Category: Critical Care
Posted: 11/22/2016 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
What Matters in Cardiac Arrest?
Jentzer JC, et al. Improving survival from cardiac arrest: A review of contemporary practice and challenges. Ann Emerg Med. 2016. [epub ahead of print]
Category: Visual Diagnosis
Keywords: Intussusception, pediatric, ultrasound (PubMed Search)
Posted: 11/21/2016 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
A 15 months old male with no past medical history, presenting with two days of decreased oral intake and decreased urine output. The exam was notable for minimal tenderness of abdomen. During an oral fluid challenge in the ED, the patient had a single episode of bilious vomiting. The ED physician ordered an ultrasound study and the results are shown below. What is the diagnosis?

Diagnosis: Intussusception.
- The use of point of care ultrasound in the ED shortens the time to diagnosis and to definitive treatment. It has a sensitivity of 98-100% even if done by an inexperienced sonographer.
- To diagnose intussusception in the pediatric population, use the High-frequency linear probe for a better image quality. Start with scanning the right upper quadrant, and then move down to scan all four quadrants.
- Classic ultrasound findings include either a Donut-shaped or a Pseudo-kidney appearance, seen as a hypoechoic outer ring and a hyperechoic center. Other variants include; Mesenteric Crescent, where the inner loop will have a crescent hyperechoic appearance with few hypoechoic areas representing lymph nodes, or Central Limb of the Intussusceptum, where a fluid collection is present in the central limb of the intussusceptum instead of a collapsed limb.
- Utilize the US doppler to check for blood flow to the intestinal loops. Diminished blood flow correlates with irreducibility.
Del-Pozo, Gloria, et al. "Intussusception in children: current concepts in diagnosis and enema reduction." Radiographics 19.2 (1999): 299-319.
Category: Pediatrics
Keywords: Ketamine, conscience sedation, pharmacology, pediatrics (PubMed Search)
Posted: 11/18/2016 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Using 1.5 mg/kg or 2 mg/kg of IV ketamine led to less redosing compared to using 1 mg/kg IV.
This was a prospective, double blinded, randomized controlled trial of children 3-18 years. 125 children were included in the study. They compared 1mg/kg, 1.5 mg/kg and 2 mg/kg doses. All doses were IV. Adequate sedation was achieved with all 3 doses of ketamine, and there was no increased risk of adverse events with the higher doses. However, using 1.5mg/kg or 2 mg/kg required less redosing.
Previous studies suggested a higher risk of adverse events if the initial dose was greater than 2.5 mg/kg or the total dose was more than 5 mg/kg.
Kannikeswaran et al. Optimal dosing of intravenous ketamine for procedural sedation in children in the ED – a randomized control trial. American Journal of Emergency Medicine 24 (2016) 1347-1353.
Category: Toxicology
Keywords: heroin overdose, observation period, bystander naloxone (PubMed Search)
Posted: 11/16/2016 by Hong Kim, MD
(Updated: 11/17/2016)
Click here to contact Hong Kim, MD
Recently a review paper was published regarding the duration of observation in heroin overdose patients who received naloxone.
It made several conclusions regarding heroin overdose:
It should be pointed out that this is a review paper of limited number of articles with variable quality. Additionally, the clinical history of “heroin use” may be unreliable as fentanyl and novel synthetic opioids are also sold as “heroin.” Providers should exercise appropriate clinical judgement when caring for these patients.
The paper attempted to answer following questions
Review conclusion (8 articles): Patients were safe to release if they had normal mentation and vital signs. Mortality from recurrent heroin toxicity was 0.13% - 0.49% within 24 to 48 hours after naloxone administration.
Review conclusion (5 articles): Wide range of observation period is reported. One study showed that 1-hour observation is sufficient when patients have normal ambulation, normal vital signs and GCS of 15 after 1-hour observation.
Review conclusion (15 articles): Rate of successful reversal ranged from 83% to 100% in the literature. Bystander and first responder naloxone administration is associated with minimum risk outside of mild opioid withdrawal symptoms.
The conclusion of this review paper only applies to heroin intoxication, a short-acting opioid. However, it can be difficult to discern clinically what type of opioid is causing the clinical toxicity as “heroin” may actually be other opioids such as fentanyl or other novel synthetic opioids (e.g. U-47700).
Clin Toxicol (Phila). 2016 Nov 16:1-7. [Epub ahead of print]
Do heroin overdose patients require observation after receiving naloxone?
Willman MW1, Liss DB1, Schwarz ES1, Mullins ME1.
Category: Critical Care
Keywords: CPR, Cardiac Arrest (PubMed Search)
Posted: 11/15/2016 by Rory Spiegel, MD
(Updated: 2/8/2026)
Click here to contact Rory Spiegel, MD
It is well documented that when left to our own respiratory devices we will consistently over-ventilate patients presenting in cardiac arrest (1). A simple and effective method of preventing these overzealous tendencies is the utilization of a ventilator in place of a BVM. The ventilator is not typically used during cardiac arrest resuscitation because the high peak-pressures generated when chest compressions are being performed cause the ventilator to terminate the breath prior to the delivery of the intended tidal volume. This can easily be overcome by turning the peak-pressure alarm to its maximum setting. A number of studies have demonstrated the feasibility of this technique, most recently a cohort in published in Resuscitation by Chalkias et al (2). The 2010 European Resuscitation Council guidelines recommend a volume control mode targeting tidal volumes of 6-7 mL/kg and a respiratory rate of 10 breaths/minute (3).
Category: Orthopedics
Posted: 11/12/2016 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
https://images.radiopaedia.org/images/3173801/1ee24da1a6fe907a27d2bf20481174.jpg
Young toddler presents with left lower leg pain. What is the diagnosis??
Metaphyseal Corner Fracture.
These are often very subtle findings! This fracture pattern was first seen in association with children with subdural hematomas.
https://images.radiopaedia.org/images/3173808/48ab0d13eb24f10de978b5c65af064_jumbo.jpg
It occurs due to shearing forces on the growth plate.
Most frequently seen in the distal femur, proximal humerus and tibia.
Can be bilateral.
Similar to bucket handle fracutres
Category: Neurology
Keywords: subarachnoid hemorrhage, mimic, pseudosubarachnoid hemorrhage, cerebral edema (PubMed Search)
Posted: 11/9/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Patient found pulseless after submersion in water for 20 minutes. After ROSC, patient’s GCS was 3 and pupils are dilated and nonreactive.

Kim JM, Eom TH. The pseudosubarachnoid hemorrhage: clinical implications of subarachnoid hemorrhage misdiagnosis. Pediatr Emerg Care. 2016 May 12. [Epub ahead of print]
Category: Critical Care
Posted: 11/8/2016 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
It's Election Day in the US, so here are some interesting facts about Presidential causes of death:
George Washington likely died from epiglottitis on 12/14/1799
CLICK BELOW FOR MORE INTERESTING FACTS!
Other interesting facts:
Leading causes of death:
Category: Visual Diagnosis
Posted: 11/7/2016 by Tu Carol Nguyen, DO
Click here to contact Tu Carol Nguyen, DO
8 year-old female with no PMH who presents with concerns for "purple patches" popping up on her arm for 2-3 days. Stated that one appeared and then, the other one appeared 12 hours later. She denied any trauma whatsoever, history of easy bleeding/bruising and did feel safe at home. The rest of the review of systems was negative.
Patient said there was mild pain when the area was touched. The rest of the physical examination was normal.
What's the diagnosis? (Image below)

Superficial Thermal Burn
Upon further questioning, patient stated that she had been making s'mores by roasting marshmallows over an electric stove 3 days prior. The burns showed up the subsequent morning.
Take Home Points:
Previous pearls about burns:
Pediatric Burns:
Monseau AJ, Reed ZM, Langley KJ, Onks C. Sunburn, Thermal, and Chemical Injuries to the Skin. Prim Care. 2015;42(4):591-605.
"Pathophysiology of Thermal Injury." Civic Plus. 2007.
Category: Pharmacology & Therapeutics
Keywords: anticoagulation, warfarin, heparin, bridge, DVT (PubMed Search)
Posted: 11/5/2016 by Michelle Hines, PharmD
Click here to contact Michelle Hines, PharmD
Do you have a patient with renal insufficiency who is in need of an anticoagulation bridge to warfarin? Subcutaneous unfractionated heparin (UFH) as an initial dose of 333 Units/kg subcutaneously followed by a fixed dose of 250 Units/kg (actual body weight) every 12 hours may be an alternative to admission for heparin infusion with monitoring.
Practical Considerations:
Kearon C, Ginsberg JS, Julian JA, et al. Comparison of fixed-dose weight-adjusted unfractionated heparin and low-molecular-weight heparin for acute treatment of venous thromboembolism. JAMA 2006; 296:935-42. [PMID 16926353]
Morris TA, Jacobson A, Marsh JJ, et al. Pharmacokinetics of UH and LMWH are similar with respect to antithrombin activity. Thromb Res 2005; 115:45-51. [PMID 15567452]
Holbrook A, Schulman S, Witt DM, et al. Evidence-based management of anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. CHEST 2012; 141(2)(Suppl):e152S-e184S. [PMID 22315259]
Follow me on Twitter @mEDPharmD
Category: International EM
Keywords: Infectious Disease, ultrasound, HIV, TB (PubMed Search)
Posted: 9/29/2016 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 11/3/2016)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
As noted in a previous post, the FASH exam is the Focused Assessment with Sonography for HIV/TB. Below are typical ultrasound images of a positive FASH exam.
Peri-aortic lymph nodes- Multiple enlarged nodes, 97.1% specific for TB
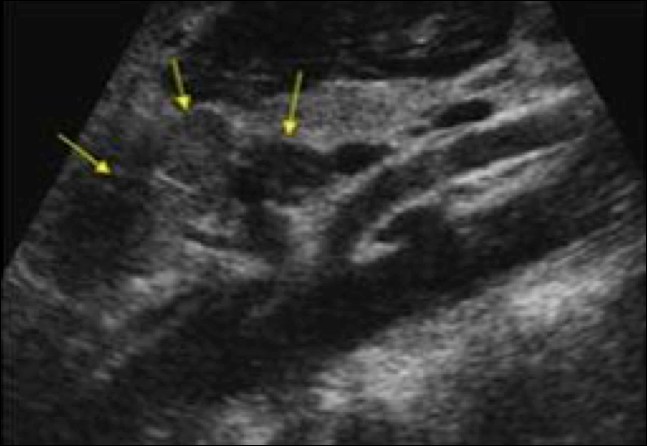
Splenic lesions – multiple ‘punched out’ lesions

The effusions often have fibrous stranding
Submitted by Dr. Laura Diegelmann
Category: Critical Care
Posted: 11/1/2016 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Dynamic LVOT Obstruction
Category: Visual Diagnosis
Posted: 10/31/2016 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
30 year old female presents with a painful finger for 1 week. Finger exam showed the following. What is the diagnosis ?

Herpetic whitlow
- It is caused by either HSV 1 or 2.
- Infection is usually transmitted by direct unprotected contact.
- Healthcare workers are at risk of contracting the infection if appropriate preventative measures were not taken when dealing with patients who have the infection.
- Diagnosis is mainly clinical. Tzank smears can be done to confirm the diagnosis if in doubt.
- Treatment with Acyclovir is thought to shorten the duration of the infection and prevent recurrence if started within 72 hours of beginning of symptoms.
- Incision of the vesicular lesion is contraindicated and can cause severe bacterial superinfection.
McDonald, Lucas S., et al. "Hand infections." The Journal of hand surgery36.8 (2011): 1403-1412.
Category: Pediatrics
Keywords: sickle cell, acute chest syndrome, pneumonia (PubMed Search)
Posted: 10/28/2016 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Typically, empiric treatment for lobar community acquire pneumonia (CAP) in immunized < 5 year olds (preschool) is amoxicillin (45mg/kg BID or 30 mg/kg TID for resistant S. pneumoniae) for outpatient and ampicillin or ceftriaxone for inpatient. Additional coverage with azithromycin is typically recommended for school age and adolescent patients (>= 5 years), but not necessarily for younger children unless there is a particular clinical suspicion for atypical pneumonia with history, xray findings, or sick contacts.
However, in sickle cell patient with suspicion for acute chest syndrome, azithromycin is recommended for all ages groups, as atypical bacteria such as Mycoplasma are a common cause of acute chest syndrome in patients of all ages with sickle cell disease even young children. In a prospective series of 598 children with acute chest syndrome, 12% of the 112 cases in children less than 5 had positive serologic testing of M. pneumoniae (9% of all cases had M. pneumoniae) (Neumayr et al, 2003).
1) Bradley et al. The Management of Community-Acquired Pneumonia in infants and children older than 3 months of age: Clinical Practice Guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin. Infect. Dis. 53:617-630 (2011)
2) Miller, S. How I treat acute chest syndrome in children with sickle cell disease. Blood 117:5297-5305 (2011)
3) Neumayr L, et al. Mycoplasma disease and acute chest syndrome in sickle cell disease. Pediatrics 1212:87-95 (2003)
Category: Toxicology
Keywords: buprenorphine exposure, pediatrics, retrospective study (PubMed Search)
Posted: 10/26/2016 by Hong Kim, MD
Click here to contact Hong Kim, MD
Recently, a retrospective study of unintentional buprenorphine/naloxone exposure among pediatric population was published. All patients were evaluated by toxicologists at the time of initial hospital presentation (or transfer) at the study center.
Bottom line
A retrospective study of single center/referral center’s toxicology consultation service.
88 patients were included. (median age: 24 months [range: 10 to 77 months]). Majority were transferred from other hospitals.
Sources of the medication were
Clinical effects
Naloxone
The median hospital stay was 22 hours (7 - 248 hours).
Category: Neurology
Keywords: contrast, epidural, multiple sclerosis (PubMed Search)
Posted: 10/26/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Magnetic resonance imaging (MRI) is the method of choice for imaging the spine for the suspicion of non-traumatic disorder, such as multiple sclerosis (MS), transverse myelitis, epidural abscess, spinal cord infarcts, and spondylotic myelopathy (changes in the spinal cord due to disk herniation or osteophytes in degenerative joint disease).
If the differential diagnosis includes infection, neoplasm, demyelination or inflammation, then IV contrast should be administered.
Singh K, Mechtler LL and Klein JP. Imaging of Spinal Cord Disorders. Continuum 2016;22(5):1595 1612
Category: Critical Care
Keywords: US, right ventricle, heart failure (PubMed Search)
Posted: 10/25/2016 by Rory Spiegel, MD
Click here to contact Rory Spiegel, MD
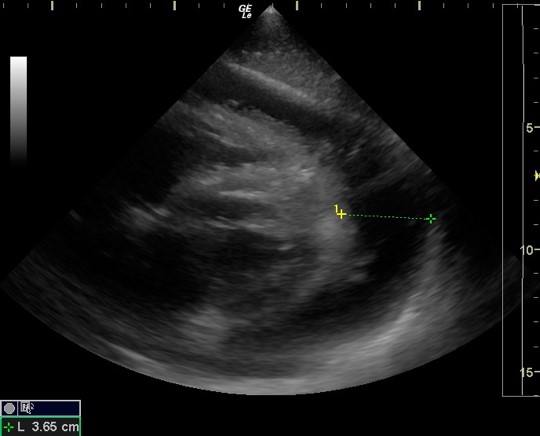
Recently Emergency Physicians have become far more aware of the importance of right ventricular (RV) function in our critically ill patient population. One of the methods that has been proposed to assess RV systolic function with bedside ultrasound (US) is the tricuspid annular plane systolic excursion (TAPSE). This simple bedside measurement utilizes M-mode to quantify the movement of the tricuspid annulus in systole. And while it has demonstrated reasonable accuracy at predicting RV dysfunction, adequate visualization of the lateral tricuspid annulus is not always obtainable in our critically ill patient population (1,2). In these circumstances an alternative measurement obtained in the subcostal window may be a viable option.
Similar to TAPSE, subcostal echocardiographic assessment of tricuspid annular kick (SEATAK) utilizes M-mode to assess the apical movement of the tricuspid annulus during systole. In a recent prospective observational study, Díaz-Gómez et al examined 45 ICU patients, 20 with known RV dysfunction and 25 with normal function. They compared the measurements obtained from TAPSE and SEATAK and found a strong correlation between the two measurement (Spearman’s ρ coefficient of .86, P=.03).
The small sample size and limited evaluation of RV function is far from ideal and more robust data sets are required before we cite SEATAK’s diagnostic accuracy with any confidence, but in the subset of patients where a TAPSE is unobtainable this may serve as an adequate surrogate until a more thorough echographic assessment can be obtained. 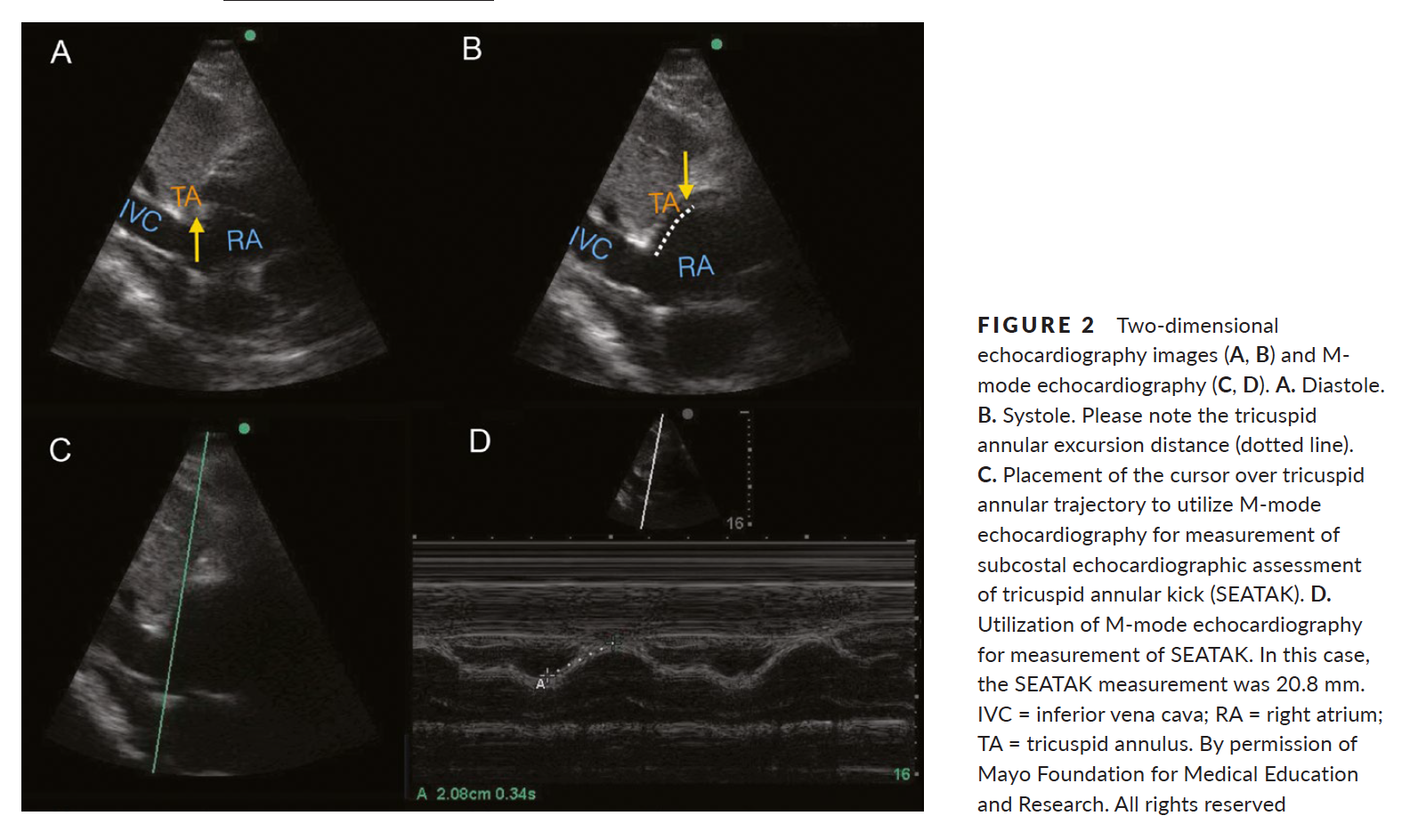
1. Ueti OM, Camargo EE, Ueti Ade A, et al. Assessment of right ventricular function with Doppler echocardiographic indices derived from tricuspid annular motion: comparison with radionuclide angiography. Heart. 2002;88:244–248.
2. Díaz-Gómez, J. L., Alvarez, A. B., Danaraj, J. J. , Freeman, M. L., Lee, A. S., Mookadam, F., Shapiro, B. P. and Ramakrishna, H. (2016), A novel semiquantitative assessment of right ventricular systolic function with a modified subcostal echocardiographic view. Echocardiography, 00: 1–9. doi: 10.1111/echo.13400.
Category: Visual Diagnosis
Posted: 10/25/2016 by Tu Carol Nguyen, DO
(Updated: 10/26/2016)
Click here to contact Tu Carol Nguyen, DO
20 year-old female presents with sore throat, right throat fullness, difficulty speaking for 2-3 days. A bedside ultrasound and subsequent CT was obtained as seen below. What's the diagnosis?
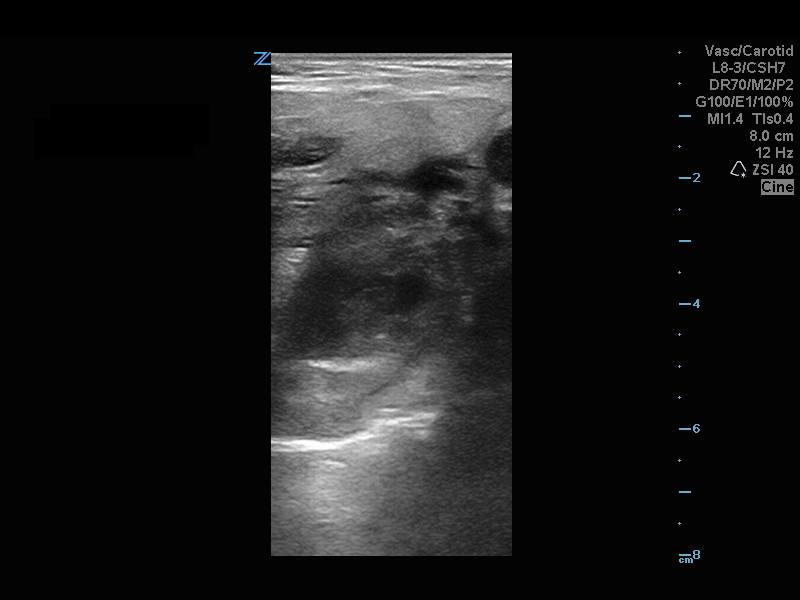
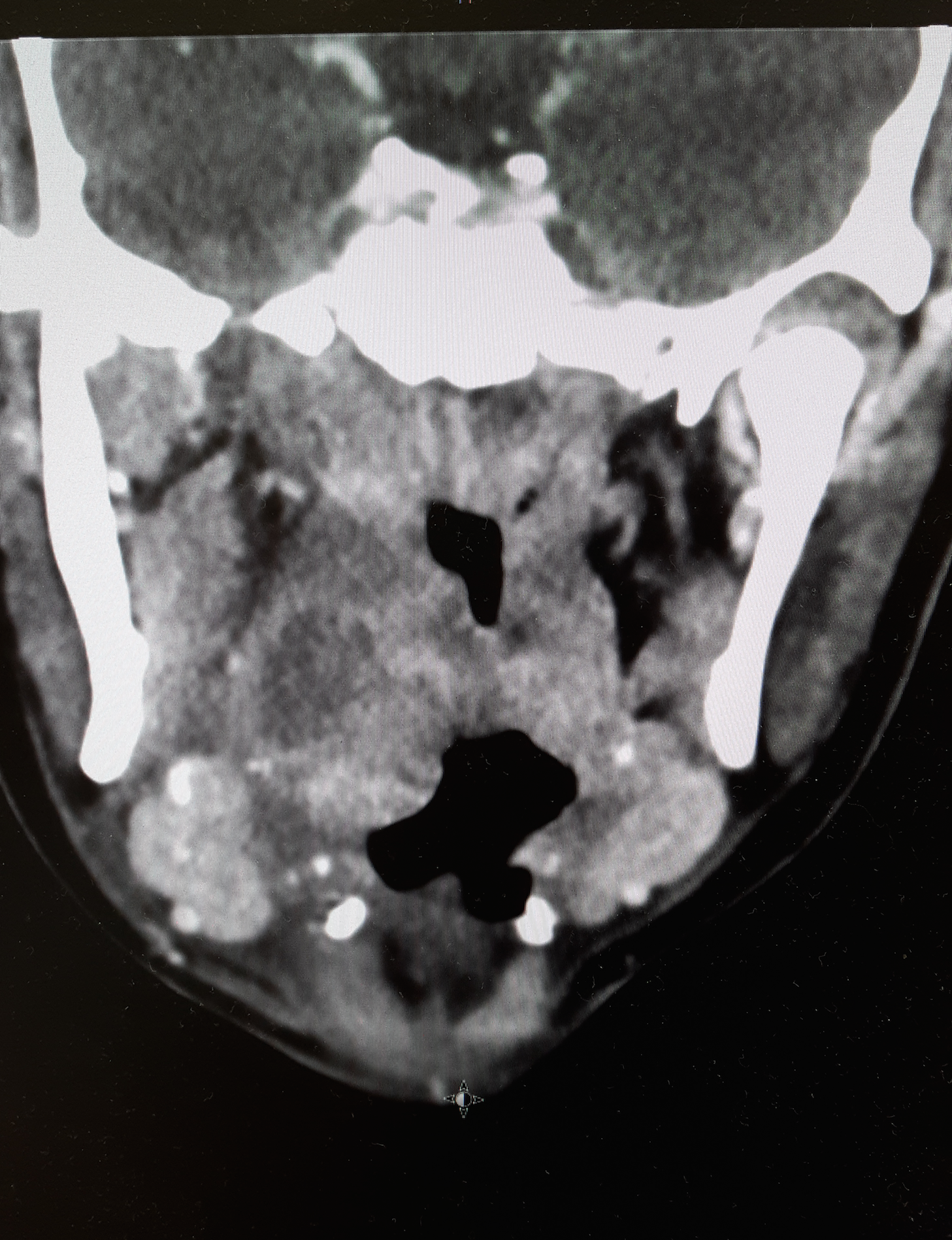
Peritonsillar Abscess
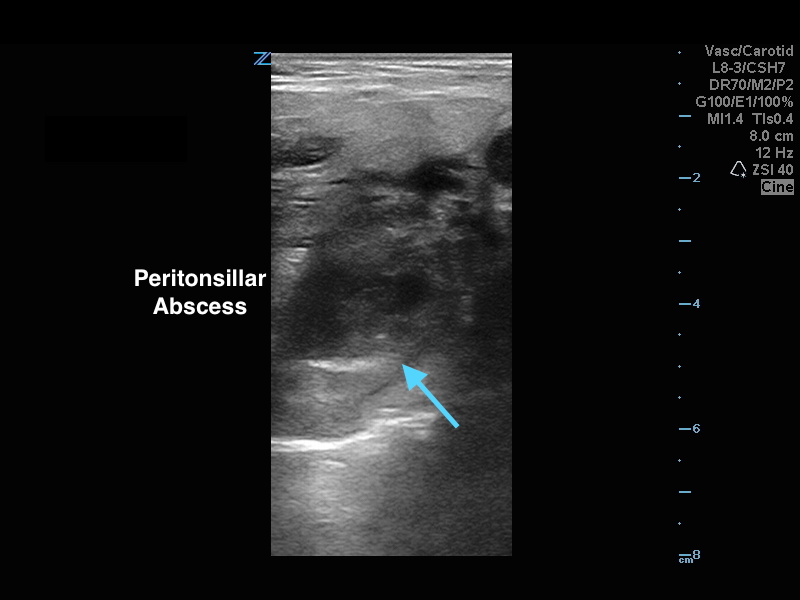
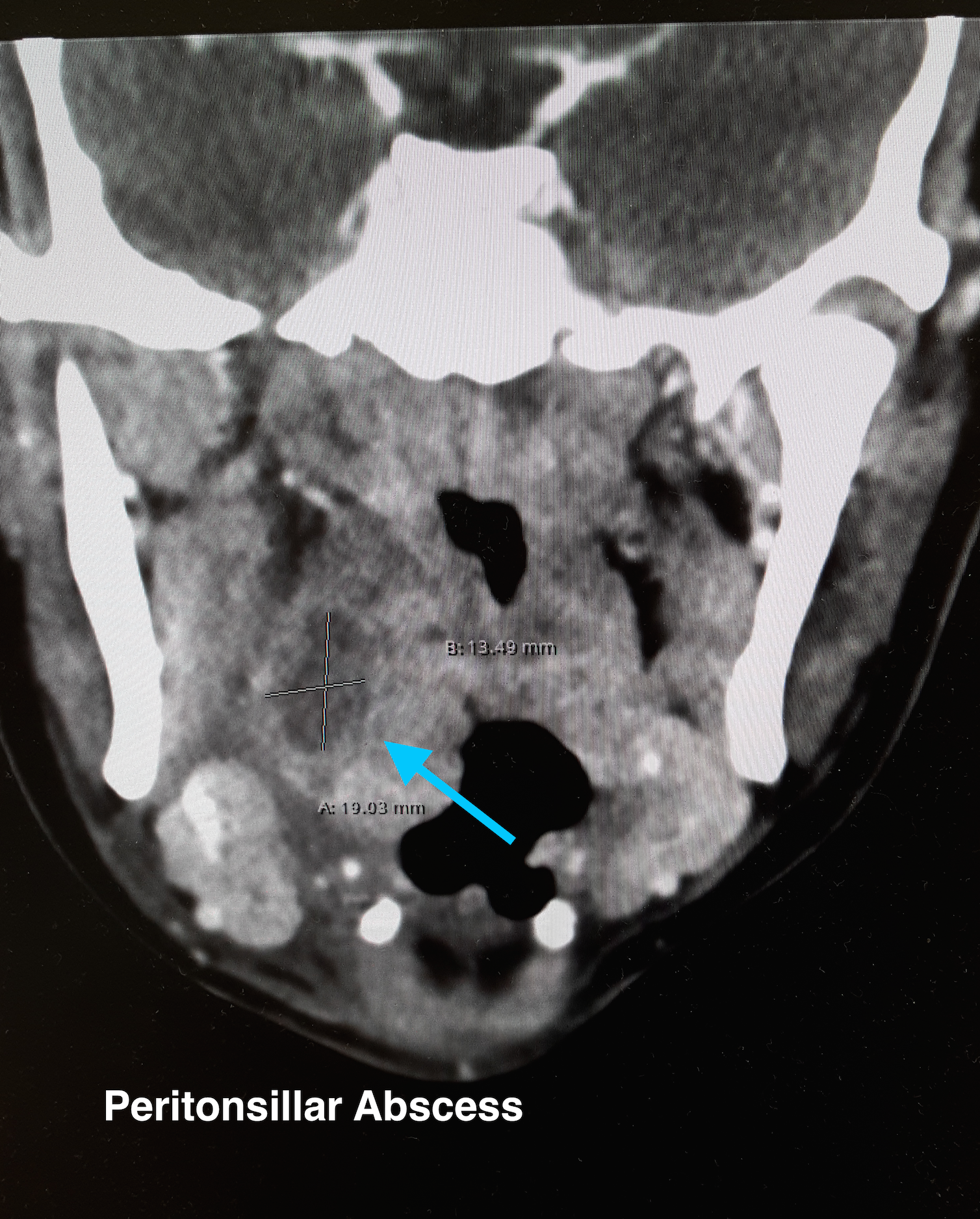
The ultrasound image is a transcutaneous approach with a linear transducer that is placed at the angle of the mandible of the affected side. This is an alternative approach to an intra-oral ultrasound with the endocavitary transducer if the patient has trismus.
Take Home Points:
How to do an intra-oral US-guided needle aspiration of PTA, check out:
http://www.ultrasoundpodcast.com/2012/01/episode-21-full-peritonsillar-abscess-podcast/
For a brief video on how to perform a transcutaneous US for PTA:
https://www.youtube.com/watch?v=JkIYOhKCweI&t=28s
Halm BM, Ng C, Larrabee YC. Diagnosis of a Peritonsillar Abscess by Transcutaneous Point-of-Care Ultrasound in the Pediatric Emergency Department. Pediatr Emerg Care. 2016;32(7):489-92.
Rehrer M, Mantuani D, Nagdev A. Identification of peritonsillar abscess by transcutaneous cervical ultrasound. Am J Emerg Med. 2013;31(1):267.e1-3.
Category: Orthopedics
Keywords: MI, exercise (PubMed Search)
Posted: 10/15/2016 by Brian Corwell, MD
(Updated: 10/22/2016)
Click here to contact Brian Corwell, MD
Many of us use exercise as a coping strategy when emotionally stressed or to blow off steam when angry. This may place your heart at risk.
A recent observational study in Circulation surveyed 12,000 first MI patients about potential triggers. The associations didn't depend on age, smoking status, hypertension, or baseline physical activity.
Anger or emotional upset in the hour before onset elevated odds of MI 2.44 fold
A similar 2.31 fold elevation was observed form heavy exertion
However, the combination of the two raised the odds to 3.05 fold (P<0.001 for interaction)
http://circ.ahajournals.org/content/134/15/1059
Category: Pediatrics
Keywords: Fluid resuscitation, gastroenteritis, dehydration (PubMed Search)
Posted: 10/21/2016 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Plasma-Lyte A outperformed 0.9% NaCl for rehydration in children with acute gastroenteritis showing a more rapid improvement in serum bicarbonate levels and dehydration scores.
This was a prospective randomized double blinded study in 8 pediatric emergency departments. Patients were at least 6 months old and younger than 11 years. To be included they had to have at least 3 episodes of vomiting or diarrhea in the previous 12 hours and a Gorelick score of at least 4. 100 children were included. Serum bicarbonate was measured at 0 and 4 hours and dehydration scores were reassessed. There was a change of bicarbonate of 1.6 mEq/L for plasma-lyte A (PLA) and no change for sodium chloride. There as an improvement in the dehydration score at 2 hours for the PLA group, but the dehydration scores were not statistically significant between the 2 groups at the 4 hours mark.
Allen et al. A randomized trial of Plasma-Lyte A and 0.9% sodium chloride in acute pediatric gastroenteritis. BMC Pediatrics 2016 16:117.
