Category: Pediatrics
Keywords: intraosseous access, pediatrics (PubMed Search)
Posted: 1/3/2015 by Ashley Strobel, MD
(Updated: 2/8/2026)
Click here to contact Ashley Strobel, MD
Are you comfortable with Intraosseous Catheter Placement in Children during a code? A pediatric code or child in distress is also distressing to care providers. Your staff may not feel comfortable with IO access in children. Read on to be more comfortable with your options as IO access in children can be difficult, especially the chubby toddlers. The basics for a patient in distress are "IV, O2, Monitor". Access is vital to giving resuscitation medications.
Indications for IO access: Any child in whom IV access cannot readily be obtained, but is necessary.
All IOs are 15G for infusion equal to central vascular access.
Different colors indicate different sizes:
Preferred sites:
Kids-do NOT use the sternum or distal radius
The reference from NEJM has videos to review placement and different tools (manual, EZ IO, and autoinjector).
Category: Pediatrics
Keywords: appendicitis, ultrasound, bedside (PubMed Search)
Posted: 11/8/2014 by Ashley Strobel, MD
Click here to contact Ashley Strobel, MD
Emergency Physician Bedside Ultrasound for Appendicitis
Why?
To reduce length of stay, improve patient care, and reduce radiation exposure in young patients.
How?
Start with pain medication so you get a better study. (Consider intranasal fentanyl for quicker pain relief and diagnostics in pediatrics.) Study results are also improved with a slim body habitus.
Place the patient supine
Use a high-frequency linear array transducer
Start at the point of maximal tenderness in the RLQ
Transverse and longitudinal planes "graded compression" to displace overlying bowel gas which usually has peristalsis (See Sivitz, et al article for images of "graded compression")
Appendix is usually anterior to the psoas muscle and iliac vein and artery as landmarks
Measure from outer wall to outer wall at the most inflamed portion of the appendix (usually distal end)
Example:
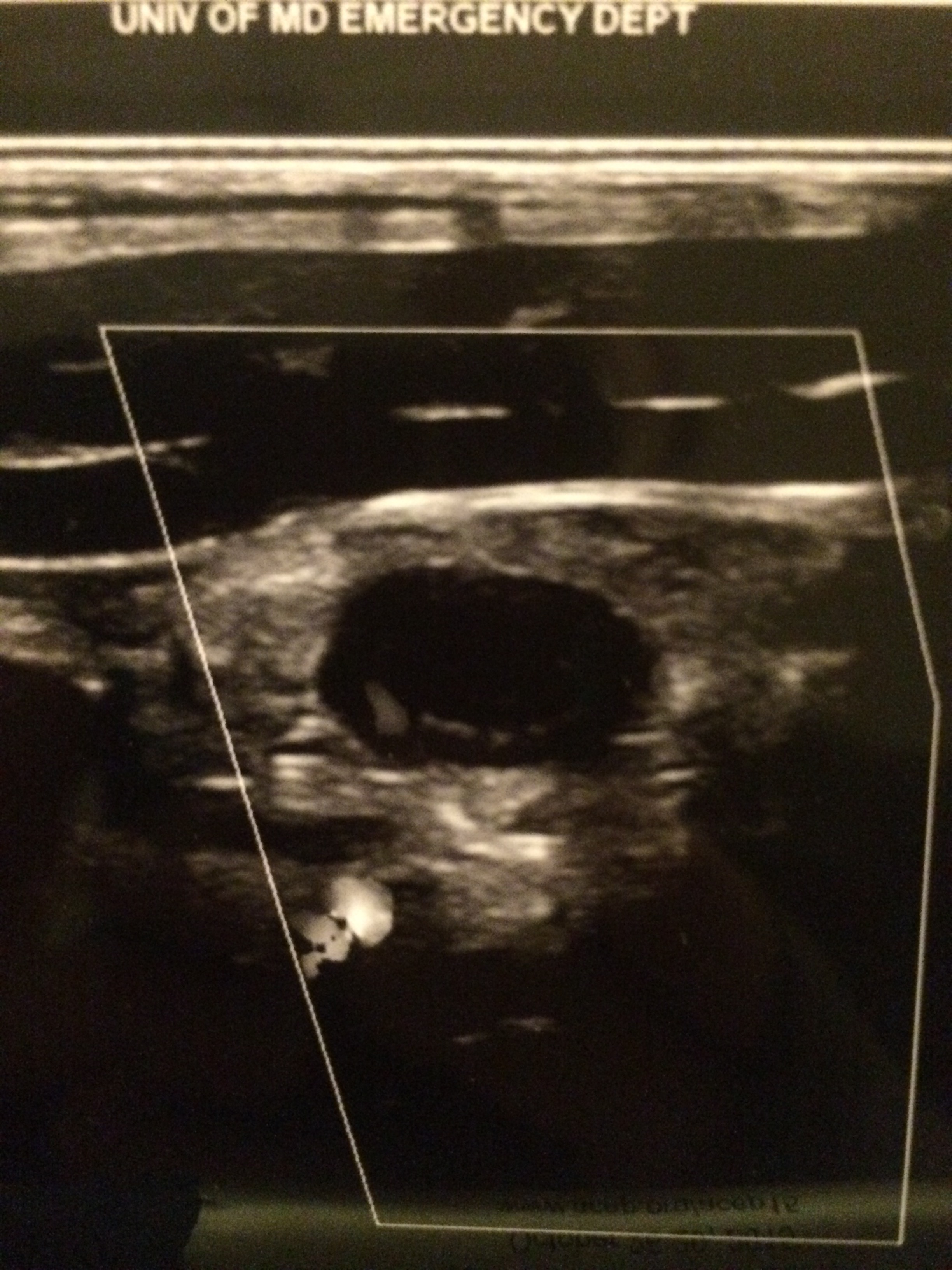
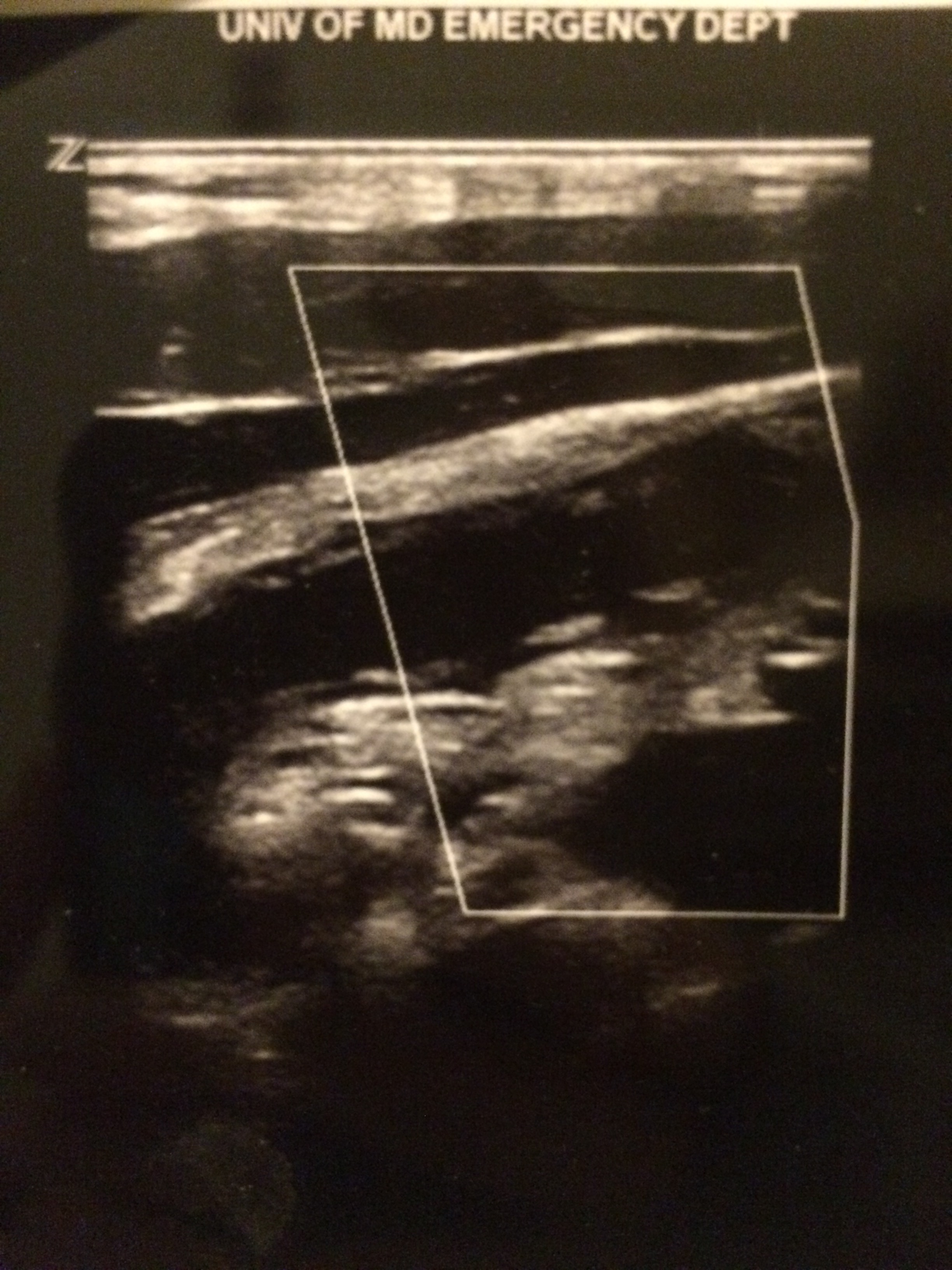
Positive study:
A non-compressible, blind-ending tubular structure in the longitudinal axis >6 mm without peristalsis (see second image above with 8.3 mm diameter measurement)
A target sign in the transverse view (see first image above)
Additional suggestive findings: appendiceal wall hyperemia with color Doppler, appendicoliths hyperechoic (white) foci with an anechoic (black) shadow, periappendiceal inflammation or free fluid
Negative study:
Non-visualization of the appendix with adequate graded compression exam in the absence of free fluid or inflammation.
Limitations for visualization and possible false negative result:
Retrocecal appendix and perforated appendix are difficult to visualize with US.
Pitfalls:
US has good specificity (93% in Sivitz et al article), but limited sensitivity (85% in Sivitz et al article), so trust your clinical judgement. You may need a MRI (pregnant/pediatrics) or CT as they have improved, but not perfect sensitivity.
Valesky, et al. Focus On: Ultrasound for Appendicitis. ACEP Now. June 2012.
Sivitz AB, Cohen SG, Tejani C. Evaluation of Acute Appendicitis by Pediatric Emergency Physician Sonography. Annals of Emerg Med. Oct 2014; 64: 358-363.
Category: Pediatrics
Keywords: Macklin Phenomenon, asthma, pneumomediastinum (PubMed Search)
Posted: 9/22/2014 by Ashley Strobel, MD
Click here to contact Ashley Strobel, MD
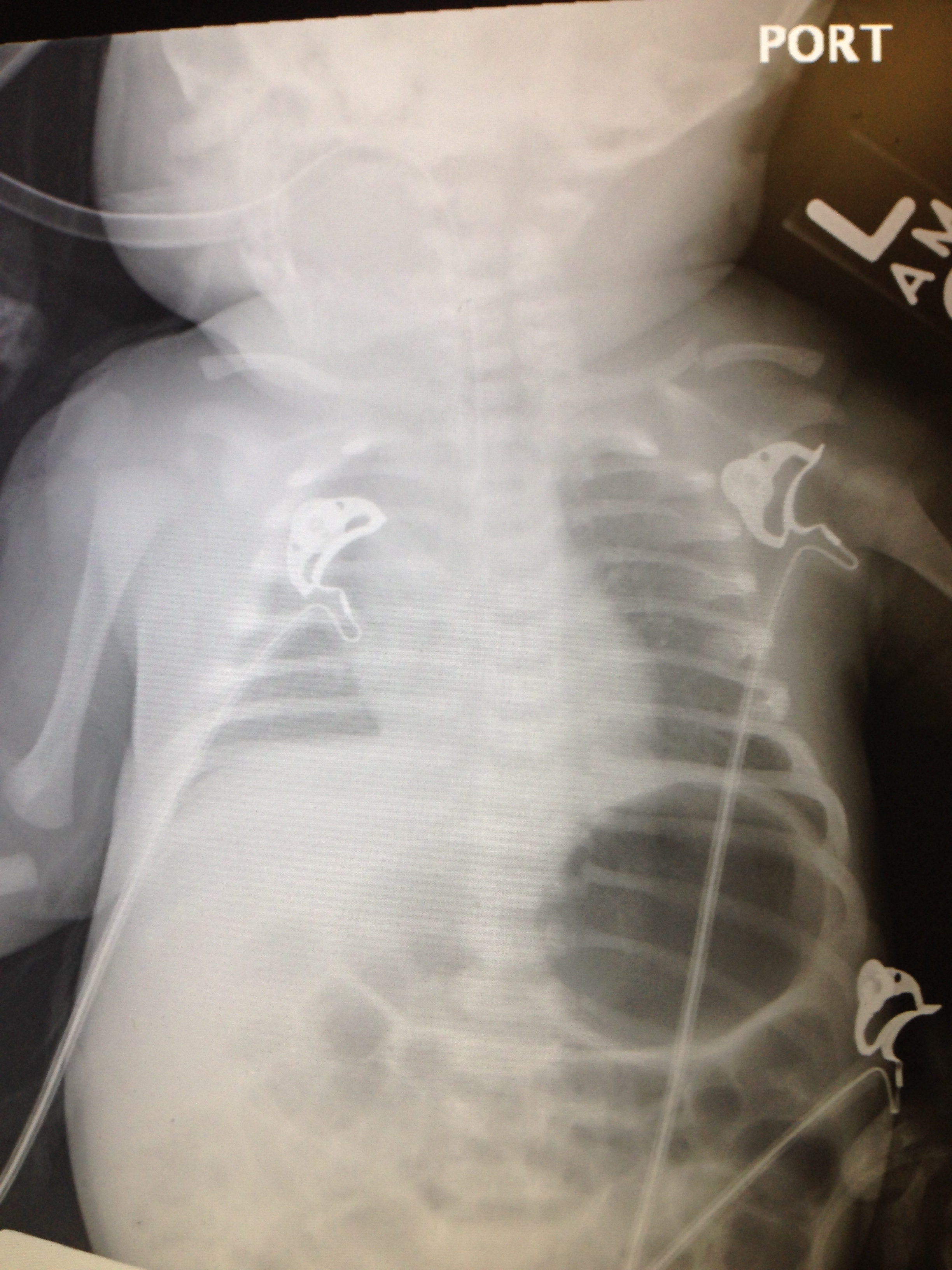
16 yo M with pleuritic right upper chest pain that started today. He is suffering from an asthma exacerbation currently in the setting of URI with cough. He is afebrile, tachycardic to 140-150s, respiratory rate 20, and sats 98% on room air. ECG was performed which incidentally diagnosed this patient WPW and he went for ablation as an outpatient. His chest x-ray showed:
Besides a bad day, what do we call this chest x-ray finding?
Macklin Phenomenon
-asthma exacerbation rupture of the alveoli causing pneumomediastinum
-typically a young man
-most common chief complaint is chest pain
Physical Exam: Hamman’s sign may be present (crackle with heartbeat) or subcutaneous emphysema
Etiology: Esophagus, lungs, or bronchial tree
Rupture of alveoli: asthma exacerbation (bronchial hyper-reactivity/constriction), barotrauma, valsalva maneuvers (lifting, childbirth), deep respiratory maneuvers/Valsalva (strenuous exercise or FVC breathing), drug use (crack cocaine causing bronchial constriction, marijuana), vomiting, blunt thoracic/abdominal trauma, scuba diving with rapid ascent
Aerodigestive tract injuries: bronchoscopy tracheobronchial injuries, laryngeal fx, bronchial fx, tracheal neoplasm, esophageal injuries (Boerhaave syndrome, paripartum, asthma exacerbation, esophageal neoplasm)
Extension from neck: head/neck sx, RPA/PTA, dental abscess/extractions
Extension from RP/chest wall: rupture RP hollow viscus
Management:
-self -limited
-treat underlying condition
-swallow study for all cases following emesis to rule out Boerhaave’s syndrome
-no repeat CXR, advance diet as tolerated, 23 hour observation
-Al-Mufarrei, et al suggest without trauma, pleural effusion, hemodynamic instability, pneumoperitoneum, or severe vomiting, the finding of spontaneous pneumomediastinum (with or without Meckler’s triad of esophageal rupture: vomiting, lower chest pain, and cervical subcutaneous emphysema after overindulgence) usually leads to unnecessary radiologic investigations, dietary restriction, and antibiotic administration
-surgery for decompression
Gray JM and Hanson GC. Mediastinal emphysema: aetiology, diagnosis, and treatment. Thorax. 1966; 21: 325-332.
Al-Mufarrej F, Badar J, Gharagozloo F, Tempesta B, Strother E, Margolis M. Spontaneous pneumomediastinum: diagnostic and therapeutic intervnetions. Journal of Cardiothoracic Surgery. November 2008; 3: 59.
Category: Pediatrics
Keywords: non-accidental trauma, clavicle fracture, neonate, pediatrics, abuse (PubMed Search)
Posted: 10/4/2014 by Ashley Strobel, MD
Click here to contact Ashley Strobel, MD
Q: What is wrong with this baby? And what Dx should you entertain?
Previously healthy 7d old presents after difficulty feeding, one episode of vomiting and now with intermittent apneic episodes.
Non-accidental trauma (NAT) is most prevalent in children 0-3 months of age.
Radiographically classic metaphyseal lesions, rib fractures, and multiple fractures in various stages of healing are most commonly described in child abuse cases.
How do we know this is not just birth trauma from a shoulder dystocia, LGA (large for gestational age), or difficult vaginal delivery?
The key is dating the fracture. In this recent publication by Walters MM et al, prior to 8 days of life, 100% of radiographs did NOT have callus present. Callus formation is highly unlikely in fractures less than 9 days old, and typically appears by 15 days old. Callus thickness decreases inversely with fracture age. Additionally, subperiosteal new bone formation is highly unlikely in fractures less than 7 days old and typically appears by 10 days old. Subperiosteal new bone formation increases in thickness inversely with fracture age. Therefore, a clavicle fracture in a 7 day old without subperiosteal new bone formation or callus is unlikely from birth trauma and NAT should be considered.
How can you tell if subperiosteal new bone formation is present?
Subperiosteal new bone formation appears as a hazy cortical margin or a thin layer of bone separated from the original cortex by a discrete lucent interval. The new bone increases in thickness with time and may evolve to appear as a lamellated or multilayered linear hyperdensity parallel to the cortex of the bone. See referenced article for great picture examples.
NAT Work-up:
CT head without contrast if ≤2 yo
Skeletal Survey if ≤ 2 yo
AST, ALT, amylase, lipase, CBC, Manual Differential, BMP, UA, Urine Toxicology
Consults: Ophthalmology, Social Work, Child Protection
OH BUTT TUBE (Dark Green Top Sodium Heparin) for further inpatient team studies
ALTE Work-up:
Guided by history, however consider the following:
Full sepsis evaluation for neonate <30 days
ECG
Possible reflux or seizure evaluation
Consider NAT or Pertussis/RSV with cyanosis
It is controversial to send these infants home from the ED. Typically they benefit from 24 hours of monitoring, but this is a pearl for another day.
See article for further pictures of subperiosteal new bone formation:
Walters MM, Forbes PW, Buonomo C, and Kleinman PK. Healing Patterns of Clavicular Birth Injuries as a guide to fracture dating in cases of possible infant abuse. Pediatric Radiology. October 2014; 44: 1224-1229.
@AstrobelMD
