to improved diagnosis and survival of children with VTE.
The mortality rate is estimated at 2%.
The most common etiologies vary by age - Central venous catheters in neonates and infants, and inherited thrombophilia in children and adolescents.
Learning Points:
With neonates and infants, carefully assess medical history from neonatal period. Umbilical lines? PICC? Broviac? History of these is likely to be the cause.
In children and adolescents, unprovoked VTE is most likely due to inherited thrombophilia, and can be DVT, PE, Portal venous thrombus, etc.
Antithrombin deficiency: The first discovered inherited thrombophilia. The result is a lack of inhibition of coagulation factors – IIa, IXa, Xa, XIIa.
Protein C or/and S deficiency: The result is lack of inhibition of activated Factor V.
Factor V Leiden: Most common inherited thrombophilic defect. Resultant activated Factor V is resistant to normal Protein C and S activity.
Prothrombin Mutation: Second most common inherited thrombophilia. The result is increased levels of prothrombin, which increases the half-life of factor Va.
Initial treatment of clinically significant VTE can start with enoxaparin (1-1.5 mg/kg q12-24h, while checking Anti-Xa levels 4 hours after administration for therapeutic dosing.)
Pearl: Testing for thrombophilia is not always appropriate when diagnosing pediatric patients with their first VTE, but in children and adolescents with first diagnosed, unprovoked VTE, it is worthwhile to send off the initial hypercoaguability work up as this can affect the duration of treatment and need for testing or evaluation. Enoxaparin is a recommended medication to start therapeutic treatment of VTE, even in pediatric patients.
Van Ommen CH, Nowak-Gottl U. Inherited Thrombophilia in Pediatric Venous Thromboembolic Disease: Why and Who to Treat. Frontiers in Pediatrics. 2017: 5(20).
The Harriet Lane Handbook, 20th edition. Chapter 29: Drug Dosages. 2015
Category: Toxicology
Keywords: Botulinum, Dimethylmercury, VX, Tetrodotoxin (PubMed Search)
Posted: 8/17/2017 by Kathy Prybys, MD
(Updated: 8/31/2017)
Click here to contact Kathy Prybys, MD
VX ("venomous agent X")
LD50 expresses the dose at which 50% of exposed population will die as a result of exposure.
Category: Critical Care
Keywords: Mechanical ventilation, sedation (PubMed Search)
Posted: 8/30/2017 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Background: Sedation and analgesia are key components for mechanically ventilated patients. While significant data exists regarding how to manage sedation and analgesia in the ICU setting, very little data exists on management in the ED.
Data: A prospective, single-center, observational study of mechanically-ventilated adult patients used linear regression to identify ED sedation practices and outcomes, with a focus on sedation characteristics using the Richmond Agitation-Sedation Scale (RASS).
Findings:
Bottom line: Avoid early deep sedation in your intubated patients as this may be directly associated with increased mortality. Instead, a goal RASS of 0 to -2 should be appropriate for most non-paralyzed, mechanically-ventilated ED patients, extrapoloating from ICU guidelines.
Stephens, R.J., et al., Analgosedation Practices and the Impact of Sedation Depth on Clinical Outcomes Among Patients Requiring Mechanical Ventilation in the ED: A Cohort Study. Chest, 2017 [Epub ahead of print].
Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, Davidson JE, Devlin JW, Kress JP, Joffe AM, et al.; American College of Critical Care Medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013;41:263–306.
Category: Orthopedics
Keywords: Concussion recovery (PubMed Search)
Posted: 8/26/2017 by Brian Corwell, MD
(Updated: 2/9/2026)
Click here to contact Brian Corwell, MD
There is tremendous interest in identifying factors that may influence outcome from sports related concussion.
The strongest predictor of slower recovery is the severity of symptoms in the 1-2 days post injury
-Fewer Sx's in this time period predict a quicker recovery
Pre injury history of mental health problems, depression or migraine headaches predict a longer recovery course
Teenagers might be more vulnerable to having persistent symptoms with greater risk for girls than boys
Having a prior concussion is a risk for having a future concussion
The large majority of injured athletes recover from a clinical perspective within the first month of injury many within the first 10 days
McCrory P et al. Br J Sports Med 2017;51:838-847.
Category: Pediatrics
Keywords: allergic reaction, anaphylaxis, auto-injector, epi-pen (PubMed Search)
Posted: 1/27/2017 by Mimi Lu, MD
(Updated: 8/25/2017)
Click here to contact Mimi Lu, MD
Anaphylaxis is a life threatening emergency with mortality of up to 2% [1]. Early recognition is imperative and administration of timely Epinephrine is the single most important intervention [2]. While providers may be hesitant to administer epinephrine in older patients due to fear of precipitating adverse cardiovascular events, they may also hesitate in younger patients due to fear of overdose.
Iimmediate administration with any dose available is recommended because:
Bottom line:
There are no absolute contraindications (including age) for epinephrine in patients with anaphylaxis. Give the initial dose IM into the anterolateral thigh.
1- Bock SA, Muñoz-Furlong A, Sampson HA. Fatalities due to anaphylactic reactions to foods. J Allergy Clin Immunol. 2001 Jan. 107(1):191-3. [Medline].
4- Wood JP, Traub SJ, Lipinski C. Safety of epinephrine for anaphylaxis in the emergency setting. World Journal of Emergency Medicine. 2013;4(4):245-251. doi:10.5847/wjem.j.issn.1920-
Category: Toxicology
Keywords: dabigatran reversal, Idarucizumab (PubMed Search)
Posted: 8/25/2017 by Hong Kim, MD
Click here to contact Hong Kim, MD
Full cohort analysis idarucizumab for dabigatran associated bleeding was recently published in NEJM.
This study evaluated the laboratory correction of elevated ecarin clotting time or diluted thrombin time induced by dabigatran and time to either cessation of bleeding (Group A: patients with GI bleeding, traumatic bleeding, or ICH) or time to surgery (Group B: patients requiring surgical intervention within 8 hours).
Findings
Group A (n=301): Median time to the cessation of bleeding was 2.5 hours in 134 patients.
HOWEVER:
Group B (n=202): Median time to intended surgery after infusion of idarucizumab was 1.6 hours.
Laboratory markers:
100% reversal of abnormal ecarin clotting time or diluted thrombin time within 4 hours after the administration
Mortality
Conclusion
Authors concluded thate idaurcizumab is an "effective" reversal agent for dabigatran.
Overall, the findings are more promising compared to the interim analysis that was published in 2015.
Other findings:
Infusion of idarucizumab decreased the dabigatran level from 110 ng/mL (Group A) and 73.6 ng/mL (Group B) to < 20 ng/mL.
Rebound levels of > 20 ng/mL were noted in 191 patients after 12 – 24 hours after idarucizumab adminiatration
Thrombotic events occured in 24 patients (14 in Group A and 10 in Group B) within 30 days after treatment
Serious adverse events occured in 23.3% of the patients within 5 days.
Most frequent events were:
Pollack CV et al. Idarucizumab for dabigatran reversal - full cohort analysis. N Eng J Med 2017;377:431-41.
Category: Neurology
Keywords: meningitis, CSF, glucose, glucometer (PubMed Search)
Posted: 8/24/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Category: Critical Care
Posted: 8/22/2017 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Hyponatremic Encephalopathy
Archinger SG, Ayus JC. Treatment of hyponatremic encephalopathy in the critically ill. Crit Care Med. 2017; epub ahead of print.
Category: Pediatrics
Keywords: Febrile seizure, meningitis (PubMed Search)
Posted: 8/18/2017 by Jenny Guyther, MD
(Updated: 2/9/2026)
Click here to contact Jenny Guyther, MD
Febrile seizures occur in children 6 months through 5 year olds. A complex febrile seizure occurs when the seizure is focal, prolonged (> 15 min), or occurs more than once in 24 hours.
The prevalence of bacterial meningitis in children with fever and seizure after the H flu and Strep pneumomoniae vaccine was introduced is 0.6% to 0.8%. The prevalence of bacterial meningitis is 5x higher after a complex than simple seizure.
From the study referenced, those children with complex febrile seizures who had meningitis all had clinical exam findings suggestive of meningitis. More studies are needed to provide definitive guidelines about when lumbar punctures are needed in these patients.
This study was a retrospective review of children aged 6 months to 5 years who had complex febrile seizures in France between 2007-2011.
Children were excluded if they had a simple febrile seizure, history of non-febrile seizure, conditions associated with a higher risk of seizure (cerebral malformations, genetic syndrome, trauma in the previous 24 hours) or predisposing to bacterial meningitis (sickle cell, cancer, immunosuppressive treatments). Outcomes were the diagnosis of bacterial or HSV meningitis at 7 days
The rate of bacterial meningitis was 0.7% (CI 0.2-1.6). There were no cases of HSV meningitis.
69% of the study patients did not have a lumbar puncture, however, follow up was done by repeat exam, phone and review of the meningitis and also death registry if the patient was lost to follow up.
The clinical exam in the 5 children with bacterial meningitis was suggestive of meningitis (irritability, altered mental status, bulging fontanel). In a subgroup of patients without physical exam findings suggestive of meningitis, there were no cases of bacterial meningitis.
Guedji R et al. Do All Children Who Present With a Complex Febrile Seizure Need a Lumbar Puncture? Annals of Emergency Medicine. 2017; 70 (1):52-62.
Category: International EM
Keywords: suicide, clinical policies, risk-assessment tools (PubMed Search)
Posted: 8/11/2017 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 8/16/2017)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
In patients presenting to the ED with suicidal ideation, physicians should not use currently available risk-assessment tools in isolation to identify low-risk patients who are safe for discharge. The best approach to determine risk is an appropriate psychiatric assessment and good clinical judgment, taking patient, family, and community factors into account. (Level C Recommendation, based upon the quality of the research.)
As noted in a previous Pearl (see August 2, 2017), the American College of Emergency Physicians recently published a methodological rigorous clinical policy entitled “Critical Issues in the Diagnosis and Management of the Adult Psychiatric Patient in the Emergency Department.”
Another question addressed within the document was the following: “In the adult patient presenting to the ED with suicidal ideation, can risk-assessment tools in the ED identify those who are safe for discharge?”
They determined that in patients presenting to the ED with suicidal ideation, physicians should not use currently available risk-assessment tools in isolation to identify low-risk patients who are safe for discharge. The best approach to determine risk is an appropriate psychiatric assessment and good clinical judgment, taking patient, family, and community factors into account. (Level C Recommendation, based upon the quality of the research.)
http://www.annemergmed.com/article/S0196-0644(17)30070-7/fulltext
Category: Critical Care
Keywords: autoimmune, rheumatology, thrombosis, hematology (PubMed Search)
Posted: 8/15/2017 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Catastrophic Antiphospholipid Syndrome (CAPS):
A life-threatening “thrombotic storm” of multi-organ micro & macro thrombosis in patients with antiphospholipid syndrome (known or unknown).
Triggered circulating antibodies (usually by infection, but can be prompted by malignancy, pregnancy, and lupus itself) cause endothelial disruption and inflammation leading to prothrombotic state, commonly with SIRS response.
Mortality is high at an estimated 40%.
Confirm diagnosis with antiphospholipid antibody titers.
Treat ASAP with unfractionated heparin, corticosteroids, and Hematology consultation for plasma exchange and/or IVIG.
Kazzaz NM, McCune WJ, Knight JS. Treatment of catastrophic antiphospholipid syndrome. Curr Opin Rheumatol. 2016;28(3):218-27.
Cervera R, Rodriguez-Pinto I, Colafrancesco S, et al. 14th International Congress on Antiphospholipid Antibodies Task Force. Report on catastrophic antiphospholipid syndrome. Autoimmun Rev 2014; 13:699–707.
Category: Neurology
Keywords: pituitary apoplexy, subarachnoid hemorrhage, meningitis, headache, CT, MRI (PubMed Search)
Posted: 8/9/2017 by Danya Khoujah, MBBS
(Updated: 2/9/2026)
Click here to contact Danya Khoujah, MBBS
Bottomline: Keep pituitary apoplexy in your differential when considering SAH or meningitis, especially in the presence of risk factors, and have a low threshold to order an MRI.
