Category: Critical Care
Posted: 2/17/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
As the cold and snow rips through the United States, hypothermia is a major concern because each year approximately 1,300 Americans die of hypothermia.
Classification of hypothermia:
The risk of cardiac arrest increases when the core temperature is less than 32 Celsius and significantly rises when the temperature is less than 28 Celsius. Rapid rewarming is required as part of resuscitation should cardiac arrest occur.
A rescue therapy to consider (when available) is extra corporeal membrane oxygenation (ECMO). ECMO not only provides circulatory support for patients in cardiac arrest, but allows re-warming of patients by 8-12 Celsius per hour.
Some studies quote survival rates of 50% with hypothermic cardiac arrest patients receiving ECMO versus 10% in similar patients who do not receive ECMO.
As winter lingers in the United States, consider speaking to your cardiac surgeons now to plan an Emergency Department protocol for hypothermic patients that may require ECMO.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 2/16/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Reference
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 2/15/2015 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
The Unforgotten: ECG Utilization to Differentiate Athletic Heart vs. Brugada
- Highly trained athletes develop ECG changes as a physiologic consequence of increased vagal tone; The ECG manifestations of early repolarization (ER) can range from simple J–point elevation to anterior (V1 to V3) "domed" ST-segment elevation and negative T wave.
- The former raises problems of differential some forms of ER with the “ coved-type” pattern seen in Brugada Syndrome (BS).
- A recent study compared the ECG tracings of 61 athletes w/a “domed” ST-segment elevation & negative T wave and 92 age/sex-matched BS patients w/a “ coved-type” pattern to identify an ECG criteria for distinguishing benign athletic changes seen in ER from BS.
- ECG analysis focused on ST-segment elevation at J-point (STJ ) and at 80 milliseconds after J-point (ST80 ).
- Athletes had a lower maximum amplitude of STJ (p < 0.001) & lower STJ /ST80 (p < 0.001)
- All patients (100%) with BS showed a downsloping ST-segment configuration (STJ/ST80 > 1) versus only 2 (3%) athletes (p < 0.001)
- An upsloping ST-segment configuration (STJ /ST80 < 1) showed a sensitivity of 97%, a specificity of 100%, and a diagnostic accuracy of 98.7% for the diagnosis of ER.
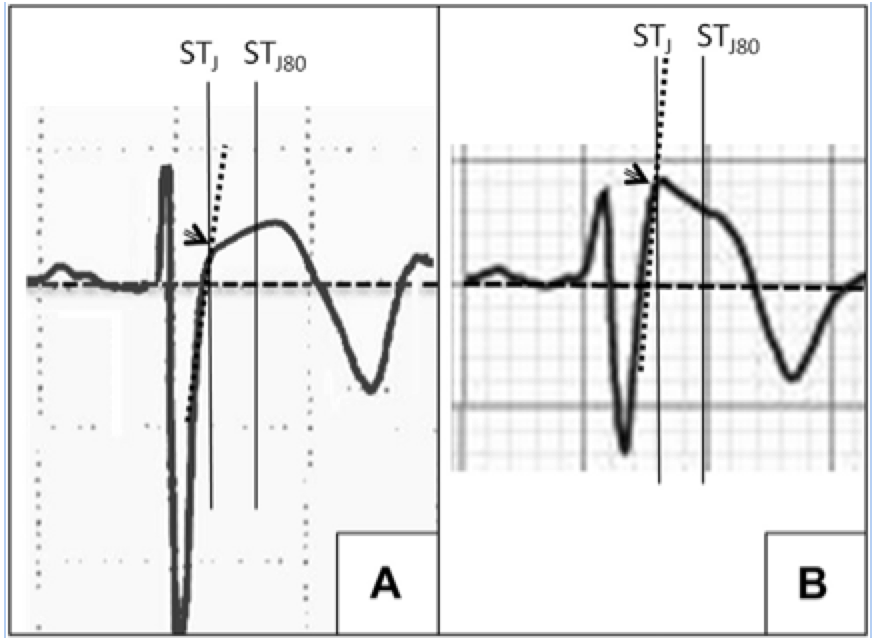
A: ER
B: Brugada
Zorzi A, Leoni L, et al. Differential Diagnosis Between Early Repolarization of Athlete’s Heart and Coved-Type Brugada Electrocardiogram. Am J Cardiol. 2015 Feb 15;115(4):529-32.
Category: Orthopedics
Keywords: LATERAL ANKLE TENDINOPATHY (PubMed Search)
Posted: 2/14/2015 by Brian Corwell, MD
(Updated: 2/15/2015)
Click here to contact Brian Corwell, MD
LATERAL ANKLE TENDINOPATHY
Hx: subacute onset (weeks) of the pain seen in athletes esp. runners (banked or uneven surfaces).
PE: Tenderness to palpation posterior to the lateral malleolus or over the course of the tendon. Pain worse with resisted ankle eversion from a dorsiflexed postion. Examine for subluxation of tendon.
The diagnosis is made from the above and does not require imaging.
Tx: Rest, conservative care, physical therapy (eccentric exercise focus), ankle taping or lace up brace. Severe cases may even require a walking boot.
http://www.epainassist.com/images/Article-Images/Peroneal_Tendonitis.jpg
Category: Pediatrics
Keywords: Caffeine, Energy Drinks, Overdose, Tox, Pediatrics (PubMed Search)
Posted: 2/13/2015 by Melissa Rice, MD
Click here to contact Melissa Rice, MD
Pediatric Caffeine Overdose
As the in-service draws closer and the hours to study wind down, I find myself becoming more and more of a caffeine enthusiast. While a No-Doz or Diet Mt. Dew may put a little more pep in my step, the caffeine found in energy drinks, caffeine pills, and diet supplements can quickly result in an dangerous overdose in a young child.
Caffeine Overdose Presentation- Sympathomimetic Toxidrome
Available Sources of Caffeine-
Toxic Doses
Management- treat the symptoms (metabolic, cardiovascular, and neurologic)
Good Luck on the In-Service!

Jones, Maya A., and Elizabeth R. Alpern. "A 16-Month-Old Girl With Irritability After Ingesting White Pills." Pediatric emergency care 30.1 (2014): 69-71.
Wolk, Brian J., Michael Ganetsky, and Kavita M. Babu. "Toxicity of energy drinks." Current opinion in pediatrics 24.2 (2012): 243-251.
Category: Toxicology
Keywords: ECMO, fat emulsion, lipid, intralipid, poison, extracorporeal membrane oxygenation (PubMed Search)
Posted: 2/3/2015 by Bryan Hayes, PharmD
(Updated: 2/12/2015)
Click here to contact Bryan Hayes, PharmD
A new review summarized published adverse effects when IV lipid emulsion is used along with venous-arterial extracorporeal membrane oxygenation (VA-ECMO) in patients with cardiotoxic drug poisoning.
Not surprisingly, running fat through the ECMO circuit can cause some issues. Here's what's been published:
It's unclear how these findings should change management if using both treatment modalities, but at the very least, be aware that fat depostion in the VA-ECMO circuits and increased blood clot formation can occur.
Lee HM, et al. What are the adverse effects associated with the combined use of intravenous lipid emulsion and extracorporeal membrane oxygenation in the poisoned patient? Clin Toxicol. 2015 Jan 29. [Epub ahead of print, PMID 25634667]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Neurology
Keywords: acute ischemic stroke, magnesium, neuroprotectant, IMAGES, FAST-MAG (PubMed Search)
Posted: 2/12/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Magnesium, another failed neuroprotectant?
Stroke is a leading cause of adult disability and the second leading cause of death worldwide. Currently available therapies for acute ischemic stroke are based on restoring perfusion to the ischemic penumbra. However, they are only moderately effective.
A series of pathological cascades leading to neuronal death are triggered in acute ischemia. Thus it may be logical to suggest that if one can interrupt the propagation of these cascades, perhaps part of the brain tissue can be protected and salvaged.
Magnesium has been shown in various animal models to have pluripotent neuroprotective properties. It is also widely available, simple to administer, and has a favorable risk profile. A prior study of magnesium in acute ischemic stroke (IMAGES) did not show a benefit when the agent was administered a median 7.4 hours after symptom onset. However, a subgroup of patients treated within 3 hours of symptom onset showed possible benefit.
The Field Administration of Stroke Therapy - Magnesium (FAST-MAG) trial, funded by the NIH, looked at magnesium administered within 2 hours after symptom onset on the degree of disability at 90 days after stroke as measured by the modified Rankin scale.
Magnesium was not found to have any benefit in functional outcome at 90 days.
This study was unique in several ways:
However, despite this study being very well executed, demonstrating the feasibility of conducting a phase 3 trial with targeted intervention within the hyperacute window, it is another neuroprotective agent that failed to translate from the laboratory bench to the clinical realm.
Potential explanations for the discrepancies between preclinical and clinical outcomes of neuroprotective agents thus far include discrepancies on outcome measures, functional assessments, pre-morbid conditions, therapeutic windows, and drug-dosing schedules between animal studies and clinical trials.
Take Home Point: Magnesium does not have any clear benefit in acute ischemic stroke at this time.
Muir KW, Lees KR, Ford I, et al. Magnesium for acute stroke (Intravenous Magnesium Efficacy in Stroke trial): a randomised controlled trial. Lancet. 2004;363(9407):439-445.
Saver JL, Starkman S, Eckstein M, et al. Prehospital use of magnesium as neuroprotection in acute stroke. N Engl J Med. 2015;372(6):528-536.
Cheng YD, Al-Khoury L, Zivin JA. Neuroprotection for ischemic stroke: two decades of success and failure. NeuroRx. 2004;1(1):36-45.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: VAP, chlorhexidine baths, subglottic suctioning (PubMed Search)
Posted: 2/10/2015 by Feras Khan, MD
Click here to contact Feras Khan, MD
Updates in preventative strategies in the ICU
Preventing Ventilator Associated Pneumonia (VAP)
The trial
Bottom Line
Daily bathing with chlorhexidine does not reduce health care associated infections
The trial
Bottom Line
Category: Pharmacology & Therapeutics
Keywords: vancomycin, loading dose (PubMed Search)
Posted: 1/26/2015 by Bryan Hayes, PharmD
(Updated: 2/7/2015)
Click here to contact Bryan Hayes, PharmD
We know vancomycin should be dosed based on weight rather than the default 1 gm dose so many patients receive. A past Academic Life in EM post explores the nuances of proper vancomycin dosing. But do higher loading doses in the ED actually lead to more therapeutic trough levels?
New Data
A new randomized trial compared ED patients receiving 30 mg/kg initial doses vs. 15 mg/kg. [1] There was a significantly greater proportion of patients reaching target trough levels of 15 mg/L at 12 hours among the patients who received a 30 mg/kg loading dose as compared with a traditional 15 mg/kg dose (34% vs 3%, P < 0.01). This study did not use a max dose of 2 gm. They included patients up to 120 kg who received 3.6 gm loading doses! Patients with creatinine clearance < 50 mL/min were excluded. There was no difference in incidence of nephrotoxicity between the groups.
Application to Clinical Practice
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Toxicology
Keywords: Drug Screens, Drug Intervals (PubMed Search)
Posted: 2/5/2015 by Kishan Kapadia, DO
Click here to contact Kishan Kapadia, DO
| Performance Characteristics of Common Drug Abuse Screening Immunoassays | ||
| Drug/Class | Detection Interval (***) | Comments |
| Amphetamines | 1-2 days (2-4 days) | Decongestants, ephedrine,l-methamphetamine, selegilene & bupropion metabolites may give False (+) results; MDA & MDMA are variably detected |
| Barbiturates | 2-4 days | Phenobarbital may be detected for up to 4 weeks |
| Benzodiazepines | 1-30 days | Benzos vary in reactivityand potency; False (+) results may be seen with oxaprozin |
| Cannabinoids | 1-3 days (>1 month) | Screening assays detect inactive and active cannabinoids; Confirmatory assays detects inactive metabolite THCA (tetrahydrocannabinoic acid) |
| Cocaine | 2 days (1 week) | Screening & confirmatory assays detect inactive metabolite BE (benzoylecgonine); False (+) results are unlikely |
| Opiates | 1-2 days; 2-4 days (<1 week) | Semisynthetic opiates derived from morphine show variable cross-reactivity; Fully synthetic opioids (e.g., fentanyl, meperidine, methadone, propoxyphene, tramadol) have minimal cross reactivity; Quinolone may cross-react |
| Methadone | 1-4 days | Doxylamine may cross-react |
| Phencyclidine | 4-7 days (>1 month) | Dextromethorphan, diphenhydramine, ketamine, & venlafaxine may cross react |
| Propoxyphene | 3-10 days | Duration of positivity depends on cross reactivity of metabolite norpropoxyphene |
(***)Values are after typical use; values in parentheses are after heavy or prolonged use.
Adapted from Goldfrank's Toxicologic Emergencies, 9th ed; Table 6-10.
Category: International EM
Keywords: Measles, international, pediatrics, vaccination, public health (PubMed Search)
Posted: 2/4/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
From January 1st to January 30th, 2015, 102 people from 14 states were reported to have measles. This one month total is greater than the annual number of U.S. cases from 2002 to 2012. Most of these cases are related to a large outbreak from a Californian amusement park. Measles can spread in communities without adequate vaccination (low herd immunity). The majority of the people in the US who get measles are unvaccinated. However, measles remains common in many parts of the world.
Bottom Line:
As noted in the recent ACEP Fact Sheet, “A very high index of suspicion for Rubeola is necessary especially among patients with an exposure history, travel to foreign or domestic areas where disease is present, and those without adequate immunization. Immediate isolation of these patients should be considered in the ED or other outpatient healthcare setting.”
Category: Critical Care
Posted: 2/3/2015 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Hypertensive Emergency Pearls
Monnet X, Marik PE. What's new with hypertensive crisis? Intensive Care Med 2015; 41:127-130.
Category: Visual Diagnosis
Posted: 2/2/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Patient presents with right shoulder pain following minor trauma. What's the diagnosis....and what's the Cunningham technique?
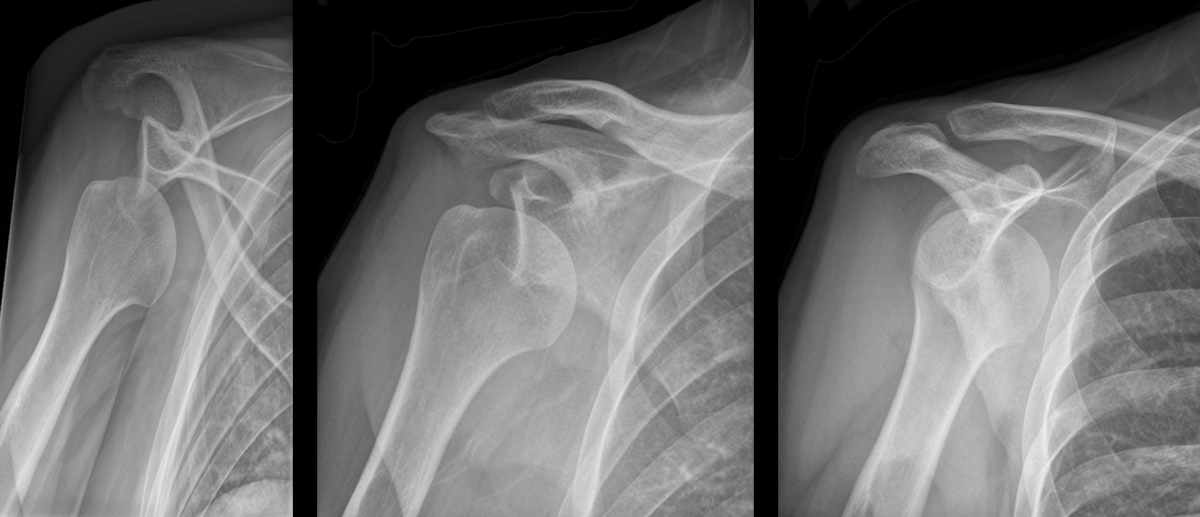
Anterior shoulder dislocation
Cunningham Technique
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Toxicology
Keywords: tetrodotoxin (PubMed Search)
Posted: 1/29/2015 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
Tetrodotoxin is lethal poison that blocks sodium channels. A famous sushi called "Fugu" is cut from a puffer fish that contains this poison. The idea is to get just enough of the toxin to cause peri-oral paresthesia but not too much to get seizures, paralysis and cardiac dysrrhythmias. A recent outbreak in Minneapolis, Minnesota was just reported in the MMWR so it can really happen anywhere, its a great read - dried puffer was bought from a market in NYC.
http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6351a2.htm
2-3 mg of the toxin is lethal to an adult human. No antidote exists though I would try hypertonic sodium bicarbonate for the cardiac dysrrhythmias and appropraite supportive. If the patient survives 24 hrs, the patient will do well without sequelae if appropriately supported.
Category: Neurology
Keywords: Myasthenia gravis, myopathy, iatrogenic (PubMed Search)
Posted: 1/29/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Patients with myasthenia gravis (MG) may be seen in the emergency department for symptoms that are not related to their MG, such as an upper respiratory tract infection or chest pain, for example.
The emergency physician should be careful in prescribing new medications to patients with MG, as that can precipitate a myasthenic crisis (and therefore cause significant morbidity and mortality). Below is a list of medications that are commonly implicated; an extensive list can be found on www.myasthenia.org/docs/MGFA_medicationsandmg.pdf)
Sanders DB, Guptill JT. Myasthenia Gravis and Lambert-Eaton Myasthenic Syndrome. Continuum. 2014 Oct;20(5)
Category: Critical Care
Keywords: Methanol, toxicology, methanol toxicity, critical care (PubMed Search)
Posted: 1/20/2015 by John Greenwood, MD
(Updated: 1/30/2015)
Click here to contact John Greenwood, MD
Extracorporeal Treatment Strategies for Acute Methanol Poisoning (When to Dialyze)
Methanol toxicity is classically included in the differential for the intoxicated patient presenting to the ED. Add a negative EtOH level, anion/osmolar gap, blindness and you have yourself a slam dunk diagnosis. The goal is to stop the liver from metabolizing methanol to formic acid. Outside of fomepizole (or old school ethanol therapy), dialysis is often discussed, but when should you actually get the nephrologist on the phone?
This month the Extracorporeal Treatments in Poisoning Workgroup released a systematic review and consensus statement to help clinicians decide when to pull the HD trigger. Their suggestions are below.
When to start HD:
Which Modality: Intermittent HD (IHD) should be used over continuous renal replacement therapies (CRRT), as you can clear the toxin faster with higher HD flows.
When to stop HD: Extracorporeal treatment can be terminated when the methanol concentration is less than 200 mg/L or 6.2 mmol/L and a clinical improvement is observed.
Bottom Line: Consider early hemodialysis in most patients presenting with methanol toxicity. Clinical exam and routine lab testing will likely provide enough information to determine the need for IHD, but specific methanol levels can be helpful to guide adjunctive treatment options.
Reference
Roberts DM, Yates C, Megarbane B, et al. Recommendations for the Role of Extracorporeal Treatments in the Management of Acute Methanol Poisoning: A Systematic Review and Consensus Statement. Crit Care Med. 2015;43(2):461-472.
Follow me on Twitter @JohnGreenwoodMD
Category: Visual Diagnosis
Posted: 1/26/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Elderly male presents with the skin findings below. He is also on a medication for atrial fibrillation. What's the diagnosis?

Severe ecchymosis from coumadin overdose
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 1/26/2015 by Semhar Tewelde, MD
(Updated: 2/8/2026)
Click here to contact Semhar Tewelde, MD
Posterior Myocardial Infarctions (PMI)
- Posterior myocardial infarctions (PMI) are different than typical ST-elevation MI; the ECG findings include: septal & anterior ST-segment depression, dominant tall/broad R waves, and upright T waves.
- In a study among 117,739 subjects with STEMI, 824 with PMI were more likely to present with cardiac arrest, cardiogenic shock, and congestive heart failure.
- The median time from arrival ECG to revascularization with PCI was longer among subjects with PMI.
- The median time from arrival ECG to systemic thrombolysis was also longer among subjects with a PMI.
- Increased awareness and recognition of PMI is needed to improve reperfusion times among this subpopulation with STEMI.
Waldo S, et al. Reperfusion times and in-hospital outcomes among patients with an isolated posterior myocardial infarction. Am Heart J 2014;167:350-354.
Category: Orthopedics
Keywords: Heel pain, bone injury (PubMed Search)
Posted: 1/24/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Overuse injury
Seen in runners, military recruits (marching), ballet dancers and in jumping sports (heavy landing).
Insidious onset of heel pain, that is worse with jumping then running then later with simple weight bearing.
Tenderness to palpation posteriorly (medially or laterally), and squeezing bilateral posterior calcaneus.
Testing:
XR: May not be positive for 2 to 4 weeks. Sclerotic appearance (vertically oriented) posterior calcaneus.
MRI: high signal T2 at fracture site.
DDx: plantar fasciitis.
Treatment: Reduction of activity if Sxs mild, for severe pain start a trial of non weight-bearing (boot or splint with crutches).
Stretching of calf, achilles, plantar fascia.
Category: International EM
Keywords: Tuberculosis, infectious disease, drug resistance, multidrug resistant tuberculosis (PubMed Search)
Posted: 1/21/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
As noted previously (UMEM Pearl of 1/7/2015), tuberculosis (TB) is a major infectious disease that occurs worldwide. Strains of tuberculosis can be resistant to one or more anti-tuberculosis medications. TB strains resistant to at least one medication have been found in all surveyed countries.
What is multidrug-resistant tuberculosis (MDR TB)?
Treatment of MDR TB
Bottom line:
As noted previously, in your emergency department have a high index of suspicion for TB and MDR TB in patients with an appropriate risk profile.
http://www.who.int/mediacentre/factsheets/fs104/en/
http://www.cdc.gov/tb/topic/drtb/default.htm
http://www.cdc.gov/tb/publications/factsheets/drtb/mdrtb.htm
