Category: Orthopedics
Keywords: Davos, Shoulder, Reduction (PubMed Search)
Posted: 10/15/2016 by Michael Bond, MD
Click here to contact Michael Bond, MD
Davos Shoulder Reduction Technique
Take Home Points
Interested, well find out more by watching this video by Larry Mellick https://www.youtube.com/watch?v=u2MsnjVNoPM or clicking the link below.
The Davos technique is a novel technique that requires no exertion on the part of the provider and can be done without sedation
Do the technique by:
The original article can be found here http://www.jem-journal.com/article/S0736-4679(16)00030-5/abstract
Category: Toxicology
Keywords: CCB poisoning (PubMed Search)
Posted: 10/13/2016 by Hong Kim, MD
Click here to contact Hong Kim, MD
US, Canadian and European critical care and toxicology societies recently published a consensus recommendation is the management of CCB poisoning.
Bottom line:
1. First line therapy remains unchanged: IV calcium, atropin, high-dose insulin (HIE) therapy, vasopressor support (norepinephrine and/or epinephrine).
2. Refractory to first line therapy: increase HIE, lipid-emulsion, transvenous pacemaker
3. Refractory shock, periarrest or cardiac arrest: Above (#1 & #2) plus ECMO if available.
Overall, there has not been a signficant changes to the current management of CCB poisoning. However, there is a nice flow chart of the algorithm/recommendation in the article. The authors note that the "level of evidenc was very low" for all intervention.
Briefly:
A. asymptomatic patients
B. First line therapy
C. Refractory to first line therapy
D. Refratory shock or periarrest
E. Cardiac arrest
St-Onge, M et al. Experts consensus recommendations for the management of calcium channel blocker poisoning in adults. Crit Care Med 2016 (http://journals.lww.com/ccmjournal/Abstract/publishahead/Experts_Consensus_Recommendations_for_the.96757.aspx)
Category: Neurology
Keywords: Brain Trauma Foundation, BTF, guideline, traumatic brain injury, TBI (PubMed Search)
Posted: 10/12/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Updated Guidelines for Traumatic Brain Injury
The Brain Trauma Foundation (BTF) Guidelines for the Management of Severe Traumatic Brian Injury (TBI) was recently updated and published in September 2016.
Updated recommendations include:
For the executive summary and complete guidelines, go to https://braintrauma.org/guidelines/guidelines-for-the-management-of-severe-tbi-4th-ed#/
Category: Critical Care
Posted: 10/11/2016 by Mike Winters, MBA, MD
(Updated: 2/7/2026)
Click here to contact Mike Winters, MBA, MD
Oxygen-ICU Trial
A few additional important points about this particular study should be emphasized:
Girardis M, et al. Effect of conservative vs conventional oxygen therapy on mortality among patients in an intensive care unit. The Oxygen-ICU randomized trial. JAMA 2016. [epub ahead of print]
Category: Visual Diagnosis
Posted: 10/10/2016 by Tu Carol Nguyen, DO
Click here to contact Tu Carol Nguyen, DO
57 year-old female with history of bilateral lung transplants presents with fever, and 2 days of a painful, red, bumpy rash over the left labia and left buttock, but also notes a small tender area on the plantar surface of the left foot.
Below is a figure depicting the location of the rash, as well as a photo of her foot.
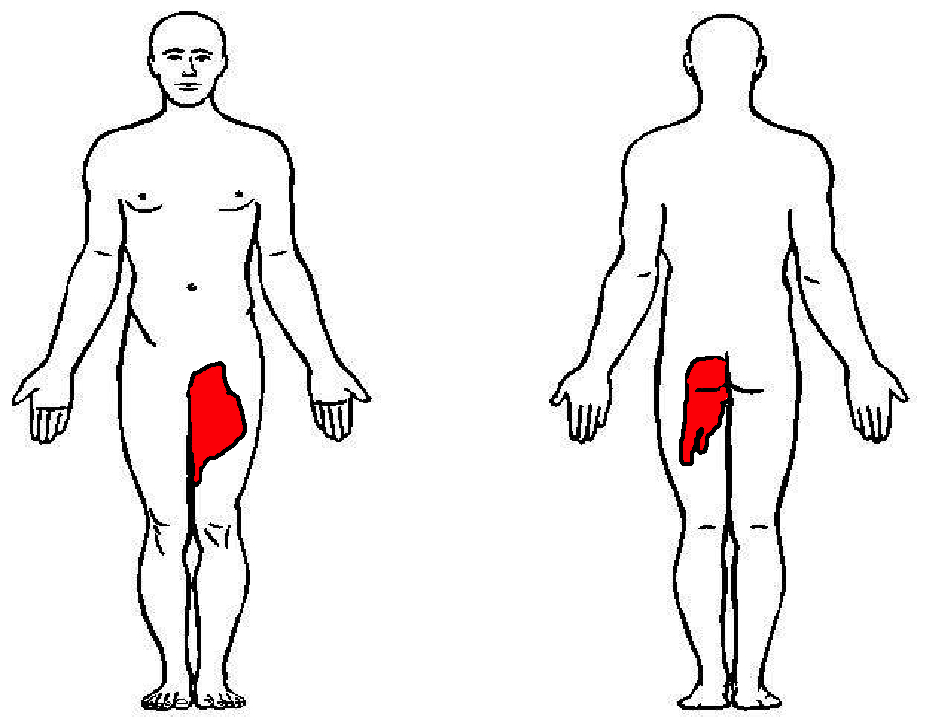
This is Herpes Zoster (Shingles).
Presentation:
Treatment:
Dworkin RH, Johnson RW, Breuer J, et al. Recommendations for the management of herpes zoster. Clin Infect Dis. 2007;44 Suppl 1:S1.
Category: Orthopedics
Keywords: Shoulder dislocation (PubMed Search)
Posted: 10/8/2016 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Recurrence depends on age and activity level
27% if >30yo and 72% if <23yo
Surgical Recommendations:
Large bony Bankart lesion, glenoid or humeral head defect >25%, recurrent instability, event near the end of season
Non surgical return to play:
If event occurs at beginning/early in season
Rehabilitation for 2 to 3 weeks (most return to play in this time frame)
Immobilization for 3 to 7 days in simple sling, gentle range of motion, cryotherapy
Physical therapy to strengthen dynamic stabilizers
Shoulder stabilization brace for non overhead throwing and contact sports
http://sph.sagepub.com/content/early/2016/06/02/1941738116651956.abstract
Category: Toxicology
Keywords: Poison Ivy, Toxicodendron, Urushiol (PubMed Search)
Posted: 10/6/2016 by Kathy Prybys, MD
(Updated: 10/7/2016)
Click here to contact Kathy Prybys, MD
Fall clean up = Poison Ivy, oak, sumac (Toxicodendron species) which is ubiquitous in North America but it can also be found in British Columbia, Mexico and in parts of Asia. These plants are truly the scourge of outdoor enthusiasts and agricultural workers responsible for up to 40 million cases of miserable often temporarily incapacitating rashes annually.
Fast Facts:
Treatment Tips:
Toxicodendron dermatitis:poison ivy,oak, sumac. Gladman AC. Wilderness Environ Med. 2006. Summer ;17(2):120-8.
Compositions and methods for removing urushiol and treating resulting skin condition.
US 7858570 B2
Category: International EM
Keywords: Infectious disease, ultrasound, HIV, TB (PubMed Search)
Posted: 9/29/2016 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 10/5/2016)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
What is the FASH Exam?
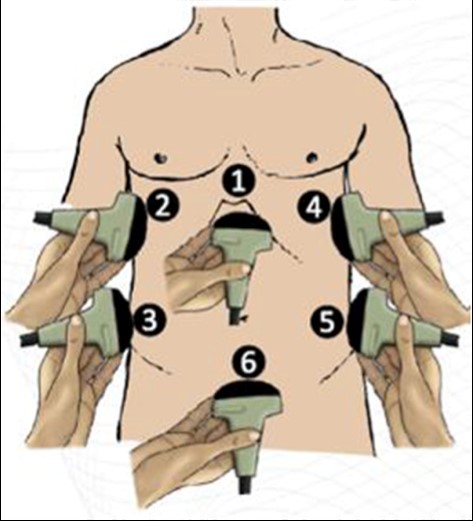
Submitted by Dr. Laura Diegelmann
Category: Critical Care
Keywords: Acid-base, SID, Delta Gap (PubMed Search)
Posted: 10/4/2016 by Rory Spiegel, MD
Click here to contact Rory Spiegel, MD
The delta gap is a measurement intended to assess for mixed acid-base disorders. A straightforward alternative, the strong ion difference (SID), allows for a quick and simple assessment of any non-gap acidosis or alkalosis that may be present.
The SID is simply the difference between the strong cations (Na+, K+, Mg+, Ca+) and the strong anions (Cl-) present in the serum. The abbreviated SID is the difference between the serum sodium and serum chloride levels (approximately 138-102). Values typically range from 36-40 mg/dl. Values less than 36 denote the presence of some degree of hyperchloremic, non-gap, acidosis. While values greater than 40 demonstrate the presence of hypochloremic, non-gap, alkalosis. And while on rare occasions, variations in albumin or elevated levels of cations other than sodium can lead you astray, the SID is as accurate as a delta gap at identifying mixed acid-based disorders without the added mathematical complexity.
Story DA. Stewart Acid-Base: A Simplified Bedside Approach. Anesth Analg. 2016;123(2):511-5.
Category: Visual Diagnosis
Posted: 10/3/2016 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
A 41 year old female presenting with intermittent RUQ abdominal pain for 1 week. An ultrasound of the right upper quadrant was performed. What is the diagnosis ?
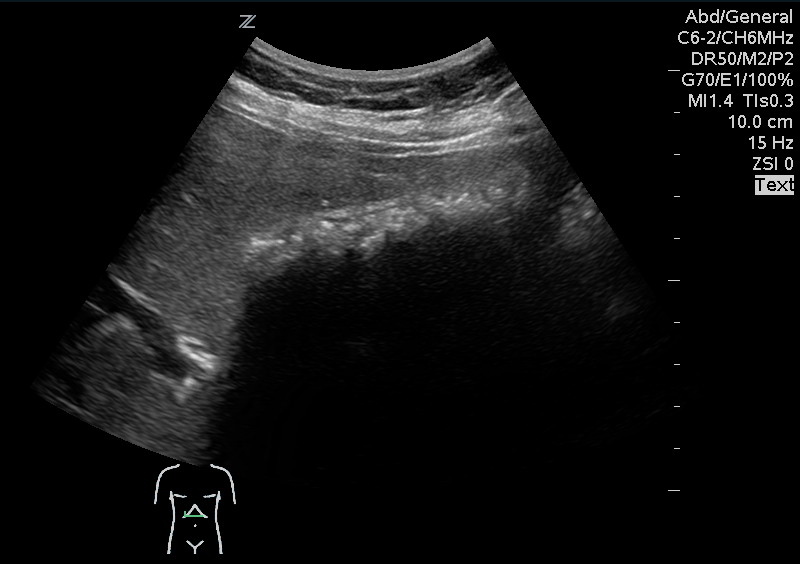

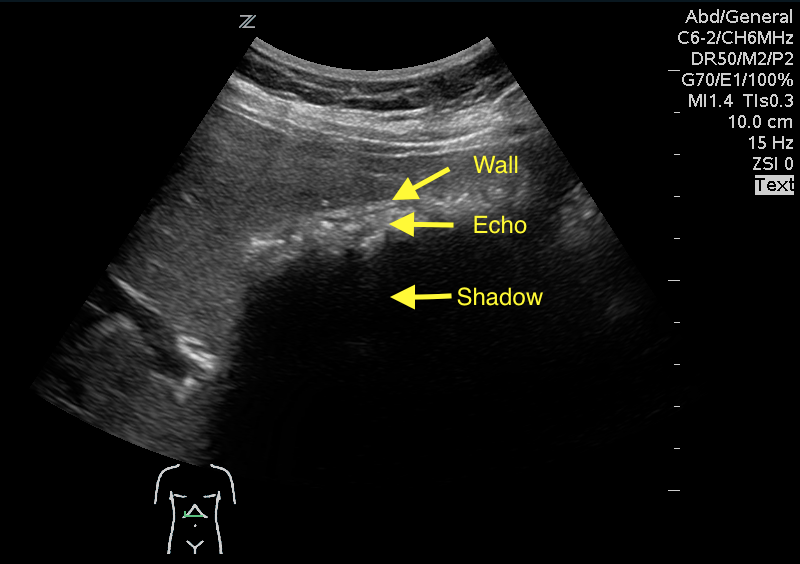
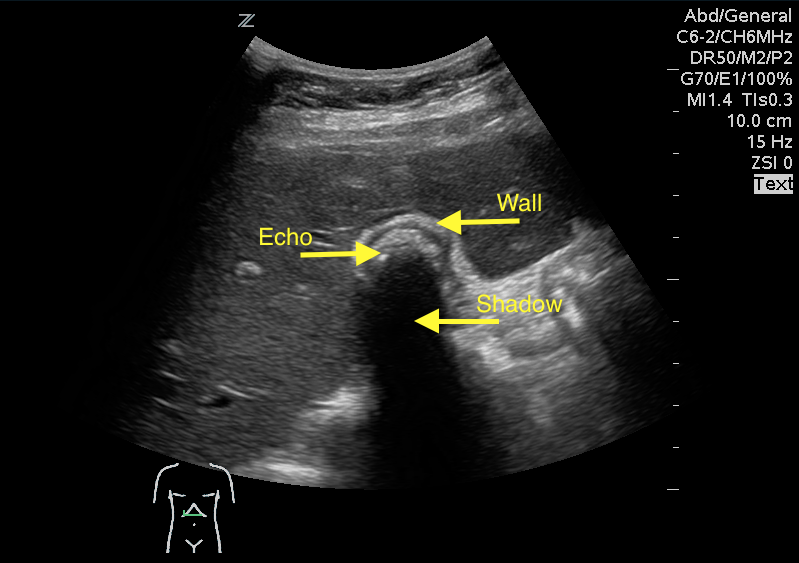
Answer: WES sign
WES sign stands for Wall Echo Shadow sign. It is a triad of:
1- Thick echogenic gall bladder wall (W)
2- Echoes filling the gallbladder (E)
3- A posterior acoustic shadow (S)
Rybicki, F. J. (2000). The WES Sign 1. Radiology, 214(3), 881-882.
Category: Pharmacology & Therapeutics
Keywords: QTc prolongation, torsades, antiemetics, antihistamines (PubMed Search)
Posted: 10/1/2016 by Michelle Hines, PharmD
Click here to contact Michelle Hines, PharmD
What they did:
What they found:
Application to clinical practice:
Burdette S, Roppolo LP, Green W, et al. The effect of antiemetics and antihistamines on the QTc interval in emergent dialysis patients with baseline QTc prolongation. J Emerg Med 2016; 51:99-105. (PMID 27614302)
Follow me on Twitter @mEDPharmD
Category: Pediatrics
Keywords: nickel dermatitis, contact irritant, allergy (PubMed Search)
Posted: 10/1/2016 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
A 12 year old male who recently started middle school presents to the ED with a rash in the periumbilical region that has been developing over the last few weeks. The rash is scaly, somewhat itchy, but otherwise benign appearing. The patient has no known medical conditions other than eczema, and is otherwise well. What is the diagnosis?
Picture courtesy of Mara Haseltine, MD

-Nickel allergy dermatitis is a type of allergic contact dermatitis common in skin tests in 8-16% of the pediatric population. Unlike irritant dermatitises (such as exposure to poison ivy), it usually takes repeated exposure over time to develop. In this case, the back of the button on a pair of blue jeans was the offending agent, though belt buckles, earrings, watches, piercings, and any other metal that touches skin can also cause a similar reaction. -The process is a delayed type hypersensitivity reaction mediated by T cells. Topical steroids can help clear up the rash, but the best treatment is to remove contact with the offending agent. One simple method is to apply clear nail polish to the back of the metal button or otherwise cover it with a piece of cloth. -Between 10 and 16 percent of blue jean buttons may contain nickel according to two studies. -Commercial test kits are available to help determine what metal components contain nickel -Known metal allergies should be communicated and documented as it can complicate orthopedic appliances or cardiac stents
1. T. Suneja, K. Flanagan and D. Glaser, "Blue-jean button nickel; prevalence and prevention of its release from buttons," Dermatitis, vol. 18, no. 4, pp. 208-211, December 2007 .
2. T. Byer and D. Morrell, "Periumbilical Allergic Contact Dermatitis: Blue Jeans or Belt Buckles?," Pediatric Dermatology, vol. 21, no. 3, pp. 223-226, May-June 2004.
3. J. Brasch and J. Geier, "Patch Test REsults in Schoolchildren. Results from the Information Netowrk of Departments of Dermatology (IVDK) and the German Contact Dermatitis Group (DKG)," Contact Dermatitis, vol. 37, pp. 286-93, 1997.
4. W. Weston, J. Weston and J. Kinoshita, "Prevalence of Positive Epicutaneous Tests Among Infants, Children, and Adolescents," Pediatrics, vol. 78, pp. 1070-1074, 1986.
Category: Neurology
Keywords: lumbar puncture, meningitis, INR, warfarin, spinal, bleeding (PubMed Search)
Posted: 9/28/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
You have a patient in whom you suspect meningitis, but he is on warfarin for a history of pulmonary embolism. You started empirical antibiotics. His INR is 2.6, and you want to do a lumbar puncture (LP) to confirm your diagnosis. Can you use Prothrombin Complex Concentrate to lower his INR and safely perform the LP?
Take Home Point:
Using PCC to lower INR to enable LP is relatively safe and effective in patients on vitamin K antagonists. The dose used was individually determined by the physician according to initial INR.
Limitation:
This is a retrospective study, with no control group. One patient (2.7%) had a myocardial infarction that was “possibly related” to the PCC administration.
In Depth:
This is a retrospective study, with no control group. However, it is the largest study to date that was specifically designed to answer this clinical question, including 37 patients over a 10-year period, with the following results:
- PCC was effective 90% of patients
- The median INR was 2.2 before, and 1.3 after (checked immediately after the infusion)
- The median time from starting the infusion and LP was 135 minutes.
- None of the patients had a spinal hemorrhage or allergic reaction.
- Some patients were started on vitamin K according to the physician’s discretion, with variable starting times of anticoagulation after the procedure (if at all).
Laible M, Beynon C, Sander P, et al. Treatment with Prothrombin Complex Concentrate to Enable Emergency Lumbar Puncture in Patients Receiving Vitamin K Antagonists. Ann Emerg Med. 2016 Sep;68(3):340-4
Category: Critical Care
Keywords: Fluids, Fluid resuscitation, Metabolic Acidosis (PubMed Search)
Posted: 9/27/2016 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
TAKE HOME POINTS:
-- High chloride load is associated with adverse outcomes in large-volume resuscitation (>60mL/kg in 24h), including increased risk of death [1]
-- Avoid supraphysiologic chloride solutions (i.e. normal saline) when resuscitation volumes are likely to exceed 60mL/kg (e.g. sepsis, DKA)
-- Hyperchloremic metabolic acidosis (HMA) is frequently associated with large-volume resuscitation, particularly with normal saline (0.9% NS) [2]
--HMA can result in decreased renal blood flow and renal cortical hypoperfusion, even in healthy volunteers [3]
-- Chloride load is also associated with acute kidney injury in this study, but this effect goes away once severity of illness is controlled.
-- It is not clear why increased chloride load is associated with increased mortality
-- Consider more "physiologic" fluids, such as plasmalyte A
1. Sen A, Keener CM, et al. Chloride Content of Fluids Used for Large-Volume Resuscitation Is Associated With Reduced Survival. Crit Care Med. 2016 Sep 15. [Epub ahead of print]
2. Kellum JA. Saline-induced hyperchloremic metabolic acidosis. Crit Care Med. 2002 Jan;30(1):259-61.
3. Chowdhury AH, Cox EF, et al. A randomized, controlled, double-blind crossover study on the effects of 2-L infusions of 0.9% saline and plasma-lyte 148 on renal blood flow velocity and renal cortical tissue perfusion in healthy volunteers. Ann Surg. 2012 Jul;256(1):18-24.
Category: Visual Diagnosis
Posted: 9/14/2016 by Tu Carol Nguyen, DO
(Updated: 9/26/2016)
Click here to contact Tu Carol Nguyen, DO
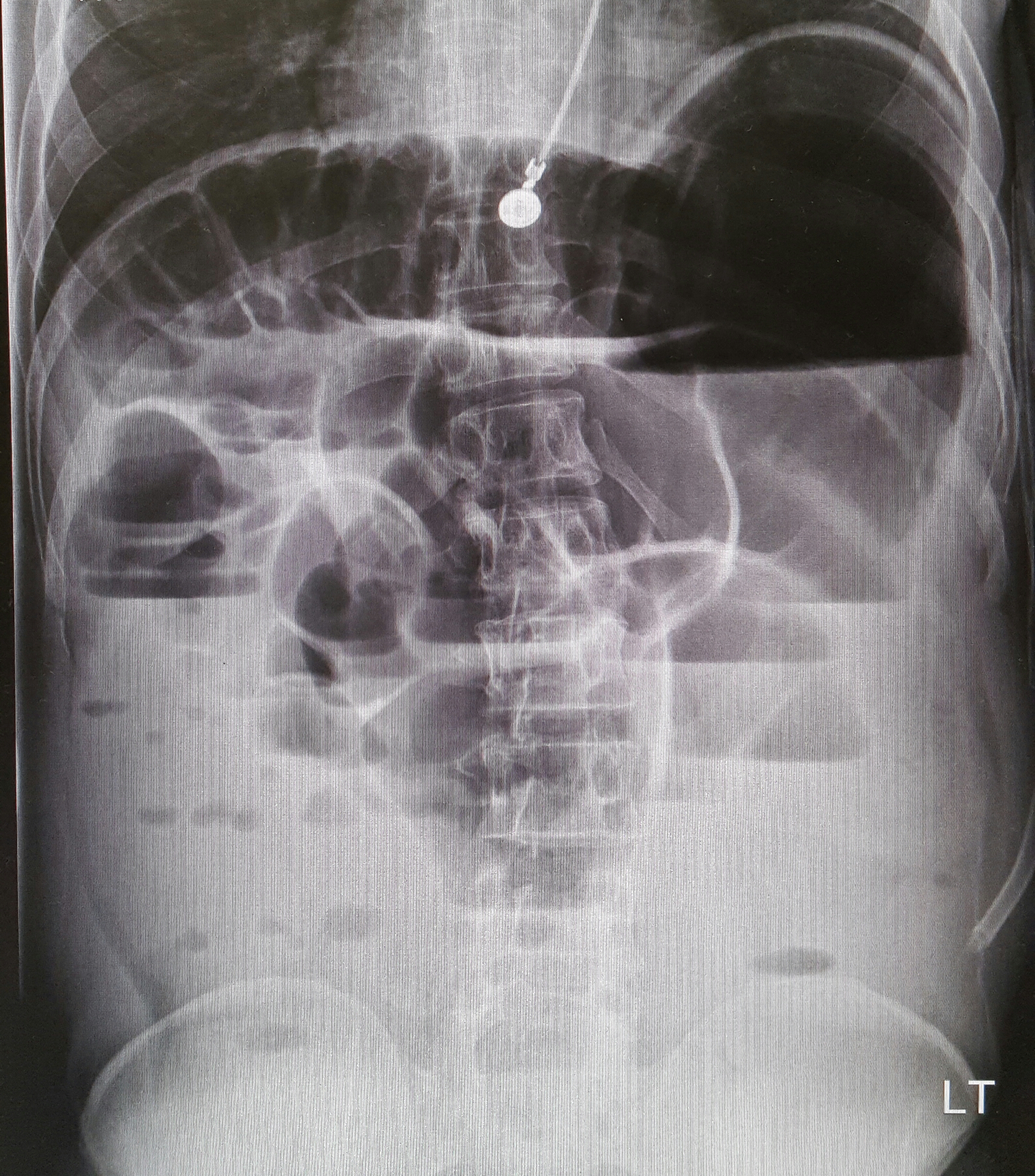
22-year-old male with history of autism, mental retardation who is non-verbal presents with abdominal pain and vomiting for one day. Patient was found clutching his abdomen and moaning. What's the diagnosis?
Small Bowel Obstruction
See the corresponding upright abdominal x-ray, showing dilated bowel with air fluid levels.
Kameda T, Taniguchi N. Overview of point-of-care abdominal ultrasound in emergency and critical care. J Intensive Care. 2016 Aug 15;4:53. doi: 10.1186/s40560-016-0175-y. eCollection 2016. Review.
Unl er EE, Yava i O, Ero lu O, Yilmaz C, Akarca FK. Ultrasonography by emergency medicine and radiology residents for the diagnosis of small bowel obstruction. Eur J Emerg Med. 2010 Oct; 17(5):260-4.
Category: Orthopedics
Keywords: Back pain, groin pain (PubMed Search)
Posted: 9/22/2016 by Brian Corwell, MD
(Updated: 9/24/2016)
Click here to contact Brian Corwell, MD
Retroperitoneal hemorrhage
The pathophysiology is unknown. Some hypothesize that occult vasculopathy and arteriosclerosis of the small vessels in the retroperitoneum may render them friable and therefore prone to rupture. This can be seen in minor trauma in sports and forceful vomiting or coughing. Spontaneous bleeding starts at the microvascular level, and large vessels become disrupted or stretched as the hematoma enlarges.
Retroperitoneal hemorrhage occurs in a variety of clinical circumstances, including spontaneous hemorrhage into a pre-existing benign adrenal cyst or bleeding from a left inferior phrenic artery, tumors of the adrenal gland and kidney, rupture of any blood vessel (most commonly infrarenal aorta); percutaneous interventions (such as cardiac catheterization), trauma, and polycythemia vera,
It is most commonly seen in association with patients with bleeding abnormalities, in HD patients and with anticoagulation therapy,. Risk is much greater with unfractionated heparin therapy than with warfarin. In most of the heparin patients studied, their coagulation parameters were in the therapeutic range.
Patients may present to the non acute area of the ED with back, lower abdominal or groin discomfort, Over time, this may progress to hemodynamic instability, and a fall in hemoglobin, Early identification is crucial to improving patient morbidity and mortality. Early symptoms depend on the location of the bleeding.
Hematoma near or within the iliopsoas muscle usually presents as femoral neuropathy (groin pain or leg weakness).
Femoral neuropathy caused by retroperitoneal hematoma can present with sudden onset severe pain in the affected groin and hip, with radiation to the anterior thigh and the lumbar region. This can easily be missed as the presentation is similar to a pulled msucle or strained hip/back. Iliopsoas muscle spasm often results in the characteristic flexion and external rotation of the hip, and any attempt to extend the hip will result in severe pain. Over time, pain and parasthesia in the antero-medial thigh and leg is seen.
Chan, Morales; et al., 2008. Int J Clin Pract.
Category: International EM
Keywords: Non-communicable diseases, heart attack, cardiac arrest, NSTEMI (PubMed Search)
Posted: 9/21/2016 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Non –communicable diseases (NCDs), primarily cardiovascular diseases, cancer, respiratory diseases and diabetes, are significantly increasing globally. According to the WHO, cardiovascular diseases alone account for 17.5 million deaths annually- the most of any NCD.
If someone has return of spontaneous circulation after cardiac arrest, but does not have ST-elevations on their post-arrest ECG, should you emergently activate the cath lab?
In a just released systematic review and meta-analysis in Resuscitation, Dr. Millin and colleagues found that almost one third of patients successfully resuscitated without ST elevation on their ECG had a culprit lesion that would benefit from emergent intervention.
Bottom Line: While this is not definitive proof to emergently activate the cath lab for a NSTEMI, it is another strong indication that post cardiac arrest patients without ST elevation may benefit from emergent percutaneous coronary intervention.
http://www.who.int/mediacentre/factsheets/fs355/en/
Millin MG, Comer AC, Nable JV, Johnston PV, Lawner BJ, Woltman N, Levy MJ, Seaman KG, Hirshon JM. Patients without ST elevation after return of spontaneous circulation may benefit from emergent percutaneous intervention: a systematic review and meta-analysis. Resuscitation. 2016 Sep 15. pii: S0300-9572(16)30461-0. doi: 10.1016/j.resuscitation.2016.09.004. [Epub ahead of print]
Category: Critical Care
Keywords: passive leg raise, arterial pressure, pulse pressure variation, volume responsiveness, fluid resuscitation (PubMed Search)
Posted: 9/20/2016 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Pitfalls with PLR
Aneman A, Sondergaard S. Understanding the passive leg raising test. Intensive Care Med. 2016; 42:1493-5.
Category: Visual Diagnosis
Posted: 9/19/2016 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
A 67 year old female with history of CVA, presented from a nursing home with RUQ abdominal pain and inablitiy to tolerate PO for 3 days. A CT scan of her abdomen was obtained. What is the diagnosis ?

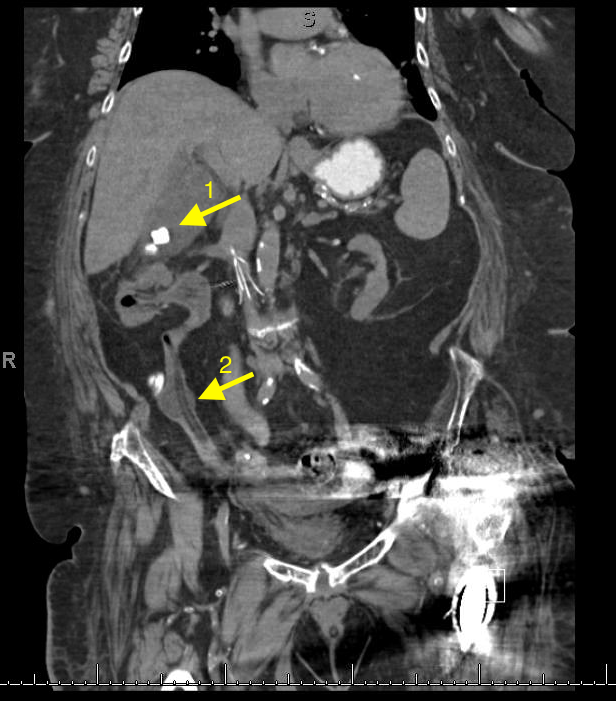
1- Cholecystitis
Ultrasound remains the best modality to test for cholecystitis. However, CT scans can still be obtained for non-classic presentations. The negative predictive value of CT is still relatively high. CT has a negative predictive value of 89%, compared to 97% to that of ultrasound. The absence of cholecysitis on CT will help the argument against the diagnosis, but if the suspicion is high an ultrasound study should still be obtained.
Things to look for on an abdominal CT that are suggestive of cholecysitis:
Gallbladder distension ( >5 cm width, >8 cm length).
Wall thickening ( >4mm thickness).
Pericholecystic fat stranding.
Presence of gallstones.
2- An inflated foley catheter in the ureter!
Ureteric insertion of foley catheters is a very rare complication of foley catheterization. There are no clear predisposing factors to this complication. However, it is thought that the presence of an underlying anatomical deformity (e.g. abnormal ureteric insertion site) might put the patient at a higher risk for it. Inflating a balloon in the ureter might result in severe ureteric injury. A suggested method to prevent this kind of injury is to perform bladder aspiration to insure balloon positioning prior to inflation.
References
1- Shakespear, Jonathan S., Akram M. Shaaban, and Maryam Rezvani. "CT findings of acute cholecystitis and its complications." American Journal of Roentgenology 194.6 (2010): 1523-1529.
2- Kim, Myung Ki, and Kwangsung Park. "Unusual complication of urethral catheterization: a case report." Journal of Korean medical science 23.1 (2008): 161.
Category: Orthopedics
Keywords: Patellofemoral Syndrome (PubMed Search)
Posted: 9/10/2016 by Michael Bond, MD
(Updated: 9/17/2016)
Click here to contact Michael Bond, MD
Patellofemoral Syndrome Treatment options
Patients do best with a combined intervention (ie, exercise therapy, education, manual therapy and taping) plan or patellofemoral bracing may improve outcomes for people with patellofemoral syndrome and the subtype of patellofemoral osteoarthritis.
For for the ED, we can start NSAIDs, and then have them follow up with Physical Therapy, A sports trainer if in organized sports, or with a sports medicine physician/PCP. Physical therapy is targeted at strengthening the quadricep muscle particularly vastus medialis, which improves the patella’s tracking with knee flexion.
