Category: Neurology
Keywords: drug reaction, toxicity, neurotoxicity, antibiotics (PubMed Search)
Posted: 11/10/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Recognition of antibiotic associated neurotoxicity reduces unnecessary workup and serious adverse effects.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: burr hole, trephination, subdural hematoma, epidural hematoma, herniation (PubMed Search)
Posted: 10/13/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Your patient presents with a large traumatic subdural hematoma with midline shift and clinical evidence of herniation. Your nearest neurosurgeon is several hours away, what do you do?
Initial resuscitation should follow ATLS. Treatment of intracranial hypertension and herniation includes elevating the head of bed, administering osmotic therapies, optimizing analgesia/sedation, and hyperventilation. If all measures have been exhausted and there is a delay to definitive neurosurgical intervention, an emergency department burr hole may be considered.
Indications:
Contraindications:
Equipment:
Transtemporal Approach:
Additional Points:
Follow us on Twitter @christinap0well @EM_NCC
Category: Neurology
Keywords: stroke, large vessel occlusion, basilar artery, posterior circulation, thrombectomy (PubMed Search)
Posted: 6/9/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: There is no significant difference between endovascular thrombectomy and medical management for basilar artery occlusion strokes within 6 hours of symptom onset.
Category: Neurology
Keywords: Lumbar puncture, LP, post-dural, headache, intracranial hypotension (PubMed Search)
Posted: 5/12/2021 by WanTsu Wendy Chang, MD
(Updated: 2/7/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The use of atraumatic needles is most effective in reducing the risk of post-LP headaches. These needles are easy to use and have similar rate of success as cutting needles.
Cognat E, Koehl B, Lilamand M, et al. Preventing post-lumbar puncture headache. Ann Emerg Med. 2021 May 6;S0196-0644(21)00151-7. Online ahead of print.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: functional neurological disorder, FND, stroke mimic, non-epileptic seizure (PubMed Search)
Posted: 4/28/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Functional neurological disorders (FND) are commonly encountered in the ED. A thorough neurological exam may reveal positive signs suggestive of FND. Early diagnosis and referral to specialists may improve outcomes.
Finkelstein SA, Cortel-LeBlanc MA, Cortel-LeBlanc A, Stone J. Functional neurological disorder in the emergency department. Acad Emerg Med. 2021 Apr 18 [Online ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: acute ischemic stroke, alteplase, tPA, thrombolysis, error (PubMed Search)
Posted: 4/15/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Alteplase administration in acute ischemic stroke is associated with errors, most commonly with over-dosage of the medication.
Dancsecs KA, Nestor M, Bailey A, Hess E, Metts E, Cook AM. Identifying errors and safety considerations in patients undergoing thrombolysis for acute ischemic stroke. Am J Emerg Med. 2021;47:90-94.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Idiopathic intracranial hypertension, IIH, pseudotumor cerebri, obesity, healthcare utilization (PubMed Search)
Posted: 3/10/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The incidence and prevalence of IIH is increasing, likely related to rising rate of obesity. This has also been associated with more healthcare utilization compared to the general population.
Category: Neurology
Keywords: Bell's palsy, facial palsy, Lyme disease, Borrelia burgdorferi (PubMed Search)
Posted: 2/24/2021 by WanTsu Wendy Chang, MD
(Updated: 2/7/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: In a Lyme-endemic area, the incidence of positive Lyme tests and Bell’s palsy are highest in the Lyme months. This seasonal variation may help guide the management of patients with Bell’s palsy.
Pacheco A, Rutler O, Valenzuela I, Feldman D, Eskin B, Allegra JR. Positive tests for Lyme disease and emergency department visits for Bell’s Palsy patients. J Emerg Med. 2020;59(6):820-827.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: seizure, status epilepticus, nonconvulsive, electrographic, EEG (PubMed Search)
Posted: 1/27/2021 by WanTsu Wendy Chang, MD
(Updated: 2/7/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Persistent or recurrent seizures are not uncommon in the first 24 hours after status epilepticus even in patients with resolved clinical seizure activity. Early use of EEG can help identify patients who need further escalation of treatment.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: stroke, thrombolysis, tissue plasminogen activator, tPA, monitoring (PubMed Search)
Posted: 1/13/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
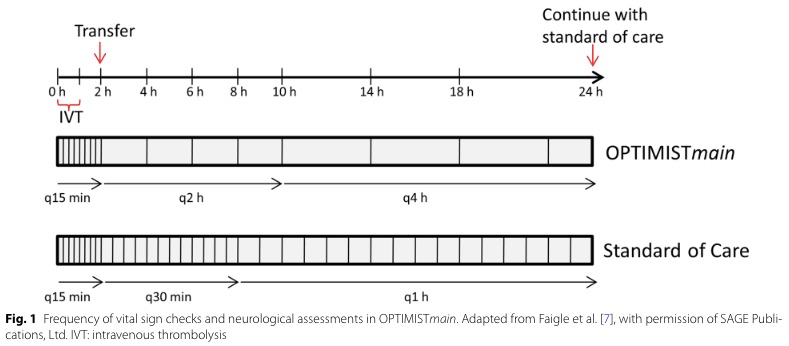
Bottom Line: Patients with NIHSS <10 may be safe for low-intensity post-tPA monitoring if they do not require critical care after an initial period of q15 min standard monitoring for the first 2 hours.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: acute ischemic stroke, guideline, metric, English, non-English (PubMed Search)
Posted: 12/9/2020 by WanTsu Wendy Chang, MD
(Updated: 12/10/2020)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Patients' language preference does not appear to affect the efficiency of acute ischemic stroke care, especially at experienced high volume stroke centers.
Zachrison KS, Natsui S, Luan Erfe BM, et al. Language preference does not influence stroke patients' symptom recognition or emergency care time metrics. Am J Emerg Med. 2020 Nov 2 [Online ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: migraine, headache, diagnosis, treatment, prevention (PubMed Search)
Posted: 11/11/2020 by WanTsu Wendy Chang, MD
(Updated: 11/13/2020)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Migraine is a common and debilitating condition that benefits from early treatment. Consider initiating preventive therapy for patients who experience at least 2 migraine days per month and adverse effects despite treatment.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: CNS, PNS, UMN, LMN, reflex, Babinski, tone (PubMed Search)
Posted: 10/14/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
| Central Nervous System | Peripheral Nervous System | |
| Pattern of Symptoms | • Hemibody involvement • Weakness of UE extensors • Weakness of LE flexors | • Distal involvement in polyneuropathy • Distal and proximal involvement in polyradiculoneuropathy • Proximal involvement in polyradiculopathy • Sensory often precedes motor symptoms • Pure proximal>distal weakness may be due to myopathy or NMJ disorder |
| Sensory Symptoms | • Central poststroke pain (hyperalgesia, allodynia) • Sensory level in spinal cord pathology • Proprioception involved early in dorsal column disorders | • Neuropathic pain (burning, tingling, shock-like) • Ascending sensory loss involving distal BLE>BUE in polyneuropathy • Proprioception involved late in polyneuropathy |
| Reflexes | • Hyperreflexia in affected limb(s) after acute period • Positive Babinski’s sign | • Hyporeflexia in affected limb(s) |
| Tone | • Increased after acute period | • Decreased |
Category: Neurology
Keywords: cerebral venous thrombosis, CVT, symptoms, treatment, endovascular (PubMed Search)
Posted: 9/23/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Severity of CVT presentation depends on the location and clot burden. Anticoagulation is key, though consider endovascular intervention if patient does not improve or deteriorates despite anticoagulation.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: cerebral venous thrombosis, CVT, prothrombotic, headache (PubMed Search)
Posted: 9/10/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The incidence of CVT is increasing with rate of increase higher in males and older females. Consider CVT beyond traditional risk factors.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: trigeminal neuralgia, TN, tic douloureux, neuropathic facial pain (PubMed Search)
Posted: 8/26/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: New onset trigeminal neuralgia needs workup for its etiology. Carbamazepine and oxcarbazepine can be effective for symptom management though continuous or long-lasting pain exacerbations are difficult to treat.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: cerebrospinal fluid, rhinorrhea, otorrhea, halo, double ring, beta-2 transferrin (PubMed Search)
Posted: 8/12/2020 by WanTsu Wendy Chang, MD
(Updated: 2/7/2026)
Click here to contact WanTsu Wendy Chang, MD
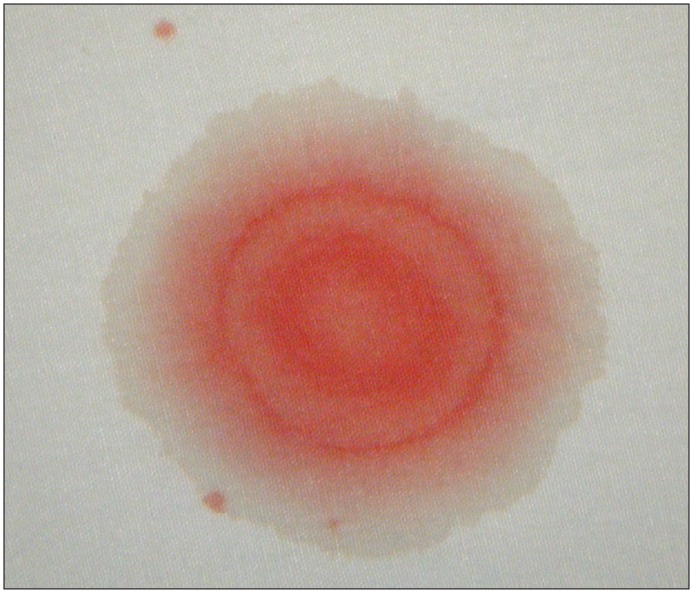
Bottom Line: Beta-2 transferrin is more accurate than the halo sign to identify CSF containing fluid.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: idiopathic intracranial hypertension, papilledema, intracranial pressure, cranial nerve palsy (PubMed Search)
Posted: 7/8/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Idiopathic intracranial hypertension (IIH) is a vision-threatening illness with significant morbidity and needs to be considered as a possible headache diagnosis in the ED. Most often, this occurs in women of childbearing age with a BMI >30, but atypical varieties exist.
Symptoms: Headache (90%), visual disturbance, pulsatile tinnitus, horizotal diplopia.
Signs: Papilledema, 6th cranial nerve (abducens) palsy.
Evaluation: Neuroimaging including CTV or MRV to identify alternate cause including cerebral venous outflow obstruction, lumbar puncture with opening pressure >30 cmH2O (25-30 cmH2O is gray zone), blood work per clinical presentation, CSF analysis.
Treatment: No clear consensus, but typically acetazolamide. Severe or refractory symptoms may require surgical intervention such as optic nerve sheath fenestration, VP shunt, venous sinus stenting.
Hoffmann J, Mollan SP, Paemeleire K, et al. European Headache Federation guideline on idiopathic intracranial hypertension. J Headache Pain. 2018;19(1):93.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: pregnancy, postpartum, migraine, RCVS, CVT, Bell's Palsy, facial palsy (PubMed Search)
Posted: 6/10/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Pregnancy is associated with an increased risk for RCVS, CVT, and Bell’s Palsy. Pregnancy also affects the frequency of migraines due to hormonal fluctuations.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: traumatic brain injury, clinical decision rule, CT utilization, patient decision, benefit, risk, financial incentive (PubMed Search)
Posted: 5/14/2020 by WanTsu Wendy Chang, MD
(Updated: 2/7/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Discussion of benefit/risk and financial incentive associated with head CT in mild TBI affects patient decision. Interestingly in this population studied, more than half of patients will elect to obtain a head CT even in a low-risk scenario.
Iyengar R, Winkels JL, Smith CM, et al. The effect of financial incentives on patient decisions to undergo low-value head CT scans. Acad Emerg Med. 2019;26(10):1118-24.
Follow me on Twitter @EM_NCC
