Category: Critical Care
Keywords: Noninvasive Ventilation, BiPAP, hypoxic respiratory failure (PubMed Search)
Posted: 5/6/2025 by Mark Sutherland, MD
(Updated: 2/7/2026)
Click here to contact Mark Sutherland, MD
Duan et al recently published in Intensive Care Medicine the results of a trial looking at a PEEP of 5 cm H2O vs 10 cm H2O and impact on failure rate (progression to intubation) when using non-invasive ventilation (NIV). In their trial, the high PEEP group had a lower rate of intubation (32% vs 43%), and this was statistically significant. It is important to note that they excluded patients whose indication for NIV was heart failure, asthma, or COPD exacerbation.
Ultimately, how to choose the right PEEP is a very complex question and requires tailoring to your patient's physiology and clinical circumstances. For example, hypercarbic patients may benefit more from a maximization of their driving pressure (Pplat - PEEP), which can involve lowering their PEEPs, especially when trying to avoid gastric insufflation (remember, pressures of 30 cm of H2O or higher are very likely to open the LES).
Bottom Line: PEEP and other vent settings should be tailored to the patient's pathophysiology, but this trial suggests that in hypoxemic patients not getting NIV for heart failure, asthma, or COPD exacerbation, a higher PEEP (10 vs 5) may reduce the risk of intubation.
Duan, J., Liu, X., Shu, W. et al. Low versus high positive end expiratory pressure in noninvasive ventilation for hypoxemic respiratory failure: a multicenter randomized controlled trial. Intensive Care Med (2025). https://doi-org.proxy-hs.researchport.umd.edu/10.1007/s00134-025-07902-4
Category: Ultrasound
Keywords: Point-of-care ultrasound; Cholecystitis; Gallbladder distention; Biliary ultrasound (PubMed Search)
Posted: 5/5/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/7/2026)
Click here to contact Alexis Salerno Rubeling, MD
The normal gallbladder dimensions on ultrasound are approximately 3 cm in width by 10 cm in length.
A recent study evaluated the diagnostic test characteristics of gallbladder distension on POCUS for cholecystitis.
The authors conducted a retrospective cohort study of 227 patients who were admitted to the hospital after undergoing a POCUS biliary study in the emergency department.
They found the prevalence of gallbladder distension to be 30% in their study population. When combined with other sonographic findings, the presence of distension increased the specificity for cholecystitis to 95.6%.
Gallbladder wall distension was associated with the presence of an obstructing stone in the gallbladder neck and with acute cholecystitis.
Additionally, gallbladder wall distension was associated with longer operative times (mean 114 minutes) compared to those without distension (mean 89 minutes; p=0.03), suggesting more severe disease and potentially more complex surgical intervention.
Bottom Line: When gallbladder wall distension is present, it is important to carefully evaluate the gallbladder neck for signs of an obstructing stone.
Cannata D, Chin KA, Anslip A, et al. Association of biliary distention with a diagnosis of acute cholecystitis. Am J Emerg Med. 2024 Jul;81:130-135. doi: 10.1016/j.ajem.2024.04.056.
Category: Cardiology
Keywords: aorta, dissection (PubMed Search)
Posted: 5/3/2025 by Robert Flint, MD
(Updated: 5/4/2025)
Click here to contact Robert Flint, MD
Aortic dissection remains a difficult diagnosis to make. This article is a nice review. The pathology behind this involves an intimal flap in the aortic wall. Death occurs due to aortic rupture or obstruction of branching artery.
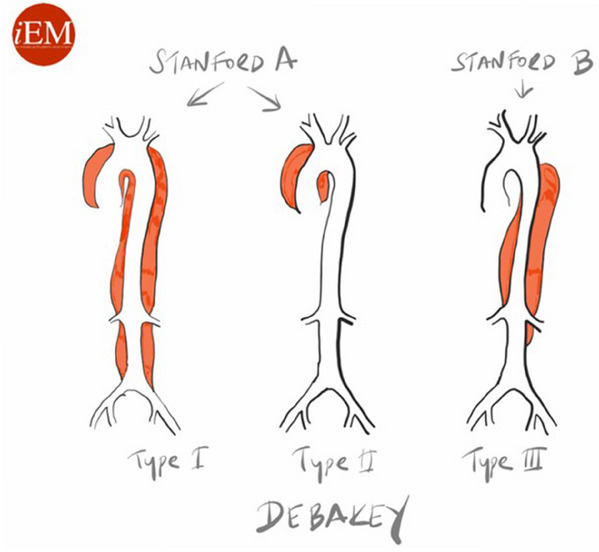
Risk factors: male 2:1 female, Marfan Syndrome, HTN, aortic aneurysm, cocaine and methamphetamine use, pregnancy
Pain is variable however tearing, ripping migrating, maximum at onset, and sharp are all associated with Aortic Dissection. Think about Dissection with atypical CP with ECG changes as well as in stroke like presentations along with chest pain.
Gold standard for diagnosis is CT angiogram. Decision rules with the use of D-Dimer have been proposed however there is still not sufficient evidence to use these. ACEP guidelines currently give use of decision rules a long with DDImer a level C recommendation.
Briggs, Blake et al.
JACEP Open, Volume 5, Issue 4, e13225
Category: Obstetrics & Gynecology
Keywords: Bacterial vaginosis (PubMed Search)
Posted: 5/3/2025 by Michele Callahan, MD
Click here to contact Michele Callahan, MD
A study published in the NEJM (March 2025) looked at recurrence of bacterial vaginosis at 12 weeks in two groups: a control group where women received standard treatment but male partners were not treated, and a partner-treatment group. In the partner-treatment group, women received standard treatment, and the male partner received both oral and topical treatment. Male partners in this study received Metronidazole 400 mg BID x 7 days in addition to 2% topical clindamycin cream applied to penile skin BID x 7 days. The trial was actually stopped early as it was found that only treating the female was inferior to treatment of both.
This study concluded that treatment of both the female and male partners led to significantly decreased recurrence of bacterial vaginosis within 12 weeks (35% with dual treatment vs. 65% with female-only treatment). This study suggests that we should consider offering treatment to both sexual partners for patients presenting with bacterial vaginosis.
Category: Critical Care
Posted: 4/29/2025 by Mike Winters, MBA, MD
(Updated: 2/7/2026)
Click here to contact Mike Winters, MBA, MD
Sedation for the Mechanically Ventilated Adult ICU Patient
Lewis K, et al. Executive summary of a focused update to the clinical practice guidelines for the prevention and management of pain, anxiety, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2025; 53:e701-e710.
Category: Trauma
Keywords: Gun violence, mental health, suicide (PubMed Search)
Posted: 4/28/2025 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This study looked at exposure to gun violence and found increased use of mental health resources, depression and suicide risk even with a single exposure. Repetitive exposure increased suicide risk as well as mental health service utilization, depression and overall health service utilization. While further work is needed, screening our patients for gun violence exposure could undercover mental health needs.
Daniel C. Semenza, Allison E. Bond, Devon Ziminski, Michael D. Anestis,
Frequency, recency, and variety of gun violence exposure: Implications for mental health and suicide among US adults,
Social Science & Medicine,
Volume 366,
2025,
117672,
ISSN 0277-9536,
https://doi.org/10.1016/j.socscimed.2025.117672.
(https://www.sciencedirect.com/science/article/pii/S0277953625000012
Category: Infectious Disease
Keywords: Necrotizing infection, antibiotic selection (PubMed Search)
Posted: 4/27/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
In the April edition of Annals of EM, there are opposing view points on the optimal antibiotic regiment for necrotizing soft tissue infection. One group proposes linezolid alone will cover all the worrisome pathogens namely group A Strep and Staph. There are less side effects including C. Diff infection with this medication. Another group suggests sticking to vancomycin plus/minus BLactam along with clindamycin. Their arguement centers around clindamycin is useful as an antitoxin more so than its antibacterial property.
Both offer reasonable evidence and neither is compelling enough to say one is superior to the other.
Optimal antibiotic Selevtion for Necrotizing soft tissue infections. Annals of Emergency Medicine. April 2025. Vol 8, No. 4 358-360
Category: Cardiology
Keywords: Brugada, ECG, hyperkalemia (PubMed Search)
Posted: 4/26/2025 by Visiting Speaker
(Updated: 2/7/2026)
Click here to contact Visiting Speaker
Pseudo-Brugada pattern in hyperkalemia
Category: ECG
By: Chuck Siegel
Keywords: Brugada sign, hyperkalemia, ECG, arrhythmia
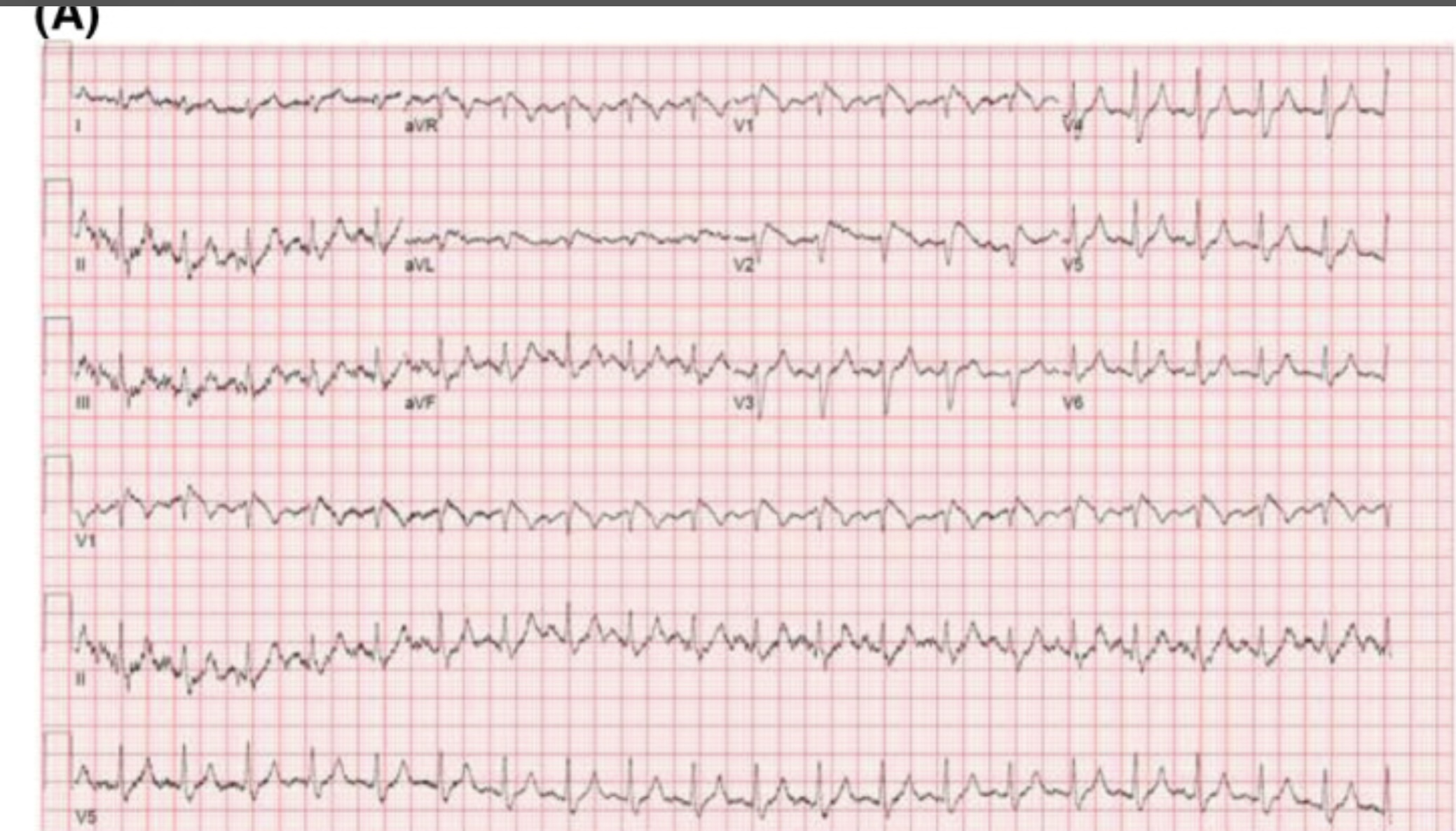
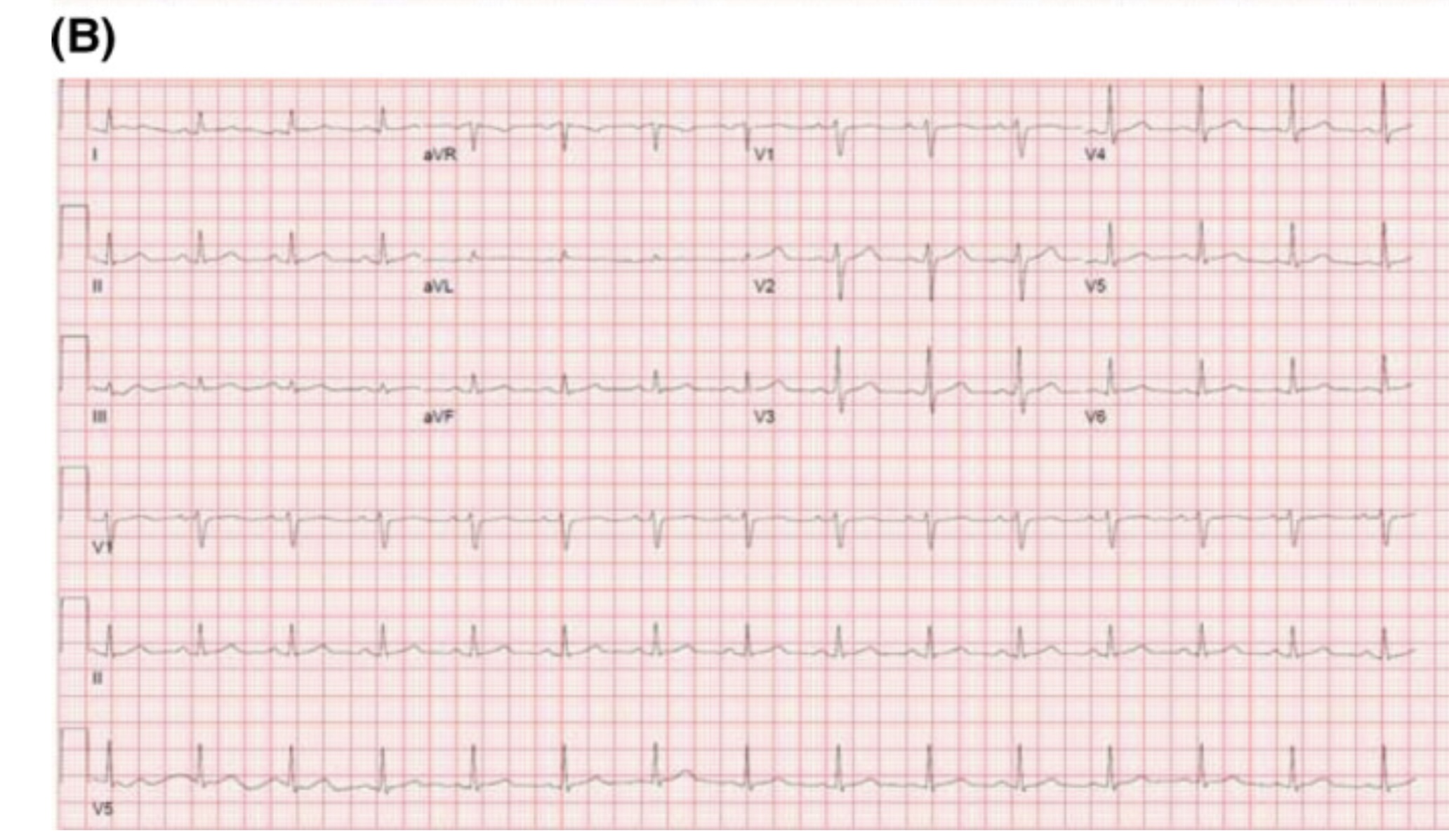
Hyperkalemia can produce a variety of ECG changes, including well-known changes such as peaked t-waves, QRS widening, PR-interval prolongation, loss of the p-waves, and the sine wave morphology. One change not as commonly seen is coved ST-elevation in V1-V3 that mimics the ECG changes associated with Brugada sign. Unlike Brugada syndrome, these ECG changes are transient and resolve upon treatment of the hyperkalemia.
The mechanism of these ECG findings relate to the elevated extracellular potassium’s inactivating effect on sodium channels, similar to the sodium channelopathy found in Brugada syndrome. The mean serum potassium concentration of reported cases is often above 6.5 mEq/L. Importantly, hyperkalemia-induced Brugada pattern has not been associated with sudden cardiac death or ventricular arrhythmias.
An example of a hyperkalemia-induced pseudo Brugada pattern in a patient with a K of 7.2 mEq/L (A) as well as that same patient’s ECG following treatment of their hyperkalemia (B).
References
Manne JRR, Garg J. Hyperkalemia induced Brugada phenocopy. J Arrhythm. 2021 Jan 7;37(1):249-250. doi: 10.1002/joa3.12498. PMID: 33664911; PMCID: PMC7896447.
Alnajjar AZ, Ibrahim AI, Ellebedy M. Hyperkalemia-induced Brugada phenocopy: a systematic review of case reports. Clin Res Cardiol. 2025 Feb 18. doi: 10.1007/s00392-025-02607-6. Epub ahead of print. PMID: 39964614.
Xu G, Gottschalk BH, Anselm DD, Benditt DG, Maheshwari A, Sreenivasan S, Shama RA, Dendramis G, Barajas-Martínez H, Rubio Campal JM, Aznaurov SG, Baranchuk A. Relation of the Brugada Phenocopy to Hyperkalemia (from the International Registry on Brugada Phenocopy). Am J Cardiol. 2018 Mar 15;121(6):715-717. doi: 10.1016/j.amjcard.2017.12.008. Epub 2017 Dec 29. PMID: 29397883.
Rivera-Juárez A, Hernández-Romero I, Puertas C, Zhang-Wang S, Sánchez-Álamo B, Martins R, Figuera C, Guillem MS, Climent AM, Fernández-Avilés F, Tejedor A, Jalife J, Atienza F. Clinical Characteristics and Electrophysiological Mechanisms Underlying Brugada ECG in Patients With Severe Hyperkalemia. J Am Heart Assoc. 2019 Feb 5;8(3):e010115. doi: 10.1161/JAHA.118.010115. PMID: 30675825; PMCID: PMC6405573.
Category: Administration
Keywords: CT scanning, cancer risk, administration, EMR, diagnostic algorithms (PubMed Search)
Posted: 4/23/2025 by Steve Schenkel, MPP, MD
(Updated: 2/7/2026)
Click here to contact Steve Schenkel, MPP, MD
You may have seen the headline.
93 million CT examinations conducted on 62 million US patients in 2023 projected to lead to 103000 new cancer diagnoses accounting for 5% of new cancers.
The details of the modeling can be found here, https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2832778.
What does this have to do with administration?
The solutions rely on administrative involvement:
There’s an editorial here, https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2832782 and a commentary with interviews that put the findings nicely in context here https://arstechnica.com/health/2025/04/ct-scans-could-cause-5-of-cancers-study-finds-experts-note-uncertainty/ (including pointing out that lifetime risk of cancer in the US is 40% and the increase from CT scanning on the order of 0.1% / scan).
Smith-Bindman R, Chu PW, Firdaus HA, et al. Projected lifetime cancer risks from current computed tomography imaging. JAMA Intern Med 2025; doi:10.1001/jamainternmed.2025.0505.
Category: Critical Care
Posted: 4/22/2025 by Cody Couperus-Mashewske, MD
Click here to contact Cody Couperus-Mashewske, MD
This large RCT compared High-Flow Nasal Oxygen (HFNO) against Noninvasive Ventilation (NIV) via face mask in 5 types of Acute Respiratory Failure (ARF): non-immunocompromised hypoxemia, immunocompromised hypoxemia, COPD with acidosis, acute cardiogenic pulmonary edema (ACPE), and COVID-19.
Bottom Line:
RENOVATE suggests HFNO might be a reasonable, more comfortable initial choice for non-immunocompromised hypoxemic ARF or COVID-19 ARF. However, exercise caution using HFNO first-line for COPD exacerbations with acidosis or immunocompromised hypoxemic ARF due to conflicting analyses and potential harm signals. The signal for HFNO benefit in ACPE is intriguing but needs confirmation before changing practice. Close monitoring for failure and timely escalation are essential regardless of the initial noninvasive strategy.
High-flow nasal oxygen vs noninvasive ventilation in patients with acute respiratory failure: the RENOVATE randomized clinical trial RENOVATE Investigators and the BRICNet Authors, Maia IS, Kawano-Dourado L, et al. JAMA. Published online December 10, 2024. doi:10.1001/jama.2024.26244
Category: Trauma
Keywords: Rural trauma care (PubMed Search)
Posted: 4/19/2025 by Robert Flint, MD
(Updated: 4/20/2025)
Click here to contact Robert Flint, MD
This study looking at the type of facility that cared for rural injured patients reminds us that the majority of trauma care for rural patients occurs in non-trauma centers. This included some of the most severely injured and for many definitive care was received at these centers.
This may lead to lack of inclusion in trauma registries and under valuing the care being delivered by non-trauma centers. Protocols to facilitate transfers, air medical protocols and availability along with tele-health all are important in rural trauma care. Non-trauma designated centers are a critical part of the trauma network for rural residents and their value can not be ignored.
Kaufman, Elinore J. MD, MSHP*; Prentice, Carter MD†; Williams, Devin BA‡; Song, Jamie MPH§; Haddad, Diane N. MD, MPH§; Brown, Joshua B. MD, MSc?; Chen, Xinwei MS¶; Colling, Kristin MD#; Chatterjee, Paula MD, MPH¶
Annals of Surgery 281(4):p 533-539, April 2025. | DOI: 10.1097/SLA.0000000000006540
Category: Administration
Posted: 4/19/2025 by Kevin Semelrath, MD
(Updated: 2/7/2026)
Click here to contact Kevin Semelrath, MD
This study was the first look at the author's experiences with racial disparities in head and neck trauma in children. It looked at community EDs, and found that white children were more likely to be diagnosed with concussion compared to black children. White children were more likely to be seen as a result of sports or motor vehicle accidents, while black children were more likely to be seen as a result of an assault.
This study revealed the need for further research into the cause of the disparities in care that they identified.
Wallace, Jessica et al.
Journal of Emergency Medicine, Volume 59, Issue 6, 783 - 794
Category: Pediatrics
Keywords: literature updates, PED, evidence based medicine (PubMed Search)
Posted: 4/1/2025 by Jenny Guyther, MD
(Updated: 4/18/2025)
Click here to contact Jenny Guyther, MD
Have you been wondering what the latest pediatric emergency medicine lecture says?
See the attached table from this review which highlights the 10 top articles from 2024 with their key findings!
Rose E, Easter JS. Pediatric emergency 2024 updates. Am J Emerg Med. 2025 Feb 16;91:13-24. doi: 10.1016/j.ajem.2025.02.019. Epub ahead of print. PMID: 39983287.
Category: EMS
Keywords: cardiac arrest, EMS, TOR (PubMed Search)
Posted: 4/16/2025 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
Pulseless electrical activity (PEA) is the initial rhythm in up to 25% of out of hospital cardiac arrests.
This paper is a systemic review and analysis examining if the rate or width of the initial PEA qrs complex was associated with survival. The qrs complex was either wide (>= 120 ms) or narrow (<120ms) and a frequency of fast (>= 60/s) or slow (<60/s). 7 studies including 9727 patients were included. Analysis showed:
- mortality was higher in the wide qrs group compared to narrow
- mortality was higher in the slow PEA rate compared to fast
- neurological outcome was better in patients with a fast PEA rate compared to slow.
Kim JH, Lee J, Shin H, et al. Association Between QRS Characteristics in Pulseless Electrical Activity and Survival Outcome in Cardiac Arrest Patients: A Systematic Review and Meta-Analysis. Prehosp Emerg Care. Published online June 3, 2024. doi:10.1080/10903127.2024.2360139
Category: Obstetrics & Gynecology
Posted: 4/13/2025 by Jennifer Wang, MD
(Updated: 4/15/2025)
Click here to contact Jennifer Wang, MD
Emergency contraception comes in multiple forms, all of which have their own side effects and best case use scenarios that emergency medicine providers should be aware of to offer the best counseling.
Consider your patient before advising - if their BMI is > 25, consider ulipristal. If they want the most effective method, that'll be a copper IUD - but make sure they can get an appointment within 5 days of the unprotected intercourse! If they cannot afford ulipristal or levonorgestrel (which can both be $50 without insurance), but they already have OCPs, combining OCPs to the total noted above can be a method of emergency contraception that is still very effective.
Mazer-Amirshahi M, Ye P. Emergency contraception in the emergency department. Am J Emerg Med. 2023;63:102-105. doi:10.1016/j.ajem.2022.10.034
Rudzinski P, Lopuszynska I, Pazik D, et al. Emergency contraception - A review. Eur J Obstet Gynecol Reprod Biol. 2023;291:213-218. doi:10.1016/j.ejogrb.2023.10.035
Category: Critical Care
Posted: 3/22/2025 by Jordan Parker, MD
(Updated: 4/15/2025)
Click here to contact Jordan Parker, MD
Background:
Acetaminophen can reduce hemoprotein induced oxidative damage. There has been growing discussion about its benefits in critically ill patients with sepsis. Multiple observational studies have found conflicting results on mortality in critically ill patients with sepsis. The ASTER trial found no difference in number of days alive and free of organ support. Interestingly their secondary outcomes found significantly less development of ARDS in the acetaminophen group 2.2% vs 8.5%, p = .01. There was also a non-statistically significant difference in mortality between the groups in favor of the acetaminophen group, 17% vs 22% p = 0.19. This study looked to further evaluate if acetaminophen used in critically ill patients with sepsis would have a decrease in mortality and increase in ventilator free days.
Study:
- Retrospective analysis of the Ibuprofen in Sepsis Study (ISS)
- The ISS was a randomized clinical trial comparing ibuprofen with placebo in critically ill patients with sepsis. Careful documentation of Acetaminophen use was recorded for the trial
- Critically-ill adults across 7 ICU’s in the US and Canada with known or suspected infection and severe organ dysfunction
- Acetaminophen use within 48 hours of enrollment = Acetaminophen exposed
- Primary outcome: 30-day mortality
- Secondary outcome: Renal failure and ventilator free days up to day 28
- 455 patients. 172 Acetaminophen unexposed, 235 Acetaminophen exposed.
Results:
- Propensity-matched analysis showed a lower mortality risk at 30 days in patients exposed to acetaminophen compared to unexposed, 32% vs 49% (HR 0.58, p .004)
- Secondary outcomes found acetaminophen exposed group had more ventilator free days (p .02) but there was no difference in renal failure among the groups.
Limitations:
- Major risk for confounding variables
- Retrospective and the data used was from decades ago (1989 -1995). Sepsis care has evolved and improved since this time
- Dose and frequency of acetaminophen administration was not standardized
Take Home Points:
- Interesting research that provides further support on the possible benefit to using acetaminophen in the management of critically ill patients with sepsis.
- With the ASTER trial showing a signal for the decrease in development of ARDS and this study showing improvement in mortality one could make a case for starting acetaminophen early in the course for these patients. However, the data is conflicting and more prospective, RCT’s are needed to confirm these findings before making this a staple for sepsis care in critically ill patients.
Obeidalla, S. N., Bernard, G. R., Ware, L. B., & Kerchberger, V. E. Acetaminophen and Clinical Outcomes in Sepsis: A Retrospective Propensity Score Analysis of the Ibuprofen in Sepsis Study. CHEST Critical Care. 2025;3(1):100-118. https://doi.org/10.1016/j.chstcc.2024.100118
Ware LB, Files DC, Fowler A, et al. Acetaminophen for Prevention and Treatment of Organ Dysfunction in Critically Ill Patients With Sepsis: The ASTER Randomized Clinical Trial. JAMA. 2024;332(5):390–400. doi:10.1001/jama.2024.8772
Category: Trauma
Keywords: Mental health, trauma, intervention, blunt injury (PubMed Search)
Posted: 4/13/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
This study looked at pre-trauma mental health diagnosis (from medical records) and post-trauma mental health symptoms as assessed by survey. The majority of patients suffered blunt trauma and mean age was 67. Having pre/traumatic mental health diagnosis and particularly post-traumatic symptoms lead to worse health outcomes and financial conditions. Further work needs to be done to assess how to improve mental health symptoms post-traumatic injury.
Johnson, Patrick L. MD, MPH; Hemmila, Mark R. MD; Mullens, Cody L. MD, MPH; Oliphant, Bryant W. MD, MBA, MSc; Monahan, Janessa R. MS; Kelm, Julia D. BS; Jakubus, Jill L. PA-C, MHSA, MS; Curtiss, William J. MD; Mosher, Benjamin D. MD; Kieninger, Alicia N. MD; Scott, John W. MD, MPH
Journal of Trauma and Acute Care Surgery 98(3):p 425-434, March 2025. | DOI: 10.1097/TA.0000000000004521
Category: Orthopedics
Posted: 4/12/2025 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Non benzodiazepine muscle relaxants
Muscle relaxants were the most commonly (32%) prescribed medication upon discharge from the ED for lower back pain.
Muscle relaxants, such as cyclobenzaprine, provide short term pain-relief for patients with acute low back pain compared to placebo.
There is little difference in efficacy among the various muscle relaxants.
Evidence for muscle relaxants for back pain is weak compared to NSAIDs, so limit use to patients who have contraindications to NSAIDS.
There is no strong evidence that combination therapy with NSAIDs is more effective than NSAIDs alone.
If using during the day, consider using a lower dose (cyclobenzaprine 5mg) and a higher dose at night (10mg).
If treating with NSAIDs, consider using only at night to promote sleep.
Also, limit use to those patients who can tolerate the side effect profile of muscle relaxants, which include anticholinergic effects, dizziness, and sedation.
Risks of these agents increase with age, so should be used with caution in older adults.
Often given to this population due to fears of NSAID side effects.
Friedman et al., 2019. Annals of Emergency Medicine
A Randomized, Placebo-Controlled Trial of Ibuprofen Plus Metaxalone, Tizanidine, or Baclofen for Acute Low Back Pain.
Category: Pediatrics
Keywords: Pediatrics, seizures, adolescent, myolonic jerks (PubMed Search)
Posted: 4/11/2025 by Kathleen Stephanos, MD
Click here to contact Kathleen Stephanos, MD
Presentation:
JME is a common cause of juvenile/adolescent seizures.
Patients typically present between 12-18 years of age with a combination of myoclonic movements, absence seizures and generalized tonic-clonic seizures.
This diagnosis is often mistaken for morning clumsiness due to the myoclonic movements and asking about myoclonic movements can help make the diagnosis.
Diagnosis:
Diagnosis is primarily based on history. Myoclonic seizures are required to make the diagnosis. Patients with consistent history can receive outpatient EEG to confirm the diagnosis.
No ED images or tests needed with the correct clinical history and return to baseline. (even outpatient with appropriate history imaging is not needed as it is usually normal)
Treatment:
Valproic acid is typically the treatment of choice for patients though must be used with caution in women of childbearing age. Other common treatment options include levetiracetam and lamotrigine. With the correct clinical history, these can be started in the ED.
Be sure to discuss good sleep hygiene and avoidance of alcohol with patients as these can be triggers.
Mantoan L, Walker M. Treatment options in juvenile myoclonic epilepsy. Curr Treat Options Neurol. 2011 Aug;13(4):355-70. doi: 10.1007/s11940-011-0131-z. PMID: 21494841.
Category: Pharmacology & Therapeutics
Keywords: Albuterol, Lactate (PubMed Search)
Posted: 4/10/2025 by Wesley Oliver
(Updated: 2/7/2026)
Click here to contact Wesley Oliver
Albuterol, a common bronchodilator used in the treatment of asthma and chronic obstructive pulmonary disease (COPD), can cause a surprising increase of lactate levels. The increase in lactate is usually mild to moderate (typically < 4 mmol/L) and transient. It does not necessarily indicate underlying sepsis, tissue hypoxia, or severe metabolic acidosis.
Mechanism:
Albuterol can cause a transient increase in lactate levels due to its beta-2 agonist effects, which promote glycogenolysis and increase anaerobic metabolism. This can result in elevated lactic acid production, even in the absence of tissue hypoxia or shock.
Timing:
This effect is typically seen within 30 minutes of albuterol administration and can persist for 1-2 hours after discontinuing treatment.
Monitoring:
If lactate levels are elevated in a patient receiving albuterol, consider the possibility of a pharmacologic cause rather than immediately assuming a more serious etiology like shock or severe metabolic disturbance.
Differentiating Causes of Elevated Lactate:
In a critically ill patient, elevated lactate can indicate hypoperfusion (e.g., septic shock, cardiogenic shock, or hypovolemic shock). However, when elevated lactate is associated with albuterol administration, the rise in lactate is often lower and resolves without intervention.
Management:
If albuterol-induced lactate elevation is suspected, continue with supportive care and monitor lactate trends. No specific treatment is necessary for the elevated lactate unless there are other concerning clinical findings that suggest a different underlying cause.
Conclusion:
In emergency settings, it's important to recognize that albuterol can cause a transient increase in lactate levels. Understanding this phenomenon can help avoid misdiagnosis and prevent unnecessary interventions in patients receiving albuterol therapy. Always correlate lactate levels with the broader clinical picture to guide management decisions.
Hockstein M, Diercks D. Significant Lactic Acidosis from Albuterol. Clin Pract Cases Emerg Med. 2018 Mar 14;2(2):128-131. doi: 10.5811/cpcem.2018.1.36024. PMID: 29849230.
Lewis LM, Ferguson I, House SL, Aubuchon K, Schneider J, Johnson K, Matsuda K. Albuterol administration is commonly associated with increases in serum lactate in patients with asthma treated for acute exacerbation of asthma. Chest. 2014 Jan;145(1):53-59. doi: 10.1378/chest.13-0930. PMID: 23949578.
Liedtke AG, Lava SAG, Milani GP, Agostoni C, Gilardi V, Bianchetti MG, Treglia G, Faré PB. Selective ß2-Adrenoceptor Agonists and Relevant Hyperlactatemia: Systematic Review and Meta-Analysis. J Clin Med. 2019 Dec 27;9(1):71. doi: 10.3390/jcm9010071. PMID: 31892109.
Maeda T, Paralkar J, Kuno T, Patrawalla P. Inhaled Albuterol Use and Impaired Lactate Clearance in Patients With Sepsis: A Retrospective Cohort Study. J Intensive Care Med. 2021 Mar;36(3):284-289. doi: 10.1177/0885066619901095. Epub 2020 Jan 22. PMID: 31964210.
Zitek T, Cleveland N, Rahbar A, Parker J, Lim C, Elsbecker S, Forred W, Slattery DE. Effect of Nebulized Albuterol on Serum Lactate and Potassium in Healthy Subjects. Acad Emerg Med. 2016 Jun;23(6):718-21. doi: 10.1111/acem.12937. Epub 2016 May 11. PMID: 26857949.
