Category: Orthopedics
Keywords: x-ray, child abuse, fracture dating (PubMed Search)
Posted: 3/14/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Imaging plays an important role in the evaluation of child abuse.
It aids in the identification, evaluation and in treatment.
Additionally, it is often the only objective evidence of abuse available to the courts.
It is often discovered through two means.
1) Injuries/fractures that are inconsistent with the alleged mechanism of injury.
2) Pathognomonic fracture patterns are found on routine radiographs
The ED physician should not attempt to precisely "date" the injury.
That said, soft tissue swelling resolves in 2-5 days. The periosteum becomes radiodense in 7 to 10 days. In subtle fractures this may be the only radiographic finding. If there is no evidence of bone healing (periosteal reaction), the fracture is less than 2 weeks old. Callus formation and resorption of the bone along the fracture line begins at 10 to 14 days. The callus is visible for up to 3 months. Bone remodeling continues for up to one year.
Emergency Radiology, chapter 22, "pediatric considerations" by Ken Butler and Martin Pusic.
Category: Pediatrics
Posted: 3/13/2015 by Rose Chasm, MD
Click here to contact Rose Chasm, MD
Debrovsky AS, Kempinska A, Bank I, Mok E. Accuracy of Ultrasonography for Determining Successful Realignment of Pediatric Forearm Fractures. Annals of Emergency Medicine. Vol 65;Number 3. March 2015.
Category: Toxicology
Keywords: naloxone, opioid overdose (PubMed Search)
Posted: 3/10/2015 by Bryan Hayes, PharmD
(Updated: 3/14/2015)
Click here to contact Bryan Hayes, PharmD
In the midst of an unprecedented opioid epidemic, there have been considerable efforts to expand access to naloxone (Doyon S, et al. J Med Toxicol 2014;10:431-4). If the situation arises when you need to write a prescription for it, here's how:
Option 1: Naloxone vial and needle traditional IM/SQ using 0.4 mg/mL injection vial and needles (least expensive $40, FDA approved)
Naloxone 0.4 mg/mL single dose vial and 3 cc, 23 g, 1 inch syringes, #2 each
SIG: Inject 1 mL intramuscularly upon signs of opioid overdose. May repeat X 1. Call 911.
Option 2: IMS/Amphastar 2 mg/2 mL prefilled syringe and mucosal atomization device ($95/kit, products FDA approved but intranasal administration is off-label)
Naloxone 2 mg/2 mL prefilled syringe and intranasal atomizer device, #2 each
SIG: Spray one-half of syringe (1 mL) into each nostril upon signs of opioid overdose. May repeat X 1. Call 911.
Option 3: Evzio Autoinjector ($200-700 per Rx though many insurances cover it and the company has vouchers available, FDA approved in 2014, evzio.com/hcp)
Evzio 0.4 mg, #1 two-pack
SIG: Use as directed upon signs of opioid overdose. May repeat X 1. Call 911.
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Neurology
Keywords: back pain, spinal cord (PubMed Search)
Posted: 3/12/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Cauda Equina Syndrome is a true neurologic and surgical emergency. Unfortunately, no constellation of symptoms or exam findings is 100% sensitive. In fact, no single symptoms predicts the radiographic finding of cauda equina syndrome with an accuracy greater than 65%.
The most common symptoms are sciatica (96%), micturition dysfunction (89%), saddle anesthesia or hypoethesia (81%) and defecation dysfunction (47%).
Tarulli AW. Disorders of the Cauda Equina. Continuum Lifelong Learning Neurol 2015;21(1):146 158
Category: Critical Care
Keywords: massive transfusion, trauma, bleeding, critical care, severe trauma, PROPPR (PubMed Search)
Posted: 3/10/2015 by Feras Khan, MD
Click here to contact Feras Khan, MD
Transfusion in Major Trauma: The PROPPR Trial
What should we be transfusing in major trauma?
The Trial
Results
Conclusions
How does this affect my practice?
A 1:1:1 transfusion practice is safe and can decrease mortality from hemorrhage in major trauma
Other points: control bleeding, permissive hypotension, avoid crystalloids, use TEG to guide therapy (TXA etc)
Category: Visual Diagnosis
Posted: 3/9/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
35 year-old female presents with acute leg pain and swelling. What's the diagnosis?

Phlegmasia cerulea dolens; there was extensive clot found in the left external iliac, common femoral, superficial femoral, and popliteal veins.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 3/8/2015 by Semhar Tewelde, MD
(Updated: 2/8/2026)
Click here to contact Semhar Tewelde, MD
Afib Clinical Decision Aid: AFFORD
- Atrial fibrillation (AF) affects ~34 million people worldwide; the hospital admission rates vary with frequencies of 81%, 62%, and 24% in the US, Australia, and Canada respectively.
- Lack of a reproducible and accurate risk stratification/decision aid likely contributes to variability in ED disposition.
- AFFORD (Atrial fibrillation and flutter outcome risk determination) was the 1st clinical decision aid (contains 17 variables) to predict 30-day adverse events in a prospective ED patient cohort with acute symptomatic AF.
- Vanderbilt University Medical Center's ED (2010-2013) derived and internal validated an ED based clinical decision aid for prediction of MACE within 30 days utilizing the AFFORD decision aid in hemodynamically stable patients whose AF reverted to sinus rhythm, either spontaneously or after cardioversion (pharmacologic or electrical), and those who are adequately rate controlled and candidates for outpatient management.
- Incorporating AFFORD with a shared decision model into ED practice may help identify patients at low risk and potentially reduce rate of hospitalizations.
Barrett TW, Storrow AB, et al. The AFFORD Clinical Decision Aid to Identify Emergency Department Patients With Atrial Fibrillation at Low Risk for 30-Day Adverse Events. The American Journal of Cardiology Volume 115, Issue 6, Pages 763-770 (15 March 2015).
Barrett TW, Storrow AB, et al. Atrial fibrillation and flutter outcomes and risk determination (AFFORD): design and rationale. J Cardiol, 58 (2011), pp. 124–130.
Category: Pharmacology & Therapeutics
Keywords: ketamine, pain, opioid (PubMed Search)
Posted: 2/24/2015 by Bryan Hayes, PharmD
(Updated: 3/7/2015)
Click here to contact Bryan Hayes, PharmD
Emergency Departments are increasingly searching for alternatives to opioids for acute pain management.
An urban trauma center in California retrospectively evaluated their use of low-dose ketamine for acute pain over a two-year period. [1]
Application to Clinical Practice
There was no comparison group and there was no mention of what other pain medicines were given. Adverse events are often under-reported in retrospective studies. This study seems to demonstrate that low-dose ketamine administration for acute pain management in the ED is feasible with a low rate of adverse effects.
It's worth noting that a new review of 4 randomized controlled trials evaluating subdissociative-dose ketamine found no convincing evidence to support or refute its use in the ED. The 4 included trials had methodologic limitations. [2]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: International EM
Keywords: international health, noncommunicable diseases, chronic diseases, World Health Organization (PubMed Search)
Posted: 3/4/2015 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 3/18/2015)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Background: While much of international health focuses on communicable diseases, it is clear that noncommunicable diseases (NCDs), such as cardiovascular diseases, cancer and diabetes, causes substantial morbidity and mortality.
Epidemiology:
Bottom line: As in developed countries, risk factors for NCDs deaths include physical in activity, tobacco use, unhealthy diabetes, harmful use of alcohol.
http://www.who.int/mediacentre/factsheets/fs355/en/
Category: Critical Care
Posted: 3/3/2015 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
High-Flow Nasal Cannula for Apneic Oxygenation
Miguel-Montanes R, et al. Use of high-flow nasal cannula oxygen therapy to prevent desaturation during tracheal intubation of intensive care patients with mild-to-moderate hypoxemia. Crit Care Med 2015;43:574-83.
Category: Visual Diagnosis
Posted: 3/2/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
6 day-old child is brought in by parents with 1 day of reduced oral intake and 4 hours of rapid breathing. The child has no fever and no significant birth history. The child is tachycardic, hypotensive, and hypoxic. What’s the diagnosis?
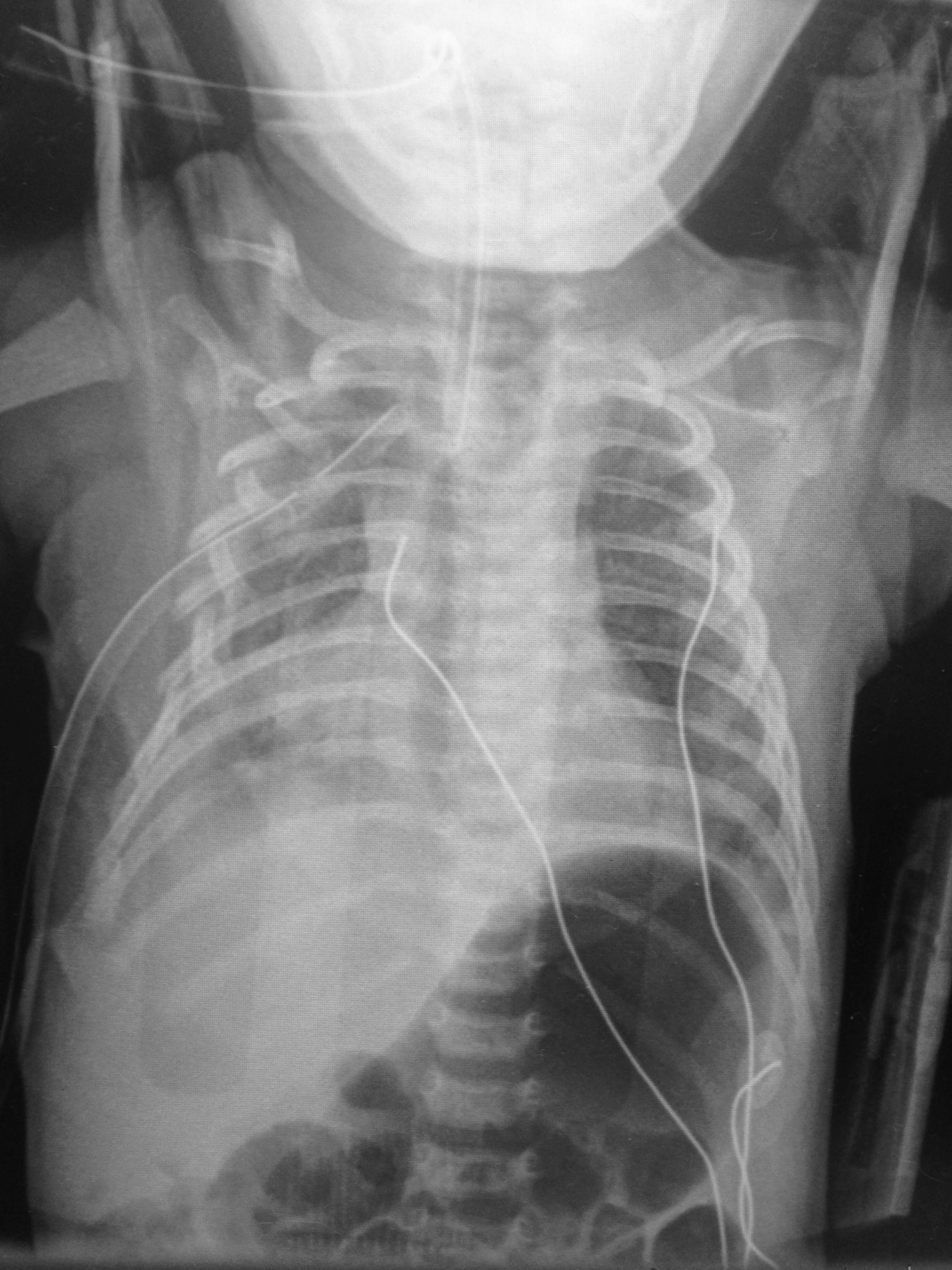
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 3/1/2015 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Safety Risk? Digoxin in Atrial Fibrillation
- Digoxin is commonly utilize for atrial fibrillation/flutter with rapid ventricular response, though beta blockers and/or calcium channel blockers are a better 1st line therapy given digoxin’s narrow therapeutic index and lack of mortality benefit.
- Digoxin in the acute setting is often favored given its ability to reduce the heart rate while maintaining or slightly augmenting blood pressure.
- 2014 AHA/ACC guidelines recommend digoxin, specifically for rate control in patients with heart failure and/or reduced ejection fraction.
- There have been 2 post hoc studies from the AFFIRM trial which showed conflicting results w/regards to digoxin and risk of mortality.
1. Increased risk of mortality associated w/digoxin (on-treatment analytic strategy)
2. No association w/mortality (intent-to-treat analytic strategy)
- A recent retrospective cohort examination of newly diagnosed afib patients without heart failure & no prior use of digoxin; digoxin was independently associated with a 71% higher risk of death & a 63% higher risk of hospitalization.
- Consistent and substantial increase in mortality and hospitalization risk was seen using both on-treatment and intent-to-treat analytic methods.
- Given other available rate control options, digoxin should be used with caution.
Freeman J, Reynolds K, et al. Digoxin and Risk of Death in Adults With Atrial Fibrillation The ATRIA-CVRN Study. Circ Arrhythm Electrophysiol. 2015;8:49-58.
Category: Orthopedics
Keywords: Foot pain, stress fractures (PubMed Search)
Posted: 2/28/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Sesamoid Injuries
The first MTP joint contains the 2 sesamoid bones. They play a significant part in the proper functioning of the great toe. 30% of individuals have a bipartite medial or lateral sesamoid.
http://www.coreconcepts.com.sg/mcr/wp-content/uploads/2008/05/sesamoid_foot.jpg
Injury can occur from trauma, stress fracture or sprain of the sesamoid articulation or of the sesamoid metatarsal articulation. Overuse injuries tend to occur in sports with a great deal of forefoot loading (basketball/tennis).
SXs: Pain with weight bearing, pain with movement of first MTP, ambulation on lateral part of foot.
PE: Tenderness and swelling over medial or lateral sesamoid. Resisted plantar flexion (flexor hallucis) reveals pain and weakness.
Imaging: plain film with sesamoid view to assess for a sesamoid fracture. Stress fractures may take 3-4 weeks to show on plain film.
http://www.agoodgroup.com/running/Fracture002.jpg
Treatment for fractures and suspected stress fractures involve 4 to 6 weeks of non weight bearing.
Category: Orthopedics
Keywords: Orthopaedic, Chest Pain (PubMed Search)
Posted: 2/28/2015 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Orthopedic Causes of Chest Pain
The first thing that pops into everybody’s mind when they hear a patient state they have chest pain radiating to the left arm is Acute Coronary Syndrome and specifically a Myocardial Infarction. However, there are a lot of orthopedic causes of chest pain that can also radiate to the left arm. It is estimate that up to 20% of patients with pectoral symptoms have an underlying orthopedic problem.
Some of them are:
Some other less common causes are
So instead of just ordering some troponin and admitting to medicine, consider that the cause can be orthopedic in origin.
Fromm B. Often an orthopedic problem can manifest as chest pain. Cervical vertebrae syndrome mimics myocardial infarct. MMW Fortschr Med 2002 Apr 25; 144(17):31-3.
http://www.ncbi.nlm.nih.gov/pubmed/12048845
Category: Toxicology
Keywords: cyanide, carbon monoxide, methanol, hypoglycemia (PubMed Search)
Posted: 2/26/2015 by Fermin Barrueto
Click here to contact Fermin Barrueto
Patient has the following Head CT, what is your differential diagnosis? There are only a few characteristic toxins that can cause this type of finding on CT.
Bilateral Basal Ganglia Infarcts think:
Cyanide
Carbon Monoxide
Hypoglycemia
Methanol
Hypoxia and Uncouplers of Oxidative Phsophorylation can cause this
Category: Neurology
Keywords: cardiac arrest, subarachnoid hemorrhage, intracerebral hemorrhage, ischemic stroke, seizure (PubMed Search)
Posted: 2/25/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Neurologic causes of cardiac arrest have not been well described. Two recent retrospective studies looked at the epidemiology and clinical features of these patients.
Hubner P. et al.
Arnaout M. et al.
Neurologic causes of cardiac arrest are uncommon presentations that may be difficult to distinguish from cardiac etiology of cardiac arrest. If history and clinical presentation suggests a neurologic cause, obtain a non-contrast head CT for evaluation.
Hubner P, Meron G, Kurkciyan I, et al. Neurologic causes of cardiac arrest and outcomes. J Emerg Med. 2014;47(6):660-667.
Arnaout M, Mongardon N, Deye N, et al. Out-of-Hospital Cardiac Arrest from Brain Cause: Epidemiology, Clinical features, and Outcome in a Multicenter Cohort. Crit Care Med. 2015;43(2):453-460.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: CVP (PubMed Search)
Posted: 2/24/2015 by John Greenwood, MD
Click here to contact John Greenwood, MD
The Role of the CVP in a Post- “7 Mares” Era
The role for using central venous pressure (CVP) as a measure of volume responsiveness has largely fallen out of favor over the years.1 There are certainly better indices for fluid responsiveness, but don’t be fooled – the CVP isn’t a one trick pony. In fact, a high or rapidly rising CVP should raise a significant concern for impending cardiovascular collapse.
Consider the following differential diagnosis in the patient with an abnormally high or rising CVP ( >10 cm H2O).
Bottom Line: In a time where the utility of the CVP has been largely dismissed, remember that an abnormal CVP offers great deal of information beyond a simple measure of volume status.
References
Follow me on Twitter: @JohnGreenwoodMD
Category: Visual Diagnosis
Posted: 2/23/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
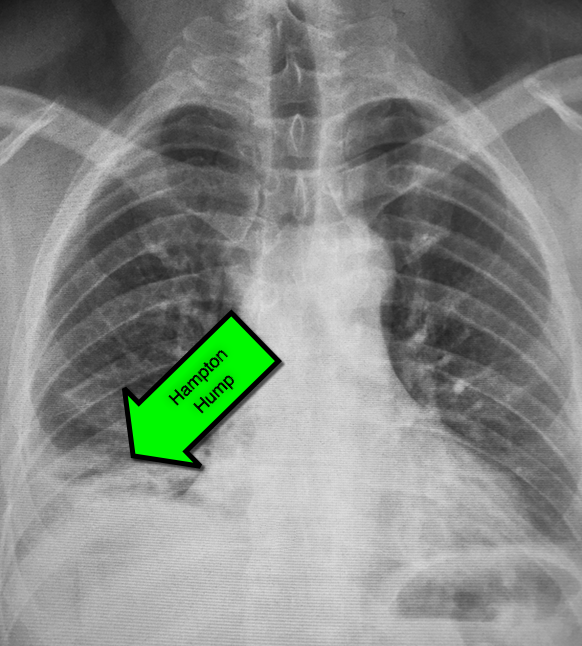
45 year-old male complains of pleuritic chest pain following a "long" flight. What's the diagnosis and what's this sign called?
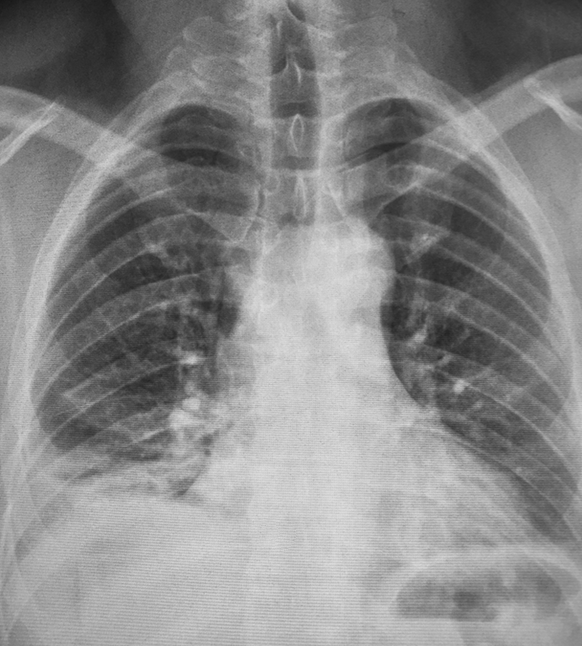
First described by Dr. Aubrey Hampton in 1940, hampton hump is a peripheral (pleural) based opacification found on chest X-ray; it occurs secondary to infarction of the lung
Although commonly associated pulmonary embolism it may occur secondary to other causes of lung infarction
Here are some other infrequent, but not rare signs, of pulmonary embolism on chest X-ray:
Category: Pediatrics
Keywords: Stroke, congenital heart disease (PubMed Search)
Posted: 2/20/2015 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
This study is a case control study of the association of congenital heart disease (CHD) and stroke using a base population of 2.5 million Kaiser patients in California. 412 cases of stroke were identified and compared to 1236 controls. Of these stroke patients, 11/216 ischemic strokes and 4/196 hemorrhagic strokes were attributed to CHD (both cyanotic and acyanotic lesions). CHD was found in 7/1236 controls.
Children with CHD and history of cardiac surgery had the strongest risk of stroke (31 fold over the control group). Many of these children had strokes years after their surgery. Children with CHD who did not have cardiac surgery had a trend towards elevated stroke risk, but the confidence intervals included the null. More children without CHD history presented with headache.
Bottom line: Stroke risk (both hemorrhagic and ischemic) extend past the immediate postoperative period in patients with CHD.
Fox CK, Sidney S and Fullerton HJ. Community-Based Case Control Study of Childhood Stroke Risk Associated With Congenital Heart Disease. Stoke 2015; 46:336-340.
Category: International EM
Keywords: Measles, outbreak, complications (PubMed Search)
Posted: 2/19/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
The Centers for Disease Control continues to report increased numbers of measles patients in the US. From January 1 to February 13, 2015 there have been 141 cases. It has spread to 17 states and the District of Columbia, with 80% linked to the multistate outbreak from Disneyland.
Measles is not a benign disease!
Per the World Health Organization, there were 146,700 measles deaths globally in 2013. Most of these deaths occur in lower- and middle-income countries,
Even in the US, measles can cause serious complications and death. Complications from measles can be seen in any age group, but particularly in children <5 years of age and in adults >20 years of age.
Measles Complications:
Common:
Severe:
Long-term:
Bottom Line:
Per Dr. Anne Schuchat of the CDC: “This is not a problem with the measles vaccine not working. This is a problem of the measles vaccine not being used.”
http://www.who.int/mediacentre/factsheets/fs286/en/
http://www.cdc.gov/measles/about/complications.html
