Category: Toxicology
Keywords: naloxone, opioid intoxication (PubMed Search)
Posted: 9/15/2016 by Hong Kim, MD
Click here to contact Hong Kim, MD
Naloxone has been used to reverse opioid-induced respiratory depression for decades. The “standard” dose of opioid intoxication has been 0.4 mg. However, over the past decade, initial naloxone dose for opioid intoxication has evolved to recommend a lower initial dose (0.04 – 0.05 mg).
A recent article by Connors et al. reviewed 25 medical resources (internet, medical texts and study guides) of different medical specialties (internal medicine, medical toxicology, emergency medicine, pediatrics, anesthesiology, pain medicine and general medicine)
Findings:
Recent editions of emergency medicine text (Rosen’s and Tinitinalli) recommend using 0.04 – 0.05 mg IV in ED patients with history of opioid dependence. Higher doses of naloxone are recommended for non-opioid dependent/apneic patients.
However, history of opioid dependence is difficult to obtain in patients with opioid induced CNS/respiratory depression.
Administering 0.4 mg or higher dose may/can acute agitation or opioid withdrawal symptoms that can utilize more ED resources to calm agitated patient/management of withdrawal. Thus it may be prudent to use low-dose strategy (0.04 mg IV with titration) to minimize the risk of precipitating naloxone-induced opioid withdrawal/agitation.
Bottom line:
In opioid-induced respiratory depression/apneic patients:
To make 0.04 mg naloxone solution:
Connors NJ, Nelson LS. The evolution of recommneded naloxone dosing for opioid overdose by medical specialty. J Med Toxicol 2016;12:276-281.
Category: Neurology
Keywords: eyelid apraxia, eye opening apraxia (PubMed Search)
Posted: 9/14/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Category: Airway Management
Keywords: RSI, Preoxygenation (PubMed Search)
Posted: 9/13/2016 by Rory Spiegel, MD
Click here to contact Rory Spiegel, MD
During rapid sequence intubation (RSI) we endeavor to avoid positive pressure ventilation, prior to securing a definitive airway. As such, an adequate buffer of oxygen is necessary to ensure a safe apneic period. This process involves replacing the residual nitrogen in the lung with oxygen. It has been demonstrated that a standard nonrebreather (NRB) mask alone does not provide a high enough fractional concentration of oxygen (FiO2) to optimally denitrogenate the lungs (1). Even when a nasal cannula at 15L/min is utilized in addition to the NRB, the resulting FiO2 is not ideal. A bag-valve mask (BVM) with a one-way valve or PEEP valve has been demonstrated to provide oxygen concentrations close to that of an anesthesia circuit. But its effectiveness is drastically reduced if a proper mask seal is not maintained during the entire pre-oxygenation period (1). This is not always logistically possible in the chaos of an Emergency Department intubation.
A standard NRB with the addition of flush-rate oxygen appears to be a viable alternative. Recently published in Annals of Emergency Medicine, Driver et al demonstrated that a NRB with wall oxygen flow rates increased to maximum levels, rather than the standard 15L/min, provided end-tidal O2 (ET-O2) levels similar to an anesthesia circuit (2).
1. Hayes-bradley C, Lewis A, Burns B, Miller M. Efficacy of Nasal Cannula Oxygen as a Preoxygenation Adjunct in Emergency Airway Management. Ann Emerg Med. 2016;68(2):174-80.
2. Driver BE, Prekker ME, Kornas RL, Cales EK, Reardon RF. Flush Rate Oxygen for Emergency Airway Preoxygenation. Ann Emerg Med. 2016;
Category: Visual Diagnosis
Posted: 9/8/2016 by Tu Carol Nguyen, DO
(Updated: 9/12/2016)
Click here to contact Tu Carol Nguyen, DO
A 25-year-old male was brought in by EMS with a stab wound to the chest. What's the diagnosis?
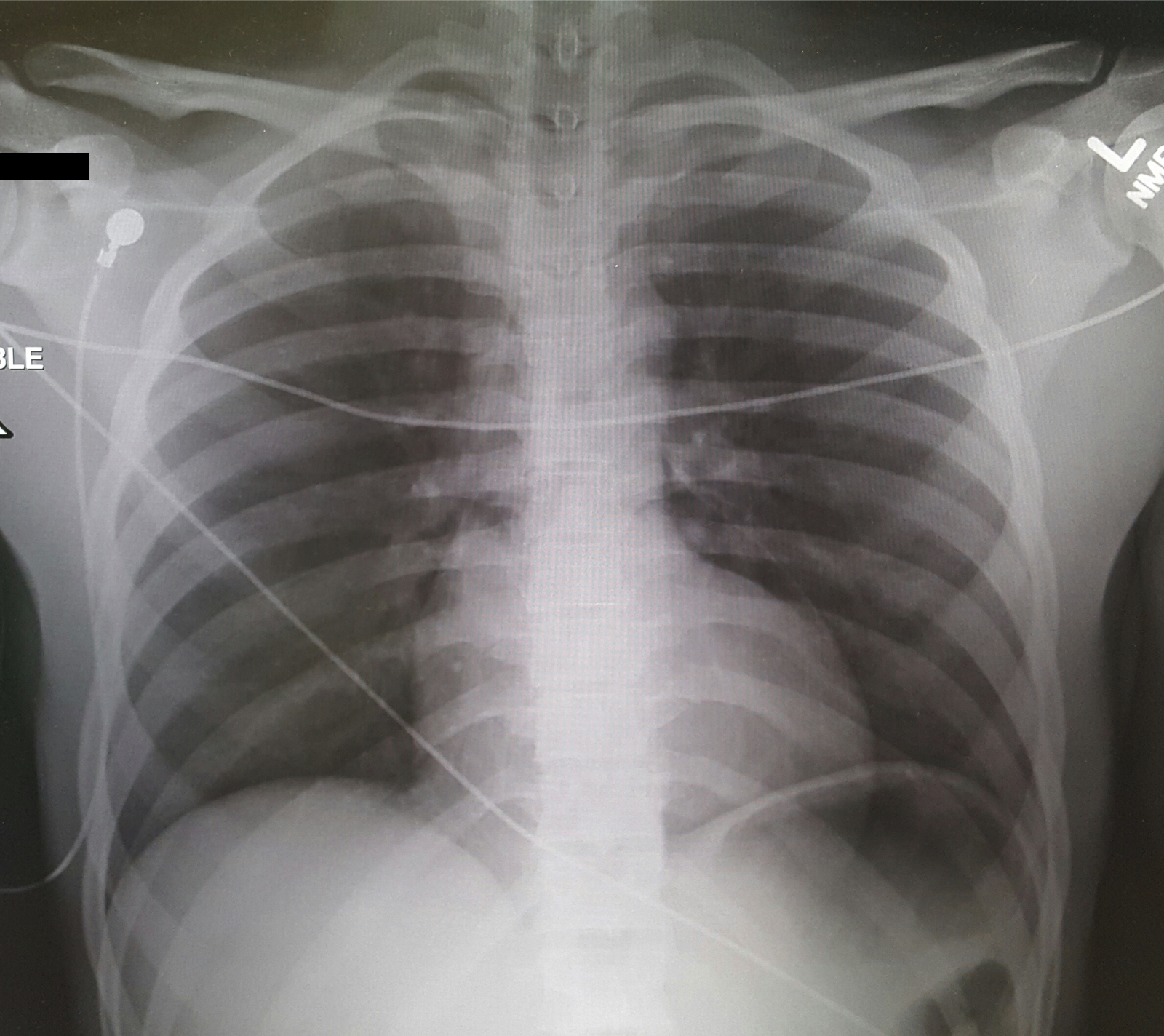
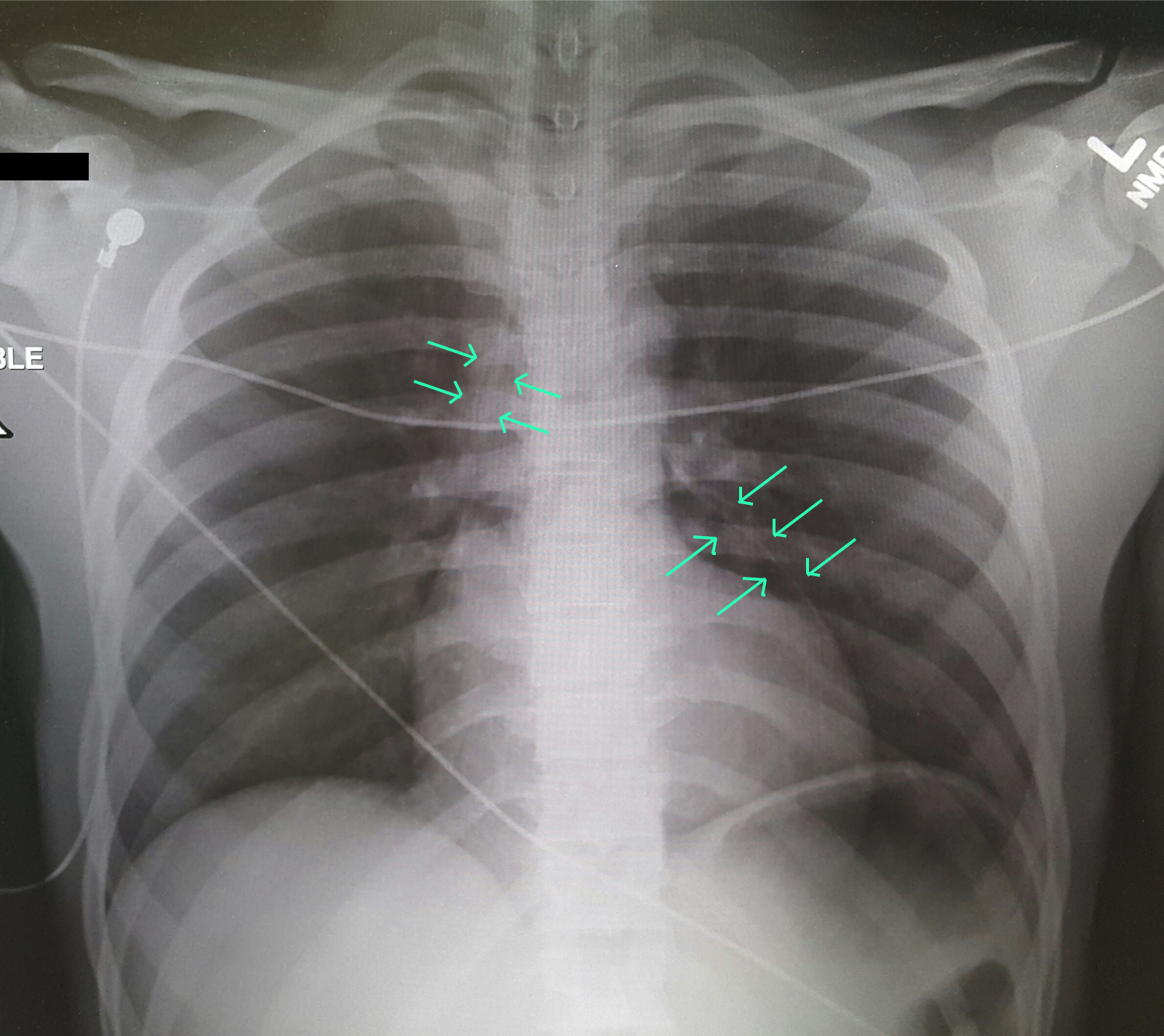
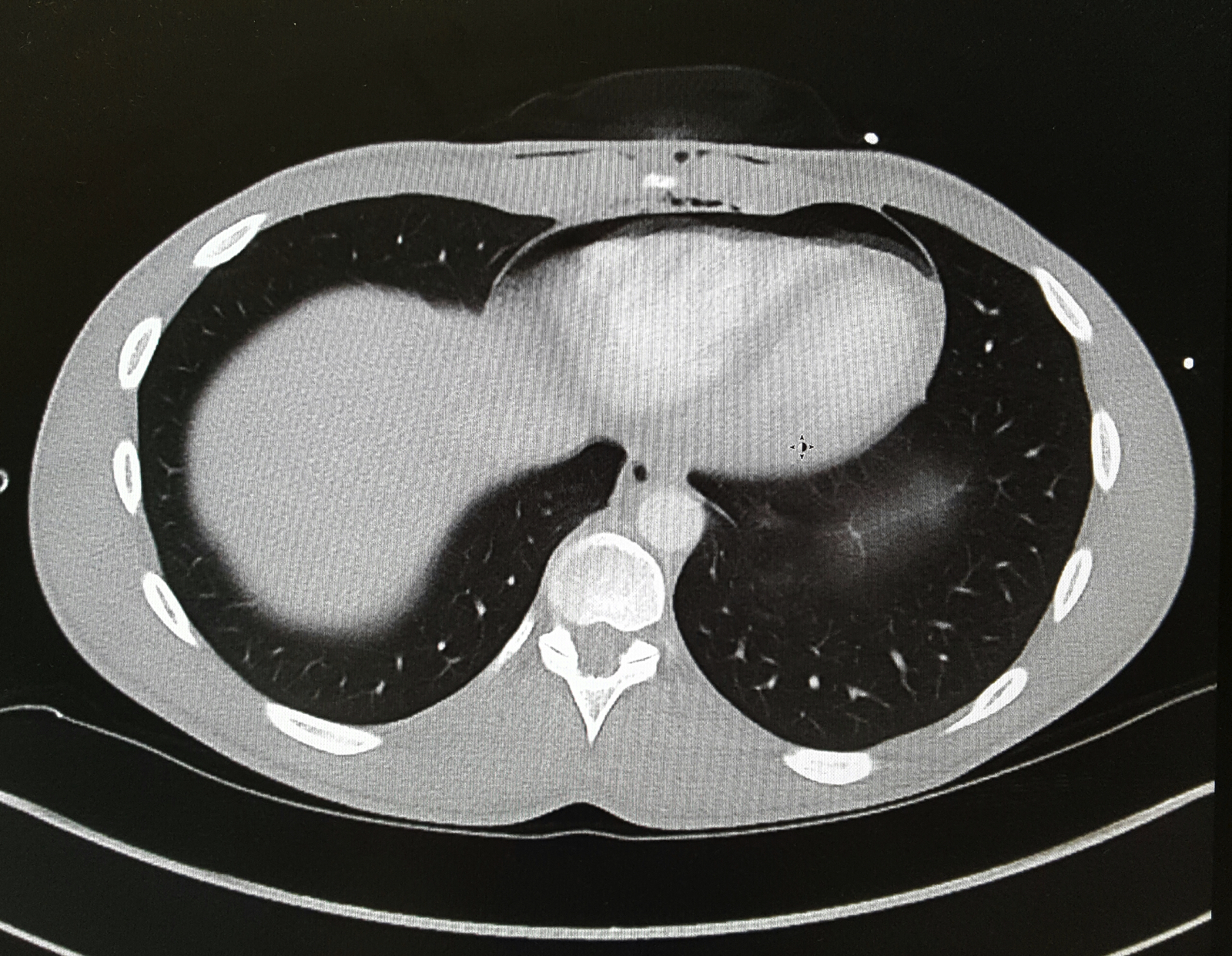
Differential Diagnosis: Bronchial injury, Diaphragm injury, Hemothorax, Tension Pneumothorax, Aortic Transection, Esophageal injury, Pneumomediastinum
Evaluation: Ultrasound (FAST Exam), CXR, CTA in stable patients, ECG, troponin.
Management: Penetrating cardiac trauma require emergent thoracotomy, pericardial window.
Clancy K, Velopulos C, Bilaniuk JW, et al. Screening for blunt cardiac injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73(5 Suppl 4):S301-6.
El-menyar A, Al thani H, Zarour A, Latifi R. Understanding traumatic blunt cardiac injury. Ann Card Anaesth. 2012;15(4):287-95.
Tintinalli's 7th Edition. Emergency Medicine Manual. Chapter 164: Cardiothoracic Trauma.
Category: Orthopedics
Posted: 9/10/2016 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Young athletes, especially around the age of puberty, are at higher risk for pelvic avulsion fractures
Often seen in sports that require sprinting, rapid changes in movement or jumping
Caused by sudden, forceful contraction of the muscles of the abdominal, the hip and thigh or the hamstring
Avulsion fractures can occur at many areas of the pelvis.
A mnemonic is: Alabama’s stoned rappers got ill hunting armadillos
· Iliac crest: Abdominal muscles
· Anterior superior iliac crest: Sartorius
· Anterior inferior iliac crest: Rectus femoris
· Greater trochanter: Gluteal muscles
· Lesser trochanter: Iliopsoas **(rare in adults)
· Ischial tuberosity: Hamstrings
· Pubic symphysis: Adductor group
http://roentgenrayreader.blogspot.com/2010/07/pelvic-avulsion-fractures.html
** Isolated nontraumatic avulsion fractures of the lesser trochanter in adults is a pathognomonic sign of metastatic disease
This site has some good images of common injury patterns
http://radiopaedia.org/articles/apophyseal-avulsion-fractures-of-the-pelvis-and-hip
http://roentgenrayreader.blogspot.com/2010/07/pelvic-avulsion-fractures.html
Category: Toxicology
Keywords: atypical antipsychotic toxicity (PubMed Search)
Posted: 9/8/2016 by Hong Kim, MD
(Updated: 2/6/2026)
Click here to contact Hong Kim, MD
Antipsychotic as a class has diverse range of toxicity. The atypical (2nd generation) antipsychotics are considered to possess less toxicologic manifestation compared to the typical (1st generation) antipsychotics - lower K channel blockade and minimum Na channel blockade properties. However, select atypical antipsychotics overdose can results in significant morbidity in addition to sedation.
Alpha-1 blockade (hypotension)
Antimuscarinic effect (anticholinergic toxicity)
Delayed rectifier K channel blockade (QT prolongation)
Bottom line: Although lethal overdose from atypical antipsychotics are rare, they can result in significant clinical toxicity when ingested alone or in combintation with other classes of medications.
Category: International EM
Keywords: Cancer, mortality, burden of disease (PubMed Search)
Posted: 9/7/2016 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 9/8/2016)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Bottom Line:
Cancer is a leading cause of death worldwide, accounting for 8.2 million deaths in 2012 (1). The most common causes of cancer death are cancers of:
More than 30% of cancer deaths could be prevented by modifying or avoiding key risk factors, including:
http://www.who.int/mediacentre/factsheets/fs297/en/
Category: Critical Care
Keywords: Intracerebral hemorrhage, intraparenchymal hemorrhage, ICH, IPH, hypertensive emergency, blood pressure, neurocritical care, nicardipine (PubMed Search)
Posted: 8/15/2016 by Daniel Haase, MD
(Updated: 9/6/2016)
Click here to contact Daniel Haase, MD
--Aggressive BP management (SBP <140) in atraumatic intracerebral hemorrhage (ICH) does NOT signifcantly improve mortality or disability compared with traditional goal (SBP <180) [1]
--However, a lower goal (SBP <140) has been shown to decrease hematoma size and be safe compared to a higher goal (SBP <180) [2]
The recently published ATACH-2 study investigated aggressive BP control in hypertensive acute atraumatic ICH/IPH (intraparenchymal hemorrhage). [1]
--Control group SBP 140-179 mmHg vs. intervention group SBP 110-139 mmHg with nicardipine infusion (control group actually had SBP 140-150 vs. intervention group SBP 120-130 most of the time).
--Study stopped early for futility. No difference in mortality or modified Rankin.
Previously, INTERACT2 demonstrated that aggressive SBP management (<140) was safe, decreasing hematoma expansion leading to a change in some individuals' practice. [2]
1. Qureshi AI, Palesch YY, et al; ATACH-2 Trial Investigators and the Neurological Emergency Treatment Trials Network. Intensive Blood-Pressure Lowering in Patients with Acute Cerebral Hemorrhage. N Engl J Med. 2016 Jun 8. [Epub ahead of print] PubMed PMID: 27276234.
2. Anderson CS, Heeley E, et al; INTERACT2 Investigators. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013 Jun 20;368(25):2355-65. doi: 10.1056/NEJMoa1214609. Epub 2013 May 29. PubMed PMID: 23713578.
Category: Pharmacology & Therapeutics
Keywords: FFP,PCC,ICH,warfarin (PubMed Search)
Posted: 9/3/2016 by Michelle Hines, PharmD
Click here to contact Michelle Hines, PharmD
Prothrombin complex concentrate (PCC) and fresh frozen plasma (FFP) are used for INR reversal in patients on vitamin K antagonists (VKA) (e.g., warfarin) with life-threatening bleeding. Guidelines from the Neurocritical Care Society and Society of Critical Care Medicine recommend using PCC over FFP for patients with VKA-associated hemorrhage and an INR >=1.4.
New study-INCH trial:
What they found:
Application to clinical practice:
Frontera JA, Lewin JJ, Rabinstein AA, et al. Guideline for reversal of antithrombotics in intracranial hemorrhage. Neurocrit Care 2016; 24:6-46. (PMID 26714677)
Steiner T, Poli S, Griebe M, et al. Fresh frozen plasma versus prothrombin complex concentrate in patients with intracranial haemorrhage related to vitamin K antagonists (INCH): a randomised trial. Lancet Neurol 2016; 15:566-73. (PMID 27302126)
Follow me on Twitter @mEDPharmD
Category: Infectious Disease
Keywords: Zika, arbovirus, infectious disease, mosquitos (PubMed Search)
Posted: 8/31/2016 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Zika virus and its transmission is currently an important infectious disease topic in the United States and the Western Hemisphere. With domestic spread in the Continental United States, and the likely further spread to other parts of the southern United States, continued vigilance by healthcare providers remains important.
What are the signs and symptoms of Zika?
Most common signs and symptoms are:
Other symptoms can include
Symptoms can generally last 2 to 7 days. Most individuals will have minimal or no significant symptoms and may not seek medical care. These symptoms are similar to other arboviruses, such as dengue or chikungunya. Potential serious complications include Guillian Barre syndrome.
Of course, the main concern remains infection of pregnant women and the impact that Zika has on the developing fetus, especially for the brain.
https://www.cdc.gov/zika/symptoms/symptoms.html
Shastry S, Koenig KL, Hirshon JM. Zika Virus: Critical Information for Emergency Providers. Emerg Med Clin North Am. 2016 Aug;34(3):e25-37.
Category: Critical Care
Keywords: refractory status epilepticus, ketamine, propofol, siezure, midazolam (PubMed Search)
Posted: 8/30/2016 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Ketamine for RSE?
Legriel S, et al. What's new in refractory status epilepticus? Intensive Care Med 2016. [Epub ahead of print]
Category: Pediatrics
Keywords: procedural sedation (PubMed Search)
Posted: 8/26/2016 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Alai, A. Nitrous Oxide Administration. Medscape/emedicine. http://emedicine.medscape.com/
Guideline for Monitoring and Management of Pediatric Patients During and After Sedation Diagnostic and Therapeutic Procedures. American Academy of Pediatrics. 2011
Clinical Policy: Critical Issues in the Sedation of Pediatric Patients in the Emergency Department. Annals of Emergency Medicine, 51(4):378-399 (2008)
Category: Neurology
Keywords: cerebellar disease, tremor, nystagmus (PubMed Search)
Posted: 8/24/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Ataxia is an important clinical sign of cerebellar pathology, but how is it actually described?
Stance ataxia: inability to stand with feet together for more than 30 seconds
Gait ataxia
Sensory ataxia: the first 2 elements, in addition to a positive Romberg sign
Truncal ataxia: oscillation of body while sitting or standing
Limb ataxia: functional impairment in performing actions such as writing or buttoning and improves with slowing down the movement
Dysdiadokinesia: impairment of rapidly alternating movement
Intention tremor: tested by finger-to-nose and heel-to-shin.
Dysmetria: pastpointing or undershooting on finger-chasing or shin-tap.
Dysarthria: irregular and slow speech with unnecessary hesitation
Nystagmus and other ocular disturbances, such as ocular flutter and opsoclonus.
The first 3 are present in both cerebellar pathology and loss of proprioceptive input, the rest are usually due to cerebellar pathology or ataxic syndrome.
Ashizawa T and Xia G. Ataxia. Continuum 2016;22(4):1208-1226
Category: Critical Care
Keywords: DKA (PubMed Search)
Posted: 8/23/2016 by Rory Spiegel, MD
Click here to contact Rory Spiegel, MD
Is it possible to have a patient present in diabetic ketoacidosis (DKA) with both negative serum and urinary ketone levels?
A case report published in American Journal of Emergency Medicine by Jehle et al provides a helpful reminder of this phenomenon (1). The degree of acidosis is directly related to the ratio of the various ketones/ketone metabolites: acetone, acetoacetate and beta-hydroxybutyrate present in the serum. The proportion of each respective substance is determined by the existing redox state in the blood. At any given time, acetoacetate and beta-hydroxybutyrate exist in an equilibrium dependent upon the ratio of NAD+ and NADH(fig.1). These substances freely convert with the assistance of the enzyme beta-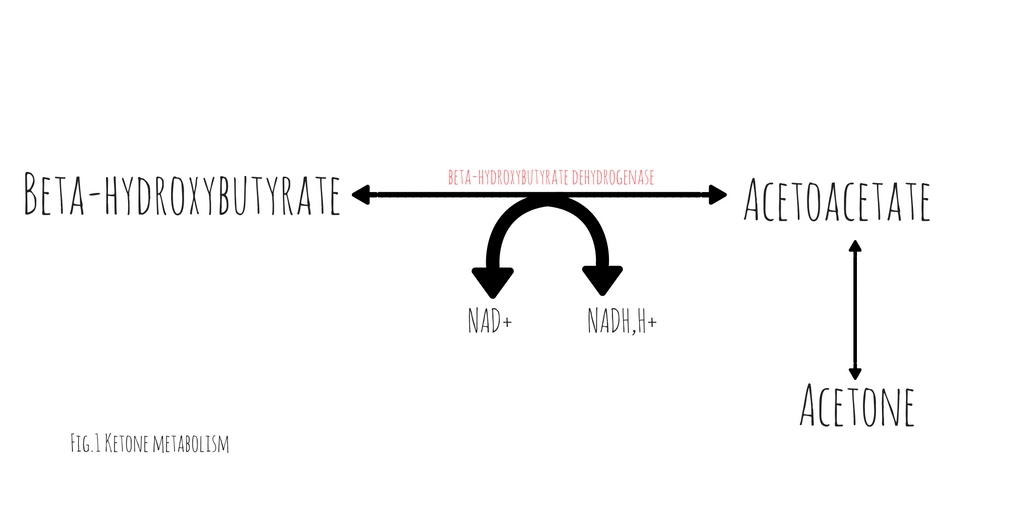 hydroxybutyrate dehydrogenase (2). This conversion requires the donation of a hydrogen atom from NADH. The balance between beta-hydroxybutyrate and acetoacetate, is determined by the ratio of NADH to NAD+. Acetoacetate will freely degrade into acetone through non-enzymatic decarboxylation. Early in DKA, acetoacetate is the most prevalent substance. As the disease progresses and the serum ratio of NADH to NAD+ increases, the proportion of beta-hydroxybutyrate rises, decreasing the quantity of acetoacetate and acetone.
hydroxybutyrate dehydrogenase (2). This conversion requires the donation of a hydrogen atom from NADH. The balance between beta-hydroxybutyrate and acetoacetate, is determined by the ratio of NADH to NAD+. Acetoacetate will freely degrade into acetone through non-enzymatic decarboxylation. Early in DKA, acetoacetate is the most prevalent substance. As the disease progresses and the serum ratio of NADH to NAD+ increases, the proportion of beta-hydroxybutyrate rises, decreasing the quantity of acetoacetate and acetone.
Traditional serum and urinary ketone assays react strongly to acetoacetate but neither reliably react with beta-hydroxybutyrate. Patients in whom the majority of their anion gap is filled by beta-hydroxybutyrate, urinary or serum ketone levels may be negative. In such cases, serum beta-hydroxybutyrate assays would be positive but are not universally available.
It is important to note, with resuscitation and insulin therapy, the ratio of NADH/NAD+ will start to normalize causing an increase in the quantity of acetoacetate. As the patient improves and the anion gap clears, the degree of ketones detected in the serum and urine will paradoxically increase.
1. Jehle D, et al, Severe diabetic ketoacidosis presenting with negative serum ketones: First case report and a review of the mechanism, Am J Emerg Med (2016)
2. Konijn, Abraham M., Naama Carmel, and Nathan A. Kaufmann. The redox state and the concentration of ketone bodies in tissues of rats fed carbohydrate free diets. The Journal of nutrition 10 (1976): 1507.
Category: Orthopedics
Keywords: Patellofermoral Syndrome (PubMed Search)
Posted: 8/20/2016 by Michael Bond, MD
(Updated: 2/6/2026)
Click here to contact Michael Bond, MD
According to the 4th International Patellofemoral Pain Research Retreat recently published in British Journal of Sports Medicine, the core criterion required to define Patelofemoral Pain (PFP) syndrome is pain around or behind the patella, which is aggravated by at least one activity that loads the patellofemoral joint during weight bearing on a flexed knee (eg, squatting, stair ambulation, jogging/running, hopping/jumping).
Additional criteria (not essential):
PFP is common in young adolescents, with a prevalence of 7–28%, and incidence of 9.2%.
Stay tuned for recommendations on treatment and diagnosis.
Category: Pediatrics
Keywords: Trampoline, injury patterns (PubMed Search)
Posted: 8/19/2016 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
From 2010-2014 ED visits in the US for injuries from trampoline parks (TPI) increased from 581 visits per year to 6932 visits per year. There was no change in the number of injuries related to home trampoline use. TPI were more likely to involve the lower extremity, be a dislocation and warrant admission and less likely to involve the head.
Bottom line: TPIs are increasing and have a different injury pattern compared to home trampolines.
Kasmire K, Rogers S and Sturm J. Trampoline Park and Home Trampoline Injuries. Pediatrics 2016: 138 (3).
Category: Toxicology
Keywords: One pill killers, pediatric (PubMed Search)
Posted: 8/17/2016 by Hong Kim, MD
(Updated: 8/18/2016)
Click here to contact Hong Kim, MD
In pediatric population, small dose or single pill ingestion can potential result in severe or lethal toxicity.
Clinicians should be mindful of potential toxicity following xenobiotic exposure (below) in pediatric population, especially under the age of 5 years old, even if the patient may initially appear asymptomatic.
Suspected ingestion of above medications/xenobiotics may warrent observation up to 24 hours in asymptomatic pediatric population.
Category: International EM
Keywords: Climate change, infectious diseases, environment (PubMed Search)
Posted: 8/17/2016 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
July 2016 was the hottest month ever recorded. As the temperature of the planet continues to rise, changes in infectious disease patterns of transmission are likely to occur. Many formerly exotic diseases, such as Zika, West Nile, malaria and cholera are spreading to new areas. Some of these are now found in the United States. Below is a table (from M. L. Wilson) that exemplifies how environmental changes can impact infectious diseases.
Bottom Line: Remain vigilant for unusual infectious diseases, especially among travelers. However recognize that many diseases have the potential to spread to the U.S., especially considering ongoing environmental changes.
www.who.int/globalchange/environment/en/chapter6.pdf
http://www.chgeharvard.org/topic/climate-change-and-infectious-disease
http://www.who.int/globalchange/climate/summary/en/index5.html
Wilson, M.L., Ecology and infectious disease, in Ecosystem Change and Public Health: A Global Perspective, J.L. Aron and J.A. Patz, Editors. 2001, Johns Hopkins University Press: Baltimore. p. 283-324.
Category: Orthopedics
Keywords: Hand infection (PubMed Search)
Posted: 8/13/2016 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
47yo M chef presents to your ED with 2 days of worsening left hand pain after sustaining a puncture wound to hand at work. The hand is red and swollen and he complains of pain. Interestingly, his index and middle digits are in an ABducted position at rest.
Collar Button Abscess
Web space infection of the palmer AND dorsal hand
The Palmer aponeurosis prevents volar extension (but promotes dorsal encroachment)
The pus spreads between the MC bones and erupts dorsally....creating a DORSAL abscess.
Loss of palmer concavity is seen.
ABduction of the adjacent digits, resulting in a "V" configuration with the apex pointing to the site of infection. This would not happen from simple pus in the dorsal space!
Can be missed if only focused on the dorsal hand. The palm will show the original injury (splinter, cut, foreign body)
Treatment is urgent surgical drainage.
http://www.eplasty.com/article_images/eplasty16ic06_fig1.gif
| Collar Button Abscess 2016 www.eplasty.com | |
| Elle Kalbfell, BSa, Nicholas S. Adams, MDa,b, and William T. Cullen, MD, MA, FACSa,b,c | |
|
|
Category: Neurology
Keywords: Uncal herniation, ipsilateral hemiplegia, Kernohan's notch, Kernohan's sign (PubMed Search)
Posted: 8/10/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD

Diagram modified from "Localised Neurological Disease and Its Management A Intracranial". clinicalgate.com/localised-neurological-disease-and-its-management-a-intracranial/. Accessed 10 Aug 2016.
Follow me on Twitter @EM_NCC
