Category: Obstetrics & Gynecology
Posted: 1/12/2026 by Jennifer Wang, MD
Click here to contact Jennifer Wang, MD
At this point, I think we've all heard about vacuum-induced uterine tamponade (where negative pressure is used to draw down the uterine walls and stop postpartum hemorrhage), which is achieved in our OBGYN colleagues world with the Jada device, something that costs between 600-1200 USD and that most emergency medicine doctors are not trained on. However, our colleagues in Columbia and South Africa have come up with an alternative: the simple gastric tube.

59 patients were enrolled in this randomized feasibility trial with the goal to look for a 50% reduction in the primary outcome (blood loss >1000ml) comparing a 24 Fr Levin gastric tube and standard balloon uterine tamponade. Patients were given a survey asking about their experiences with the two devices.
Researchers analyzed this both with intention-to-treat and with per-protocol analysis looking at their primary outcome, and while their intention-to-treat analysis fell sort of significance (p value = 0.07), their per protocol just snuck to significance (p value = 0.04). They had one patient who had to switch over from the suction tube/gastric tube over to a balloon tamponade method, which was responsible for the change in their intention-to-treat analysis falling short. Still, the fact that a gastric tube reduced postpartum hemorrhage >1000ml around 40% compared to standard balloon uterine tamponade is both impressive and intriguing to me. Additionally, patients reported that the suction tube was much less painful than the balloon tamponade.
Some caveats: a very small number of patients, lack of dedicated research staff/missing data, only in Columbia and South Africa
So if you're ever in a desperate situation with a hemorrhage postpartum patient without the appropriate resources, a gastric tube could be your best friend!
Singata-Madliki M, Nieto-Calvache AJ, Rivera Torres LF, et al. Suction tube uterine tamponade versus uterine balloon tamponade for treatment of refractory postpartum hemorrhage: A randomized clinical feasibility trial. Int J Gynaecol Obstet. 2025;170(1):326-337. doi:10.1002/ijgo.16164
Category: Trauma
Keywords: Prehospital, transfusion, non-trauma (PubMed Search)
Posted: 1/11/2026 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
Much has been written about the benefits of prehospital blood transfusion for traumatic hemorrhage. Can this success be ascribed to non-traumatic hemorrhage as well? This small study (50 patients over 10 years!) says there were improvements in patient physiology (shock index) for those patients receiving blood for GI bleed, etc. Much more research is needed however this could be a beneficial practice in the future.
Kodakadath, H., Dillane, S., Griggs, J. et al. Pre-hospital blood transfusion in non-traumatic major haemorrhage: a retrospective observational study. Scand J Trauma Resusc Emerg Med 33, 191 (2025). https://doi.org/10.1186/s13049-025-01495-z
Category: Administration
Posted: 1/10/2026 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Plain films are often the first imaging test ordered in patient’s with knee injuries.
Plain films do NOT directly show the ACL but may reveal indirect signs of an ACL tear.
Key Plain Film Findings:
1) Effusion
ACL injury generates a large joint effusion (swelling/hemarthrosis). The presence of a fat/fluid interface (lipohemarthrosis) suggests associated bone injury.
This may be seen as joint fluid on the plain film lateral view. This view is best obtained with the patient in the supine position. This allows a layering of fluid in the suprapatellar bursa. A fat/fluid level indicates the presence of a lipohemarthrosis, signifying the likelihood of an intraarticular fracture.
http://radiologykey.com/wp-content/uploads/2019/03/f10-02ad-9781437727791.jpg
( A ) The normal suprapatellar bursa is seen on the lateral view as a line extending obliquely anterior and superior from the superior/posterior surface of the patella to the posterior surface of the quadriceps tendon.
(B) A small to moderate-sized effusion.
(C) A larger effusion.
In (D) the quadriceps tendon is bulged outward by an even larger joint effusion.
In the correct clinical setting, the presence or absence of a new fusion can be highly suggestive of ACL tear. Effusion can usually accurately be assessed on both physical exam and the lateral plain film. The absence of a knee effusion makes acute tear of the ACL unlikely as clinical practice suggests a rapidly developing hemarthrosis. Effusion of the knee may be associated with other entities such as intraarticular fracture or underlying arthritis. Typically, patients with acute ACL tears are young and do not have chronic infusions. Most acute meniscal tears and chondral injuries do not develop acute large effusions due to lack of significant vascularity.
Category: Orthopedics
Posted: 1/10/2026 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Plain films are often the first imaging test ordered in patient’s with knee injuries.
Plain films do NOT directly show the ACL but may reveal indirect signs of an ACL tear.
Key Plain Film Findings:
1) Effusion
ACL injury generates a large joint effusion (swelling/hemarthrosis). The presence of a fat/fluid interface (lipohemarthrosis) suggests associated bone injury.
This may be seen as joint fluid on the plain film lateral view. This view is best obtained with the patient in the supine position. This allows a layering of fluid in the suprapatellar bursa. A fat/fluid level indicates the presence of a lipohemarthrosis, signifying the likelihood of an intraarticular fracture.
http://radiologykey.com/wp-content/uploads/2019/03/f10-01ae-9781437727791.jpg
( A ) The normal suprapatellar bursa is seen on the lateral view as a line extending obliquely anterior and superior from the superior/posterior surface of the patella to the posterior surface of the quadriceps tendon.
(B) A small to moderate-sized effusion.
(C) A larger effusion.
In (D) the quadriceps tendon is bulged outward by an even larger joint effusion.
In the correct clinical setting, the presence or absence of a new fusion can be highly suggestive of ACL tear. Effusion can usually accurately be assessed on both physical exam and the lateral plain film. The absence of a knee effusion makes acute tear of the ACL unlikely as clinical practice suggests a rapidly developing hemarthrosis. Effusion of the knee may be associated with other entities such as intraarticular fracture or underlying arthritis. Typically, patients with acute ACL tears are young and do not have chronic infusions. Most acute meniscal tears and chondral injuries do not develop acute large effusions due to lack of significant vascularity.
Category: Pediatrics
Keywords: Pediatrics, BLS, resuscitation, CPR (PubMed Search)
Posted: 1/9/2026 by Kathleen Stephanos, MD
(Updated: 2/7/2026)
Click here to contact Kathleen Stephanos, MD
In 2025, the AHA and AAP teamed up for the latest Cardiac arrest guides- worth a read overall, Peds had a couple tweaks which should be recognized.
2-finger CPR is OUT. It has been shown to be ineffective, so the Two Thumb–Encircling Hands Technique should be used on ALL infants.
Grab your AED early. While a staple of adult BLS, this is now being emphasized in pediatrics as well.
For foreign body aspiration, remember to start with 5 back blows, but if the child is <1year old follow with chest thrusts, those who are older may receive abdominal thrusts. Repeat as needed. This has been in the literature for a while but was re-enforced due to potential injury to infants who receive abdominal thrusts.
Lasa JJ, Dhillon GS, Duff JP, Hayes J, Kamath-Rayne BD, Levy A, Mahgoub M, Morgan RW, McCormick T, Roberts JS, Ross CE, Schexnayder SM, Sweberg T, Valdés SO, Topjian AA. Part 8: Pediatric Advanced Life Support: 2025 American Heart Association and American Academy of Pediatrics Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2025 Oct 21;152(16_suppl_2):S479-S537. doi: 10.1161/CIR.0000000000001368. Epub 2025 Oct 22. PMID: 41122885.
Category: Pharmacology & Therapeutics
Keywords: complicated UTI, urinary tract infection, UTI, pyelonephritis, cystitis (PubMed Search)
Posted: 1/6/2026 by Alicia Pycraft
(Updated: 1/8/2026)
Click here to contact Alicia Pycraft
Previous guidelines for the treatment of urinary tract infections (UTI) were published in 2010 and focused on treatment of uncomplicated cystitis and pyelonephritis in women. Due to lack of published evidence at the time, these guidelines notably omitted discussion of complicated UTI (cUTI) and UTI in men. In July 2025, the Infectious Diseases Society of America (IDSA) released new, long-awaited guidelines for the treatment of cUTI. Below are key guideline updates to consider in the treatment of patients with cUTI presenting to the emergency department:
Bottom line: UTIs in males are no longer considered inherently complicated, treatment should be selected among preferred antimicrobials using a 4-step approach, and shorter (5-7 day) antibiotic courses may be considered for some patients with cUTI. As always, consult with your local antibiogram or pharmacist for guidance!
Category: Toxicology
Keywords: Water beads, foreign body ingestion, gastrointestinal obstruction (PubMed Search)
Posted: 1/7/2026 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
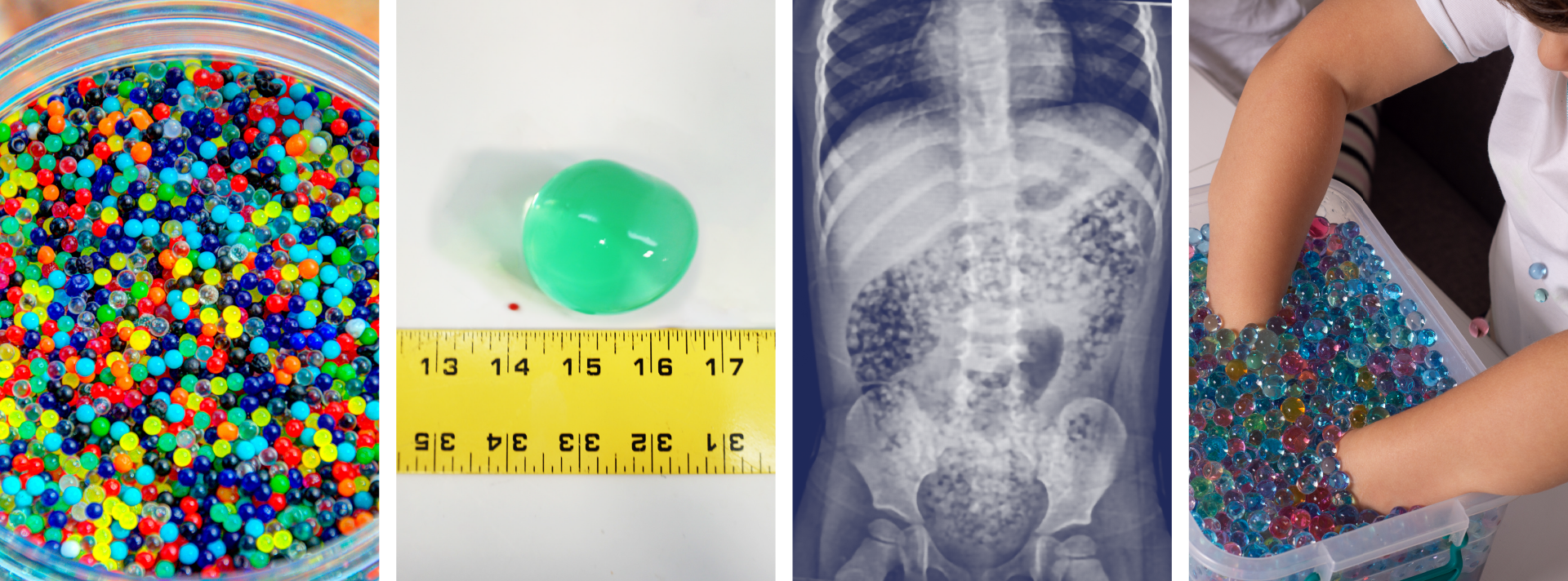
Water beads are a colorful, fun, popular, and widely available product found in children’s toys, stress squeeze balls, arts and crafts supplies, plant hydration products, air fresheners, and first aid ice packs.
These jelly-like small super-absorbent polymer balls are similar to the material found in diapers and absorb water expanding 100-800 percent of original size.
Pediatric ingestion is by far the most common poisoning exposure route but insertion into ears and nose and aspiration can occur and has led to serious adverse effects. More than 8000 water bead-related ingestion injuries have been treated in U.S. Emergency Departments.
Over the past 10 years, U.S. Poison Centers reported 19,660 exposures with 55% occurring in 2023 alone. In the majority of cases, no clinical effects (~88%) were seen, however in >11% of cases mild to moderate effects (abdominal discomfort, nausea, and vomiting) were reported and severe effects including complete bowel obstruction, necrosis, and surgical intervention in 0.11%. The Consumer Product Safety Commission reported at least one death of a 10-month-old girl in 2023 due to water bead ingestion.
Ingested water beads quickly pass into the small intestines where they continue to expand over the next few days and can become large enough (especially in children less than 2 year of age) to be unable to pass through the ileocecal valve causing small bowel obstruction requiring surgical intervention.
There is little data to guide management after ingestion. The majority of cases have no clinical effects and home observation is appropriate for asymptomatic for patients greater than 2 years. Recommendations from a report of case series and literature review , in patients less than 2 years of age with evidence of ingestion and symptomatic patients include hospitalization, imaging with US or CT, and close monitoring. CT, ultrasound, and endoscopy are not 100% reliable and often do not visualize these intraluminal foreign bodies.
In December 2025, the CPSC approved new federal safety standards for water beads toys setting limits on maximum expansion size of beads and amount of allowable acrylamide.
Risks of Water Bead Ingestion. Reeves PT, Pasman EA Pediatrics February 2025; 155 (2): e2024069447. 10.1542/peds.2024-069447
Water bead injuries by children presenting to emergency departments 2013-2023: An expanding issue. ?Pasman EA, Khan MA, et al. J Pediatr Gastroenterol Nutr. 2024 Sep;79(3):752-757. doi: 10.1002/jpn3.12333. Epub 2024 Jul 24. PMID: 39045753.
Pediatric water bead-related visits to United States emergency departments, Joynes HJ, Kistamgari S, et al. The American Journal of Emergency Medicine, Volume 84, 2024, Pages 81-86, ISSN 0735-6757, https://doi.org/10.1016/j.ajem.2024.07.048.
Water beads: Expanding toy and ‘new’ problem for paediatric surgeons and community. Bollettini, T., Mogiatti, M., et al. J Paediatr Child Health, 61: 204-208. 2025. https://doi.org/10.1111/jpc.16730
Aspiration of superabsorbent polymer beads resulting in focal lung damage: a case report. Alharbi N, Dabbour M. BMC Pediatr. 2020 May 29;20(1):262. doi: 10.1186/s12887-020-02168-9. PMID: 32471401; PMCID: PMC7257448.
Category: Critical Care
Keywords: alcohol withdrawal syndrome, AWS, phenobarbital (PubMed Search)
Posted: 1/6/2026 by William Teeter, MD
Click here to contact William Teeter, MD
Yet another study (this time ED focused) has shown benefits to patients and hospital systems when implementing a Phenobarbital-based treatment algorithm. Shorter ED LOS, fewer admissions, and treatment with phenobarbital alone was independently associated with discharge when compared to mixed treatment regimens. Higher age and heart rate, as well as treatment with benzodiazepines alone were independently associated with hospitalization.
Cautions/contraindications include: pregnancy, cirrhosis with history of hepatic encephalopathy (consider dose reduction in hepatic dysfunction), acute intermittent porphyria, and prior chronic phenobarbital use.
Phenobarbital has a long half life (one of its benefits in AWS) and works synergistically with benzodiazepines, so should be used preferentially as monotherapy in patients where the diagnosis is relatively certain and who have not received high doses of benzos. Once the diagnosis is made, go with phenobarbital and stick with it.
PulmCrit has an excellent in-depth article on this and also see Dr. Flint's pearl describing another centers experience in a hospital-wide rollout (links below).
Category: Ultrasound
Keywords: POCUS, arterial occlusion, limb ischemia (PubMed Search)
Posted: 1/5/2026 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
POCUS can be a valuable tool for screening both peripheral venous and arterial pathology.
If you suspect critical limb ischemia, you can use a similar approach to venous evaluation to assess for arterial occlusion.
Evaluate for:
Conclusion: POCUS can expedite diagnosis and resources prior to definitive testing with CT angiography.
Gonzalez AA, Brenner DS. Arterial Thrombosis Diagnosed With Point-of-Care Ultrasound. Cureus. 2024 Sep 13;16(9):e69357. doi: 10.7759/cureus.69357.
Frederick MK, Stolz LA, Duran-Gehring PE. Vascular Ultrasound. Emerg Med Clin North Am. 2024 Nov;42(4):805-818. doi: 10.1016/j.emc.2024.05.011.
Drake A, Dreyer N, Hoffer M, Boniface K. Point-of-care Ultrasound for the Evaluation of Acute Arterial Pathology in the Emergency Department: A Case Series. Clin Pract Cases Emerg Med. 2022 Feb;6(1):1-7. doi: 10.5811/cpcem.2021.11.54904.
Category: Trauma
Keywords: Ketamine, nebulized, pain control (PubMed Search)
Posted: 1/3/2026 by Robert Flint, MD
(Updated: 1/4/2026)
Click here to contact Robert Flint, MD
This systematic review found improved pain scale at 15 and 120 minutes in 495 patients who received nebulized ketamine. Dosing at 0.75 mg/kg was as effective as 1.5 mg/kg and the nebulized ketamine was non-inferior to IV morphine and ketamine with fewer side effects.
Kirk, D., Whiles, E., Jones, A. et al. Breathing new life into pain management: a systematic review of nebulised ketamine for analgesia. Scand J Trauma Resusc Emerg Med 33, 196 (2025). https://doi.org/10.1186/s13049-025-01501-4
Category: Geriatrics
Keywords: FRAIL, geriatric, prediction tool, Barthel (PubMed Search)
Posted: 1/1/2026 by Robert Flint, MD
(Updated: 1/3/2026)
Click here to contact Robert Flint, MD
The Geriatric Measurement Tool (GMT) was used in this study prospectively to assess 24 hour mortality rate in ED patients over age 65. The GMT is a combination of FRAIL Questionnaire and Barthel index for Activity of Daily Living. The study found:
“ From 700 enrolled patients, GMT categorization revealed that 53.6% of patients were in Category-4 (moderate/more dependent and frail), while 34% were in Category-1 (independent or slight dependency, prefrail/fit). The 24-h mortality rate was 9%. GMT Category-4 demonstrated high sensitivity (87.3%) for mortality prediction, but low specificity (49.7%). Conversely, GMT Category-1 showed low sensitivity (44.1%) but high specificity (90.2%) for predicting discharge.”
Probably the biggest take away is we should be thinking about assessing our older patient's health status using some validated scale/tool to help us have conversations with patients and families regarding prognosis and interventions.
Category: Geriatrics
Keywords: FRAIL, geriatric, prediction tool, mortality, (PubMed Search)
Posted: 1/1/2026 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
The Geriatric Measurement Tool combines the FRAIL Questionnaire with the Barthel Index For Daily Living to give a prognosis on your patient's mortality. First used to predict mortality in older patients with pneumonia during COVID-19 pandemic. Now being investigated for other ED patient populations.
FRAIL Questionnaire: Fatigue, Resistance, Aerobic, Illness, Weight loss. https://www.activeagingweek.com/pdf/abbott/FRAILQuestionnaire.pdf
Barthel: Ten questions about ADL's to create a score 0-100. https://www.mdcalc.com/calc/3912/barthel-index-activities-daily-living-adl
Zaman, Süeda et al. Journal of Emergency Medicine, Volume 79, 560 - 567
2. Gómez-Moreno, C., Chacón-Corral, A.A., Pérez-Méndez, A. et al. Association between a geriatric measure tool and adverse outcomes among older adults treated in an emergency department: a retrospective cohort study. Intern Emerg Med 20, 2205–2213 (2025). https://doi.org/10.1007/s11739-024-03843-w
Category: Administration
Keywords: industry sponsored, money, research, PI (PubMed Search)
Posted: 12/27/2025 by Robert Flint, MD
(Updated: 12/31/2025)
Click here to contact Robert Flint, MD
This study looked at industry sponsored payments to EM physician through non-covered entities (ie not directly to physician or through an academic institution). It found a $100 million increase from 2015-23 in this payment model. It appears that private equity is not the only money entering emergency medicine in the past decade.
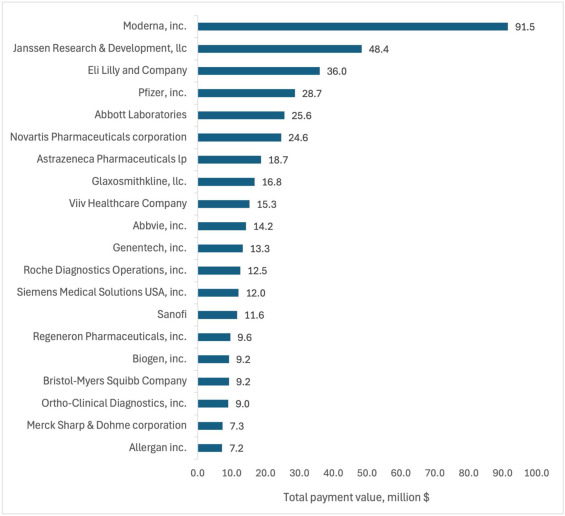
Total value of Industry-Sponsored Research Payments (ISRPs) by company. The 20 companies with highest total ISRPs awarded to emergency physician PIs.
Rizer, Nicholas W et al.
Journal of Emergency Medicine, Volume 79, 21 - 30
Category: Critical Care
Keywords: Intubation, RSI, norepinephrine, hypotension, vasopressors (PubMed Search)
Posted: 12/29/2025 by Mark Sutherland, MD
(Updated: 12/30/2025)
Click here to contact Mark Sutherland, MD
Perintubation hypotension is a major problem, and can precipitate hemodynamic collapse and cardiac arrest for a multitude of reasons. To prevent this, many different strategies have been explored (some of which work and some of which don't), including empiric IV fluid boluses, additional resuscitation before intubation, switching or dose-reducing induction agents and much more. But we know pressors like norepinephrine raise blood pressure effectively, so should we just put everybody on a norepinephrine drip before we intubate them?
Probably not. The EPITUBE trial included 210 patients at a single-institution undergoing cardiac surgery, and randomized them to empirically starting a norepinephrine infusion before induction vs just rescue ephedrine when needed (fairly standard anesthesia practice). For the empiric norepinephrine group, they started at 0.06 ug/kg/min, and once the drip was up and running, they titrated for a MAP of 65-80 (which could include stopping the norepi if that the patient remained above 80 despite downtitration)
The incidence of severe hypotension (MAP < 55) did not differ between the groups, although fewer empiric norepinephrine patients had a MAP < 65 at any point (which was a secondary outcome). Naturally, the differences between this practice setting (the cardiac surgery OR) and the emergency department should be noted and are not addressed by this study.
Bottom line: There isn't good evidence to support empirically starting all patients on a norepinephrine infusion prior to intubation as a method to prevent perintubation hypotension. You should always have rapid access to vasopressors when intubating, and should continue to tailor your therapy to the individual patient, but probably don't start just putting everyone on norepinephrine before you intubate them.
Category: Toxicology
Posted: 12/29/2025 by TJ Gregory, MD
Click here to contact TJ Gregory, MD
Winter is in full swing and an escape to warmer climes is the only answer for many. That also means enjoying local tropical seafood and associated toxins. How do you differentiate, manage, and properly recognize the ABEM prompt?
Scombroid - HISTAMINE reaction
Ciguatera - CIGUATOXIN contaminated reef fish
Category: Quality Assurance/Quality Improvement
Keywords: radiology, report, risk, management (PubMed Search)
Posted: 12/27/2025 by Robert Flint, MD
(Updated: 12/29/2025)
Click here to contact Robert Flint, MD
We have all been on that busy shift and just quickly looked at the impression section of the radiology report whether that is a CT, plain film, US or MRI. In doing this you run the risk of missing important information that is contained in the body of the report and has either not been carried down into the impression or contradicts the impression by some error.
To avoid missing important information that can impact patient care, always read the entire report and look at the images yourself. You have seen the patient, know the clinical history, and a second set of eyes never hurts.
Category: Trauma
Keywords: hypocalcemia, trauma, mortaility, rate (PubMed Search)
Posted: 12/27/2025 by Robert Flint, MD
(Updated: 12/28/2025)
Click here to contact Robert Flint, MD
Previous small studies had put the prevalence of hypocalcemia in trauma patients at 23-56%. This single center study of 2200 patients looked at prevalence and outcome and found a much lower prevalence however worse outcomes than those who were not hypocalcemic.
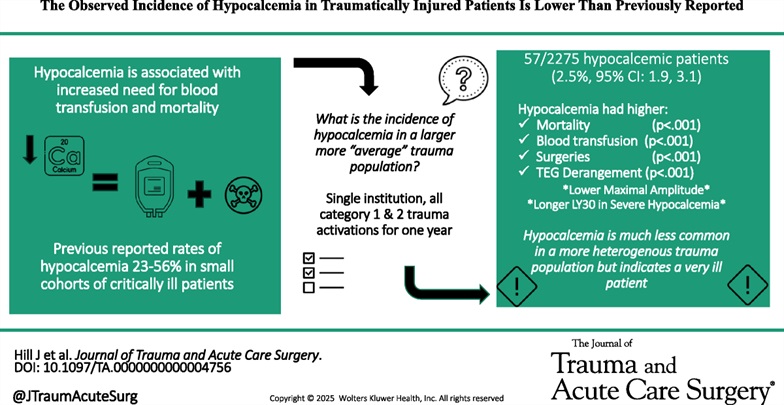
Hill, Joshua H. MD; Shah, Bhairav DO; Rady, Emily MD; Lieber, Michael MS; Lauria, Julia DO; Lee, Katarina DO; Wierzbicki, Katrina BS; Kashikar, Tanisha DO; Kincaid, Michelle MD. The observed incidence of hypocalcemia in traumatically injured patients is lower than previously reported. Journal of Trauma and Acute Care Surgery 99(6):p 920-927, December 2025. | DOI: 10.1097/TA.0000000000004756
Category: Geriatrics
Keywords: delirium, hip fracture, nerve block (PubMed Search)
Posted: 12/27/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
This study is a reminder of the efficacy of regional nerve blocks for older patient's with hip fractures. The authors trained EM physicians for 2 hours then evaluated delirium levels in patients who did and did not receive nerve blocks for hip fractures.
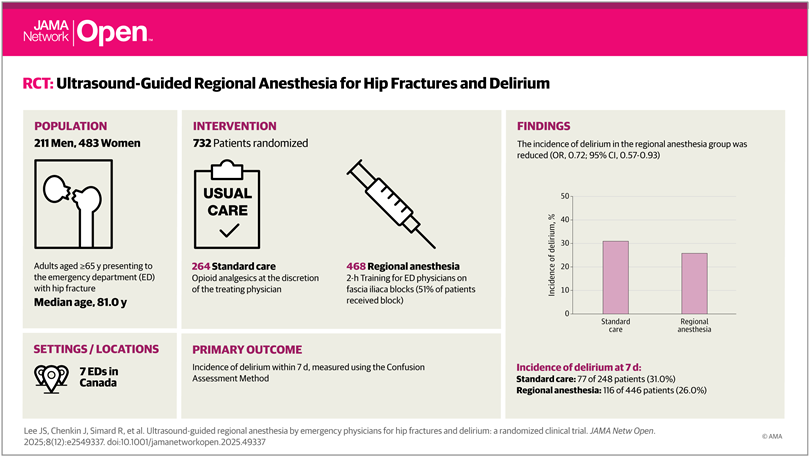
Lee JS, Chenkin J, Simard R, et al. Ultrasound-Guided Regional Anesthesia by Emergency Physicians for Hip Fractures and Delirium: A Randomized Clinical Trial. JAMA Netw Open. 2025;8(12):e2549337. doi:10.1001/jamanetworkopen.2025.49337
Category: Trauma
Keywords: prehospoital, blood, survival, unexpected (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 12/25/2025)
Click here to contact Robert Flint, MD
This study demonstrated that administration of prehospital blood to trauma patients lead to a higher rate of survival in patients whose initial ED vital signs or pre-hospital shock index would have predicted death.
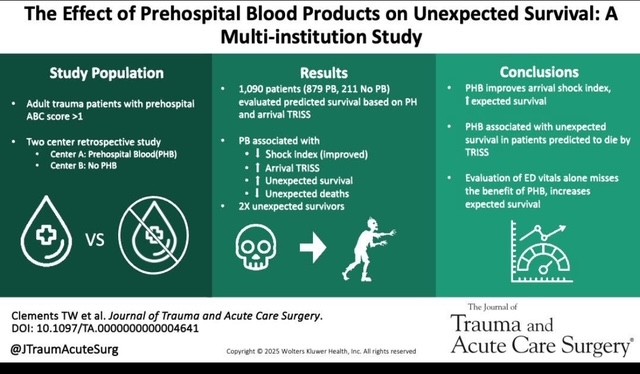
Clements TW, Van Gent JM, Krzyzaniak A, Campbell B, Carroll A, Mericle M, Sise M, Peck KA, Cotton BA. The effect of prehospital blood products on unexpected survival: A multi-institution study. J Trauma Acute Care Surg. 2025 May 2. doi: 10.1097/TA.0000000000004641. Epub ahead of print. PMID: 40312787.
Category: Administration
Keywords: holidays, scheduling, daily volumes, behavioral health (PubMed Search)
Posted: 12/18/2025 by Steve Schenkel, MPP, MD
(Updated: 12/24/2025)
Click here to contact Steve Schenkel, MPP, MD
How do ED volumes change around the winter holidays?
The anticipated US pattern is one of lower volumes on the holidays themselves followed by increased volumes on the first weekdays after.
Behavioral health visits show similar patterns – a drop before the holidays and perhaps an increase after the holiday.
Many departments adjust scheduling accordingly, reducing staff on major holidays, which has the added benefit of allowing more people to enjoy the holiday.
This pattern isn’t necessarily what happens everywhere, though. At least one Australian ED reported increased visits over the holidays.
While not perfect, the best guide to future holiday volumes remains past experience thoughtfully applied.
Agoritsas A, et al. Predicting Flow in the Pediatric Emergency Department: Are Holidays Lighter? Annals of Emergency Medicine 2015, Volume 66, Issue 4, S143
Halpern, Scott D. et al. Emergency department patterns in psychiatric visits during the holiday season. Annals of Emergency Medicine 1994, Volume 24, Issue 5, 939 – 943.
Leming, M. et al. Effect of Holidays on the Patient Severity and Census In the Emergency Department. Annals of Emergency Medicine 2010, Volume 56, Issue 3, S128
Silverman M. Holiday Scheduling: Fair and Balanced. EP Monthly, Dec 1, 2010. https://epmonthly.com/article/holiday-scheduling-fair-and-balanced/.
Zheng, W., Muscatello, D.J. and Chan, A.C. (2007), Deck the halls with rows of trolleys … emergency departments are busiest over the Christmas holiday period. Medical Journal of Australia, 187: 630-633. https://doi.org/10.5694/j.1326-5377.2007.tb01451.x
