Category: Vascular
Keywords: popliteal artery injury review (PubMed Search)
Posted: 2/4/2026 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Popliteal artery injuries are very rare (4% of all vascular injuries).
The majority of injuries are secondary to penetrating injury (70+%)
Blunt mechanism of injury has the higher rate of amputation.
Prolonged ischemia time (from injury to repair greater than 6 hours) leads to higher rates of amputation
Hard signs of vascular injury should prompt X-ray imaging of the knee, femur, and lower extremity and transfer to an operating room for repair.
Soft signs ("a history of significant bleeding which has ceased, nonexpanding hematomas, and the presence of an Ankle-Brachial Index of less than 0.9") and shotgun injury should prompt CT angiogram to evaluate arterial injury.
Asensio, Juan A. MD, PhD, DABS, FACS, FCCM, FRCS (England), FSVS, FAIM, FISS, KM; Ceron, Santiago A. MD; Inyang, Ime D. BA; Johnson, Sarah E. DHSc, MS; Williams, Mallory MD, MPH, FACS, FICS, FCCP, FCCM; Velasco, Jose M. MD, FACS, FCCM. Popliteal artery injuries: What you need to know. Journal of Trauma and Acute Care Surgery 100(2):p 162-172, February 2026. | DOI: 10.1097/TA.0000000000004752
Category: Trauma
Keywords: ICh, risk factor head injury, geriatric (PubMed Search)
Posted: 2/4/2026 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
In a metanalysis of studies looking at intercranial hemorrhage in fall patients older than 65 years, the following were unadjusted odds ratio risk factors for finding an ICH in this patient population:
suspected open or depressed skull fracture , signs of basal skull fracture ), reduced baseline Glasgow Coma Scale score , focal neurologic signs , seizure , vomiting , amnesia , loss of consciousness , headache ), external sign of head trauma , male sex , chronic kidney disease , preinjury single antiplatelet , and dual antiplatelet medication .
Preinjury anticoagulant was not a significant risk factor.
When looking at adjusted odds rations only focal neurologic signs , external sign of head trauma , loss of consciousness , and male sex were found to be associated with intercranial hemorrhage.
Dubucs, Xavier et al.
Annals of Emergency Medicine, Volume 87, Issue 2, 181 - 191
Category: Toxicology
Keywords: medetomadine, withdrawal (PubMed Search)
Posted: 2/4/2026 by Robert Flint, MD
(Updated: 2/5/2026)
Click here to contact Robert Flint, MD
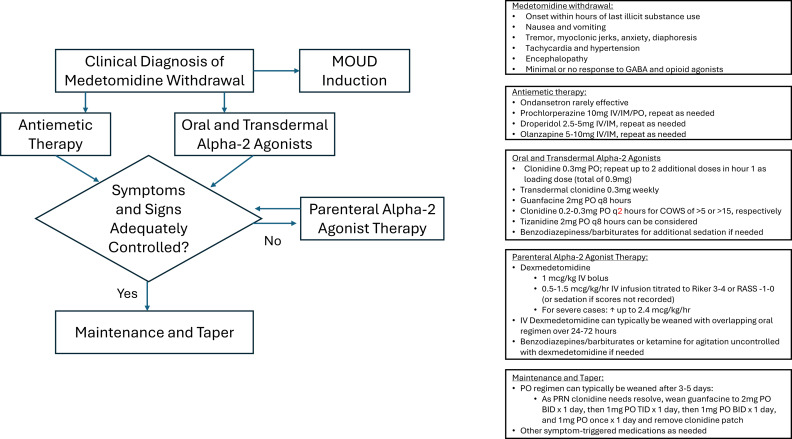
The US drug supply has been found to contain medetomidine as an adulterant to heroine/fentanyl. It is a potent tranquilizer used in animals. It is an alpha 2 blocker (similar pharmacology to clonidine and xylazine). Exposure to this drug can induce withdrawal symptoms to include anxiety, tremor, diaphoresis, nausea, vomiting, agitation, sympathetic hyperactivity, and delirium. Withdrawal can start within 4-6 hours of last use.
Treatment for withdrawal is outlined in this diagram.
Category: Toxicology
Keywords: toxins, misperceived for edible, food containers (PubMed Search)
Posted: 2/4/2026 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD

Poisonings due to storage in a secondary container reported to the National Poison Data System, 2007–2017. Carpenter J., Murray B. et al., Clinical Toxicology, 2021.59(6), 521–527.
Poisoning following exposure to chemicals stored in mislabelled or unlabelled containers: a recipe for potential disaster. Millard YC, Slaughter RL, et al. New Zealand Med J. 26 September 2014, Vol 127 No 1403.
Unintentional poisoning from decanted toxic household chemicals. Von Fabeck K, Boulamery A, et al. Clin Toxicol (Phila). 2023 Mar;61(3):186-189.
Antifreeze on a freezing morning: ethylene glycol poisoning in a 2-year-old. Hann G, Duncan D, et al. BMJ Case Rep. 2012 Mar
Epidemiology of Accidental Poisoning Caused by Storage of Non-Food Substances in Food Containers and unmarked Bottles/Containers. Geller RJ, Kezirian R, Bangar P, Strong D, Carlson T. Children’s Hospital Central California; California Poison Control System (CPCS). https://www.tandfonline.com/doi/pdf/10.1080/15563650903076924
Category: Critical Care
Posted: 2/2/2026 by Jessica Downing, MD
(Updated: 2/8/2026)
Click here to contact Jessica Downing, MD
Etomidate is often a go-to agent for RSI because it is considered relatively hemodynamically neutral. However, lab studies have shown an association with transient adrenal suppression, and some observational studies and meta-analyses have suggested that patients intubated with etomidate face higher risk of cardiovascular collapse and in-hospital mortality than those intubated with ketamine.
The RSI trial was a pragmatic open-label multi-center randomized control trial conducted in 6 EDs and 8 ICUs across the US and compared induction with ketamine 1-2mg/kg versus etomidate 0.2-0.3mg/kg for RSI of critically ill adults (excluding trauma patients). They found no significant difference in overall 28 day hospital mortality across the cohort. They found an increased risk of cardiovascular collapse during intubation in the ketamine group. This increased risk was more pronounced in patients with sepsis or septic shock and patients with APACHE II ?20.
Some details:
Overall - this was a well conducted randomized control trial that - at the very least - suggests that etomidate is likely as safe (if not safer) than ketamine with respect to 28d mortality and peri-intubation cardiovascular collapse, even among patients with critical illness or septic shock.
Casey JD, Seitz KP, Driver BE, Gibbs KW, Ginde AA, Trent SA, Russell DW, Muhs AL, Prekker ME, Gaillard JP, Resnick-Ault D, Stewart LJ, Whitson MR, DeMasi SC, Robinson AE, Palakshappa JA, Aggarwal NR, Brainard JC, Douin DJ, Marvi TK, Scott BK, Alber SM, Lyle C, Gandotra S, Van Schaik GW, Lacy AJ, Sherlin KC, Erickson HL, Cain JM, Redman B, Beach LL, Gould B, McIntosh J, Lewis AA, Lloyd BD, Israel TL, Imhoff B, Wang L, Spicer AB, Churpek MM, Rice TW, Self WH, Han JH, Semler MW; RSI Investigators and the Pragmatic Critical Care Research Group. Ketamine or Etomidate for Tracheal Intubation of Critically Ill Adults. N Engl J Med. 2025 Dec 9:10.1056/NEJMoa2511420. doi: 10.1056/NEJMoa2511420. Epub ahead of print. PMID: 41369227; PMCID: PMC12711137.
Category: Ultrasound
Keywords: POCUS, resident education, ultrasound guided nerve blocks (PubMed Search)
Posted: 2/1/2026 by Alexis Salerno Rubeling, MD
(Updated: 2/2/2026)
Click here to contact Alexis Salerno Rubeling, MD
Ultrasound Guided Nerve Blocks (UGNBs) provides targeted analgesia that can effectively alleviate pain from injuries or painful procedures while reducing opioid use.
In 2021, ACEP issued a policy statement affirming that ultrasound-guided regional anesthesia is within the scope of EM physicians and is a core component of multimodal pain management pathways in the ED. However, EM residencies have not uniformly defined nerve block requirements, resulting in a wide range of graduating resident skill levels. Recent ACGME updates may help standardize expectations and address this gap.
A recent review of the National Ultrasound-Guided Nerve Block Registry (NURVE) looked at the impact of operator training level on the analgesic effectiveness of ED-performed UGNBs. The most commonly performed block among attendings was the erector spinae block, while for residents it was the fascia iliaca block. Both resident and attending performed blocks showed a reduction in pain but there was an 80.7% meaningful pain reduction in attendings as compared to 63.4% for residents. Out of the 1595 nerve block cases reviewed there were only 2 complications which included transient episode of LAST and respiratory difficulty from suspected diaphragmatic hemiparesis.
These findings highlight the importance of experience while supporting the safety and effectiveness of UGNBs performed by supervised residents in the training environment.
Macias M, Driver L, Riscinti M, Dreyfuss A, et al. Training level and analgesic outcomes of ultrasound-guided nerve blocks in the emergency department: An analysis from the NURVE block registry, The American Journal of Emergency Medicine, 2026 doi.org/10.1016/j.ajem.2026.01.050.
Category: Trauma
Keywords: Hypothermia, fall, height, injury (PubMed Search)
Posted: 1/31/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
An English study describes 30 patients that jumped from a single bridge of 30 meters (98 feet) over the course of 12 years. Twenty six landed in the water. The injury pattern for those landing in water was described as “Hypothermia was the most common presentation (n = 23), followed by pneumothoraces (n = 14), rib fractures (n = 10), thoracic vertebral fractures (n = 9) and lung contusions (n = 8). Lower water temperatures at the time of the incident (p = 0.008) and lower patient body temperatures on arrival to hospital (p = 0.002) were significantly associated with increased 30-day mortality.”
The small group landing on land had more pelvic and extremity fractures than the water group and none had hypothermia.
Remember to start aggressive rewarming in patients who fall into water!
Harvey T, Nottingham T, Owen P, Hannah J, Plumb J. Injury patterns and clinical outcomes following falls from a medium-height bridge: A retrospective study. Trauma. 2025;28(1):44-53. doi:10.1177/14604086251404739
Category: Trauma
Keywords: Stab wound, chest radiograph, pneumothorax (PubMed Search)
Posted: 1/31/2026 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This small study from South Africa shows stab wounds to the chest with a pneumothorax less than 0.5 cm that were managed conservatively had completely resolved on 12 hour repeat chest X-ray. This could facilitate earlier discharge of these patients. It also supports conservative (non-tube placement) approach to asymptomatic small pneumothoraces from stab wounds.
Kong V, Cheung C, Lee D, et al. Defining the optimal timing of interval chest radiograph in conservatively managed small pneumothorax from thoracic stab wounds – a South African experience. Trauma. 2025;28(1):14-17. doi:10.1177/14604086251396434
Category: Geriatrics
Keywords: Tramadol, geriatrics (PubMed Search)
Posted: 1/29/2026 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Tramadol has been viewed as a safer alternative for pain control than opioids. This study says differently.
“Tramadol use was associated with increased risk of multiple ER utilizations, falls/fractures, CVD hospitalizations, safety event hospitalizations, and mortality (new users only) compared to nonuse.”
Musich S, Wang SS, Schaeffer JA, Slindee L, Kraemer S, Yeh CS. Safety Events Associated with Tramadol Use Among Older Adults with Osteoarthritis. Popul Health Manag. 2021 Feb;24(1):122-132. doi: 10.1089/pop.2019.0220. Epub 2020
Category: Administration
Keywords: Communication, Teamwork (PubMed Search)
Posted: 1/28/2026 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
How well does your ED care team communicate? For some high yield strategies and reasons for improvement, read on…
To explore effective and ineffective communication in the ED and its impact of patient care, physician and nurses from several academic EDs completed an online anonymous survey, then attended focus group sessions. Responses highlighted the following themes:
1: Situations, built physical environment, and medium of communications all impact quality of communication.
2: Core elements of desired professional communication include respect, closed-loop communication, and attention, often conveyed through non-verbal behaviors.
3: Poor communication begets poor communication in later interactions
4: Effective communication is seen as fundamental to patient care but also has impacts beyond patient care
5: Clinician gender and gender dyads influence communication dynamics, age and experience dyads did not.
Do any of these themes resonate with you? What can you do within your department to improve physician-nurse communication and the care you provide?
Jones DC, Phillips J, Graveson A, et al. Emergency Physician and Emergency Nurse Communication in the Emergency Department: A Mixed-methods Study. West J Emerg Med. 2026;27(1)91–98.
Category: Critical Care
Keywords: OCHA, VF, ventricular fibrillation, cardiac arrest, shockable, Occult VF (PubMed Search)
Posted: 1/28/2026 by Kami Windsor, MD
(Updated: 2/8/2026)
Click here to contact Kami Windsor, MD
A crucial part of cardiac arrest management is identification of the underlying rhythm, with key aspects of management diverging depending whether shockable (pulseless ventricular tachycardia/pVT or ventricular fibrillation/VF) or unshockable (pulseless electrical activity/PEA or asystole).
A recent study prospectively evaluated adult atraumatic out-of-hospital-cardiac-arrests (OHCAs) presenting to the ED, to determine what percentage of cases had “Occult VF” – VF found point-of-care echocardiogram but not by ECG. The researchers only included cases with simultaneous ECG and echo assessments for the initial 3 pulse checks. Echo and ECG determinations for the study were adjudicated by research team members.
They found that:
Major limitations:
Bottom Line: Point-of-care echocardiogram continues to have value in the management of cardiac arrest, potentially changing management and affecting post-ROSC decisions. Ensuring high-quality CPR, with appropriate defibrillation and anti-arrhythmic strategies, remains paramount in management of shockable OHCA.
Gaspari R, Adhikari S, Gleeson T, et al. Occult Ventricular Fibrillation Visualized by Echocardiogram During Cardiac Arrest: A Retrospective Observational Study From the Real-Time Evaluation and Assessment for Sonography-Outcomes Network (REASON). J Am Coll Emerg Physicians Open. 2025;6(1):100028. doi: 10.1016/j.acepjo.2024.100028.
Category: Toxicology
Keywords: cannabinoids, liver enzymes, toxicology (PubMed Search)
Posted: 1/20/2026 by Lena Carleton, MD
(Updated: 1/26/2026)
Click here to contact Lena Carleton, MD
Consumer use of cannabidiol (CBD) products for medicinal and recreational purposes has increased in recent years. Regulatory barriers have limited randomized controlled trials examining the clinical and physiologic effects of cannabinoids in humans. This study aimed to evaluate the impact of daily cannabidiol oil use on liver enzymes and endocrine hormones in healthy adults.
In this double-blind, randomized, placebo-controlled study conducted at a clinical pharmacology unit in Wisconsin, 201 healthy adults were randomized to receive either oral CBD (2.5 mg/kg twice daily) or placebo. Laboratory testing was performed weekly.
Among participants receiving CBD (n = 151), 8 developed AST and ALT elevations greater than three times the upper limit of normal; 7 of these also had eosinophilia. No participants in the placebo group (n = 50) developed similar transaminase elevations. There were no significant differences between groups in measured endocrine hormones, including total testosterone, inhibin B, thyroid-stimulating hormone, total triiodothyronine, and free thyroxine.
Limitations included a modest sample size, unequal group sizes, and a relatively short duration of exposure and follow-up.
Key Takeaway: CBD use may be associated with elevations in AST and ALT. However, evidence remains limited, and abnormal liver enzymes should still prompt evaluation for alternative etiologies.
Florian J, Salcedo P, Burkhart K, et al. Cannabidiol and Liver Enzyme Level Elevations in Healthy Adults: A Randomized Clinical Trial. JAMA Intern Med. 2025;185(9):1070–1078. doi:10.1001/jamainternmed.2025.2366
Category: Trauma
Keywords: Pelvic fracture, EMS (PubMed Search)
Posted: 1/25/2026 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
A reminder from a recent position paper on pelvic trauma that we should not be doing stability testing to evaluate pelvic trauma
“EMS clinicians should recognize the challenges in accurately identifying pelvic fractures by physical exam alone. Manual stability testing of the pelvis is neither sensitive nor specific and may cause harm.”
Lyng, J. W., Corsa, J. G., Raetzke, B. D., Wilson, B. R., McCoy, A., Patterson, S. C., … Bosson, N. (2025). Prehospital Trauma Compendium: Evaluation and Management of Suspected Pelvis Fractures – An NAEMSP Position Statement and Resource Document. Prehospital Emergency Care, 1–35. https://doi.org/10.1080/10903127.2025.2540420
Category: Orthopedics
Posted: 1/24/2026 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
The recommended approach for patients with suspected septic arthritis is arthrocentesis with fluid analysis sent for: Gram stain, culture, WBC count with differential, and crystal analysis before starting antibiotics.
From a classic meta-analysis of 14 studies involving greater than 6,000 patients the only 3 findings that occur in more than 50% of patients with septic arthritis were
Joint pain (sensitivity, 85%; 95% confidence interval [CI], 78%-90%),
Joint swelling (sensitivity, 78%; 95% CI, 71%-85%),
Fever (sensitivity, 57%; 95% CI, 52%-62%).
Vs.
Sweats (sensitivity, 27%; 95% CI, 20%-34%)
and rigors (sensitivity, 19%; 95% CI, 15%-24%) were less common findings in septic arthritis.
The probability of septic arthritis increases progressively with higher synovial WBC counts:
PMN percentage ?90% suggests septic arthritis with LR 3.4 (95% CI, 2.8-4.2)
VS
PMN <90% lowers the likelihood (LR 0.34, 95% CI 0.25-0.47).
Margaretten ME, Kohlwes J, Moore D, Bent S. Does This Adult Patient Have Septic Arthritis? JAMA. 2007;297(13):1478-88.
Category: Ultrasound
Keywords: knee effusion, ultrasound, method (PubMed Search)
Posted: 1/21/2026 by Kerith Joseph, MD
(Updated: 1/22/2026)
Click here to contact Kerith Joseph, MD
Study Overview
Title: Identification of Knee Effusions With Ultrasound: A Comparison of Three Methods
Design: Prospective cohort study
Setting: Outpatient orthopaedic clinic
Participants: 52 adults (104 knees), including 57 painful knees
Objective
Determine whether two simple dynamic techniques improve ultrasound detection of suprapatellar knee effusions compared with static scanning.
Ultrasound Methods Compared
Static scanning: Patient relaxed; standard long- and short-axis views.
Parapatellar pressure (Method 1): Examiner compresses medial and lateral parapatellar recesses during scanning.
Quadriceps contraction (Method 2): Patient actively contracts quadriceps during scanning.
Outcome Measure
Presence of fluid in the suprapatellar recess (graded using a standardized ultrasound effusion scale).
Key Results
Effusions detected:
Static scanning: 45
Parapatellar pressure: 58
Quadriceps contraction: 77
Comparative performance:
Quadriceps contraction was superior to parapatellar pressure for detecting:
All effusions (PR 1.33; P < 0.001)
Painful knees (PR 1.24; P = 0.036)
Painless knees (PR 1.50; P = 0.006)
Both dynamic methods outperformed static scanning.
Additional detection beyond static scanning:
Parapatellar pressure: +16.9% of knees
Quadriceps contraction: +54.2% of knees
Reliability (Inter-rater Agreement)
Static scanning: ? = 0.771
Parapatellar pressure: ? = 0.686
Quadriceps contraction: ? = 0.846
All methods showed high reliability, with quadriceps contraction highest.
Conclusions
Both parapatellar pressure and patient-initiated quadriceps contraction significantly improve ultrasound detection of suprapatellar knee effusions.
Quadriceps contraction is the most effective method, especially for small or occult (grade 1) effusions.
Category: EMS
Keywords: VT, VF, shockable, pad placement (PubMed Search)
Posted: 1/21/2026 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
The European resuscitation council recommends AL (anterior-lateral) pad positioning while the American Heart Association recommends AL or AP (anterior-posterior) pad placement for defibrillation.
This was a prospective cohort study over a 4 year period in a single EMS jurisdiction. Adult patients with a medical cardiac arrest with an initial rhythm of VT/VF were included. The primary outcome was ROSC at any period of time.
Patients with AP pad placement (compared to AL) had a higher adjusted odds ratio of ROSC at any time (1.34), but not statistically different odds of pulse in the ED, survival to hospital admission or discharge, or functional status at hospital discharge.
The AP pad placement group also required less shocks on average and had earlier and initial sustained rates of ROSC. Further research is needed with respect to initial pad placement in the cardiac arrest population.
Lupton JR, Newgard CD, Dennis D, Nuttall J, Sahni R, Jui J, Neth MR, Daya MR. Initial Defibrillator Pad Position and Outcomes for Shockable Out-of-Hospital Cardiac Arrest. JAMA Netw Open. 2024 Sep 3;7(9):e2431673. doi: 10.1001/jamanetworkopen.2024.31673. Erratum in: JAMA Netw Open. 2024 Nov 4;7(11):e2448135. doi: 10.1001/jamanetworkopen.2024.48135. PMID: 39250154; PMCID: PMC11385052.
Category: Critical Care
Keywords: sepsis, subtypes, long term mortality, disability (PubMed Search)
Posted: 1/20/2026 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
Settings: Secondary analysis of the Crystalloid Liberal or Vasopressors Early Resuscitation in Sepsis (CLOVERS) trial.
Participants:
1368 patients who survived on day 28 after enrollment, and were retrospectively assigned different subtypes:
Low risk, barriers to care. Younger patients with few comorbidities, less severe disease,
Unhealthy baseline with severe illness: Previously healthy with severe illness and complex needs after discharge, barriers to care.
Multimorbidity. Older patients with more comorbidities and are frequently readmitted.
Low functional status: Poor functional status. Older patients with high prevalence of frailty at discharge and high functional needs who are often discharged to a facility.
Unhealthy baseline with severe illness: Existing poor health with severe illness and complex needs after discharge. Older patients with severe comorbidities, more severe illness, high functional needs, prolonged hospital stay,
Outcome measurement:
A) 90-day mortality,
B) 6-month and 12-month EuroQol 5D five level score
Study Results:
A) 90-day mortality:
Unhealthy baseline with severe illness (37.6%) > low functional status (45.5%) > multimorbidity (17.4%) > unhealthy baseline, severe illness (13.2%) > Low risk (5.1%).
B) 6-month EuroQol 5D-Five Level: lower score, lower functional outcomes)
Unhealthy baseline with severe illness (0.53) > unhealthy baseline, severe illness (0.68) > low functional status (0.69) > multimorbidity (0.78) > Low risk (0.80).
Discussion:
a) The framework, readily available to clinicians provides good prognostic tools for mortality.
b) Although there was prediction of poor functional outcomes at 6-month and 12-month, the differences between subtypes in their EuroQoL 5D-5L did not seem to correspond to 90-day mortality. Low functional status group had 2nd-highest rate of mortality, but only 3rd in their EuroQoL 5D-3L score. Thus, there needs to be more studies in these nuances.
Conclusion:
Sepsis survivor subtypes—assigned using only three routinely available discharge variables—are strongly associated with 3-month mortality and long-term disability and HRQOL up to 12 months
Flick RJ, Kamphuis LA, Valley TS, Armstrong-Hough M, Iwashyna TJ. Association of Sepsis Survivor Subtypes With Long-Term Mortality and Disability After Discharge: A Retrospective Cohort Study. Crit Care Med. 2026 Jan 1;54(1):45-54. doi: 10.1097/CCM.0000000000006933. Epub 2025 Nov 13. PMID: 41231072.
Category: Ultrasound
Keywords: POCUS, GI, Hernia (PubMed Search)
Posted: 1/19/2026 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
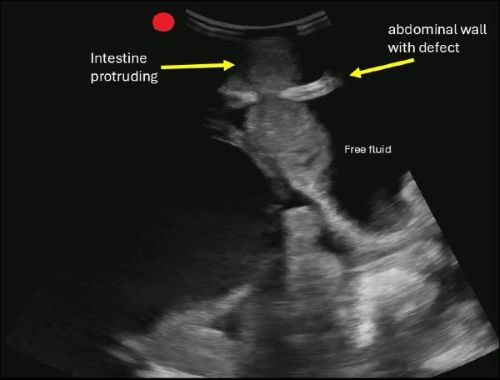
POCUS can help you identify signs of a hernia.
Begin by asking the patient to localize the point of maximal tenderness, then place a linear or curvilinear transducer over the area of concern. If there is concern for an inguinal hernia, you can have the patient perform a Valsalva maneuver while holding the probe in the area to evaluate dynamic changes.
A hernia is diagnosed when omental fat or intestinal contents are seen protruding through a defect in the abdominal wall.
If you are concerned about an incarcerated hernia, sonographic findings may include absence of peristalsis, presence of surrounding free fluid, with preserved blood flow on color Doppler. If a hernia progresses to strangulation, you may notice the absence of flow on color and power Doppler.
Boccatonda A, Brighenti A, Tiraferri V, Doglioli M, Iazzetta L, De Meis L, Safai Zadeh E, Dietrich CF, Serra C. POCUS for acute abdominal pain: practical scan protocols on gastrointestinal diseases and an evidence review. J Ultrasound. 2025 Dec;28(4):851-871. doi: 10.1007/s40477-025-01088-7.
Category: Geriatrics
Keywords: Delerium, antihistamine, geriatrics (PubMed Search)
Posted: 1/18/2026 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In 261 ED patients over age 65 receiving first generation antihistamines, 15% had an adverse reaction. Most common was delirium and urinary retention. Age over 85, previous cognitive impairment and multiple doses increased the risk of adverse reaction. Along with previous literature, this should discourage use of first generation antihistamines in older ED patients.
Killen, E., Cusumano, M., Zhang, Z., Newman, R., Voigtmann, J., Sanford, A. M, & Bitter, C. C. (2025). First-Generation Antihistamine Use in Geriatric Emergency Department Patients: Retrospective Review. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 27(1). http://dx.doi.org/10.5811/westjem.47491 Retrieved from https://escholarship.org/uc/item/7230n5z1
Category: Pediatrics
Keywords: PNA, CXR (PubMed Search)
Posted: 1/16/2026 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
This was a retrospective study at a tertiary pediatric emergency department over a 10 year period. Authors sought to determine the number of patients who developed radiographic pneumonia after an initial normal CXR.
9957 patients with suspected pneumonia were included. 240 had an additional CXR within 14 days and 27 (11% of those with a 2nd CXR) had developed PNA on the CXR. Overall, the rate was 1/370 children went on to have radiographic PNA in the next 14 days after an initial CXR. Tachypnea, hypoxia and dehydration at the initial visit were shown to be associated with later development of PNA on CXR.
Hirsch AW, Wagner A, Lipsett SC, Monuteaux MC, Neuman MI. Risk of Subsequent Pneumonia After a Negative Chest Radiograph in the ED. Pediatrics. 2025 May 1;155(5):e2024069829. doi: 10.1542/peds.2024-069829. PMID: 40189217.
