Category: Administration
Keywords: insurance, malpractice, claims-made, occurrence, lawsuit (PubMed Search)
Posted: 6/25/2025 by Steve Schenkel, MPP, MD
(Updated: 2/8/2026)
Click here to contact Steve Schenkel, MPP, MD
Malpractice Insurance comes in two varieties: Occurrence and Claims-made.
Occurrence covers lawsuits for which the event occurs while the insurance is active.
Claims-made only covers lawsuits for which the insurance is active both during the event and when the lawsuit is announced. It’s less expensive because the coverage period is both shorter and more definitive.
This is an important distinction when an event and a lawsuit may be separated by years, as happens with medical malpractice.
Occurrence is the “good” kind.
Claims-made requires a tail to cover any claims brought after the insured period ends.
Read how this can go awry in Emergency Medicine at Leon Adelman’s April post here, https://substack.com/home/post/p-161044772.
Category: Critical Care
Keywords: ventilation ineffective-trigger double-trigger (PubMed Search)
Posted: 6/24/2025 by Cody Couperus-Mashewske, MD
Click here to contact Cody Couperus-Mashewske, MD
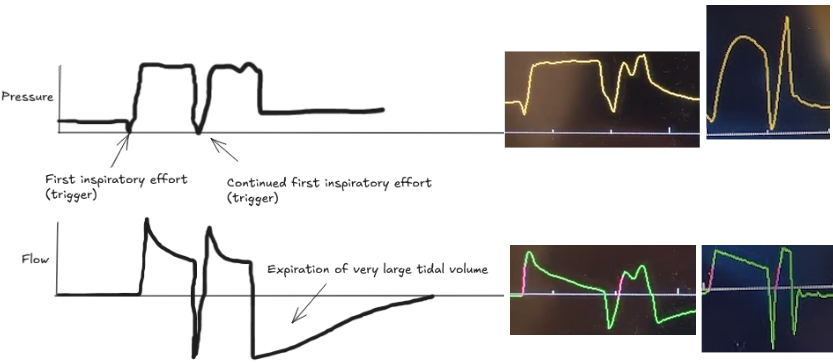
Patient-ventilator dyssynchrony is a sign of a disagreement between the patient's breathing and the ventilator's settings. Recognizing and fixing it is a critical skill to prevent lung injury and improve comfort. Ineffective triggering and double-trigger are two common types of dyssynchrony.
The patient tries to take a breath, but they are too weak to trigger the ventilator. This is the most common type of dyssynchrony. It causes increased work of breathing and discomfort.
Look for a small dip in the pressure waveform and a simultaneous scoop out of the expiratory flow waveform that is not followed by a delivered breath.
Troubleshooting options:
The patient's own breath outlasts the ventilator's set inspiratory time (Ti), causing one patient effort to trigger two stacked breaths. This results in delivery of large tidal volumes, risking lung injury (volutrauma).
Look for two consecutive breaths on the ventilator screen without a full exhalation in between.
Troubleshooting options:
Dyssynchrony means the ventilator settings do not match the patient's needs. Watch the waveforms to diagnose the mismatch, then either adjust the ventilator or treat the underlying problem.
Thille, A. W., Rodriguez, P., Cabello, B., Lellouche, F., & Brochard, L. (2006). Patient-ventilator asynchrony during assisted mechanical ventilation. Intensive care medicine, 32, 1515-1522.
Blanch, L., Villagra, A., Sales, B., Montanya, J., Lucangelo, U., Luján, M., ... & Kacmarek, R. M. (2015). Asynchronies during mechanical ventilation are associated with mortality. Intensive care medicine, 41, 633-641.
Category: Trauma
Keywords: Head injury, BIG, pediatric (PubMed Search)
Posted: 6/23/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Brain injury guidelines were designed to decrease transfers and neurosurgical consults for adults with head injuries.
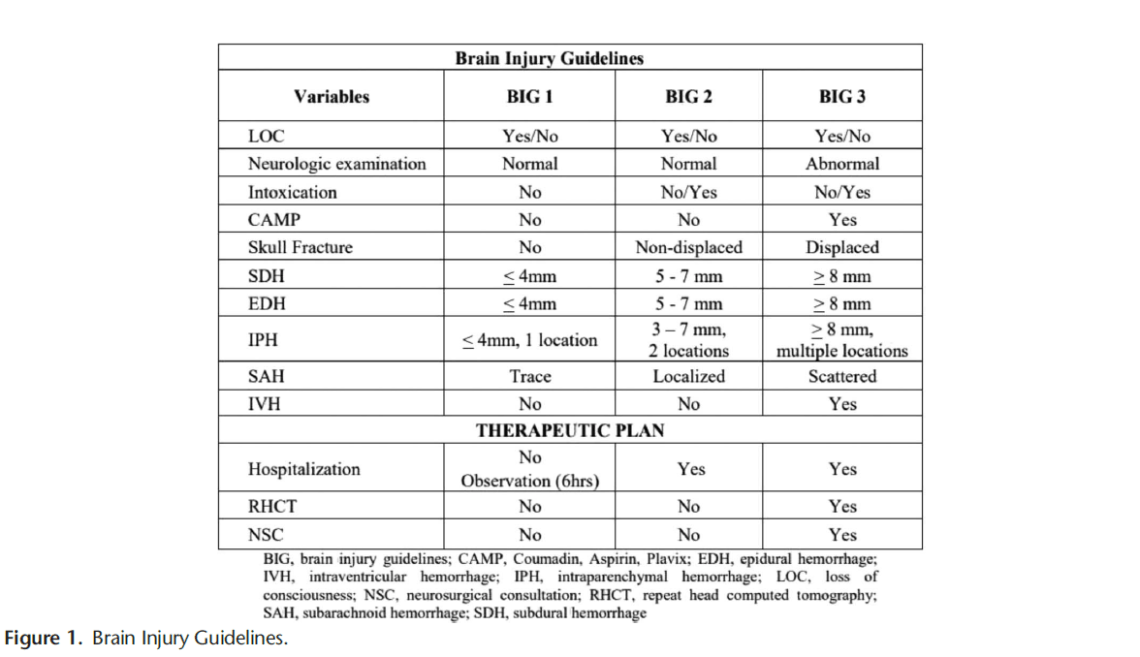
A new retrospective study suggests that modified guidelines may be feasible in the pediatric population as well. More data is needed but this is an important step in assuring safe resource utilization in pediatric head injury patients.
1. https://first10em.com/the-brain-injury-guidelines-can-we-avoid-talking-to-neurosurgeons/
2. Kay AB, Glasgow SL, Kahan AM, Swendiman RA, Kastenberg ZJ, Roach CM, Wan HY, Bollo RJ, Iyer RR, Ravindra VM, Morris DS, Yorkgitis BK, Joseph B, Russell KW. Small Change, BIG Impact: Proposal of the Brain Injury Guidelines for kids (kBIG). J Pediatr Surg. 2025 May 17;60(8):162372.
Category: Infectious Disease
Keywords: Abscess, brain, drainage, neurosurgery (PubMed Search)
Posted: 6/22/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In a Danish study of 558 patients with a brain abscess, those that had early surgical drainage did better than those treated conservatively with antibiotics only. Prompt neurosurgical consultation is warranted for these patients.
Category: Administration
Posted: 6/19/2025 by Kevin Semelrath, MD
(Updated: 6/21/2025)
Click here to contact Kevin Semelrath, MD
Despite ongoing attacks against the principles of DEI, most medical organizations know and have acknowledged the necessary role of creating a more diverse, equitable and inclusive environment. Doing so requires both a bottom up and a top down approach, with engaged leadership supporting active efforts to increase diversity
This author, published just this month in Annals, details a unique and exciting way to engage resident leadership in the DEI efforts of an emergency department, with the creation of a Chief Resident for DEI role. They detail the creation of the role, and describe some of the roles and responsibilities and thoughfully discuss some of the limitations. It's an exciting and thought provoking read.
Ali, Fahad et al.
Annals of Emergency Medicine, Volume 85, Issue 6, 491 - 497
Category: Pediatrics
Posted: 6/20/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Intranasal (IN) midazolam is often used for anxiolysis in pediatrics prior to procedures. In this study, 0.2 mg/kg of IN midazolam (up to 6 mg total dose) was given prior to laceration repair in children 2-10 years.
90% of children were at least minimally sedated at the start of the procedure and these children also displayed less anxiety when measured on a standardized anxiety scale.
Children's whose procedure started 10-20 minutes after IN medication compared to 25-35 minutes had significantly lower anxiety.
IN midazolam can be successful as an anxiolytic, but careful attention should be directed at the timing of the procedure.
Martin SR, Bauer K, Heyming TW, Zhu J, Lee H, Kain ZN. Incidence and predictors of nonresponse to intranasal midazolam in children undergoing laceration repair. Acad Emerg Med. 2025 Feb 3. doi: 10.1111/acem.15106. Epub ahead of print. PMID: 39901057.
Category: EMS
Keywords: GCS, pediatric trauma, motor (PubMed Search)
Posted: 6/18/2025 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
GCS was first introduced in 1974 and now includes a preverbal version for patients < 2 years.
This study looked for non inferiority between motor Glascow Coma Scale (mGCS) and the total GCS in pediatric patients. The study also examined if a mGCS<6 was non inferior to a GCS < 14 in children. 582 patients < 18 years were reviewed in this retrospective review.
The mGCS was noninferior to total GCS as a triage tool in pediatric trauma. It also validated the use of mGCS <6 in place of GCS <14 in the field with identification of children at risk of death or requiring ICU care.
Yap SE, Wong HC, Chong SL, Ganapathy S, Ong GY. Validation of motor component of Glasgow coma scale in lieu of total Glasgow coma scale as a pediatric trauma field triage tool. Am J Emerg Med. 2024;81:105-110. doi:10.1016/j.ajem.2024.04.031
Category: Critical Care
Keywords: ARDS (PubMed Search)
Posted: 6/16/2025 by Jordan Parker, MD
(Updated: 6/17/2025)
Click here to contact Jordan Parker, MD
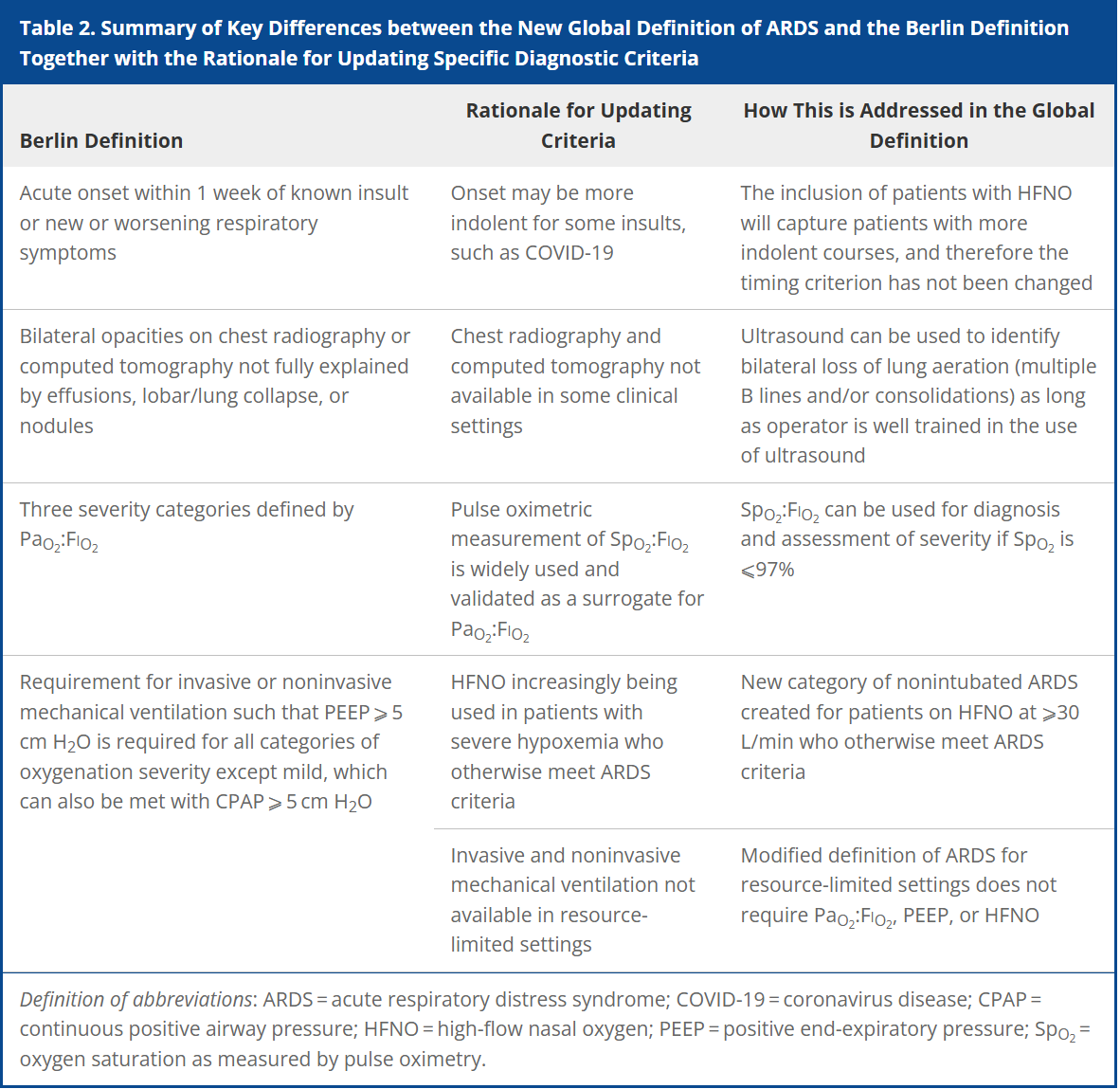
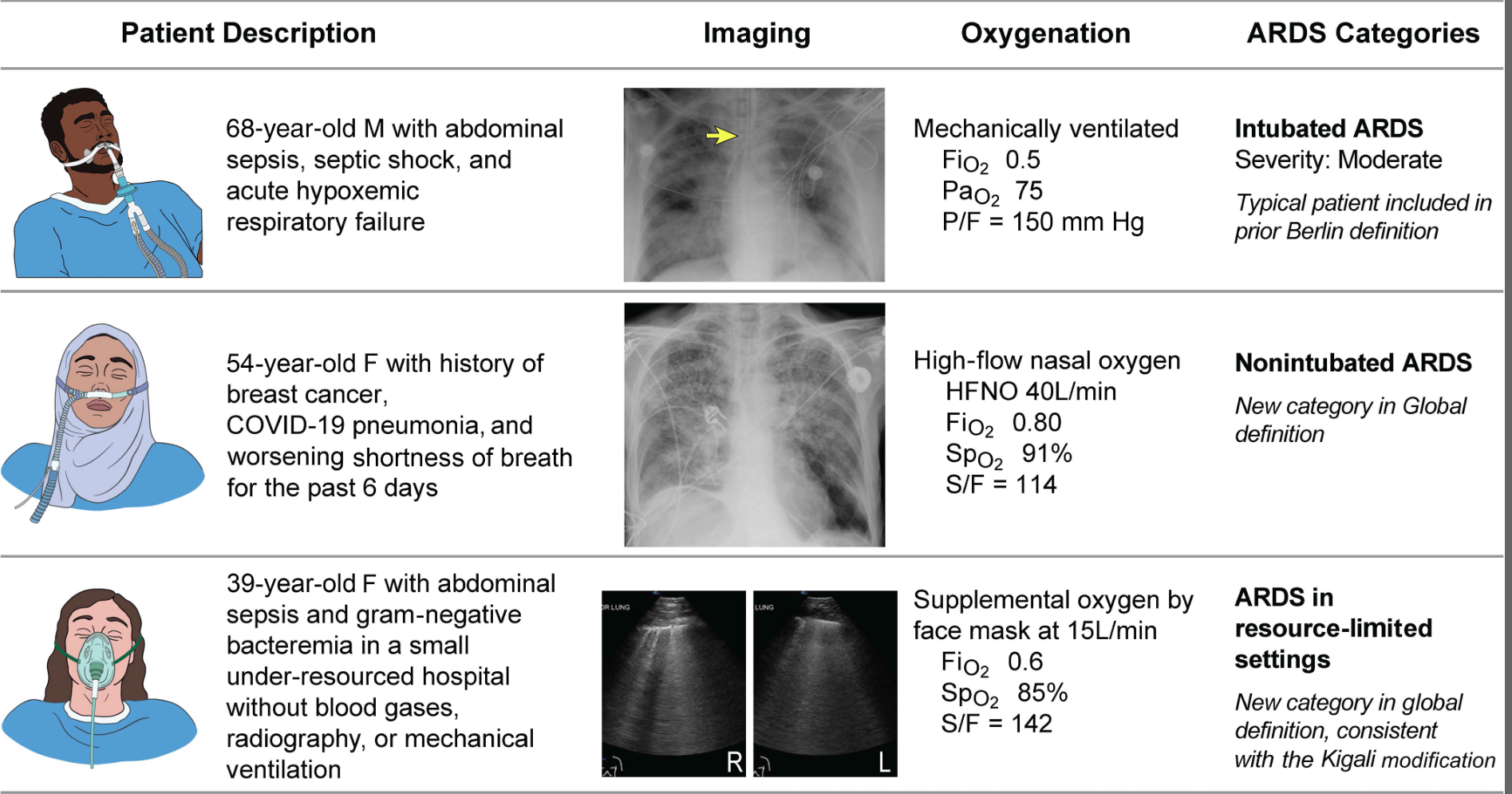
Acute respiratory distress syndrome (ARDS) is an acute, inflammatory lung injury that effects the lung diffusely and can be triggered by various insults. Aside from the Kigali modification, the most recent updated definition of ARDS was the Berlin definition in 2012. There have been many advances and changes in the understanding and clinical practice for managing patients with ARDS since then. In 2024, Matthay, et al. proposed the new global definition to build upon the Berlin criteria [1]. They addressed several important issues with the Berlin definition to improve the diagnostic criteria and improve ability for diagnosis in resource-limited settings.
ARDS Berlin Definition
Important updates for the Global definition of ARDS
Diagnostic Criteria for the New Global Definition of ARDS from Matthay et al.
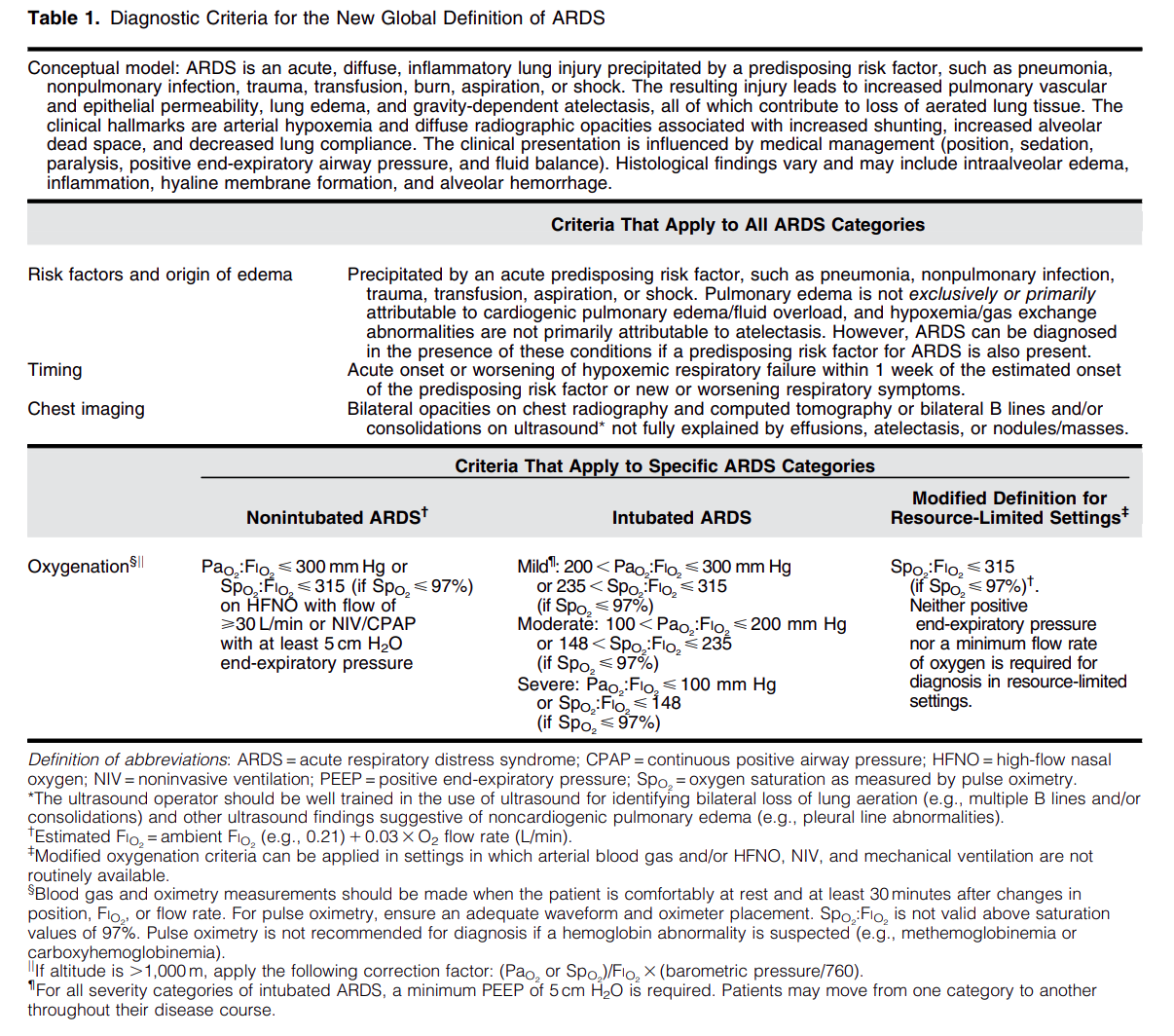
The Global Definition of ARDS expands upon the Berlin definition. It was shown that this new definition improves diagnosis in resource-limited settings, allows for earlier detection, and better classification [2]. A retrospective study evaluating this new global definition found that there was a significant number of patients identified using this new definition who would have been missed using the Berlin definition [3]. These patients may benefit from ARDS directed therapies and further prospective studies will be needed to assess how this new definition effects clinical management of these patients using the new definition.
Helpful table/figure from the paper.
Category: Ultrasound
Keywords: POCUS, Hip Effusion, MSK (PubMed Search)
Posted: 6/16/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
A hip effusion can cause pain with leg movement in both pediatric and adult patients.
A recent multicenter, prospective study assessed the diagnostic accuracy of POCUS performed by pediatric emergency physicians in detecting hip effusion.
They found that POCUS had a sensitivity of 89.3% (95% CI 80.6 to 95.0%) and specificity of 99.2% (95% CI 97.0 to 99.9%).
To scan the hip:
-Position the patient supine with the patient’s hip externally rotated.
-Place the probe transversely across the patient’s leg with the marker towards the patient’s right and scan proximally.
-Upon reaching the proximal femur, rotate the probe marker so it points towards the patient’s umbilicus.
-Look for an anechoic stripe at the femoral neck, preceding the femoral head.
An anechoic stripe measuring at least 5 mm in the anterior synovial space or an asymmetry exceeding 2 mm compared to the opposite, asymptomatic hip is diagnostic for hip effusion in BOTH pediatric and adult populations.
Jones RM, Malia L, Snelling PJ, Riera A, Mak W, Moote D, Brimacombe M, Chicaiza H. Diagnostic Accuracy of Point-of-Care Ultrasound for Hip Effusion: A Multicenter Diagnostic Study. Ann Emerg Med. 2025 Jun 7:S0196-0644(25)00279-3. doi: 10.1016/j.annemergmed.2025.04.033. Epub ahead of print. PMID: 40481828.
Category: Trauma
Keywords: Intubation, trauma, mortality, operating room, Ed (PubMed Search)
Posted: 6/15/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In this Israeli study comparing mortality for trauma patients intubated in the emergency department vs the operating room, in hospital mortality was higher for the ED group before controlling for injury severity score and shock. After controlling for injury severity and shock, there was no difference in In hospital mortality. Coupled with previous research, if intubation can wait until after resuscitation and in the OR, that is ideal. And sometimes it just has to happen in the ED and we should be prepared for rapid resuscitation.
Talmy T, Radomislensky I, Brzezinski Sinai I, Shaylor R, Katorza E, Gendler S; Israel Trauma Group Collaborators. Intubation Setting and Mortality in Trauma Patients Undergoing Hemorrhage Control Surgery: A Propensity Score-Matched Analysis. Anesth Analg. 2025 May 16. doi: 10.1213/ANE.0000000000007542. Epub ahead of print. PMID: 40378073.
Category: Orthopedics
Posted: 6/14/2025 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
NSAIDs are first line analgesic medications for many pain related ED presentations
All NSAIDs are not created equal in their side effect profile
Ibuprofen and ketorolac are both commonly used NSAIDs in the ED
A 2010 review looked at relative risk estimates of individual NSAIDs and associated upper GI bleeding/perforation.
Definitions: Most of included studies included patients with NSAID use within prior week and daignosed upper GI bleed admitted to the hospital.
Daily use predicted increased risk.
In comparison between these two common medications Ibuprofen and Ketorolac: RR as follows
Ibuprofen (2.69 [95% CI 2.17-3.33]) vs ketorolac (14.54 [95% CI 5.87-36.04])
Ketorolac has approximately double the half life of ibuprofen
Other commonly used ED medications were also included:
RRs:
Naproxen 5.63 (95% CI 3.83-8.28)
Indomethacin 5.40 (95% CI 4.16-7.00)
Meloxicam 4.15 (95% CI 2.59-6.64)
Diclofenac 3.98 (95% CI 3.36-4.72)
Conclusion: The risk of upper GI bleeding varies between individual NSAIDs at the doses commonly used in the general population. When possible, consider the relative risk of a particular NSAID when making a selection.
Massó González EL, Patrignani P, Tacconelli S, García Rodríguez LA. Variability among nonsteroidal antiinflammatory drugs in risk of upper gastrointestinal bleeding. Arthritis Rheum. 2010 Jun;62(6):1592-601.
Category: Pediatrics
Keywords: environmental, climate change, heat, pediatrics (PubMed Search)
Posted: 6/13/2025 by Kathleen Stephanos, MD
(Updated: 2/8/2026)
Click here to contact Kathleen Stephanos, MD
As the weather warms up, remember that pediatric patients have some physiologic factors that increase their risk of heat related complications. Approximately 37 infants die in cars annually, with risk of vehicular related heat illness starting with outdoor temperatures as low 72°F (32°C). Approximately 9,000 high school athletes require treatment for heat related illness annually with approximately 2 deaths per year.
Physiology:
Infants and young children have physiologically limited thermoregulation. They also may lack developmental abilities to impact their environment (they cannot ask for water, remove clothing or a seat belt, or move themselves to a cooler environment).
Older children take longer to acclimate to environments than their adult counterparts- requiring 10-14 days to adjust to work outs in higher temperatures (a gradual approach of increasing gear over time has been recommended for outdoor sports requiring padding or heavy equipment)
Management:
Heat exhaustion/stroke- focus on cooling the patient with temperatures being monitored with a core measurement. In teens and older children this can be done in a similar manner to adults- with removal of clothes, emersion therapy for heat stroke. In infants and young children, some experts favor evaporative management over emersion due to reflex bradycardia as well as patient compliance.
There are no recommended medications for use during heat stroke. Benzodiazepines may be utilized to present shivering or to treat seizures only if needed.
Prevention:
For athletes steps should include encouraging hydration (flavored drinks have been shown to increase consumption and improve hydration), developing strategies for acclimatization for athletes, and have materials present (ice baths) to intervene quickly for players with symptoms. For infants and young children car alarms or reminders, and practicing placing a needed item in the back seat can prevent parents from inadvertently leaving a child in a car.
Mangus CW, Canares TL. Heat-Related Illness in Children in an Era of Extreme Temperatures. Pediatr Rev. 2019 Mar;40(3):97-107. doi: 10.1542/pir.2017-0322. Epub 2019 Mar 1. PMID: 30824495.
Category: Pharmacology & Therapeutics
Keywords: sepsis, beta-lactam, vancomycin, antibiotic (PubMed Search)
Posted: 6/13/2025 by Alicia Pycraft
Click here to contact Alicia Pycraft
Background:
Early antibiotic administration is consistently linked to improved mortality outcomes in patients with sepsis. As a result, time-to-antibiotic delivery is a critical metric in hospital sepsis quality improvement initiatives. Empiric treatment often consists of a broad-spectrum beta-lactam to cover both gram-positive and gram-negative organisms, alongside vancomycin to ensure coverage of methicillin-resistant Staphylococcus aureus (MRSA). When multiple agents are indicated, they may be given simultaneously; however, factors such as limited intravenous (IV) access or drug incompatibilities can necessitate sequential administration. Administration of vancomycin first may delay the administration of a beta-lactam agent by at least 60-120 minutes due to its prolonged infusion time. This raises an important clinical question: Does the order in which antibiotics are administered influence outcomes in sepsis?
A 2022 retrospective study by Amoah et al. found that, among patients with confirmed bloodstream infections, a beta-lactam-first regimen was associated with a 52% reduction in the odds of short-term mortality compared to a vancomycin-first regimen. However, the generalizability of these findings to the broader population of patients with suspected sepsis, of whom only 15-20% ultimately have positive blood cultures, remains uncertain.
What's new?
A recent retrospective, multi-center, cohort study by Kondo et al. evaluated the impact of a beta-lactam-first antibiotic strategy compared to a vancomycin-first strategy on in-hospital mortality in patients with suspected sepsis. Of the 25,391 patients with sepsis who were screened, 21,449 (84.4%) received a beta-lactam first and 3,942 (15.6%) received vancomycin first. Patients who received vancomycin first had lower comorbidity burden, lower illness severity, more skin/musculoskeletal infections, and received beta lactams a median of 3.5 hours later relative to ED arrival compared to those who received a beta-lactam first. Although the overall rate of documented bloodstream infections was similar between groups, MRSA-positive cultures were more common in the vancomycin-first group, both in clinical cultures (4.5% vs. 3.2%) and in blood cultures (1.8 vs. 1.2%).
Beta-lactam administration prior to vancomycin was associated with an 11% reduction in the odds of in-hospital mortality (aOR: 0.89; 95% CI: 0.8-0.99; p=0.046). When the time-to-first antibiotic covariate was replaced with time-to-first beta-lactam, this association was no longer significant (aOR 0.93, 95% CI: 0.82-1.05, p=0.25), suggesting a possible link between time-to-first beta-lactam antibiotic and mortality. There was a trend toward lower in-hospital morality for the beta-lactam first regimen in several subgroups examined, including patients with positive blood cultures or positive MRSA cultures, and patients who received anti-pseudomonal beta-lactams; however, none reached statistical significance.
Bottom line:
Given the observed mortality benefit and absence of harm associated with a beta-lactam-first approach, even among patients with positive MRSA cultures, the findings of this study support the prioritization of beta-lactam therapy in patients with sepsis.
Category: Critical Care
Keywords: Cardiac Arrest, PEA, ROSC (PubMed Search)
Posted: 6/9/2025 by Harry Flaster, MD
Click here to contact Harry Flaster, MD
Pulse Checks in Cardiac Arrest: Your Fingers Are Not Reliable.
Summary: Whenever possible, use an ultrasound or an arterial line for pulse checks. Our fingers are not reliable.
Key points:
Multiple studies have demonstrated that manual pulse checks are not a reliable method to determine ROSC. Arterial lines and ultrasound are far more reliable methods. However, using more accurate measures of circulation lead to an additional dilemma: at what MAP, SBP, or ultrasound measured flow should we stop chest compressions? There is no agreed upon number, and as with most dilemmas in clinical medicine, the best answer is, “it depends”. However, a MAP > 50 or SBP > 60 for most patients is a reasonable choice to stop chest compressions. MAP < 50 or SBP < 60 are unlikely to provide adequate perfusion to the brain, and chest compressions should be resumed.
References:
Category: Obstetrics & Gynecology
Keywords: breech delivery (PubMed Search)
Posted: 6/9/2025 by Jennifer Wang, MD
(Updated: 2/8/2026)
Click here to contact Jennifer Wang, MD
Everyone clenches up when an imminent delivery shows up at the ED bay doors, even though most of these deliveries will not need intervention. Still, there are catastrophic ways delivery can go wrong, so today, let's talk about a new study on breech delivery.
The Study: Bogner et. al conducted a prospective single-center observational cohort study from 2006-2021 looking at breech deliveries in ~230 patients, with 92 of them being delivered in the traditional, supine way, while 140 of them delivered on all-fours. The only difference found between the two groups was that the all-fours group had heavier babies with bigger heads.
The Results: Over half (51.4%) of the patients in the all-fours position required no additional interventions from the provider compared to 11.9% of the supine group, and there were fewer perineal injuries. There was no increase in neonatal outcomes or NICU referrals in the all-fours group as compared to the supine group.
Limitations: Single center, no randomization, 11 patients started in all-fours and then had to switch to supine due to difficulty with delivery and prolonged second stage of labor, excluded footling breech
Takeaways: All-fours may be a position to consider for your patient with a breech delivery - especially if you haven't brushed up on your breech maneuvers recently.
Bogner G, Schuller J, Gargitter C, Dölzlmüller E, Fischer T, Fazelnia C. Vaginal breech delivery in all-fours position-Hands off instead of intervention: A prospective observational study. Acta Obstet Gynecol Scand. 2025;104(6):1153-1161. doi:10.1111/aogs.15078
Category: Trauma
Keywords: Hysterotomy (PubMed Search)
Posted: 6/8/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Another case series of 3 resuscitative hysterotomies, all performed by obstetricians, reported 33% maternal and 67% neonate survival.(1).
The mechanics of the procedure are:
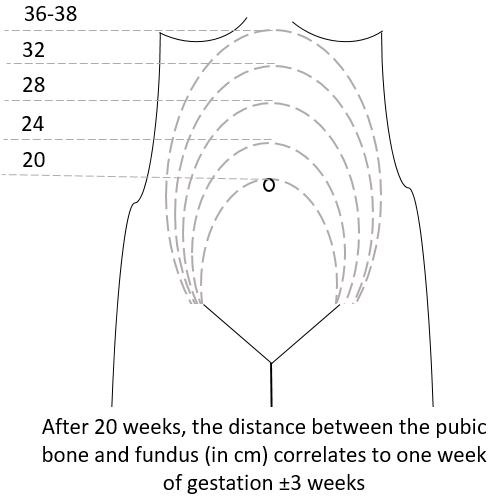
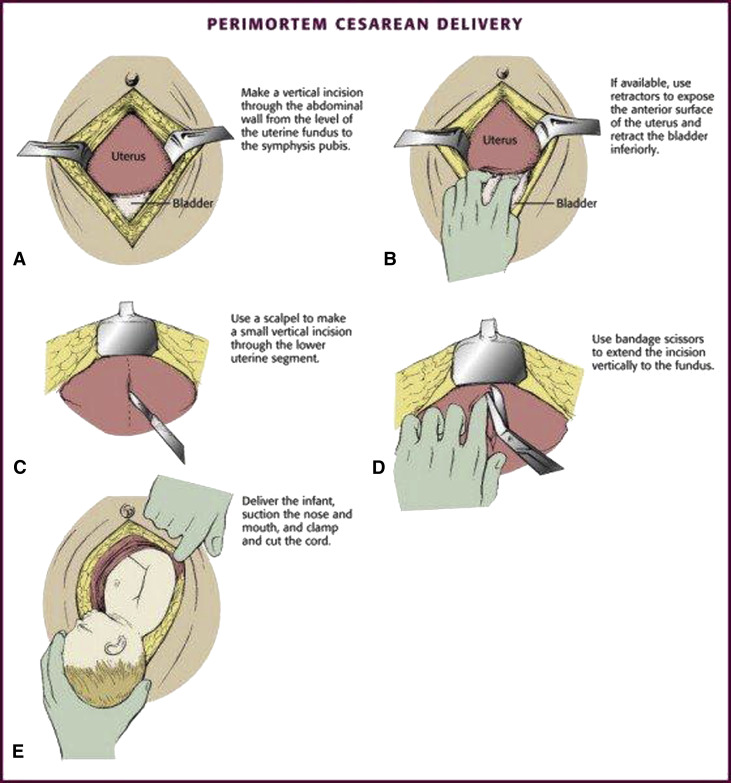
(3)
Category: Trauma
Posted: 6/7/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
A literature search revealed very little evidence, however in 66 women and 68 neonates who underwent resuscitative hysterotomy for out of hospital cardiac arrest 4.5% of women and 45% of neonates survived to discharge. The longest down time was 29 minutes and 47 minutes for women and neonates respectively. While more evidence is needed, it appears this procedure should be performed as early as possible and may lead to some survival benefit.
Leech C, Nutbeam T, Chu J, Knight M, Hinshaw K, Appleyard TL, Cowan S, Couper K, Yeung J. Maternal and neonatal outcomes following resuscitative hysterotomy for out of hospital cardiac arrest: A systematic review. Resuscitation. 2025 Feb;207:110479. doi: 10.1016/j.resuscitation.2024.110479. Epub 2024 Dec 29. PMID: 39736393.
Category: Neurology
Keywords: ischemic stroke, thrombolysis, tpa, intracranial hemorrhage (PubMed Search)
Posted: 6/6/2025 by Nicholas Contillo, MD
(Updated: 2/8/2026)
Click here to contact Nicholas Contillo, MD
Acute ischemic strokes involving the posterior circulation have significantly lower rates of hemorrhagic transformation after thrombolysis compared to anterior circulation strokes, a difference attributed to smaller infarct sizes and greater “ischemic tolerance” in the posterior circulation.
Given this lower hemorrhage risk, the EXPECTS trial evaluated the safety and efficacy of extending the thrombolysis window to 4.5–24 hours in patients with acute posterior circulation ischemic stroke who were not candidates for endovascular thrombectomy. This randomized controlled trial, conducted across 30 sites in China, enrolled 234 adults with mainly mild posterior circulation stroke (median NIHSS 3) and no evidence of extensive infarction on CT. Participants were randomized to receive either intravenous alteplase or standard medical care within the 4.5–24 hour window after symptom onset.
The primary outcome of functional independence at 90 days (modified Rankin Scale 0–2) was achieved in 89.6% of the alteplase group versus 72.6% of the standard care group. Rates of symptomatic intracranial hemorrhage were low and similar between groups (1.7% alteplase vs. 0.9% standard care), and 90-day mortality was lower in the alteplase group (5.2% vs. 8.5%).
These findings support extending the therapeutic window for intravenous thrombolysis in posterior circulation stroke beyond 4.5 hours when thrombectomy is not an option. However, the trial’s limitations, including a study population predominantly with mild strokes, exclusion of patients with extensive infarction, and enrollment limited to Chinese centers, warrant further investigation in larger and more diverse populations.
Bottom Line: Within limitations, emerging evidence supports an extended thrombolytic window beyond 4.5 hours for patients with posterior circulation strokes who are ineligible for thrombectomy.
Yan S, Zhou Y, Lansberg MG, Liebeskind DS, Yuan C, Yu H, Chen F, Chen H, Zhang B, Mao L, Zhang X, Wang X, Zhang X, Chen Y, Zhou H, Zhong W, He Y, Chen K, Wang J, Chen H, Huang Y, Campbell BCV, Lou M; EXPECTS Group. Alteplase for Posterior Circulation Ischemic Stroke at 4.5 to 24 Hours. N Engl J Med. 2025 Apr 3;392(13):1288-1296. doi: 10.1056/NEJMoa2413344. PMID: 40174223.
Category: Trauma
Keywords: Femur fracture, splint (PubMed Search)
Posted: 6/6/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
The National Association of Emergency Medical Service Physicians reminds us that femur fractures rarely cause enough blood loss to cause hemodynamic instability (look for other sources), often have concomitant injuries in the pelvis or distal extremity, and can be effectively splinted either static or with traction (which has contraindications, complications, and technical hurdles).
John W. Lyng, Joshua G. Corsa, Philip S. Nawrocki, Brad D. Raetzke, Josh
Nackenson & Nichole Bosson (07 May 2025): Prehospital Trauma Compendium: Management
of Suspected Femoral Shaft Fractures – A position statement and resource document of
NAEMSP, Prehospital Emergency Care, DOI: 10.1080/10903127.2025.2493846
To link to this article: https://doi.org/10.1080/10903127.2025.2493846
Category: Critical Care
Keywords: OHCA, shockable rhythms, VF, ventricular fibrillation, defibrillation, AED, energy (PubMed Search)
Posted: 6/4/2025 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
A recent retrospective cohort study out of China investigated an escalating energy (200 > 300 > 360J) versus fixed energy (200 > 200 > 200 J) defibrillation strategy in OHCA with ventricular fibrillation requiring repeated defibrillations.
Notes:
Results:
Caveats:
