Category: Critical Care
Posted: 3/22/2011 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Aspiration Pneumonitis and Pneumonia
Ragavendran K, Nemzek J, Napolitano LM, Knight PR. Aspiration-induced lung injury. Crit Care Med 2011; 39:818-26.
Category: Geriatrics
Keywords: geriatric, elderly, rib fractures (PubMed Search)
Posted: 3/20/2011 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Rib fractures are associated with significant morbidity and mortality in the elderly, and the risk increases dramatically with each successive rib fractured. An elderly patient with 3 rib fractures has a mortality of 20% and risk of pneumonia is 31%. As a general rule, you should really think twice about discharging home any elderly patients with rib fractures.
[credit to Dr. Joe Martinez for bringing forth this information]
Bulger EM, Arneson MA, Mock CN, et al. Rib fractures in the elderly. J Trauma 2000;48:1040-1046.
Category: Orthopedics
Posted: 3/12/2011 by Michael Bond, MD
(Updated: 3/19/2011)
Click here to contact Michael Bond, MD
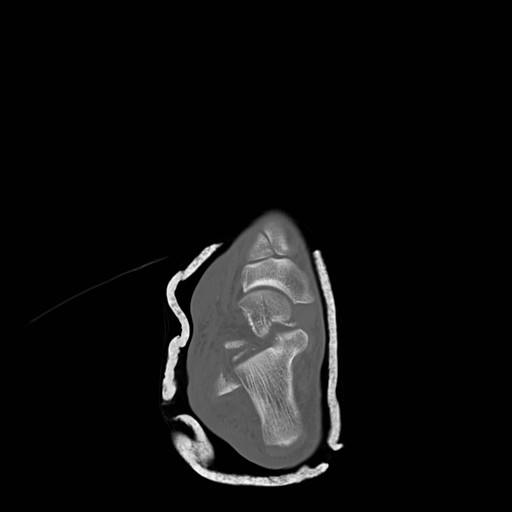
Talar Neck Fractures
Have a high rate of avascular necrosis (AVN), nonunion, and arthritis. Almost all require ORIF


Category: Toxicology
Keywords: rocuronium, succinylcholine (PubMed Search)
Posted: 3/17/2011 by Fermin Barrueto
(Updated: 2/7/2026)
Click here to contact Fermin Barrueto
Most have converted from succinylcholine to rocuronium for their choice of paralytic in RSI. Succinylcholine-induced hyperkalemia secondary to muscle fasciculations is considered usually clinically insignificant though there may be a hyperkalemic renal patient that this may tip them over. The fasciculations also may worsen traumatic long bone fractures. Here is the argument in a head to head comparison:
| Succinylcholine | Rocuronium | Winner | |
| Onset | 1-1.5min | 1.5-3min | Tie |
| Duration Recovery Index | 3-7min 2min
| 30-40min 10min | Mild S |
| Fasciculations | Yes | No | Roc |
| Histamine | Yes - Released | None | Roc |
| Pulse | Rare Brady | Rare Tachy at high dose | Tie |
Duration = injection of drug to 25% recovery of single twitch height (clinically relevant recovery in ED - essentially breathing may return)
Recovery Index = time from 25% to 75% recovery of single twitch height
The main reason succinylcholine was utilized was because of its fast onset and short duration. Rocuronium is comparable enough to succinylcholine in these characteristics tilting the overall benefits to rocuronium. If the FDA ever approves it, suggamadex is a possible reversal agent for rocuronium - currently used in Europe. Imagine having that in your RSI kit.
Category: Neurology
Keywords: metronidazole, neuropathy (PubMed Search)
Posted: 3/17/2011 by Aisha Liferidge, MD
(Updated: 2/7/2026)
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Keywords: pulmonary physiology, critical care, respiratory alkalosis (PubMed Search)
Posted: 3/15/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Many changes in pulmonary physiology occur during pregnancy. These changes are generally well tolerated but can become problematic when pathologic states arise.
Here are a few examples of the normal changes and potential consequences:
Progesterone increases tidal volume and respiratory rate.
“Normally" a mild respiratory alkalosis pH 7.4-7.47, PaCO2 28-32, and bicarbonate 17-22 (renal compensation).
Low metabolic reserve with systemic illness.
Weight gain, anasarca, and breast size reduces chest wall elasticity.
Potential for restrictive physiology and reduced lung volumes.
Can be challenging to to mechanically ventilate due to decreased compliance and intra-thoracic pressure
Mechanical displacement of abdominal and thoracic contents by growing uterus.
Reduced lung volumes leading to reduced oxygen reserve and decreased apnea time.
Aim higher if placing chest tube (avoid abdominal contents)
Uterine pressure on stomach can increase aspiration risk and pulmonary injury.
Chestnutt, A. Physiology of Normal Pregnancy. Crit Care Clinic 20 (2004) 609-615
Category: Visual Diagnosis
Keywords: lung, ultrasound, pneumonia, hepatization, sonogram, air bronchograms (PubMed Search)
Posted: 3/13/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
65 yo female with breast cancer presents with dyspnea and CXR shown below. Diagnosis? Can anything help clarify the diagnosis?
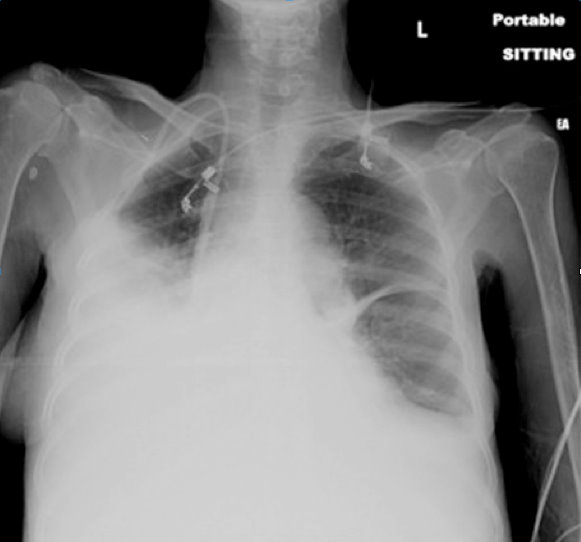
The CXR shows an opaque right hemithorax, consistent with a pleural effusion, a large consolidation, or both. Ultrasound of the lung can clarify this ambiguity.
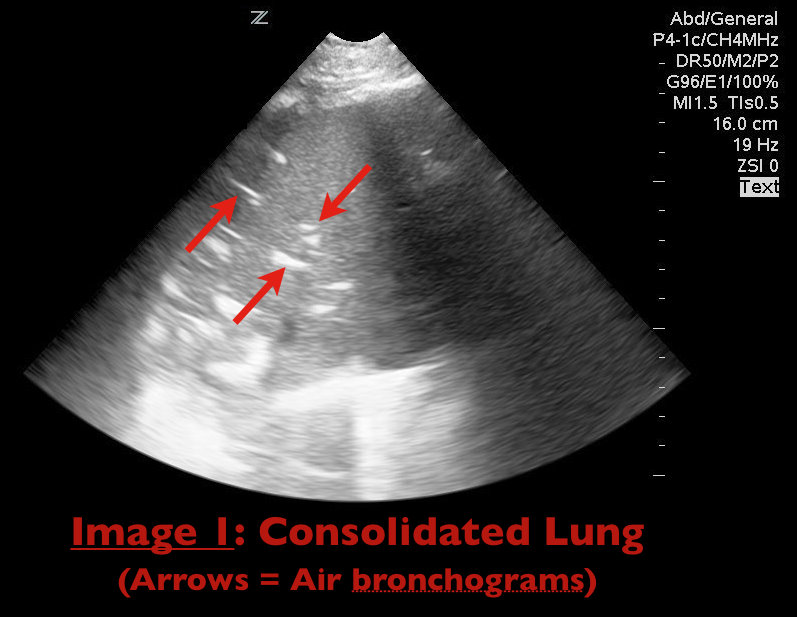
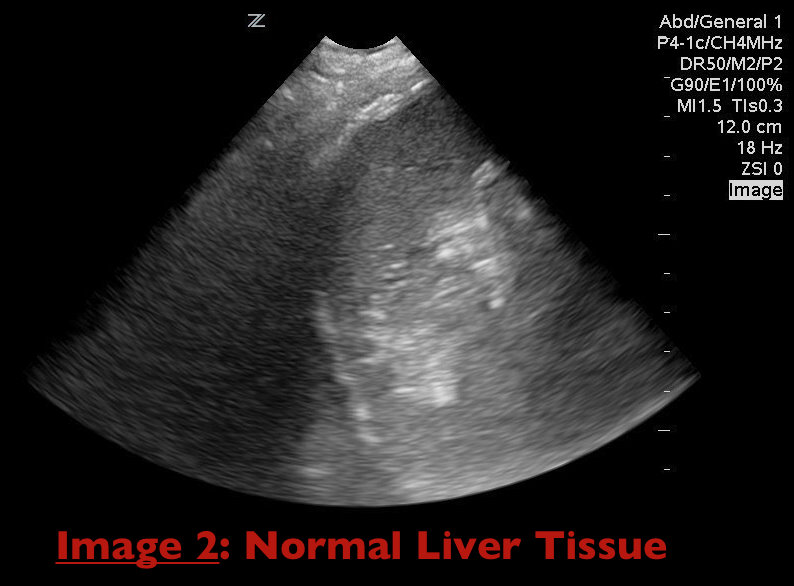
Consolidation of lung parenchyma (e.g., pneumonia) appears isoechoic to liver tissue on ultrasound and air bronchograms appear as hyperechoic areas within the consolidated lung parenchyma (Image 1). Together these findings are termed "hepatization" of the lung as consolidated lung appears similar to liver parenchyma on ultrasound (Image 2).
Durant, A. Nagdev, A. Ultrasound detection of Lung Hepatization. West J Emerg Med. 2010 September; 11(4): 322-323.
Category: Geriatrics
Keywords: hypovolemia, geriatric, elderly (PubMed Search)
Posted: 3/14/2011 by Amal Mattu, MD
(Updated: 2/7/2026)
Click here to contact Amal Mattu, MD
Elderly patients are prone to hypovolemia for the following two major reasons:
1. They have a decreased thirst response.
2. They have decreased renal vasopressin response to hypovolemia.
The result is that elderly patients have an impaired ability to compensate for a decreased cardiac output, which causes them to develop shock earlier and more easily with stressor.
Takeaway point: Always assume that most elderly patients are hypovolemic, and when they are stressed, give them fluids early!
Category: Orthopedics
Keywords: nerve entrapment, ulnar nerve, elbow (PubMed Search)
Posted: 3/12/2011 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Cubital Tunnel Syndrome aka Radial Tunnel Syndrome
Category: Toxicology
Keywords: benzyl alcohol, clonidine, ethanol, chloramphenicol (PubMed Search)
Posted: 3/9/2011 by Bryan Hayes, PharmD
(Updated: 3/10/2011)
Click here to contact Bryan Hayes, PharmD
Several medications/chemicals can cause unique toxicologic reactions in pediatric patients.
Category: Neurology
Keywords: seizure, idiopathic seizure (PubMed Search)
Posted: 3/9/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
The onset of idiopathic seizures typically affects patients between ages 5 and 20.
Therefore, be highly suspicious of a diagnosable etiology in patients who present with new onset seizure prior to age 5 or after age 20.
Common causes of such seizures include:
Category: Critical Care
Posted: 3/8/2011 by Mike Winters, MBA, MD
(Updated: 2/7/2026)
Click here to contact Mike Winters, MBA, MD
The Severely Hypoxemic ED Patient
Patroniti N, Isgro S, Zanella A. Clinical management of severely hypoxemic patients. Curr Opin Crit Care 2011; 17:50-56.
Category: Geriatrics
Keywords: adverse drug effects, side effects, interactions (PubMed Search)
Posted: 3/7/2011 by Amal Mattu, MD
(Updated: 2/7/2026)
Click here to contact Amal Mattu, MD
Adverse drug effects are a major issue in geriatrics.
Elderly patients take, on average, 5 prescription medications + 2 over-the-counter medications.
Adverse drug effects account for approximately 5% of all hospital admissions.
Nearly 20% of patients brought to the ED for psychiatric complaints have symptoms that are primarily caused by medication effects.
Be very wary whenever prescribing ANY new medications for even a short time to elderly patients.
Category: Pharmacology & Therapeutics
Keywords: PCP, clindamycin, primaquine, pentamidine, dapsone, atovaquone (PubMed Search)
Posted: 2/22/2011 by Bryan Hayes, PharmD
(Updated: 3/5/2011)
Click here to contact Bryan Hayes, PharmD
Sulfamethoxazole (SMX)/trimethoprim (TMP) is the treatment of choice for PCP pneumonia. The IV formulation has been unavailable for almost a year due to shortage. It is contraindicated in patients with sulfa allergy. Here are the alternatives with adverse effects. You'll quickly see why pentamidine should generally be reserved for those with sulfa allergy and G6PD deficiency.
Mild-to-moderate disease:
Moderate-to-severe disease:
Adverse Effects:
Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents. MMWR April 10, 2009 / 58(RR04);1-198.
Category: Pediatrics
Keywords: Influenza (PubMed Search)
Posted: 3/2/2011 by Mimi Lu, MD
(Updated: 3/5/2011)
Click here to contact Mimi Lu, MD
Now that influenza season is in full swing, remember that early antiviral treatment can reduce the risk of complications in high-risk individuals. One of those high-risk groups is children <2 years, with the highest hospitalizations and mortality in infants <6 months.
According to the CDC website:
Recommended antiviral medications (neuraminidase inhibitors) are not FDA-approved for treatment of children aged <1 year (oseltamivir) or those aged <7 years (zanamivir). Oseltamivir was used for treatment of 2009 pandemic influenza A (H1N1) virus infection in children aged <1 year under an Emergency Use Authorization, which expired on June 23, 2010. Nevertheless,
Current CDC guidance on treatment of influenza should be consulted; updated recommendations from CDC are available at http://www.cdc.gov/flu
.
Category: Toxicology
Keywords: Brown Recluse,envenomation,spider,loxoscelism (PubMed Search)
Posted: 3/3/2011 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Recently a case report was published in which a child was incorrectly diagnosed with MRSA. He actually had systemic loxoscelism from a Brown Recluse spider bite.
A patient who has been bitten by brown recluse spider bite may present with pruritis, pain and swelling. The classic lesion has a bluish-purple central region, surrounded by concentric rings of pale ischemia and erythema. (“red, white and blue”) Bites may progress over days to a bleb with necrosis and eschar formation, followed by ulceration.
Systemic loxoscelism presents with a scarlatiniform rash that spreads dependently. It may have the classic purple lesion surrounded by concentric rings of pale ischemia and erythema. The patient may be uncomfortable but is usually stable. Treatment is supportive care.

Rogers, KM, Klotz CR, Jack M, Seger D. Systemic Loxoscelism in the Age of Community-Acquired Methicillin-Resistant Staphylococcus aureus. Ann of EM Feb 2011 57(2); 138-40.
Category: Neurology
Keywords: phenytoin, dilantin, seizure, dilantin level, phenytoin level (PubMed Search)
Posted: 3/2/2011 by Aisha Liferidge, MD
(Updated: 2/7/2026)
Click here to contact Aisha Liferidge, MD
Category: Visual Diagnosis
Keywords: ultrasound, ectopic, free fluid, hypotension, pregnancy (PubMed Search)
Posted: 2/27/2011 by Haney Mallemat, MD
(Updated: 8/28/2014)
Click here to contact Haney Mallemat, MD
24 yo woman presents with syncope, abdominal pain, and normal menses 4 days prior. Urine HCG(+) and quantitative beta-HCG is 1300 with the transvaginal ultrasound seen below. Diagnosis?

Ectopic Pregnancy Pearls
Tintinalli, Judith, et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7th Edition. 2011, McGraw-Hill Companies, Inc, China
Category: Cardiology
Keywords: short QT, QT, QT interval, QTc (PubMed Search)
Posted: 2/27/2011 by Amal Mattu, MD
(Updated: 2/7/2026)
Click here to contact Amal Mattu, MD
The long QT syndrome and causes of acquired long QT interval are well-known to most emergency physicians, but a short QT can be problematic as well. Short QT-syndrome is an inherited ion-channel disease that predisposes to ventricular dysrhythmias and sudden death. The QTc in these patients is generally < 340 msec. This condition is more common in children, and it should be considered in the differential diagnosis and evaluated on ECG in children presenting with syncope.
Category: Orthopedics
Keywords: apophysitis, overuse injuries, heel pain, achilles (PubMed Search)
Posted: 2/26/2011 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Sever's disease ,aka calcaneal apophysitis, is a common overuse injury in the pediatric and adolescent population.
Occurs secondary to traction of the calcaneus that most often occurs in young athletes (8-12 yo)
-Avg. age of presentation is 11 years 10 months in boys & 8 years 8 months in girls
-Repetitive traction to the weaker apophysis, induced by the pull of the Achilles on its insertion
Hx: Heel pain that increases with activity (running, jumping).
-May involve one (40%) or both (60%) feet
PE: Tenderness of the posterior heel at the Achilles tendon insertion and ankle dorsiflexor weakness
Imaging: Radiography is often normal. When positive, show fragmentation and sclerosis of the calcaneal apophsis. NOTE: These findings are nonspecific and also are observed in asymptomatic feet.
http://t0.gstatic.com/images?q=tbn:ANd9GcQ9R-fx1iyhbhNJpNL2W72bWdK72_mRBLNX5DUDtcMfnDli-x7Ong
DDx: Includes osteomyelitis and tarsal coalition.
Tx: Rest from aggravating activities, NSAIDs, ice (both pre and post sport). When pain free a program of stretching (gastrocnemius-soleus), strengthening (dorsiflexors) and shoe inserts (heel cups, lifts, pads, or orthotics) can provide significant pain relief.
