Category: Pharmacology & Therapeutics
Keywords: antibiotic, IV, diarrhea (PubMed Search)
Posted: 11/25/2014 by Bryan Hayes, PharmD
(Updated: 12/6/2014)
Click here to contact Bryan Hayes, PharmD
Many of the oral antibiotics prescribed in the ED have good bioavailability. So, a one-time IV dose before discharge generally won't provide much benefit.
In fact, a new prospective study found that a one-time IV antibiotic dose before ED discharge was associated with higher rates of antibiotic-associated diarrhea and Clostridium difficile infection. [1] One-time doses of vancomycin for SSTI before ED discharge are also not recommended (see Academic Life in EM post).
Bottom Line
Though there are a few exceptions, if a patient has a working gut, an IV dose of antibiotics before ED discharge is generally not recommended and may cause increased adverse effects. An oral dose is just fine.
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Toxicology
Keywords: Sympathomimetic toxicity, Synthetic cathinones, Rhabdomyolysis (PubMed Search)
Posted: 12/4/2014 by Kishan Kapadia, DO
Click here to contact Kishan Kapadia, DO
Sympathomimetic toxicity is a known toxidrome that is complicated by the development of rhabdomyolysis. There are multiple stimulant agents that induce sympathomimetic toxicity including, synthetic cathinones, cocaine, amphetamines, and methamphetamines.
A recent retrospective, single-center, chart review in the age range of 14-65 years sought to determine the prevalence of rhabdomyolysis in patients with sympathomimetic toxicity and compare rates among patients using specific agents. Rhabdomyolysis and severe rhabdomyolysis were defined as CK>1000 and 10,000 IU/L, respectively.
Rhabdomyolysis occurred in 42% of study subjects (43/102)
Prevalence in 89 subjects due to a single-stimulant exposure:
Rhabdomyolysis
1) Synthetic cathinone (MDPV, alpha-PVP) 63% (12/19)
2) Methamphetamine 40% (22/55)
3) Cocaine 33% (3/9)
4) Other single agents (methylphenidate, pseudoephedrine, phentermine) 0% (0/6)
Severe Rhabdomyolysis
1) Synthetic cathinone 26% (5/19)
2) Methamphetamine 3.6% (2/55)
3) Cocaine 11% (1/9)
4) Other single agents (methylphenidate, pseudoephedrine, phentermine) 0% (0/6)
In this study, patients exposed to synthetic cathinones were more likely to develop rhabdomyolysis and severe rhabdomyolysis compared to the non-cathinone-exposed group.
Bottom Line:
Be aware of this increased risk from synthetic cathinones along with other stimulants. Treat aggressively with IV fluids, rapid correction of hyperthermia, benzodiazepines to control manifestations of sympathomimetic toxicity to reduce muscle activity and metabolic demand.
O'Connor AD, Padilla-Jones A, Gerkin AD, et al. Prevalence of Rhabdomyolysis in Sympathomimetic Toxicity: a Comparison of Stimulants. J Med Toxicol 2014; Dec 3; Epub ahead of print.
Category: International EM
Keywords: Global Health, emergency care, acute care, research (PubMed Search)
Posted: 12/3/2014 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
In December 2013, Academic Emergency Medicine published the results of the 2013 consensus conference that focused on advancing global health and emergency care research.
As noted in the issue’s executive summary, “Emergency physicians are uniquely poised to address challenges in health services, health care systems development and management, and emerging global disease burdens (both communicable and noncommunicable). “
The consensus conference covered developing research in eight focus areas, including understanding of cardiac and injury resuscitation, ethics of research, health systems development, and the education of future global health leaders.
For anyone interested in global health and emergency care, this issue of Academic Emergency Medicine is an outstanding resource and roadmap to developing research. It can be found at: http://onlinelibrary.wiley.com/doi/10.1111/acem.2013.20.issue-12/issuetoc
Category: Critical Care
Posted: 12/2/2014 by John Greenwood, MD
Click here to contact John Greenwood, MD
Dynamic Measures of Intravascular Volume Assessment
The resuscitation of a patient in shock often requires the administration of intravenous fluid. Excessive fluid resuscitation can lead to worsening pulmonary edema, systemic edema, acid-base disturbances, as well as many other complications. There are a myriad of techniques to try and figure out if the patient needs more intravascular volume, but each has it’s pitfalls.
Recently, experts have recommend that we move away from using static measures of preload assessment such as central venous pressure (CVP) and instead focus on using dynamic measures for volume responsiveness.
Volume Responsiveness Defined: An increase of stroke volume of 10-15% after a 500 mL IV crystalloid bolus over 10-15 minutes.
Below is a chart describing key values, requirements, and contraindications for each of these dynamic measures of non-invasive intravascular volume assessment.
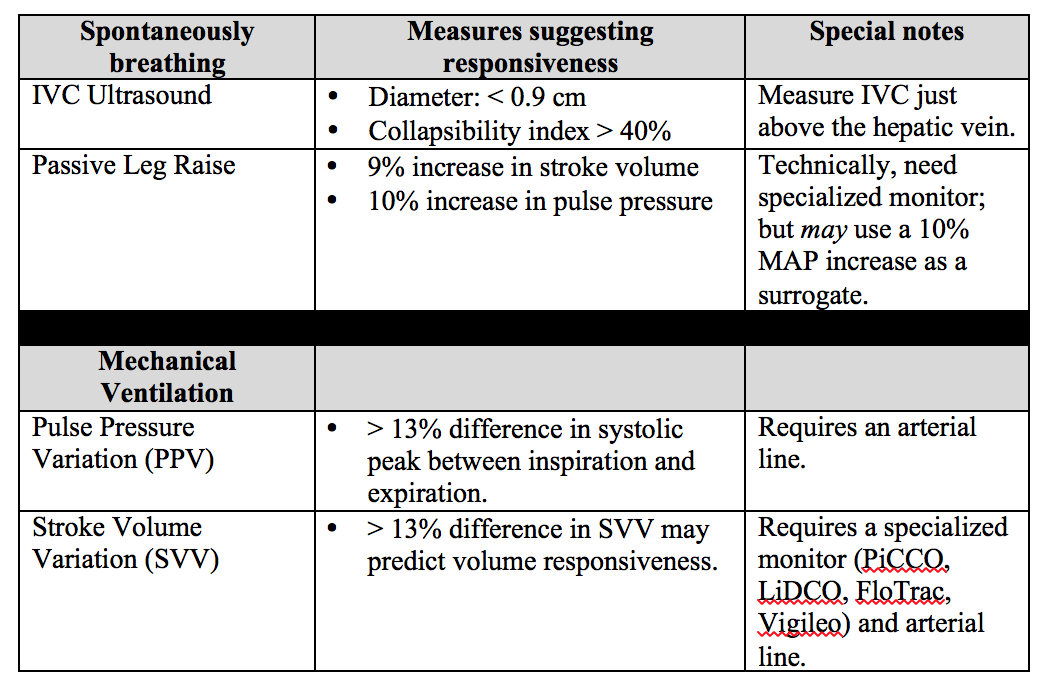
Important notes: PPV and SVV require the patient to be intubated with controlled tidal volumes. Arrhythmias and right heart failure make many of these measures invalid (except for PLR). Other methods of assessment not discussed include systolic pressure variation, left ventricular outflow track velocity time integral (LVOT VTI), and end-expiratory occlusion pressure (EEO).
Bottom Line: None of these measures are perfect and shouldn't be used in isolation to determine if the patient’s “tank is full”. Combine clinical judgment with these measures to get a best estimate of whether or not to give that next fluid bolus.
Reference
1. Enomoto TM, Harder L. Dynamic indices of preload. Crit Care Clin. 2010;26(2):307-21,
Follow Me on Twitter @JohnGreenwoodMD
Category: Visual Diagnosis
Posted: 12/1/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Patient presents with dyspnea. What's the diagnosis and name three potential causes (can be specific to the case or in general)?

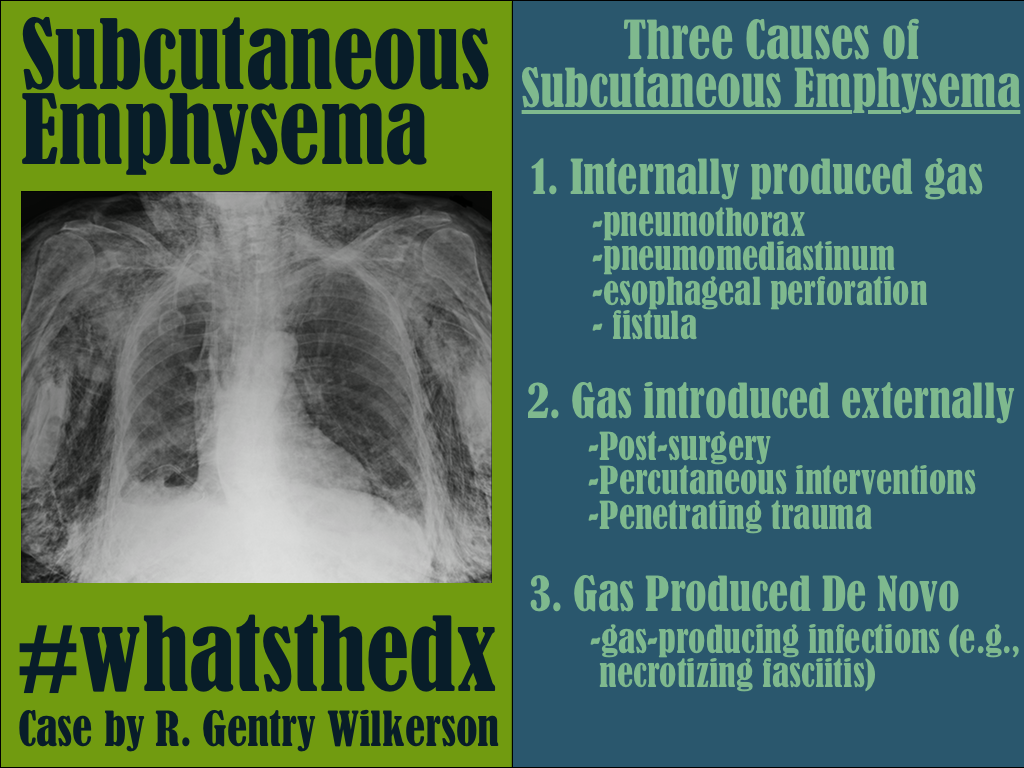
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Orthopedics
Keywords: back pain, red flag (PubMed Search)
Posted: 11/29/2014 by Michael Bond, MD
Click here to contact Michael Bond, MD
A recent meta-analysis of 14 studies looked at the typical red flags of back pain to see which ones actually truly increase the risk that the patient will have a fracture or malignancy.
The typical historical red flags that are taught are
And physical exam red flags are
However, this meta-analysis showed that the only red flags that actually increased the risk of fracture or malignancy were
So this study highlights that a lot of the red flags that we have learned do not actually increase the risk fracture or malignancy, although some like fever, IVDA, and immunocomproromised increase the risk of epidural abscesses, which was not addressed in this meta-analysis.
The take home point for me is that plain radiographs/CT scans are probably only needed in patients with older age, prolonged corticosteroid use, severe trauma or presence o contusion or abrasion. If you are really worried about others with back pain just proceed directly to MRI as the plain films/CT scans are not going to be very helpful.
Downie A, Williams CM, Henschke N, et al. Red flags to screen for malignancy and fracture in patients with low back pain. British Journal of Sports Medicine. 2014;48(20):1518–1518. doi:10.1136/bjsports-2014-f7095rep.
Category: Pediatrics
Keywords: dehydration (PubMed Search)
Posted: 11/28/2014 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Dehydration is a common pediatric ED presentation. Oral rehydration (although first choice) is often not possible secondary to patient cooperation and/ or persistent vomiting. Intravenous (IV) hydration is often difficult, requiring multiple attempts especially in the young dehydrated infant.
Hyaluronan is a mucopolysaccharude present in connective tissue that prevents the spread of substances through the subcutneous space. Hyaluronidase is a human DNA-derived enzyme that breaks down hyaluronan and temporarily increases its permeability, thereby allowing fluid to be absorbed with the capillary and lymphatic systems.
In one study, patients age 1 month to 10 years were randomized to recieve 20 mL/kg bolus NS via subcutaneous (SC) or IV route over one hour, then as needed. The mean volume infused in the ED was 334.3 mL (SC) vs 299.6 mL (IV). Succesful line placement occured in all 73 SC patients and only 59/75 IV patients. There was a higher proportion of satisfaction for clinicians and parents for ease of use and satisfaction, respectively.
Bottom line: Consider subcutaneous hyaluronidase faciliated rehydration in mild to moderately dehydrated children, especially with difficult IV access.
Spandorfer PR, et al. A Randomized Clinical Trial of Recombinant Human Hyaluronidase-Fcilitated Subcutaneous Versus Intravenous Rehydration in Mild to Moderately Dehydrated Children in the Emergency Department. Clinical Therapeutics, 2012; 34(11): 2232-2245.
Category: Toxicology
Keywords: Cyanide, smoke inhalation, lactate (PubMed Search)
Posted: 11/28/2014 by Hong Kim, MD
(Updated: 2/8/2026)
Click here to contact Hong Kim, MD
Cyanide poisoning is rare but highly lethal. Cyanide exposure can occur during residential fire (most common source of exposure) where combustion of synthetic materials (i.e. plastic and polyurethane) releases cyanide gas as well as other toxic gases, including carbon monoxide. Although carbon monoxide poisoning can be readily identified by CO-Hb level using CO-oximetry, serum/blood cyanide level is not readily available for acute management.
However, elevated lactate level (> 10 mmol/L ) has shown to be highly correlated with toxic level of cyanide (40 micromol/L or 1 mg/L) in smoke inhalation victims (Baude FJ et al. N Engl J Med 1991;325:1761-6).
Bottom line: when managing smoke inhalation victims, think about cyanide poisoning in addition to carbon monoxide poisoning and check the lactate level. Lactate > 10 mmol/L is suggestive of cyanide poisoning and should be treated with hydroxocobalamin.
Baude FJ et al. Elevated blood cyanide concentrations in victims of smoke inhalation N Engl J Med 1991;325:1761-6
Category: Neurology
Keywords: pseudotumor cerebri, visual loss, shunt (PubMed Search)
Posted: 11/27/2014 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
There are a few available options for treatment of visual loss due to idiopathic intracranial hypertension (IIH). The Idiopathic Intracranial Hypertension Treatment Trial (IIHTT), the first randomized, prospective, placebo-controlled trial for the treatment of patients with visual loss from IIH, which results were published earlier this year, provided substantial evidence for the first 2 options.
1. Weight loss
2. Carbonic anhydrase inhibitors, such as Acetazolamide
3. Therapeutic lumbar puncture (reserved for pregnant patients or for occasional flare-ups)
4. Surgery:
a. Optic nerve sheath fenestration (ONSF): visual acuity and fields improve in most cases, but symptoms may recur. Benefit? No hardware!
b. Shunts: ventriculoperitoneal (VP) and lumboperitoneal (LP) shunts are the most frequently used. No clear benefit for one over the other. VP shunts may be programmable.
c. Cerebral venous stenting: endovascular stenting of the transverse sinus may improve the symptoms in some people.
BONUS PEARL: The headache does not correlate with the lumbar opening pressure, degree of papilledema or amount of visual loss. None of the above-mentioned management strategies is meant for the treatment of the headache alone. For that, medical management with standard symptomatic treatments, avoiding opiates and barbiturates, is recommended. Surgery is not recommended for headache alone.
Friedman DI. Papilledema and idiopathic intracranial hypertension. Continuum. 2014 Aug;20(4 Neuro-ophthalmology)
Category: Critical Care
Posted: 11/25/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Running a successful resuscitation not only means doing everything right, but also remembering all the things that can go wrong. A.E.I.O.U. is a simple mnemonic that can help you remember the simple things that are sometimes forgotten during a medical resuscitation.
A – Advanced airway equipment to bedside, as well as checking the correct placement of the Airway if a patient is intubated in the field. Also consider adding another A, for Arterial line; early placement can help with pulse checks and an accurate assessment of blood pressure should there be return of spontaneous circulation (ROSC); the femoral site is fast and accurate.
E – End-tidal CO2 (ETCO2) helps detect ROSC. Ask for the ETCO2 monitor to be set up right after you receive notification of an arrest in transit; ETCO2 requires time to set-up / calibrate
I – Intraosseous line(s); compared to peripheral or central venous access, IO’s are faster, safer, and any medication can be administered through it, including vasopressors / inotropes.
O – Order (i.e., “who’s who in the Resus room?); You may be the team leader or you may be assisting, but it is important that you, and everyone else in the room, know their role prior patient arrival. If you are leading the resus, be sure everyone knows who you are, and assign everyone in the room a specific task (e.g., chest compressions, IO placement, etc.). If you are assisting and have not been assigned a task, ask the resus leader what you can do to help. If there is nothing immediate for you to do then take the initiative to de-clutter the room and step outside; be nearby and ready to help, if needed.
U – Ultrasound; can help prognosticate and detect reversible causes (e.g., pericardial tamponade). Have the ultrasound machine in the room prior to patient arrival. It should be powered on, with the proper probe connected, and in the proper mode. The most experienced ultrasonographer should scan the patient during a pulse check; experience is vital because hands-off time should be minimized.
*Tips for the Resuscitationist (#TFTR) is a new series to help you to better manage your critically ill patients. Do you have an idea for a topic or do you have a tip you would like to share? Send it to us via twitter @criticalcarenow (use (#TFTR)). You can also email us here.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 11/23/2014 by Haney Mallemat, MD
(Updated: 11/25/2014)
Click here to contact Haney Mallemat, MD
Patient with syncope and then falls down the stairs. What's the diagnosis? (hint: be very,very careful)

Right subdural hematoma and left subarachnoid hemorrhage
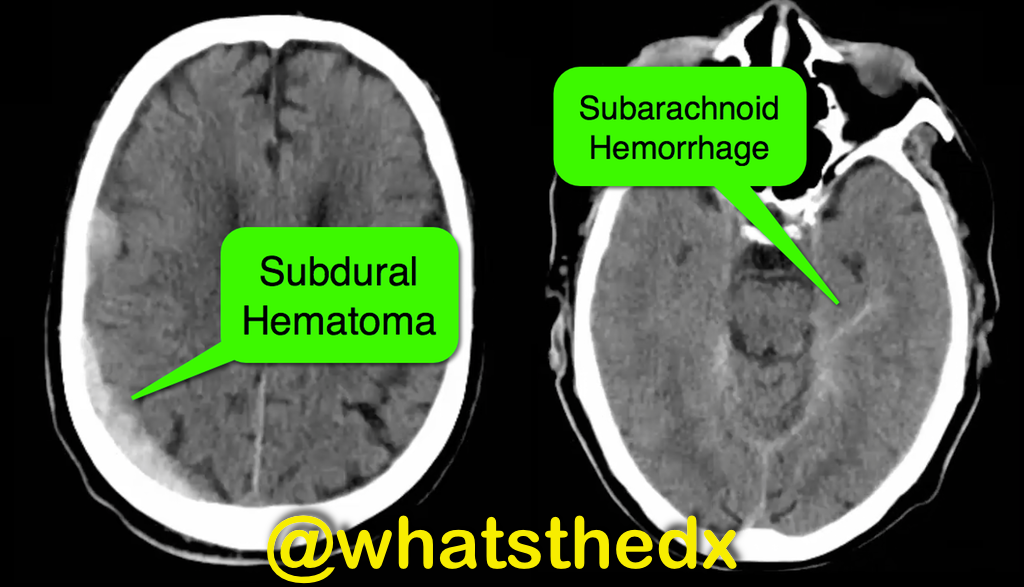
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: Patent Foramen Ovale (PubMed Search)
Posted: 11/23/2014 by Semhar Tewelde, MD
(Updated: 2/8/2026)
Click here to contact Semhar Tewelde, MD
Patent Foramen Ovale: To Close or Not to Close
- Patent foramen ovale (PFO) is associated with a 3-fold increased risk for recurrent stroke, yet current guidelines only recommends “consideration” of PFO closure after a second cryptogenic stroke.
- Studies have demonstrated reductions in recurrent neurologic events with transcatheter PFO closure compared with medical therapy alone.
- Until recently the cost-effectiveness of PFO closure has not been described.
- Although PFO closure was found to be immediately more costly per patient closure, it reached cost-effectiveness at ~2.5 years of follow-up.
- Closure of PFO is both beneficial in terms of risk-benefit and cost-effectiveness strategy, especially as cryptogenic stroke typically affects the young.
Pickett C, Villines T, Ferguson M, et al. Cost Effectiveness of Percutaneous Closure Versus Medical Therapy for Cryptogenic Stroke in Patients With a Patent Foramen Ovale. The American Journal of Cardiology. Volume 114, Issue 10, Pages 1584-89 (15 November 2014)
Category: Orthopedics
Keywords: knee dislocation, vascular and nerve injury (PubMed Search)
Posted: 11/22/2014 by Brian Corwell, MD
(Updated: 12/26/2014)
Click here to contact Brian Corwell, MD
Knee dislocation 2
Most commonly occur after MVCs but also seen after falls, industrial accidents and sports related trauma.
Up to 50% of knee dislocations will have spontaneously reduced by time of presentation to the ED.
Strongly consider a spontaneously reduced knee dislocation in those with a significant mechanism of injury in the setting of multidirectional instability (3 or more ligaments torn).
A thorough neurovascular examination is a must due to the risk of vascular (34%)(5-79%) and nerve (23%)(16-40%) injuries. There is a must higher incidence of these injuries in high force trauma such as from a MVC. The popliteal artery and common peroneal nerve are at the greatest risk
Though the absence of distal pulses suggests vascular injury, the presence of pulses cannot be used as evidence of the lack of a vascular injury.
After reduction, the knee should be immobilized in 15-20° of flexion in a knee immobilizer.
Category: Pediatrics
Keywords: Medications, overdose, pediatric, over the counter (PubMed Search)
Posted: 11/21/2014 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Category: International EM
Keywords: Bioterrorism, infectious diseases (PubMed Search)
Posted: 11/20/2014 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Background: As noted in a previous pearl (November 5, 2014), the Centers for Disease Control and Prevention (CDC) classifies potential bioterrorism agents into three categories. Category B & C agents are of less priority than the previously discussed Category A agents.
Category B: Second highest priority agents. These agents:
These Agents/Diseases include:
•Brucellosis (Brucella species)
•Epsilon toxin of Clostridium perfringens
•Food safety threats (e.g., Salmonella species, Escherichia coli O157:H7, Shigella)
•Glanders (Burkholderia mallei)
•Melioidosis (Burkholderia pseudomallei)
•Psittacosis (Chlamydia psittaci)
•Q fever (Coxiella burnetii)
•Ricin toxin from Ricinus communis (castor beans)
•Staphylococcal enterotoxin B
•Typhus fever (Rickettsia prowazekii)
•Viral encephalitis (alphaviruses [e.g., Venezuelan equine encephalitis, eastern equine encephalitis, western equine encephalitis])
•Water safety threats (e.g., Vibrio cholerae, Cryptosporidium parvum)
Category C agents: Third highest priority agents. These include emerging pathogens, such as hantavirus and Nipah virus, which could be potentially engineered for mass dissemination in the future.
Bottom Line: While in general of less concern, bioterrorism agents in Category B & C remain of significant risk. Many of these diseases still occur in various parts of the globe including the United States.
Category: Toxicology
Keywords: opioids, toxicology (PubMed Search)
Posted: 11/20/2014 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
The pattern of prescription drug abuse continues to center around semisynthetic opioids like oxycodone and hydrocodone. Federal regulations have now raised hydrocodone to a schedule II drug like oxycodone. Despite efforts, the slope for natural and semisynthetic opioids remains steep. The ED measures of education, limit prescriptions for acute pain, minimize number of days/pills prescribed and utlize the prescription drug monitoring program are some basics that can assist you in better prescribing habits.
NCHS Data Brief, Number 166, September 2014
Category: Critical Care
Keywords: cap, pneumonia, (PubMed Search)
Posted: 11/18/2014 by Feras Khan, MD
(Updated: 2/8/2026)
Click here to contact Feras Khan, MD
Tips for the inpatient management of community acquired pneumonia
Daniel M. Musher, M.D., and Anna R. Thorner, M.D.
N Engl J Med 2014; 371:1619-1628October 23, 2014DOI: 10.1056/NEJMra1312885
Category: Visual Diagnosis
Posted: 11/17/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Patient presents with dyspnea & hypoxemia (pulse oximeter is 80%). The "stat" CXR is delayed, but ultrasound is not. What's the diagnosis and what are some differential diagnoses?
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Orthopedics
Keywords: felon, management (PubMed Search)
Posted: 11/15/2014 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Management of Felons
For good photos of the incision technique please visit the reference article listed.
Category: Toxicology
Keywords: Bactrim, trimethoprim-sulfamethoxazole, ACE-inhibitor, angiotensin receptor blocker, ARB (PubMed Search)
Posted: 11/5/2014 by Bryan Hayes, PharmD
(Updated: 11/13/2014)
Click here to contact Bryan Hayes, PharmD
A new population-based case-control study in older adults has linked the administration of trimethoprim-sulfamethoxazole (Bactrim, TMP-SMX) to increased risk of sudden death in patients also receiving angiotensin converting enzyme inhibitors (ACE-I) or angiotensin receptor blockers (ARB). [1]
Hyperkalemia is the suspected cause. [2] Compared to amoxicillin, TMP-SMX was associated with an increased risk of sudden death (adjusted odds ratio 1.38, 95% confidence interval 1.09 to 1.76) within 7 days of exposure to the antibiotic.
Practice Change
In older patients receiving ACE-Is or ARBs, TMP-SMX is associated with an increased risk of sudden death. When appropriate, alternative antibiotics should be considered.
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
