Category: Obstetrics & Gynecology
Posted: 10/9/2025 by Jennifer Wang, MD
(Updated: 2/8/2026)
Click here to contact Jennifer Wang, MD
At this point, we've likely all encountered a patient who is on aspirin as a preventative for a history of pre-eclampsia or high risk pregnancy, but what about for low risk patients who have not yet had any children?
This meta-analysis came out in August of this year looking at RCTs that examined giving low dose aspirin to low-risk (no pre-eclampsia, gestational DM/HTN, autoimmune or renal disease), nulliparous individuals during pregnancy and found that while not all doses of aspirin at all ages were helpful, a planned subgroup analysis showed that giving 100mg of aspirin daily starting before 16 weeks cut the odds of preterm birth before 37 weeks in about half (RR 0.45).
That's not to say that we should all be starting aspirin for our patients in the emergency department just yet - but this might be why you're seeing aspirin pop up on more of our pregnant patients' medication list (or why your OB might be recommending it to you or your family/friends).
Wodoslawsky S, Khanuja K, Saccone G, Hoffman MK, Berghella V. Low-dose aspirin use in low-risk nulliparous pregnancies: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol MFM. 2025;7(2):101595. doi:10.1016/j.ajogmf.2024.101595
Category: Geriatrics
Keywords: fall, score, geriatric, prediction (PubMed Search)
Posted: 10/11/2025 by Robert Flint, MD
(Updated: 10/12/2025)
Click here to contact Robert Flint, MD
These authors used information available from both the medical record as well as from a survey instrument given in the emergency department to created this fall risk score. A score over 6 had a 63% sensitivity and 75% specificity of predicting future falls.
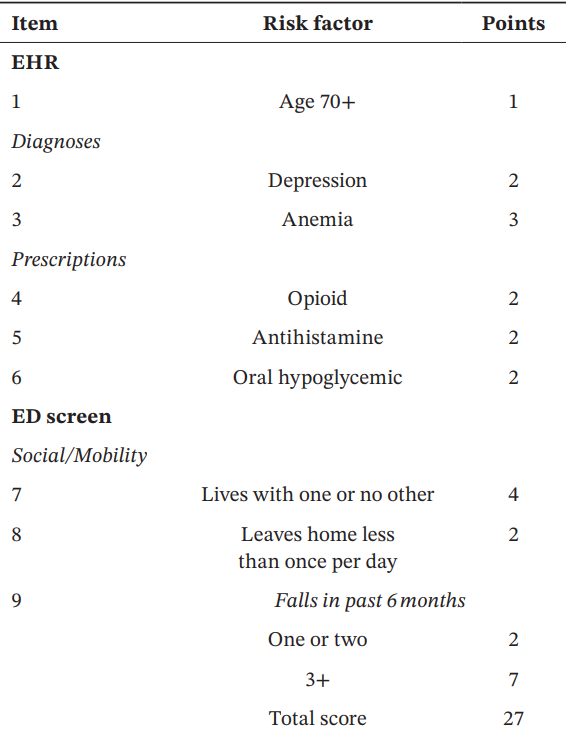

Acaemic Emergency Medicine 2025 0:1-12
Category: Orthopedics
Posted: 10/11/2025 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Use of Muscle Relaxants in the Elderly
A recent pearl discussed the risks of skeletal muscle relaxants (SMR) in the elderly population.
Risks included sedation, confusion, disorientation, orthostatic hypotension and increased risk for falls and fractures.
The Beers Criteria is a list of medications that older adults should generally avoid due to potential adverse effects.
Two commonly used muscle relaxants, Baclofen and Tizanidine (Zanaflex) are not included in the Beers criterion.
A study published last month investigated the safety profile of these medicines as compared to cyclobenzaprine (Flexeril).
Retrospective cohort study of Kaiser Permanente Southern California patients aged 65 to 99 years between 2008 and 2018.
From a population of approximately 88,000 participants (mean age 71.4 years; 59.8% women), approximately 118,000 study medication episodes were identified: 54.8% participants were dispensed baclofen, 6.3% tizanidine, and 38.9% cyclobenzaprine
Outcomes included injury-related hospitalizations, emergency department visits, and urgent care visits documented in EMR and identified through diagnostic codes for fractures, falls leading to fractures, brain injuries, and dislocation injuries
Compared with cyclobenzaprine, Baclofen demonstrated a 69% greater risk (adjusted Hazard Ratio 1.69, [95% CI 1.51-1.88]) and tizanidine carried a 34% greater risk (adjusted Hazard Ratio 1.34, [95% CI 1.11-1.62]) for composite injury outcomes.
Conclusion: Older adult patients prescribed baclofen or tizanidine have an increased risk of injury when compared with Flexeril (currently included on the Beers Criteria)
George MM, et al. Safety of Baclofen and Tizanidine in Older Adults: A Retrospective Cohort Study in a Large Integrated Health Care System. J Am Geriatr Soc. 2025 Sep 13
Category: Pediatrics
Keywords: pediatrics, sinusitis, infectious diseases (PubMed Search)
Posted: 10/10/2025 by Kathleen Stephanos, MD
(Updated: 2/8/2026)
Click here to contact Kathleen Stephanos, MD
As we enter cold and flu season, sinus issues become commonplace in the ED. What do we need to know about pediatric sinusitis?
First, it is important to know when pneumatization of the sinuses occur (so we don't look for symptoms where they can't be present). Completion of their development does not occur until around age 21 years.
Sinusitis should be a clinical diagnosis and does not require imaging unless there is concern for abscess development, cellulitis or other complications, or in cases where symptoms are not improving despite treatment.
In most otherwise healthy children, acute sinusitis is typically viral in nature, regardless of the color of nasal discharge, and can be managed with symptomatic care, including saline sprays, humidifiers, warm compresses and monitoring.
There are strict criteria for otherwise healthy children regarding when to initiate antibiotics including:
The antibiotic of choice is high-dose amoxicillin with or without clavulanic acid (cefpodoxime or cefdinir can be considered in penicillin allergic patients)
Antibiotic stewardship is critical in these patients, as unnecessary antibiotics can result in resistance or undesired side effects. There should be a clear conversation about return precautions with parents including education about the importance of symptomatic management over antibiotics in the first 10 days.
Ramadan HH, Chaiban R, Makary C. Pediatric Rhinosinusitis. Pediatr Clin North Am. 2022 Apr;69(2):275-286. doi: 10.1016/j.pcl.2022.01.002. PMID: 35337539.
Leung AK, Hon KL, Chu WC. Acute bacterial sinusitis in children: an updated review. Drugs Context. 2020 Nov 23;9:2020-9-3. doi: 10.7573/dic.2020-9-3. PMID: 33281908; PMCID: PMC7685231.
Category: Pharmacology & Therapeutics
Keywords: rapid sequence intubation, rocuronium, paralytic, awareness (PubMed Search)
Posted: 10/9/2025 by Alicia Pycraft
Click here to contact Alicia Pycraft
It is estimated that between 2.6% and 3.4% of patients undergoing rapid sequence intubation (RSI) experience awareness with paralysis, with the highest risk observed in patients receiving rocuronium. Several studies have now demonstrated prolonged time to sedation following RSI with long-acting paralytics, including a 2024 single-centered retrospective chart review by Dukes et al., which found that fewer than half of patients in the ICU receiving rocuronium for RSI were administered sedation within 15 minutes of intubation. The following study by Cappuccilli et al. sought to compare differences in sedation practices between the ED and ICUs at the same institution, hypothesizing that patients undergoing RSI in the ED would experience similar delays in sedation to those in the ICU.
Category: Gastrointestional
Keywords: GI bleed, presentation, antithrombotics (PubMed Search)
Posted: 10/8/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In a retrospective observational study comparing patients both on and not on antithromotics (DOAC/warfarin or anti platelets) who presented with a GI bleed these authors found:
“Patients with anticoagulant therapy more often present with a lower source of GI bleeding than both those on antiplatelet medications and those with no antithrombotics. Overall patients on anticoagulants are also less likely to present with hematemesis, even with a later confirmed upper GI bleeding. Furthermore, results indicate that the need for endoscopic interventions and transfusions are dependent on initial presenting symptoms but not affected by antithrombotic therapy at admission.”
Forsberg-Puckett, A., Wurm Johansson, G. & Regnér, S. Presentation of gastrointestinal bleeding in patients with antithrombotic therapy, results from a consecutive retrospective cohort. Scand J Trauma Resusc Emerg Med 33, 146 (2025). https://doi.org/10.1186/s13049-025-01431-1
Category: Critical Care
Keywords: acute respiratory failure, hypercapnia, hypercarbia, COPD, AE-COPD, noninvasive ventilation, high flow nasal cannula (PubMed Search)
Posted: 10/7/2025 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Q: Can you use high flow nasal cannula (HFNC) to manage acute hypercapnic respiratory failure?
A: It probably depends.
Background: While we now frequently utilize HFNC as an initial therapy for most acute hypoxic respiratory failure, its appropriateness in managing acute respiratory failure with hypercarbia has historically been opposed. With more recent data indicating that HFNC may be as good as noninvasive ventilation (NIV) for management of hypercapnia as well, this seemed like a good time to point out a few things:
The RENOVATE trial was a larger multicenter randomized noninferiority trial looking at HFNC vs NIV in all-comer acute respiratory failure, summarizing that HFNC was noninferior in the primary composite outcome of death + intubation at 7 days.
BUT this conclusion is not clearly supported in the smaller COPD (or acute cardiogenic pulmonary edema) subgroup:
What does seem to be clear across studies that HFNC has the capacity to clear some CO2 and is by and large better tolerated than facemask NIV.
Bottom Line: For mild-moderate acute COPD exacerbations with patient intolerance or exclusion criteria for NIV therapy, trialing HFNC is a reasonable option. For patients with severe acute or acute on chronic hypercapnia, as indicated by a [pseudo-arbitrary] pH < 7.25 and PaCO2 >70-80, noninvasive ventilation should be your go-to… or be ready to promptly intubate if/when the high flow fails.
Category: Ultrasound
Keywords: CPR, POCUS, pulse checks (PubMed Search)
Posted: 10/6/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
A recent systematic review compared the timing and diagnostic accuracy of manual pulse check versus point-of-care ultrasound (POCUS) pulse checks (this means placing an ultrasound probe on the carotid or femoral artery to evaluate for a doppler pulse).
The review included seven studies encompassing a total of 469 patients.
Six of the studies assessed the duration of pulse checks, revealing a mean time difference of –1.39 seconds (95% CI: –2.20 to –0.57) in favor of ultrasound.
Three of the studies reported the sensitivity and specificity of POCUS pulse checks, yielding pooled estimates of 99% sensitivity (95% CI: 87%–100%) and 96% specificity (95% CI: 85%–99%). In contrast, two studies evaluated manual pulse checks, with pooled sensitivity of 62% (95% CI: 22%–91%) and specificity of 91% (95% CI: 88%–93%).
As with many systematic reviews, the studies included demonstrated high heterogeneity and generally low methodological quality, indicating that further investigation may still be needed.
Neto ES, Scapin M, Lazaro-Paulina F, Campbell RL, Molinari DF, Kummer T. Duration of resuscitation interruption using point-of-care ultrasound versus traditional manual pulse check: A systematic review and meta-analysis. Am J Emerg Med. 2025 Aug 23;98:145-152. doi: 10.1016/j.ajem.2025.08.049.
Category: Trauma
Keywords: head injury, trauma, geriatric (PubMed Search)
Posted: 10/4/2025 by Robert Flint, MD
(Updated: 10/5/2025)
Click here to contact Robert Flint, MD
This paper reminds us older patients have higher mortality and worse outcomes overall if their injury includes a head injury. Any mechanism that results in head injury, including fall from standing, has a higher potential for death, disability, and long term cognitive decline in older patients. Triaging these patients to trauma centers can lead to better outcomes. The difficulty is knowing which patients to send to trauma centers vs. emergency departments. The authors write:
"clinicians should consider transporting to a trauma center in geriatric patients with head trauma, if feasible. However, given the frequency with which head injury occurs, transportation to a trauma center for all patients with head trauma is likely to overwhelm EMS systems and hospitals. Unfortunately, the existing literature does not delineate the subset of patients whose condition will benefit from this evaluation . Given these considerations, we recommend EMS clinicians consider abnormal mental status, presence of anti-coagulation, and loss of consciousness as considerations to transport to a trauma center in cases where the need for trauma center evaluation is not clear.”
Haussner, W. K., Breyre, A. M., Bascombe, K., Barrett, W. J., Camacho, M. A., Overton-Harris, P., … Colwell, C. (2025). Prehospital Trauma Compendium: Management of Geriatric Trauma Patients – A Position Statement and Resource Document of NAEMSP. Prehospital Emergency Care, 1–10. https://doi.org/10.1080/10903127.2025.2557006
Category: Geriatrics
Keywords: trauma, geriatric, prehospital, EMS (PubMed Search)
Posted: 10/4/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Reenforcing the recent pearl on geriatric trauma patient care, here is the National Association EMS Physicians statement on prehospital care.
"EMS clinicians should use age-adjusted, physiologic criteria to guide decisions to transport geriatric trauma patients to the most appropriate level of trauma center available in the community.
Geriatric trauma patients should be promptly evaluated for pain and should receive analgesic interventions in a timely manner. Analgesic medications should be dosed following weight-based guidance and should be administered with consideration of potential drug interactions and age-related changes in drug metabolism and side effects.
EMS clinicians should consult advance care planning documents, e.g., Physician Orders for Life-Sustaining Treatment (POLST), when available, to guide care in emergency scenarios, including management of traumatic injuries.
While older patients are at higher risk for spinal injuries, including lumbar and cervical spine fractures, traditional spinal motion restriction practices may not be suitable for older patients due to age-related anatomic changes in spinal alignment and increased risk for cutaneous pressure-related injuries. EMS clinicians should exercise judgment to determine when and how to best achieve spinal motion restriction if spinal injury is suspected in geriatric trauma patients."
Haussner, W. K., Breyre, A. M., Bascombe, K., Barrett, W. J., Camacho, M. A., Overton-Harris, P., … Colwell, C. (2025). Prehospital Trauma Compendium: Management of Geriatric Trauma Patients – A Position Statement and Resource Document of NAEMSP. Prehospital Emergency Care, 1–10. https://doi.org/10.1080/10903127.2025.2557006
Category: Pediatrics
Keywords: Pediatric Procedural Sedation (PubMed Search)
Posted: 10/1/2025 by Taylor Lindquist, DO
Click here to contact Taylor Lindquist, DO
In the pediatric ED, intranasal midazolam is a common choice among providers for procedural sedation. However, with widely varying recommendations, the ideal dose remains a topic of debate.
A recent randomized clinical trial published in JAMA Pediatrics involving 101 children, ages 6 months to 7 years, sought to determine the best dose of intranasal (IN) midazolam for sedation during laceration repair. Researchers compared four different doses: 0.2, 0.3, 0.4, and 0.5 mg/kg.
The primary outcome was achieving adequate sedation for at least 95% of the procedure. Secondary outcomes included the level of sedation, how quickly it took effect, recovery time, satisfaction of clinicians and caregivers, and any negative side effects.
What did they find?
The lower doses (0.2 and 0.3 mg/kg) were found to be less effective and were removed from the study early.
The two higher doses (0.4 and 0.5 mg/kg) both provided similar, adequate sedation for about two-thirds of the children.
Sedation took effect quickly, within a few minutes, and children recovered fast.
Adverse events were rare and not serious.
Satisfaction among both clinicians and caregivers was high across the board.
Bottom line: Consider reaching for higher doses of intranasal midazolam (0.4 to 0.5 mg/kg) for pediatric patients requiring procedural sedation.
Optimal Dose of Intranasal Midazolam for Procedural Sedation in Children: A Randomized Clinical Trial. JAMA Pediatr. 2025 Jul 28:e252181. doi: 10.1001/jamapediatrics.2025.2181. Epub ahead of print. PMID: 40720114; PMCID: PMC12305440.
Category: Geriatrics
Keywords: geriatrics, frail, diverticulitis (PubMed Search)
Posted: 9/24/2025 by Robert Flint, MD
(Updated: 10/1/2025)
Click here to contact Robert Flint, MD
This retrospective study looking at a readmission database for patients greater than 65 years categorized 10,000 patients into non-frail, pre-frail and frail based on the five-factor modified frailty index. They found no difference in recurrent diverticulitis among the groups but did find:
“frailty was a predictor of mortality on index hospitalization (adjusted odds ratio, 1.99; p < 0.001) and readmissions (adjusted odds ratio, 3.05; p < 0.001)…frail patients are at increased risk of mortality once they develop diverticulitis. Optimal management for frail patients with diverticulitis must be defined to improve outcomes.”
Once again, assessing your patient's frailty can help you predict outcomes and have meaningful discussions with patients and their families.
Hejazi, Omar MD; Colosimo, Christina DO, MS, FACS; Khurshid, Muhammad Haris MD; Stewart, Collin MD, FACS; Al Ma'ani, Mohammad MD; Anand, Tanya MD, MPH, FACS; Castillo Diaz, Francisco MD; Castanon, Lourdes MD, FACS; Magnotti, Louis J. MD, MS, FACS; Joseph, Bellal MD, FACS. Does frailty predict readmission and mortality in diverticulitis? A nationwide analysis. Journal of Trauma and Acute Care Surgery 99(4):p 605-610, October 2025. | DOI: 10.1097/TA.0000000000004707
Category: Critical Care
Keywords: sepsis, septic shock, omeprazole, proton pump inhibitor, anti-inflammatory (PubMed Search)
Posted: 9/30/2025 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
Settings: multinational, randomized, double- blind, placebo-controlled clinical trial conducted in 17 centers in Italy, Russia, and Kazakhstan
Participants: A total of 307 ICU patients with sepsis or septic shock. Patients who were likely to die (APACHE II > 65 points) were excluded.
Treatment group: 80 mg bolus of omeprazole at randomization, at 12 hours and infusion of 12 mg/hour for 72 hours. Total dose of 1024 mg.
Outcome measurement: primary outcome of the study was organ dysfunction measured as the mean daily SOFA score during the first 10 days. Secondary outcomes were antibiotics-free days at 28 days; all-cause mortality at 28 days
Study Results:
Discussion:
Conclusion:
In sepsis patients, Esomeprazole did not re- duce organ dysfunction, despite demonstrating in vivo immunomodulatory effects
Monti G, Carta S, Kotani Y, Bruni A, Konkayeva M, Guarracino F, Yakovlev A, Cucciolini G, Shemetova M, Scapol S, Momesso E, Garofalo E, Brizzi G, Baldassarri R, Ajello S, Isirdi A, Meroi F, Baiardo Redaelli M, Boffa N, Votta CD, Borghi G, Montrucchio G, Rauch S, D'Amico F, Pace MC, Paternoster G, Vitale F, Giardina G, Labanca R, Lembo R, Marmiere M, Marzaroli M, Nakhnoukh C, Plumari V, Scandroglio AM, Scquizzato T, Sordoni S, Valsecchi D, Agrò FE, Finco G, Bove T, Corradi F, Likhvantsev V, Longhini F, Konkayev A, Landoni G, Bellomo R, Zangrillo A; PPI-SEPSIS Study Group. A Multinational Randomized Trial of Mega-Dose Esomeprazole as Anti-Inflammatory Agent in Sepsis. Crit Care Med. 2025 Aug 1;53(8):e1554-e1566. doi: 10.1097/CCM.0000000000006720. Epub 2025 May 29. PMID: 40439536.
Category: Toxicology
Keywords: Carbon Monoxide, Hyperbaric (PubMed Search)
Posted: 9/26/2025 by TJ Gregory, MD
(Updated: 9/29/2025)
Click here to contact TJ Gregory, MD
Carbon Monoxide Poisoning (COP) is a major toxicologic pathology and a common case in the Emergency Department and pre-hospital setting. History is a key component in assessment with the standard diagnostic test being blood gas analysis of Carboxyhemoglobin (COHb).
Standard pulse oximeter devices are not capable of differentiating oxyhemoglobin from carboxyhemoglobin, leading to the classic pearl that pulse ox may be falsely reassuring in COP.
In recent years, devices capable of differentiating oxyhemoglobin from COHb have been developed and are fielded in many hospitals and EMS agencies.
This meta-analysis reviews diagnostic accuracy of pulse CO-oximetry (spCO) devices in comparison to a reference standard COHb blood test. Six studies (1734 patients) were included.
This analysis found that spCO testing has a low sensitivity and high specificity.
Pooled sensitivity 0.65 (95% CI 0.44–0.81)
Pooled specificity 0.93 (95% CI 0.83–0.98)
Pooled LR+ 9.4 (95% CI 4.4 to 20.1)
Pooled LR- 0.38 (95% CI 0.24 to 0.62)
The authors conclude that the low sensitivity precludes use of spCO as an effective screening tool for COP or substitute for COHb. Conversely, we can recognize the utility of the high specificity in identifying patients who do have clinically significant toxicity. Indeed, the authors discuss potential applications for triage and transport to a hyperbaric oxygen chamber for those who are found to have elevated readings.
Technology advancement and refinement will be interesting to follow. In the meantime, don’t skip the COHb lab just because spCO measurement is reassuring.
Category: Critical Care
Keywords: compartment syndrome, abdomen, critically ill (PubMed Search)
Posted: 9/24/2025 by Robert Flint, MD
(Updated: 9/28/2025)
Click here to contact Robert Flint, MD
This review article reminds us that abdominal hypertension and compartment syndrome need to remain on our differential diagnosis for critically ill and injured patients. Pressure is measured with an intra-bladder catheter. Normal pressure is 5-7 mm HG. Sustained over 12 mm Hg is hypertension and sustained over 20 mm Hg is compartment syndrome.
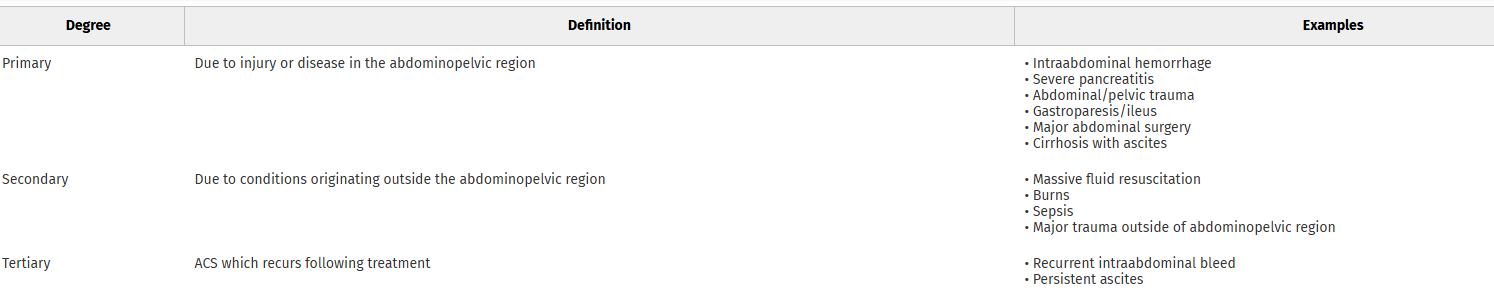
Arcieri, Talia R. MD; Meizoso, Jonathan P. MD, MSPH, FACS. Intraabdominal hypertension and abdominal compartment syndrome: What you need to know. Journal of Trauma and Acute Care Surgery 99(4):p 504-513, October 2025. | DOI: 10.1097/TA.0000000000004603
Category: Orthopedics
Posted: 9/27/2025 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Use of Muscle Relaxants in the Elderly
A 2023 Cochrane Database review found moderate-certainty evidence that muscle relaxants may increase the risk of adverse events.
Primary adverse events are due to CNS depressant effects (dizziness, sedation) and anticholinergic effects.
Geriatric patients already have baseline unsteady gait, decreased coordination and cognitive changes.
A 2015 study showed that geriatric patients who took muscle relaxants were 2.25 times more likely to visit the ED for a fall or fracture and 1.5 times more likely to be hospitalized for a fall or fracture than patients who did not take these medications.
Risk is greatest in patients >65 years of age. This population was 1.32 times more likely to have an injury compared to patients who did not take skeletal muscle relaxants.
Alvarez CA, et al. Association of skeletal muscle relaxers and antihistamines on mortality, hospitalizations, and emergency department visits in elderly patients: a nationwide retrospective cohort study. BMC Geriatr. 2015;15:2.
Category: Toxicology
Keywords: alcohol withdrawal, phenobarbital, protocol, implimentation (PubMed Search)
Posted: 9/24/2025 by Robert Flint, MD
(Updated: 9/25/2025)
Click here to contact Robert Flint, MD
This study looking at pre and post-phenobarbital order set use to treat inpatient alcohol withdrawal syndrome found:
“AWS symptoms resolved more rapidly after implementation, with a 4.2- to 5.0-point reduction in daily maximum CIWA-Ar scores at 24 to 96 hours from hospital presentation, 30.1-hour reduction in AWS treatment duration (95% CI, 16.7-43.5 hours), and 2.2-day reduction in time to hospital discharge (95% CI, 0.7-3.7 days). Safety outcomes did not significantly differ before and after implementation.”
Remember phenobarbital can be used for alcohol withdrawal for our ED patients as well.
Here is the protocol:
Nursing
Vital signs 10 minutes after phenobarbital loading dose
Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) every 1-4 hours based on score
Loading Dose
Phenobarbital 15 mg/kg intravenous piggyback (recommended for most patients)
Phenobarbital 10 mg/kg intravenous piggyback (low risk or heavily pretreated with benzodiazepines)
As-Needed Doses
Phenobarbital 130 mg intravenous twice as needed for uncontrolled agitation or CIWA-Ar ?15
Phenobarbital 260 mg intravenous once as needed for uncontrolled agitation or CIWA-Ar ?15
Wolpaw BJ, Oren H, Quinnan-Hostein L, et al. Hospital-Wide Implementation, Clinical Outcomes, and Safety of Phenobarbital for Alcohol Withdrawal. JAMA Netw Open. 2025;8(8):e2528694. doi:10.1001/jamanetworkopen.2025.28694
Category: Administration
Keywords: Operations, Disposition, Decision-Making, Disparities, (PubMed Search)
Posted: 9/24/2025 by Mercedes Torres, MD
(Updated: 2/8/2026)
Click here to contact Mercedes Torres, MD
This publication is a retrospective cross-sectional study conducted based on data collected during January 1–December 31, 2019 from a large, academic ED in the Southeastern US with the following research questions and results:
Interesting point regarding how disposition decisions are different from the ample evidence on disparities within triage decisions: The presence of disparities in disposition decisions is noteworthy not only because of their potentially long-term effects on patients’ health, but also because unlike some of the other decisions made in the ED such as triage, they are typically made under relatively less time pressure with deliberation and input from multiple individuals, conditions that are known to make biases less likely.
Authors propose pursing further research to elucidate the factors that contribute to these findings, instituting systems to alert providers in real time to the presence of conditions that could exacerbate disparities in ED care, and including the measurement of disparities along sex, race and ethnicity into health care operations data.
Cheng Q, Argon NT, Evans CS, Lin P, Linthicum B, Liu Y, Mehrotra A, Patel MD and Ziya S (2024) An Investigation into Demographic Disparities in Emergency Department Disposition Decisions. Production and Operations Management 34(4): 688–696.
Category: Trauma
Keywords: Head injury, geriatric, interracial hemorrhage (PubMed Search)
Posted: 9/21/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This systematic review of the literature found four findings associated with intercranial hemorrhage in older patients after a fall. They were: focal neurologic findings, external signs of trauma on the head, loss of consciousness, and male sex.
We still need better studies as this is completely based on the quantity and quality of literature available to review. This information is not enough to change liberal CT imagining in older patients after a fall. It is the beginning of the study process.
Dubucs X, Gingras V, Boucher V, Carmichael PH, Ruel M, De Wit K, Grewal K, Mercier É, Blanchard PG, Benhamed A, Charpentier S, Émond M. Risk Factors for Traumatic Intracranial Hemorrhage in Older Adults Sustaining a Head Injury in Ground-Level Falls: A Systematic Review and Meta-analysis. Ann Emerg Med. 2025 Jul 22:S0196-0644(25)00313-0. doi: 10.1016/j.annemergmed.2025.05.021. Epub ahead of print. PMID: 40699169.
Category: Administration
Posted: 9/20/2025 by Kevin Semelrath, MD
(Updated: 2/8/2026)
Click here to contact Kevin Semelrath, MD
Systemic racism and institutional bias affect all aspects of medicine. This position paper from 2022 highlights some of the disparities present within the EM Clinical Ultrasound community. The authors identified several areas of concern regarding the make up of the leadership of the CU community, and importantly suggest several ways to create a more equitable specialty.
Javier Rosario, Resa E. Lewiss, Lori A. Stolz, Marina Del Rios, Josie Acuña, Srikar Adhikari, David Amponsah, Almaz S. Dessie, Michael Gottlieb, Robert D. Huang, Jodi Jones, Adaira Landry, Rachel B. Liu, Lorraine Ng, Nova L. Panebianco, Anthony J. Weekes, Starr Knight,
Creating a more racial-ethnic inclusive clinical ultrasound community,
The American Journal of Emergency Medicine,
Volume 54,
2022,
Pages 208-211,
ISSN 0735-6757,
https://doi.org/10.1016/j.ajem.2022.02.015.
(https://www.sciencedirect.com/science/article/pii/S0735675722000985)
