Category: Critical Care
Keywords: NIPPV (PubMed Search)
Posted: 4/7/2015 by Feras Khan, MD
Click here to contact Feras Khan, MD
Cabrini L et al. Noninvasive ventilation and survival in acute care settings: a comprehensive systematic review and metaanalysis of randomized controlled trials. Crit Care Med 2015; 43:880-888.
Category: Visual Diagnosis
Posted: 4/6/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
25 year-old male with the acute onset of right flank pain. Ultrasound of the right flank is shown. What's the diagnosis?
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 4/5/2015 by Semhar Tewelde, MD
(Updated: 2/7/2026)
Click here to contact Semhar Tewelde, MD
The Heart Is Just a Muscle
- Heart failure and peripheral myopathies share similar symptoms such as exertional fatigue, weakness, and dyspnea.
- The role of endomyocardial biopsy (EMB) to aid in the diagnosis of new-onset heart failure is controversial and major society guidelines recommend against this procedure in the routine evaluation of patients with heat failure.
- Nevertheless when symptoms of heart failure persist despite conventional imaging modalities and treatment one must consider uncommon conditions, such as mitochondrial disorders.
- Mitochondrial disorders are characterized as clinical syndromes and patients can present with any one of the following: ophthalmoplegia, proximal muscle weakness, isolated myopathy with exercise intolerance and myalgia, severe myopathy of infancy or childhood, or multisystem involvement with myopathy.
- Myocardial tissue is highly dependent on mitochondria for energy production and is therefore susceptible to defects in mitochondrial function. Cardiac manifestations of these syndromes include both arrhythmias and cardiomyopathy.
McGarrah R. et al. The Heart is Just a Muscle. Circulation. March 2015.
Category: Pharmacology & Therapeutics
Keywords: clindamycin, SSTI, skin infection, Bactrim, trimethoprim-sulfamethoxazole (PubMed Search)
Posted: 3/20/2015 by Bryan Hayes, PharmD
(Updated: 4/4/2015)
Click here to contact Bryan Hayes, PharmD
For many institutions, clindamycin is not as good as it used to be for methicillin-resistant Staph aureus (MRSA). When treating skin and soft tissue infections (SSTI), this can be challenging. Clindamycin still covers skin strep species very well, but not always the staph. On the other hand, trimethoprim-sulfamethoxazole (TMP-SMX) covers staph really well, but not so much the strep.
What They Did
A new double-blind, multicenter, randomized study in NEJM compared these two antibiotics in 524 patients with uncomplicated skin infections who had cellulitis, abscess larger than 5 cm, or both. All abscesses underwent incision and drainage. The primary outcome was clinical cure rate 7-10 days after the end of treatment.
What They Found
There was no difference in clinical cure rate between the two groups (80.3% for clindamycin, 77.7% for TMP-SMX).
Problems with the Study
Application to Clinical Practice
Unknown. This study seems to suggest TMP-SMX might be ok in uncomplicated cellulitis even though we assume strep species are the causitive organism. However, we already know cephalexin is equivalent to cephalexin + TMP-SMX from the 2013 study by Pallin et al. Why not just use cephalexin which has less adverse effects than TMP-SMX?
With such low clindamycin resistance, even to the staph species, perhaps that is why the two treatments were similar. Also, why did successfully drained abscesses need antibiotics? Finally, there were many exclusion criteria which eliminated many of the patients we see in the ED.
For a different, critical perspective of this NEJM study, Dr. Ryan Radecki gives his thoughts on his EM Lit of Note blog.
Miller LG, et al. Clindamycin vs. Trimethoprim-Sulfamethoxazole for Uncomplicated Skin Infections. N Engl J Med 2015;372(12):1093-103. [PMID 25785967]
Pallin DJ, et al. Clinical Trial: Comparative Effectiveness of Cephalexin Plus Trimethoprim-Sulfamethoxazole Versus Cephalexin Alone for Treatment of Uncomplicated Cellulitis: A Randomized Controlled Trial. Clinical Infectious Diseases 2013;56(12):1754-62. [PMID 23457080]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: International EM
Keywords: Polio, enterovirus D68, acute flaccid paralysis (PubMed Search)
Posted: 4/1/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Background:
Enterovirus D68
Is there a relationship between Enterovirus D68 and the outbreak of acute flaccid myelitis?
Bottom Line
http://www.cdc.gov/non-polio-enterovirus/about/ev-d68.html
http://www.thelancet.com/journals/laninf/article/PIIS1473-3099%2815%2970093-9/abstract
Category: Critical Care
Posted: 3/31/2015 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Mechanical Ventilation in the ED
Category: Visual Diagnosis
Posted: 3/30/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
35 year-old male presents with increasing difficulty swallowing and tenderness in the floor of him mouth. What's the diagnosis?

Ludwig's angina
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Orthopedics
Keywords: back pain, medication seeking (PubMed Search)
Posted: 3/28/2015 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
The ED clinician must be able to distinguish between true pathologic back pain and nonorganic back pain.
Waddell’s signs are physical exam findings that can aid in making this important distinction and can be remembered by the acronym “DORST” (Distraction, Over-reaction, Regional disturbances, Simulation tests and Tenderness).
Superficial, non-anatomic, or variable tenderness during the physical exam suggests a non-organic cause.
The clinician may also simulate back pain through provocative maneuvers such as axial loading of the head or passive rotation of the shoulders and pelvis in the same plane. Neither maneuver should elicit low back pain.
There may be a discrepancy between the symptoms reported during the supine and sitting straight leg raise (SLR). The seated version of the test, sometimes termed the distracted SLR, can be performed while distracting the patient or appearing to focus on the knee. Further, radicular pain elicited at a leg elevation of less than 30° degrees is suspicious because the nerve root and surrounding dura do not move in the neural foramen until an elevation of more than 30° degrees is reached.
Sensory and motor findings suggestive of a nonorganic cause include stocking, glove or non-dermatomal sensory loss or weakness that can be characterized as “give-way,” jerky or cogwheel.
Finally, gross overreaction is suggested by the exaggerated, inconsistent painful responses to a stimulus.
Waddell’s signs, especially if three or more are present, correlate with malingering and functional complaints (physical findings without anatomic cause). When combined with shoulder motion and neck motion producing lower back pain, Waddell’s signs predict a decreased probability of the individual returning to work.
That said, Waddell’s signs should never be used independently because they lack the sensitivity and specificity to rule out true organic pathology. Further, our focus should be on evaluating for medical emergencies. Malingering and psychosocial causes of pain are diagnosis of exclusion.
Category: Pediatrics
Keywords: diabetic ketoacidosis, DKA (PubMed Search)
Posted: 3/27/2015 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
ISPAD (International Society for Pediatric and Adolescent Diabetes) Updated their Guidelines for Pediatric Diabetic Ketoacidosis (DKA) in 2014
Fluids:
· Begin fluid repletion with 10-20ml/kg of 0.9% NS over 1-2 hours
· Estimate losses (mild DKA <5%, moderate 5-7%, severe ~10%) and replete evenly over 48 hours
o Use NS, Ringers or Plasmalyte for 4-6 hours
o Afterwards use any crystalloid, tonicity at least 0.45% NaCl
· Add 5% glucose to IV fluid when glucose falls below 250-300mg/dL
Insulin
· No bolus
· Low dose 0.05 - 0.1U/kg/hr AFTER initiating fluid therapy
o higher incidence of cerebral edema in patients given insulin in 1st hour
· Short acting subQ insulin lispro or aspart can be substituted for drip in uncomplicated mild DKA
· Give long acting subQ insulin at least 2 hours before stopping infusion to prevent rebound
Potassium
· If K low (< 3.3): add 40mmol/L with bolus IV fluids (20mmol/L if rate > 10ml/kg/hr)
· if K normal (3.3-5): add 40mmol/L when insulin is started
· If K high (> 5): add 40mEq/L after urine output is documented
Bicarb
· No role for bicarbonate in treatment of Pediatric DKA
o No benefit, possibility of harm (paradoxical CNS acidosis)
Wolfsdorf JI, Allgrove J, Craig ME, et al. Diabetic ketoacidosis and hyperglycemic hyperosmolar state. Pediatr Diabetes. 2014;15 Suppl 20:154-79.
Category: Neurology
Keywords: spinal cord, numbness, herpes, CSF (PubMed Search)
Posted: 3/25/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Elsberg syndrome is sacral radiculitis caused by a viral infection, most commonly herpes simplex virus type 2 (HSV-2) - whether a primary infection or a reactivation. The typical patient is a young sexually active woman presenting wtih acute transient urinary retention and sensory lumbosacral symptoms, such as dull pain in anorectal region, paresthesias, loss of sensation or flaccid paresis of leg muscles. Patients can also have constipation or erectile dysfunction.
The presence of inguinal lymphadenopathy and/or anogenital rash can be important clues but are not necessary for diagnosis. CSF may show mild to moderate pleocytosis, with a mild elevation in proteins. Herpes PCR in the CSF may be positive as well. The MRI may show varying degrees of root or lower spinal cord edema with hyperintensity of T2-weighted images.
In immunocompetent patient, the disease usually self limiting, usually resolving in 4-10 days, but can be progressive and ascending in patients with immunocompromise, such as HIV or cancer. Antiviral treatment may shorten the duration of illness in cases with confirmed herpes, either oral or IV.
Eberhardt O, K ker W, Dichgans J, Weller M. HSV-2 sacral radiculitis (Elsberg syndrome). Neurology 63(4), 24 August 2004, 758-759
Category: Critical Care
Keywords: mechanical ventilation, ARDS, PEEP (PubMed Search)
Posted: 3/24/2015 by John Greenwood, MD
(Updated: 2/7/2026)
Click here to contact John Greenwood, MD
Stop looking for the “Best PEEP”, aim for a “Better PEEP”
Mechanical ventilation settings in the patient with acute respiratory distress syndrome (ARDS) need to provide adequate gas exchange and prevent ventilator induced lung injury (VILI). Positive end-expiratory pressure (PEEP) is often prescribed with consideration of the patient’s FiO2 requirement, estimated chest wall compliance, and hemodynamic tolerance.
So what is the best strategy for PEEP prescription?
In a recent review, Gattinoni & colleagues analyzed a number of the recent studies examining PEEP optimization. In this paper, the authors conclude that there is no “Best PEEP,” and regardless of the level chosen there will be some degree of intratidal recruitment-derecruitment and VILI. They go on to recommend a PEEP prescription strategy that reflects the severity of ARDS using the patient’s PaO2/FiO2 or P/F ratio.
Bottom line: There is no “Best PEEP” however, a “Better PEEP” is one that is primarily tailored to the severity of the patient’s ARDS, but also compensates for chest wall resistance and minimizes hemodynamic compromise.
References
Follow me on Twitter @JohnGreenwoodMD
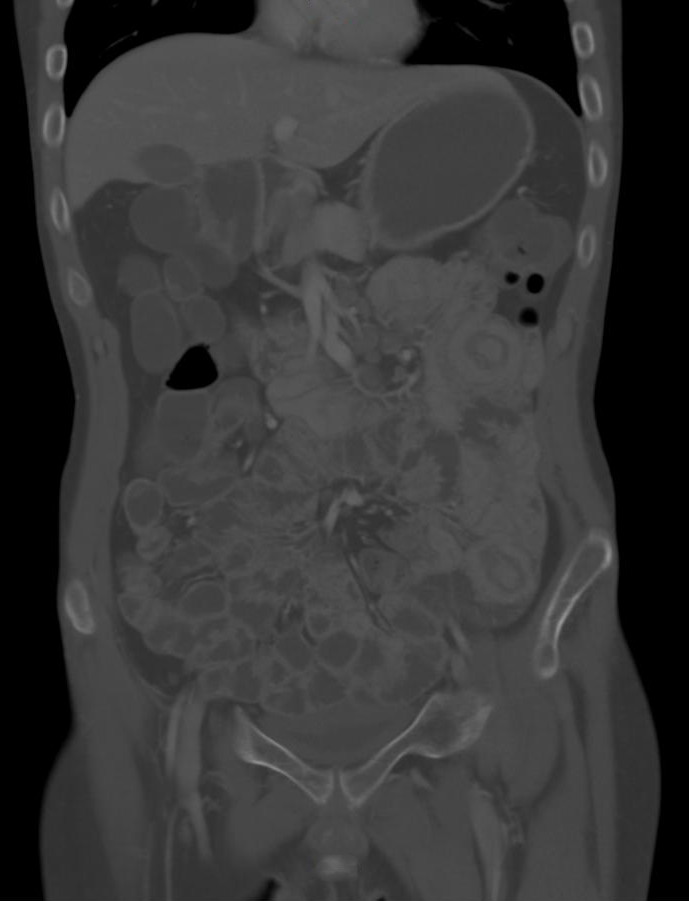
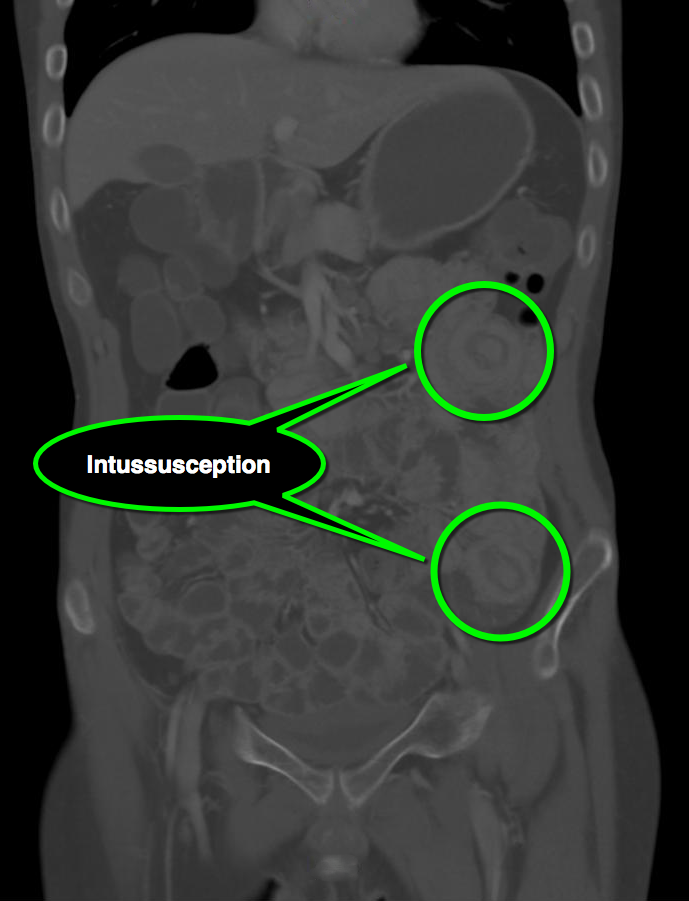
Category: Visual Diagnosis
Posted: 3/23/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
25 year-old male with autoimmune enteropathy presents with intractable vomiting and diarrhea for 7 days. What's the diagnosis?
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 3/22/2015 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Acute Pericarditis
- Pericarditis has numerous etiologies; in developed countries 80-90% of cases are idiopathic/viral & 10-20% of cases are most commonly post-cardiac injury syndromes, connective-tissue diseases, or cancer.
- Diagnosis requires at least two of the following symptoms or signs: chest pain, pericardial friction rub, typical electrocardiographic changes, and pericardial effusion.
- Since pleuritic chest pain has many possible causes, pericarditis should be diagnosed with caution in the absence of other clinical criteria, additionally a friction rub & ECG findings may be transient making the diagnosis even more challenging.
- Data from a recent RCT indicated that pericardial effusions are present in ~2/3 of patients; the vast majority are small and of no concern, nonetheless an echocardiogram is routinely indicated and if present should be carefully followed to assess for tamponade.
- Treatment for idiopathic/viral cases of pericarditis consistents of NSAIDs & colchicine.
LeWinter, MM. Acute Pericarditis. NEJM. Dec 18, 2014 Vol 371 No 25.
Category: Orthopedics
Keywords: Back Pain, Elderly (PubMed Search)
Posted: 3/21/2015 by Michael Bond, MD
Click here to contact Michael Bond, MD
It is commonly taught that radiographs are not needed in non-traumatic back pain unless the patient is <18 or > 65 years old. Several studies have started to disprove this in the pediatric population, and a recent study in JAMA is giving some weight to not having to do this in the eldery.
The JAMA study was a prospective cohort of 5239 patients over age 65 who presented to a PCP or urgent care center in three different health systems from 2011-2013 with a complaint of back pain without radiculopathy. Patients were determined to have early imaging if they had a plain films, CT, or MRI done within 6 weeks of their initial visit for back pain. The primary outcome measure was back or leg-pain related disability at 12 months when comparing those that had early imaging versus late (> 6 weeks). They excluded patients with prior surgery, prior back pain, or if they had a cancer visit in the prior year.
At one year they found that there was no statistical difference in the primary outcome of back or leg-pain related disability at one year. The early imaging did pick up more fractures of the spine, but again no change in long term outcomes. The serious diagnoses were summarized in this graph.
This study was not done in the Emergency Medicine setting, and our patients may not be equivilant, but it suggests that we do NOT have to get radiographs on all patients over 65 years old with non-traumatic back pain without radiculopathy. If you are not going to get radiographs make sure your patient has clear discharge instructions on what to return for and that they should follow up with their primary care provider within a week.
A link to the full article is here http://jama.jamanetwork.com/article.aspx?articleid=2203801
Jarvik JG, Gold LS, Comstock BA, et al. Association of Early Imaging for Back Pain With Clinical Outcomes in Older Adults. JAMA. 2015;313(11):1143–11. doi:10.1001/jama.2015.1871.
Category: Pediatrics
Keywords: Upper GI Bleeds (PubMed Search)
Posted: 3/20/2015 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Category: Toxicology
Keywords: acetaminophen toxicity, NAC, hepatic toxicity (PubMed Search)
Posted: 3/19/2015 by Hong Kim, MD
(Updated: 2/7/2026)
Click here to contact Hong Kim, MD
Elevation of AST or ALT >1000 after acute ingestion of acetaminophen indicate hepatic toxicity. N-acetylcysteine (NAC) is an effective treatment for acute acetaminophen poisoning. However, in a setting a significant transaminitis, (> 1000s) NAC infusion is continued beyond the routine 21-hour protocol.
Currently, there is no specific guideline or “level” of AST or ALT where discontinuing NAC is deemed safe and appropriate.
A recent retrospective study (n = 37 patients with 343 pairs of AST/ALT) evaluated AST/ALT ratio as a possible indicator for discontinuing NAC infusion after an acute acetaminophen induced hepatic toxicity.
This study found that post peak AST/ALT ratio of < 0.4 had sensitivity of 99% for identifying patients with resolving hepatic injury.
This finding requires validation prior to clinical application but this may be the first step to identifying a safe indicator to help guide clinician when NAC can be discontinued safely.
Mcgovern AJ et al. Can AST/ALT ratio indicate recovery after acute paracetamol poisoning? Clin Toxciol 2015;53:164-167.
Category: International EM
Keywords: Emergency Management, mitigation, preparedness, response, recovery (PubMed Search)
Posted: 3/18/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Whether in the U.S. or overseas, there are four main phases of emergency management:
fas.org/sgp/crs/homesec/R42845.pdf
Category: Critical Care
Posted: 3/17/2015 by Haney Mallemat, MD
(Updated: 3/18/2015)
Click here to contact Haney Mallemat, MD
The results of a multi-center trial from the UK, the ProMISe trial, were just released and it confirms what two prior studies (i.e., ProCESS and ARISE) have already shown; there does not appear to be any difference in mortality when septic patients are treated with a strategy of early-goal directed therapy as compared to usual care.
Patients were included in the ProMISe trial if they were in septic shock and were then randomized to either the EGDT group (630 patients) or the usual care group (630 patients); a total of 1,260.
The primary end-point was all cause mortality at 90 days and there was no difference shown in the primary outcome. There were no differences found in the measured secondary outcomes (e.g., serious adverse events)
This trial adds to the evidence that septic patients may not benefit from protocolized (i.e., EGDT) care versus usual care. One explaination why, is that our "usual care" in 2015 has significantly changed since the introduction of EGDT in 2001.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
http://www.nejm.org/doi/pdf/10.1056/NEJMoa1500896
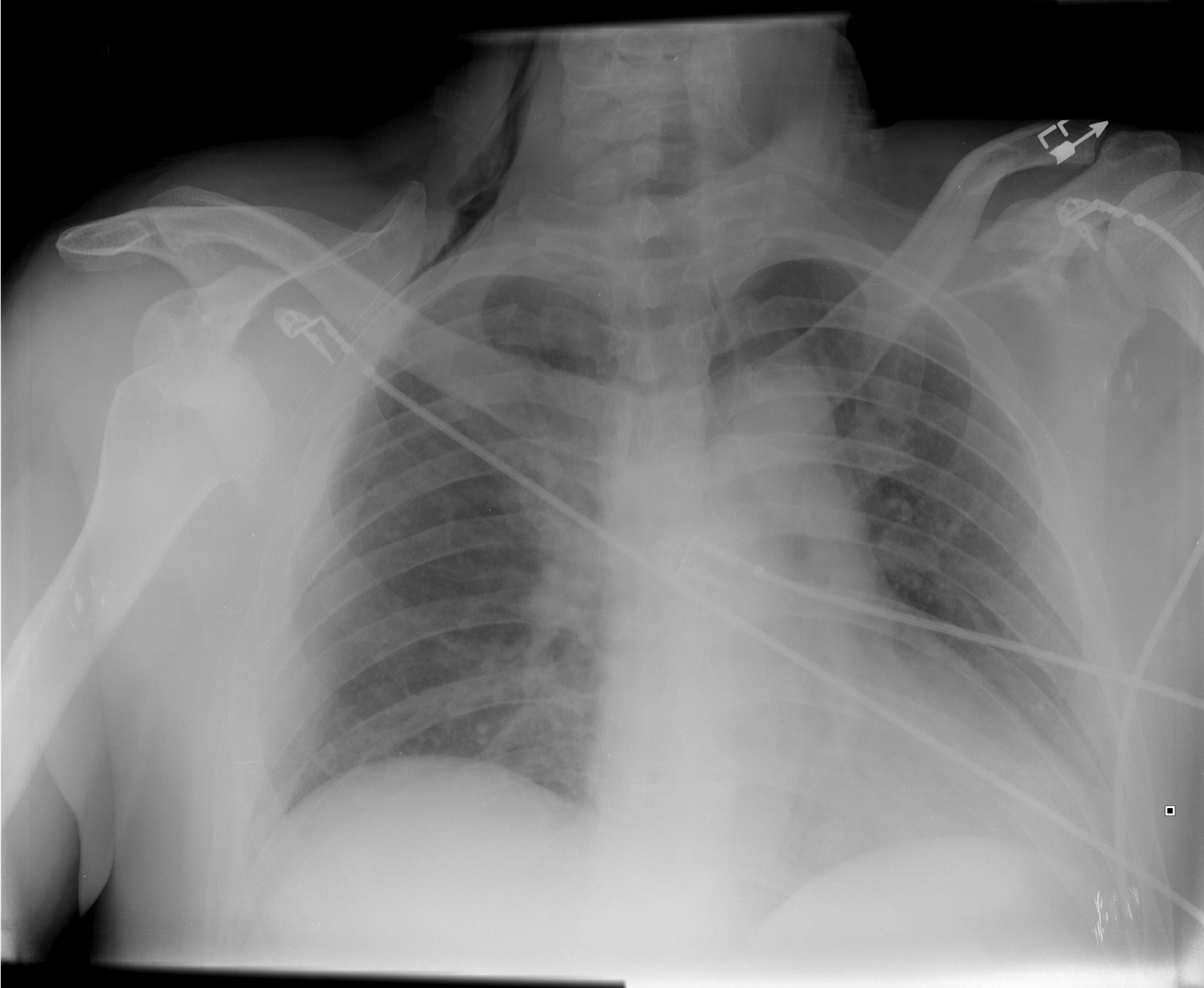
Category: Visual Diagnosis
Posted: 3/16/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
How many abnormalities can you find below?
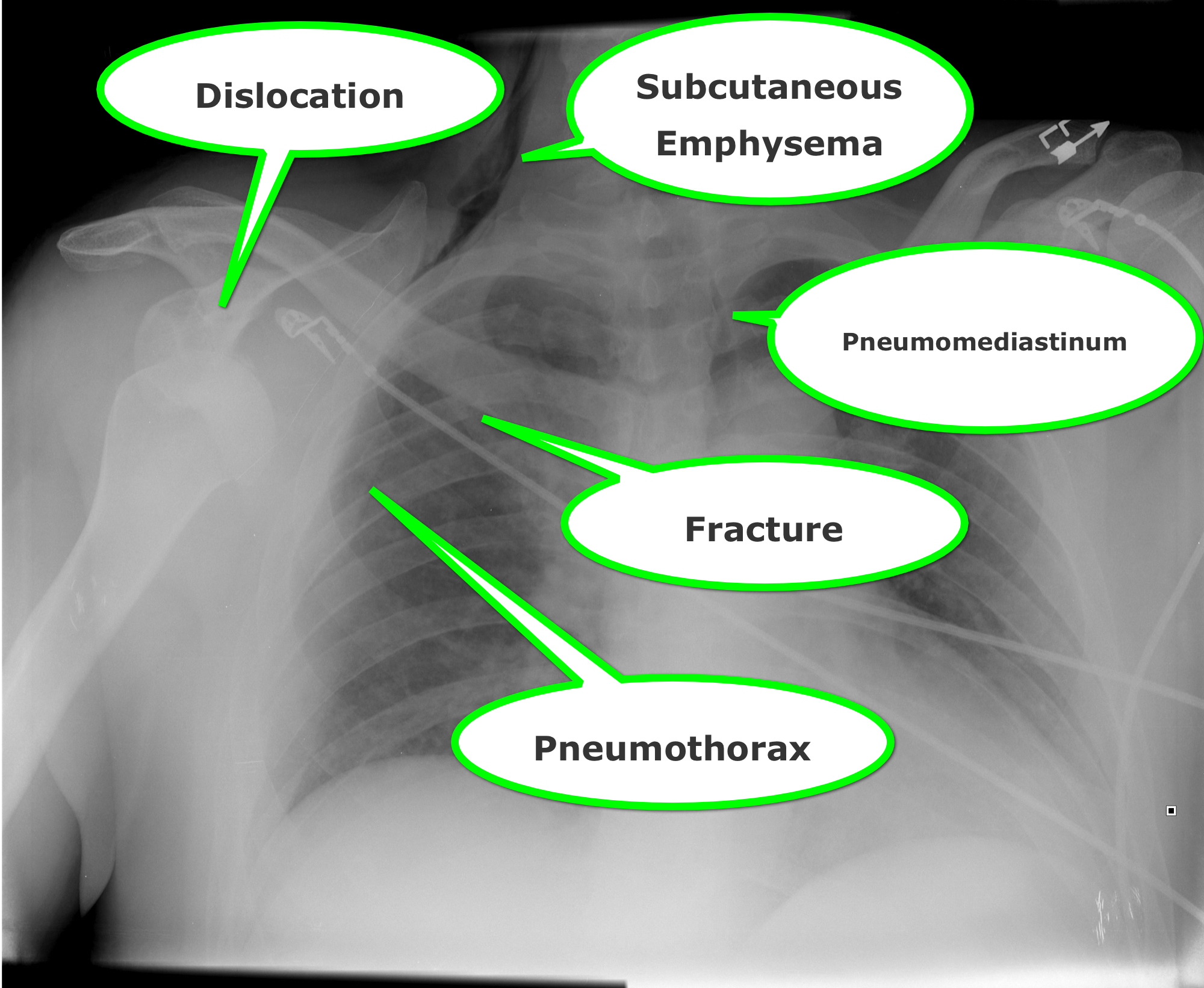
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Orthopedics
Keywords: x-ray, child abuse, fracture dating (PubMed Search)
Posted: 3/14/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Imaging plays an important role in the evaluation of child abuse.
It aids in the identification, evaluation and in treatment.
Additionally, it is often the only objective evidence of abuse available to the courts.
It is often discovered through two means.
1) Injuries/fractures that are inconsistent with the alleged mechanism of injury.
2) Pathognomonic fracture patterns are found on routine radiographs
The ED physician should not attempt to precisely "date" the injury.
That said, soft tissue swelling resolves in 2-5 days. The periosteum becomes radiodense in 7 to 10 days. In subtle fractures this may be the only radiographic finding. If there is no evidence of bone healing (periosteal reaction), the fracture is less than 2 weeks old. Callus formation and resorption of the bone along the fracture line begins at 10 to 14 days. The callus is visible for up to 3 months. Bone remodeling continues for up to one year.
Emergency Radiology, chapter 22, "pediatric considerations" by Ken Butler and Martin Pusic.
