Category: Critical Care
Posted: 11/11/2014 by Mike Winters, MBA, MD
(Updated: 11/12/2014)
Click here to contact Mike Winters, MBA, MD
Aminoglycosides in Critically Ill Patients
Matthaiou DK, et al. What is new in the use of aminoglycosides in critically ill patients? Intensive Care Med 2014; 40:1553-1555.
Category: Visual Diagnosis
Posted: 11/10/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
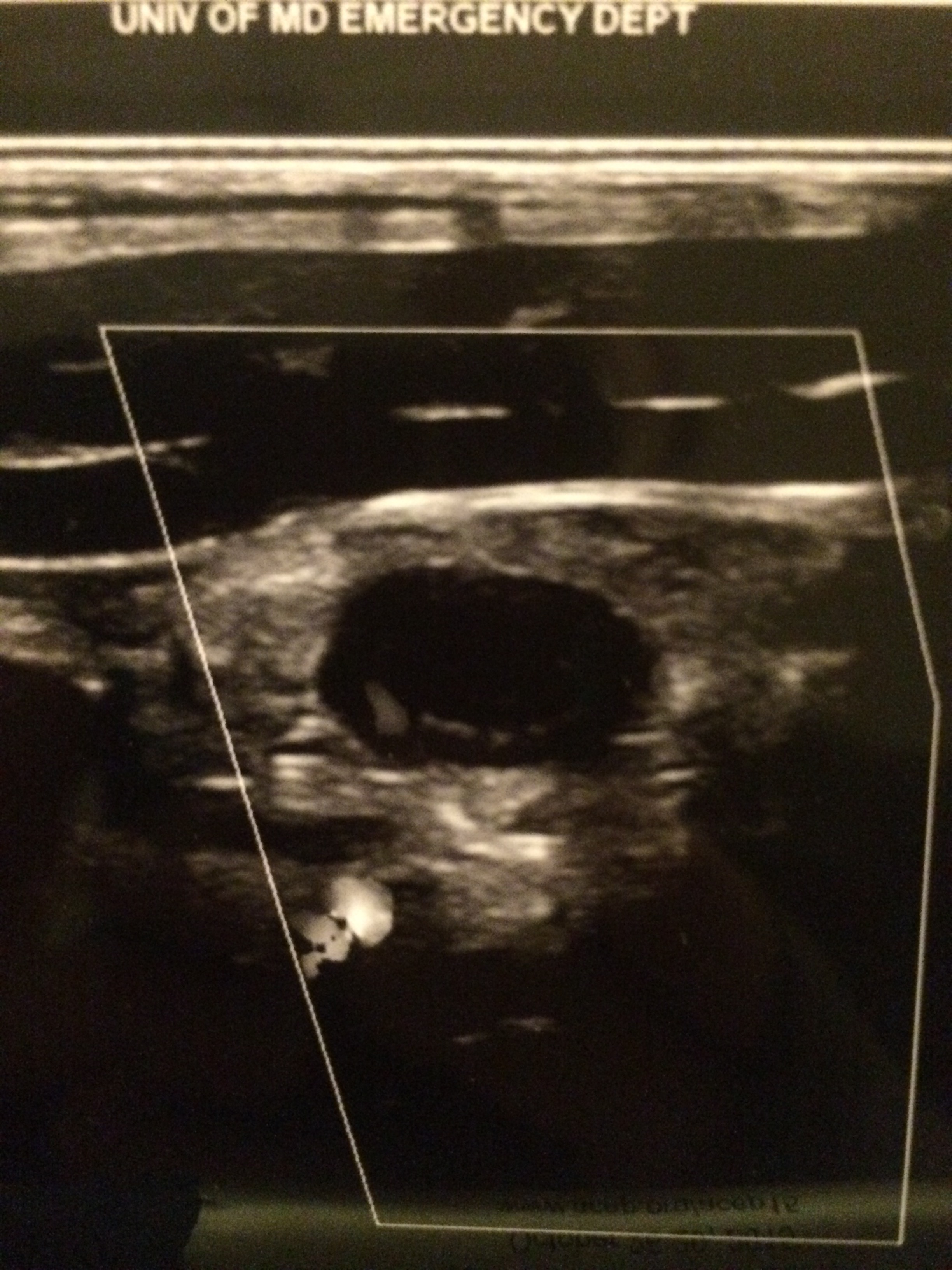
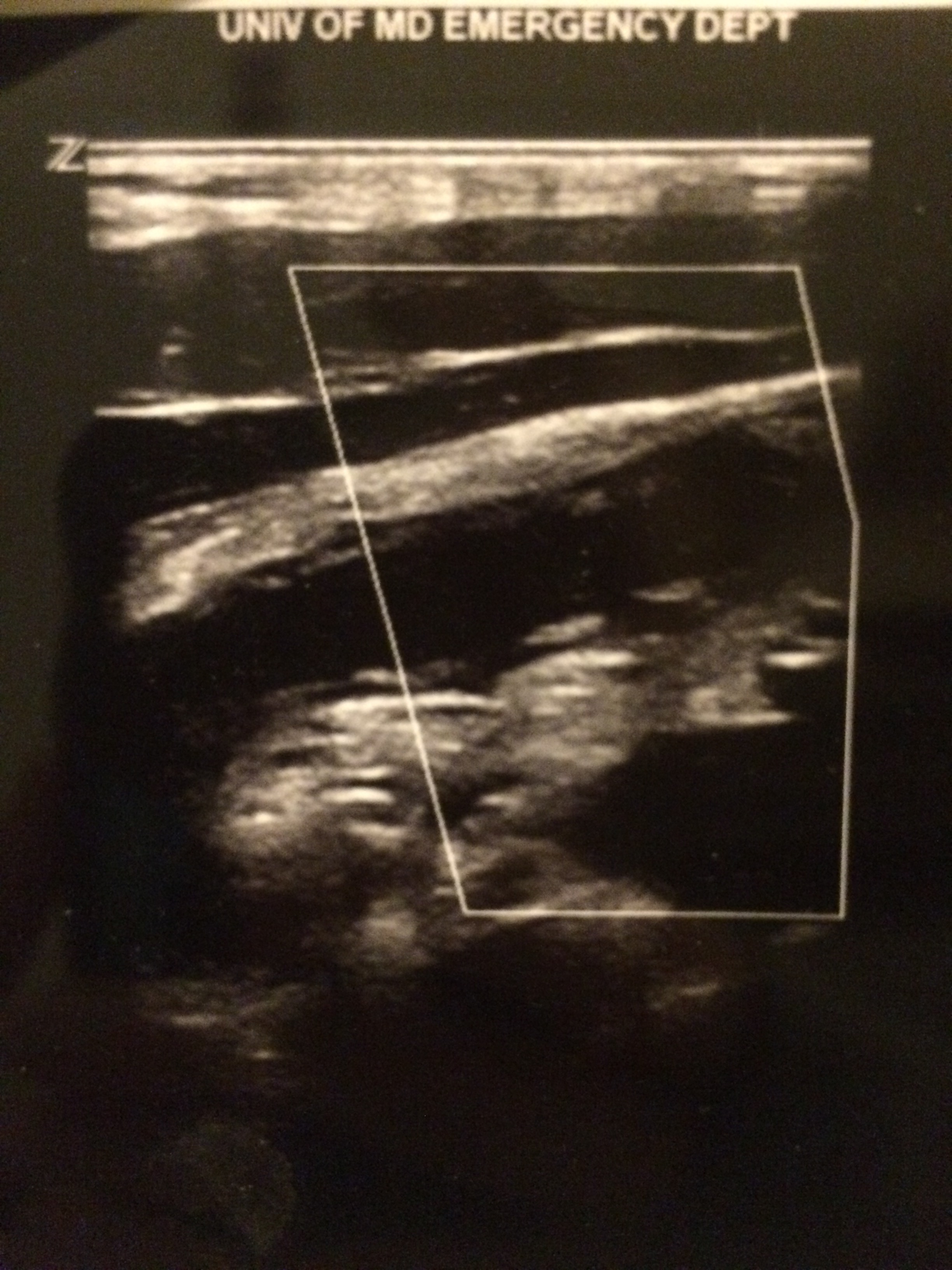
Parasternal long-axis of two different patients. What is the:
Answer:
Take home pearl: when there is fluid behind the heart, the parasternal long-axis view of the heart is helpful to distinguish between a pleural effusion and a pericardial effusion.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 11/9/2014 by Semhar Tewelde, MD
(Updated: 2/7/2026)
Click here to contact Semhar Tewelde, MD
Coronary Subclavian Steal Syndrome
Coronary subclavian steal syndrome (CSSS) is defined as coronary ischemia resulting from the reversal of flow in an internal mammary arterial graft usually secondary to subclavian stenosis.
Angiographic subclavian stenosis is defined as greater than 50% narrowing or greater than 20mmHg pressure difference across a lesion.
CSSS occurs in up to 4.5% of patients with prior CABG & common in older individuals with existing peripheral vascular disease.
CSSS most commonly manifests as stable angina, but frequently presents as unstable angina, acute myocardial infarction, acute systolic heart failure or even cardiogenic shock.
Screening for subclavian stenosis prior to CABG w/bilateral noninvasive blood pressure assessment, and a 15 mmHg or greater discordance should elicit further imaging.
Percutaneous revascularization is the first-line therapy for CSSS and has excellent long-term outcomes.
Sintek M, Coverstone E, Singh J. Coronary Sunclavian Steal Syndrome. Current Opinion in Cardiology. Issue: Volume 29(6) pgs. 506-513 November 2014.
Category: Orthopedics
Keywords: trauma, knee, dislocation (PubMed Search)
Posted: 11/8/2014 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Beware of spontaneous reduction masking the true injury!
Knee dislocations are rare due to supporting ligaments (MVCs, falls, sports)
but can be seen after minor trauma in obese patients.
Named by the direction of the displacement of the tibia relative to the femur
- Anterior and posterior are most common
Dislocations involve disruption of at least 2 of the major knee ligaments (ACL/PCL most common)
Usually associated with large hemarthrosis however capsular tearing may allow dissipation of the blood into adjacent soft tissue.
Consider a spontaneously reduced knee dislocation in those with a significant mechanism of injury in the setting of multidirectional instability,
Category: Pediatrics
Keywords: appendicitis, ultrasound, bedside (PubMed Search)
Posted: 11/8/2014 by Ashley Strobel, MD
Click here to contact Ashley Strobel, MD
Emergency Physician Bedside Ultrasound for Appendicitis
Why?
To reduce length of stay, improve patient care, and reduce radiation exposure in young patients.
How?
Start with pain medication so you get a better study. (Consider intranasal fentanyl for quicker pain relief and diagnostics in pediatrics.) Study results are also improved with a slim body habitus.
Place the patient supine
Use a high-frequency linear array transducer
Start at the point of maximal tenderness in the RLQ
Transverse and longitudinal planes "graded compression" to displace overlying bowel gas which usually has peristalsis (See Sivitz, et al article for images of "graded compression")
Appendix is usually anterior to the psoas muscle and iliac vein and artery as landmarks
Measure from outer wall to outer wall at the most inflamed portion of the appendix (usually distal end)
Example:
Positive study:
A non-compressible, blind-ending tubular structure in the longitudinal axis >6 mm without peristalsis (see second image above with 8.3 mm diameter measurement)
A target sign in the transverse view (see first image above)
Additional suggestive findings: appendiceal wall hyperemia with color Doppler, appendicoliths hyperechoic (white) foci with an anechoic (black) shadow, periappendiceal inflammation or free fluid
Negative study:
Non-visualization of the appendix with adequate graded compression exam in the absence of free fluid or inflammation.
Limitations for visualization and possible false negative result:
Retrocecal appendix and perforated appendix are difficult to visualize with US.
Pitfalls:
US has good specificity (93% in Sivitz et al article), but limited sensitivity (85% in Sivitz et al article), so trust your clinical judgement. You may need a MRI (pregnant/pediatrics) or CT as they have improved, but not perfect sensitivity.
Valesky, et al. Focus On: Ultrasound for Appendicitis. ACEP Now. June 2012.
Sivitz AB, Cohen SG, Tejani C. Evaluation of Acute Appendicitis by Pediatric Emergency Physician Sonography. Annals of Emerg Med. Oct 2014; 64: 358-363.
Category: Toxicology
Keywords: Digoxin, Cardioactive Steroids, Digitoxin, Digoxin-specific Fab Fragments (PubMed Search)
Posted: 11/7/2014 by Kishan Kapadia, DO
Click here to contact Kishan Kapadia, DO
Digoxin-specific antibodies are produced in immunized sheep and have high binding affinity for digoxin and, to a lesser extent, digitoxin and other cardiac glycosides. The Fab fragment binds free digoxin and once the digoxin-Fab complex is formed, the digoxin molecule is no longer pharmacologically active. The complex is renally eliminated and has a half-life of 14-20 hours (may increase 10-fold with renal impairment). Reversal of signs of digoxin/digitalis intoxication usually occurs within 30-60 minutes, with complete reversal varying up to 24 hours.
Contraindication: None known. Caution is warranted in patients with known sensitivity ot ovine (sheep) products. Product may contain traces of papain and caution advised in patients with allergies to papain, papaya extracts, chymopapain.
Adverse effects:
1) Monitor for potential hypersensitivity reactions and serum sickness
2) In patients with renal insufficiency and impaired renal clearance of dig-Fab complex, a delayed rebound of free serum digoxin levels may occur
3) Removal of the effect of digoxin/digitalis may exacerbate preexisting heart failure
4) Removal of digoxin/digitalis effect may cause hypokalemia
Laboratory interaction: Digoxin-Fab complex cross-reacts with the antibody commonly utilized in quantitative immunoassay techniques. This results in falsely high serum concentrations of digoxin due to measurement of the inactive Fab complex. Therefore, measure free digoxin levels, which may be useful for patients with renal impairment.
Dosing: Each vial of Fab product binds 0.5 mg of digoxin.
Digoxin-specific Fab (round up vial calculation)
# of vials = Digoxin concentration (ng/mL) x Pt Wt (kg)
100
Category: International EM
Keywords: Bioterrorism, anthrax, botulism, plague, smallpox, tularemia, viral hemmorrhagic fevers (PubMed Search)
Posted: 11/5/2014 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Background: The Centers for Disease Control and Prevention (CDC) classifies potential bioterrorism agents into three categories, with Category A the most deadly.
Category A: These are the highest priority agents/diseases because they:
Specific Category A Agents/Diseases:
Bottom Line: With the exception of smallpox, these disease still occur in various parts of the globe including the United States. As can be seen by the current Ebola epidemic in West Africa, the U.S. public health system and healthcare providers must be prepared to recognize and treat these agents.
Reference: http://www.bt.cdc.gov/agent/agentlist-category.asp
Category: Visual Diagnosis
Posted: 11/4/2014 by Haney Mallemat, MD
(Updated: 11/5/2014)
Click here to contact Haney Mallemat, MD
A patient presents post-motor vehicle crash with chest pain and dyspnea. The lung ultrasound is shown below. What's the diagnosis?
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Keywords: Airway, critical care, RSI, rapid sequence intubation (PubMed Search)
Posted: 11/3/2014 by John Greenwood, MD
(Updated: 11/4/2014)
Click here to contact John Greenwood, MD
Back 2 Basics Series: Your Simple RSI Checklist - SOAP ME
The use of a checklist during high stress medical procedures is often recommended. Rapid sequence intubation (RSI) is a classic situation where having a checklist can ensure adequate preparation however, if you don’t have a checklist – this simple mnemonic will make sure you are well prepared for a successful intubation.
| Mnemonic – “SOAP ME” | |
|---|---|
| Suction |
|
| Oxygen |
|
| Airways |
|
| Positioning |
|
| Monitors & Meds |
|
| EtCO2 & other Equipment |
|
The SOAP ME mnemonic is a quick and useful technique to remember only the basics of airway management and preparation. Always remember to also assign roles to team members and communicate clearly to maximize your chances of success.
Category: Cardiology
Posted: 11/2/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Heart Failure & Pulmonary Hypertension (Part II)
- HFpEF-PH management guidelines recommend the treatment of symptoms of congestion and volume overload, targeting LV relaxation and co-morbidities; including the management of pulmonary congestion, ischemia, sleep apnea, atrial fibrillation, and diabetes.
- Both atrial/ventricular dysrhythmias contribute to the mortality associated with HF & control of particularly atrial fibrillation, is an essential part of the early pulmonary vascular remodeling process.
- Both endothelin receptor antagonists (ERA) and prostanoids have been effective for PAH & clinical trials utilizing these agents have also been attempted in treatment of PH due to left heart disease, but have proven to be either neutral or even detrimental.
- Selective dilation of the pulmonary vessels in patients with postcapillary PH, without simultaneously ensuring the unloading of the LV, can cause profound pulmonary venous congestion resulting in sudden pulmonary edema, which greatly increases the morbidity in patients with this form of PH.
- Currently, the most compelling published data for pharmacological treatment targeting PH in HFpEF involves phosphodiesterase (PDE) inhibitor sildenafil.
Kanwar M, Tedford R, et al. Management of Pulmonary Hypertension due to Heart Failure with Preserved Ejection Fraction. Current Hypertension Reports. October 16, 2014.
Category: Pharmacology & Therapeutics
Keywords: penicillin, cephalosporin, allergy, cross-reactivity (PubMed Search)
Posted: 10/7/2014 by Bryan Hayes, PharmD
(Updated: 11/4/2014)
Click here to contact Bryan Hayes, PharmD
The cross-reactivity between cephalosporins and penicillins is significantly lower than the 10% figure many of us learned. In fact, the beta-lactam ring is rarely involved. So, when the warning pops up next time you order ceftriaxone in a penicillin-allergic patient, what should you do?
In a patient with a documented penicillin allergy, here is a simple chart to help determine when a cephalosporin is ok to use:
Common penicillins and cephalosporins with similar side chains include ampicillin/amoxicillin and cephalexin, cefaclor, cephadroxil, and cefprozil.
Campagna JD, et al. The use of cephalosporins in penicillin-allergic patients: a literature review. J Emerg Med 2012;42(5):612-20. [PMID 21742459]
Pichichero ME, et al. Penicillin and cephalosporin allergy. Ann Allergy Asthma Immunol 2014;112:404-12. [PMID 24767695]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: International EM
Keywords: Ebola, CDC, Isolation (PubMed Search)
Posted: 10/28/2014 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 10/29/2014)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Background:
ED Algorithm For Patients with Possible Ebola
If yes to both identification questions, then:
Bottom line:
Whether the patient has Ebola or not, a well-developed response is necessary for patient management and public health preparedness. The fear of the disease is much more widespread and impactful than the disease itself.
See the full algorithm, with more details at: http://www.cdc.gov/vhf/ebola/pdf/ed-algorithm-management-patients-possible-ebola.pdf
Category: Cardiology
Posted: 10/26/2014 by Semhar Tewelde, MD
(Updated: 2/7/2026)
Click here to contact Semhar Tewelde, MD
Heart Failure & Pulmonary Hypertension (Part I)
~50% of patients with heart failure & preserved ejection fraction (HFpEF) develop pulmonary hypertension (PH)
HFpEF with PH portends reduced survival and increased hospitalization rates compared to those without PH
HFpEF-PH is often confused with idiopathic pulmonary hypertension (IPAH) given the similar hemodynamics; differentiating them is challenging and requires careful consideration of clinical, radiologic, and hemodynamic data
|
| PAH | HFpEF |
| Clinical parameters: | ||
| Age | Typically 3rd–5th decade | Typically 6th–8th decade |
| Comorbidities (HTN, HLD, DM, CAD) | Rare | Common |
| Atrial arrhythmias | Rare | Common |
| Obstructive sleep apnea | Rare | Common |
| Echocardiographic parameters: | ||
| LA size/volume | Normal | Increased |
| LV diastolic function | Normal to mildly abnormal | Moderate to severely abnormal |
| Hemodynamic parameters: | ||
| Resting PAWP | Always <15 mmHg | May be < or >15 mmHg |
| Response to volume | PAWP <15 mmHg (increase ≤5 mmHg) | PAWP >15 mmHg (increase >5 mmHg) |
| Response to exercise | PAWP <15 mmHg (increase ≤5 mmHg) | PAWP >15 mmHg (increase >5 mmHg) |
(Table reproduced from article)
Kanwar M, Tedford R, et al. Management of Pulmonary Hypertension due to Heart Failure with Preserved Ejection Fraction. Current Hypertension Reports. October 16, 2014
Category: Orthopedics
Keywords: Osteoporosis, elderly, (PubMed Search)
Posted: 10/25/2014 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Iliocostal syndrome aka iliocostal friction syndrome
Consider this entity in an elderly patient with osteoporosis with unexplained abdomen/flank or back pain.
Osteoporosis and/or vertebral compression fractures can result in a narrowing of the distance between .
the lowest anterior rib and the top of the iliac crest producing pain where this rib contacts the pelvis.
This can be perceived as side or back pain. This pain can restrict walking leading to a possible misdiagnosis of spinal stenosis. Treatment is with physical therapy and therapeutic injection.
http://www.caringmedical.com/wp-content/uploads/2013/09/iliocostalis.syndrome.jpg
Category: Toxicology
Keywords: tetracycline (PubMed Search)
Posted: 10/23/2014 by Fermin Barrueto
(Updated: 2/7/2026)
Click here to contact Fermin Barrueto
Category: Neurology
Keywords: neurosurgery, trauma (PubMed Search)
Posted: 10/23/2014 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
The 2013 neurosurgery guidelines mention two of the more controversial therapies used in spinal cord injuries:
- “MAP Push” (maintaining the patient’s MAP 85-90mmHg, which theoretically increases the blood flow to the penumbra): evidence for the particular MAP goal is not great, but studies show that ICU level monitoring for the first 7-14 days improves outcome as patients may have delayed cardiovascular or pulmonary instability
- Steroids are not recommended anymore (they were an “option” in the previous guidelines)
Neurosurgery. 2013 Mar;72. Updated Guidelines for the Management of Acute Cervical Spine and Spinal Cord Injury. Resnick DK
Category: Critical Care
Keywords: choosing wisely, icu, critical care (PubMed Search)
Posted: 10/21/2014 by Feras Khan, MD
(Updated: 2/7/2026)
Click here to contact Feras Khan, MD
Choosing Wisely in the ICU
The Critical Care Societies Collaborative came up with this list for ICU providers
1. Don’t order diagnostic tests at regular intervals (such as every day) but rather in response to specific clinical questions. Do you really need a daily INR check or CBC check in all ICU patients? Really?
2. Don’t transfuse red blood cells in hemodynamically stable, non-bleeding ICU patients with a hemoglobin concentration greater than 7 g/dl. See last week’s Pearl!
3. Don’t use parental nutrition in adequately nourished critically ill patients within the first seven days of an ICU stay. TPN is the Cinnamon Toast Crunch of fungi.
4. Don’t deeply sedate mechanically ventilated patients without a specific indication and without daily attempts to lighten sedation. Use as little as possible when you can.
5. Don’t continue life support for patients at high risk for death or severely impaired functional recovery without offering patients and their families the alternative of care focused entirely on comfort. Engage families early in the hospital stay regarding aggressive life-sustaining treatments. Get palliative care involved in the ED!
Crit Care Med. 2014 Nov;42(11):2437-8. doi: 10.1097/CCM.0000000000000696.
Angus DC1, Deutschman CS, Hall JB, Wilson KC, Munro CL, Hill NS.
Category: Visual Diagnosis
Posted: 10/20/2014 by Haney Mallemat, MD
(Updated: 11/4/2014)
Click here to contact Haney Mallemat, MD
13 year-old right-hand dominant following assault with blunt object. What’s the diagnosis?

Monteggia Fracture
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 10/19/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Cardiovascular Morbidity & Sleep Apnea
Obstructive sleep apnea (OSA) is characterized by sleep-related periodic breathing, upper-airway obstruction, sleep disruption, and hemodynamic perturbations
Epidemiological data shows a strong association between untreated OSA & cardiovascular morbidity/mortality
Two recent studies by Gottlieb et al. (1) & Chirinos et al. (2) elucidated two important explicit and complicit treatment considerations for OSA
(1) In moderate-to-severe obstructive sleep apnea, the use of CPAP alone during sleep may ameliorate systemic hypertension and cardiovascular risk, even in patients who do not have "subjective" sleepiness
(2) Weight loss combined with CPAP use may further decrease cardiovascular morbidity
Basner R. Cardiovascular Morbidity and Obstructive Sleep Apnea. N Engl J Med 2014; 370:2339-2341 June 12, 2014
Category: Orthopedics
Keywords: Segond, Reverse, Fracture (PubMed Search)
Posted: 10/19/2014 by Michael Bond, MD
Click here to contact Michael Bond, MD
The Reverse Segond Fracture
Most people have heard of a segond fracture (avulsion fracture of the lateral tibeal platuea) seen on knee xrays which is a marker for Anterior Cruciate Ligament and medial meniscus injuries. See Pearl https://umem.org/educational_pearls/1015/
However, there is also a Reverse Segond Fracture that is another benign appearing avulsion fracture of the medial tibeal plateau that is marker for significant injury to the Posterior Cruciate Ligament (PCL).
If a Segond or Reverse Segond Fracture is seen consider immobilzing the patients knee until they can follow up with Orthopedics and/or get an MRI to determine if additional injuries are present.
